Increasing demand on health services during times of austerity has necessitated examination of the way we deliver health care.1,2 In 2008, Western Australian tertiary hospital emergency departments (EDs) were experiencing the highest rates of access block (the percentage of patients who wait longer than 8 hours for an inpatient bed) in the country.3,4 The well documented relationship between access block and poor health outcomes for patients,5-9 coupled with adverse media and public opinion about Western Australia’s public hospitals, demanded a significant response. A Minister for Health delegation travelled to the United Kingdom to examine National Health Service (NHS) reforms,10,11 to learn from their successes to improve health care delivery in WA. Subsequently, in April 2009, the Four Hour Rule (FHR) Program was launched in WA.12 Stage 1 of the program involved the state’s four tertiary public hospitals: Princess Margaret Hospital for Children, Royal Perth Hospital, Sir Charles Gairdner Hospital and Fremantle Hospital.
WA hospitals were initially set the same final FHR target as hospitals in the UK, which was that 98% of all patients presenting to their ED should be admitted, discharged or transferred within 4 hours of arrival. However, key differences between the two programs were that the WA FHR program had a clear and defined focus on monitoring patient safety and quality outcomes, that there were no financial incentives or sanctions for hospitals that achieved or failed to achieve the set targets, and the launch coincided with a challenging time in global finances. This presented a compelling need to examine systems and processes, so, while limited funding was made available to support change initiatives, it was agreed there would be no allocation of recurrent funding, meaning no additional beds or staff. In June 2010, the UK government introduced a suite of new clinical quality indicators and reduced their FHR target to 95%.13 The purpose of these new indicators, which were very similar to those already being monitored in WA’s FHR program, was to broaden the measurement of quality to cover effectiveness of treatment and patient satisfaction.
The aim of WA’s FHR program was to improve patients’ experience and quality of care by reducing delays in the ED and streamlining processes throughout the hospital. With the recent introduction of the National Emergency Access Target (NEAT),14 we report our experience of establishing a successful FHR program.
Princess Margaret Hospital for Children (PMH) in Perth, WA, is a 220-bed tertiary paediatric hospital, that has more than 65 000 presentations to the ED annually. The FHR program used a clinical services redesign model, based on principles from Six Sigma and “lean thinking”. Clinical services redesign is a proven, rigorous international model used in large complex organisations.15-17 The model is data-driven and consumer- (ie, patient-) focused. Six Sigma is a disciplined, data-driven approach for eliminating defects in processes.18 The Six Sigma improvement model consists of five phases: Define, Measure, Analyse, Improve and Control (DMAIC). Lean is a collection of tools and principles that aim to improve health services by eliminating waste, adding value to processes and allowing continuous improvement.19
Key outcome measures included the overall FHR percentage (ie, percentage of all patients presenting to the ED whose management complied with the FHR), and the percentages of patients admitted, discharged or transferred from the ED for whom this happened within 4 hours of arrival at triage, and the percentage of patients discharged from inpatient wards before 10 am and 12 pm. Critical countermeasures (Box 1) were also reported to ensure that any potential adverse effects of the program were apparent immediately. The Princess Margaret Hospital Ethics Committee approved the reporting of this study (ethics number, 3637).
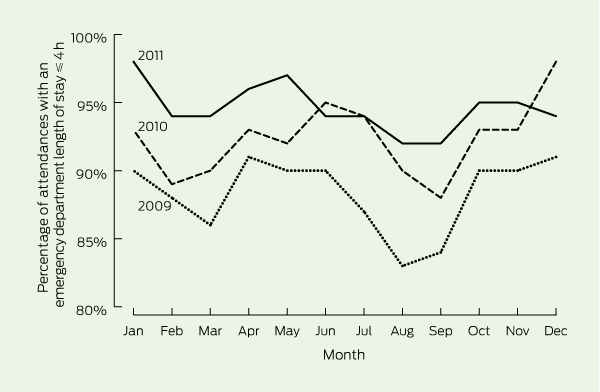
The overall FHR performance at PMH increased steadily over the first 3 years of the program, averaging 87% in 2009 and 95% in 2011 (Box 2). The increase in overall performance resulted from improvements in both the percentage of patients being admitted to hospital within 4 hours (62% in 2009; 74% in 2010; and 80% in 2011), and those being discharged home from the ED within 4 hours (94% in 2009; 96% in 2010; and 98% in 2011).
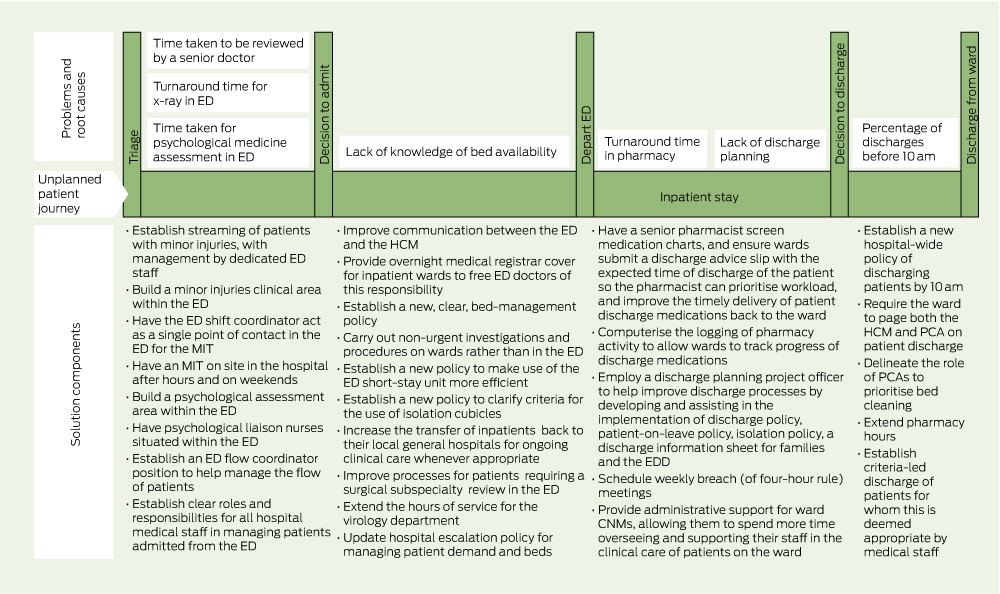
The Define phase of DMAIC identified more than 400 issues, with common themes including duplication of processes, lack of resources, mismatch between demand and availability of key services, poor communication and inadequate discharge planning. After grouping, 30 major issues remained. These were measured to determine their size and impact, followed by root-cause analysis and generation of solutions (Box 3).
ED attendances increased by 12.3% from 2009 to 2011 (Box 1). During this period, the admission rate from the ED fell, but with the increase in ED attendances, the total number of patients admitted increased marginally. There was no significant change in the percentage of unplanned reattendances to the ED within 48 hours of discharge, the percentage of patient complaints or inhospital mortality. In addition, the number of elective surgeries performed at PMH increased by 9% from 2009 to 2011.
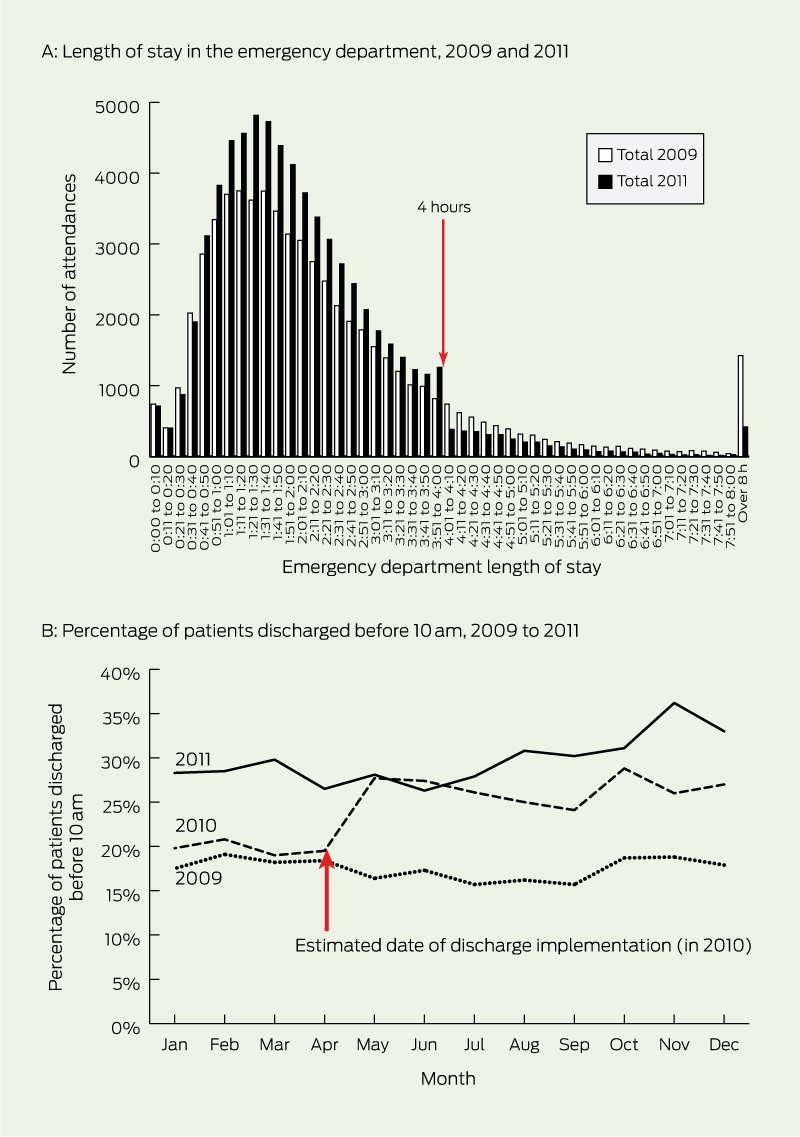
In response to UK studies suggesting that some patients were being “pushed” out of EDs just before the 4-hour target, with a spike in ED departures between 3.5 hours and 4 hours,20-22 we used a critical countermeasure, with a weekly figure showing the total time each patient spent in the ED (Box 4, A). In 2011, the median length of stay for all patients attending the ED was less than 2 hours, with only a small spike in activity before the 4-hour mark. For patients being admitted to hospital in 2011, 30% departed the ED within 2 hours, 60% within 3 hours and 80% within 4 hours of arrival. Access block fell from 2.4% in 2009 to 0.6% in 2011.
The key factor contributing to the improvement in patients being admitted from the ED within 4 hours was the increase in the percentage of patients being discharged home from an inpatient bed before 10 am. In April 2009, only 18% of all patients discharged home on a particular day were discharged before 10 am, with 50% still occupying their bed at 3 pm. PMH now consistently discharges over 30% of all patients before 10 am and 55% by 12 pm (Box 4, B).
A UK study comparing performance of hospitals close to the border between England (where waiting time targets existed) and Wales (where such targets did not), showed that patients attending English hospitals faced shorter ED waiting times and had lower mortality rates than those attending Welsh hospitals,23 consistent with the recent finding of reduced mortality rates in WA hospitals after the FHR program was introduced.8 However, there remains much debate about the pros and cons of setting targets in health, with advocates suggesting they have the potential to drive hospital-wide change and sceptics fearing adverse consequences, such as gaming and the neglect of areas not subject to targets.22,24,25 The strong leadership of WA’s FHR program, the emphasis on monitoring performance across all areas of the hospital and the lack of financial incentives for achieving “the target”, have been important factors in reducing the likelihood of adverse outcomes. In addition, while clinical staff were actively involved in the redesign process, helping to determine the direction of change, the hospital Executive made the program part of their core business and were accountable for the implementation of change.26
Our study has some limitations. Our experience and results in a tertiary paediatric hospital may not be reproducible in mixed or adult tertiary hospitals where higher admission rates, patients with multiple comorbid conditions, and dependence on community services to facilitate the discharge of elderly patients, create a greater challenge.12 In addition, the quality measures that we reported were relatively limited and may not have identified all the changes (positive and negative) resulting from the FHR program accurately.
The FHR program provided a unique opportunity to redesign aspects of the patient journey, resulting in significant and sustained benefits for patients and staff. The focus of the redesign program must remain on improving the quality of care for patients, rather than on achieving “the target”. The top 10 lessons we learned are summarised in Box 5.
1 Quality measures for the Four Hour Rule Program at Princess Margaret Hospital, Perth, Western Australia, 2009 to 2011
Rate of inhospital mortality for admissions from ED (95% CI) |
|||||||||||||||
2 Overall Four Hour Rule Program performance at Princess Margaret Hospital, Perth, Western Australia, 2009 to 2011
4 Additional measures of Four Hour Rule Program performance at Princess Margaret Hospital, Perth, Western Australia
5 Top 10 lessons learned in implementing a 4-hour-rule program
Ensure the focus for change is hospital-wide and involve as many people from all areas of the hospital as possible.
Stay true to the methods and resist all temptation to “jump to solutions”.
Ensure accurate data are available in real time, and share it with all hospital staff.
Identify and engage local champions for change.
Ensure solutions are created and developed by staff working at grassroots level in the areas requiring change.
Ensure there is strong governance with clear responsibility and accountability for all solutions.
Ensure the hospital executive view the program as a priority.
Improving discharge processes is the most effective way to reduce access block in the emergency department.
To effect real change, targets must be a challenge to achieve.
Ensure there are simple ways for clinical staff to raise issues or concerns in an open and non-confrontational manner.
Received 7 July 2012, accepted 2 December 2012
- Liana Maumill1
- Mia Zic2
- Amanda A Esson1
- Gary C Geelhoed1
- Meredith M Borland1
- Christopher Johnson1
- Philip Aylward1
- Andrew C Martin1
- Princess Margaret Hospital for Children, Perth, WA.
We thank the staff at PMH who participated in the Four Hour Rule Program and the Health System Improvement Unit, Department of Health, WA.
No relevant disclosures.
- 1. Lowthian JA, Curtis AJ, Jolley DJ, et al. Demand at the emergency department front door: 10-year trends in presentations. Med J Aust 2012; 196: 128-132. <MJA full text>
- 2. O’Connell TJ, Ben-Tovim DI, McCaughan BC, et al. Health services under siege: the case for clinical process redesign. Med J Aust 2008; 188 (6 Suppl): S9-S13. <MJA full text>
- 3. Australian Institute of Health and Welfare. Australian hospital statistics 2010–2011: emergency department care and elective surgery waiting times. Canberra: AIHW, 2011. (AIHW Cat. No. HSE 115; Health Services Series No. 41.) http:// www.aihw.gov.au/publication-detail/?id=10737420662 (accessed Jan 2012).
- 4. Mountain D. Introduction of a 4-hour rule in Western Australian emergency departments. Emerg Med Australas 2010; 22: 374-378.
- 5. Guttman A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department; population based cohort study from Ontario, Canada. BMJ 2011; 342: d2830.
- 6. Sprivulis P, Da Silva J-A, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 2006; 184: 208-212. <MJA full text>
- 7. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust 2006; 184: 213-216. <MJA full text>
- 8. Geelhoed GC, de Klerk NH. Emergency department overcrowding, mortality and the 4-hour rule in Western Australia. Med J Aust 2012; 196: 122-126. <MJA full text>
- 9. Richardson DB, Mountain D. Myths versus facts in emergency department overcrowding and hospital access block. Med J Aust 2009; 190: 369-374. <MJA full text>
- 10. WA Health. Emergency demand UK tour. 17–26 November 2008. Perth: Government of Western Australia Department of Health, 2008. http://www.health.wa.gov.au/hrit/docs/publications/WA_Health_UK_Tour_Report.pdf (accessed Dec 2012).
- 11. Hughes G. Four hour target for EDs: the UK experience. Emerg Med Australas 2010; 22: 368-373.
- 12. Stokes B. Four Hour Rule Program progress and issues review. Perth: Government of Western Australia Department of Health, 2011. http://www.health.wa.gov.au/publications/documents/FourHourRule_Review_Stokes.pdf (accessed Jan 2013).
- 13. United Kingdom Department of Health. A&E clinical quality indicators. Data definitions. London: Department of Health, 2010. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_122892.pdf (accessed Sep 2012).
- 14. Australian Government Department of Health and Ageing. Expert panel — review of elective surgery and emergency access targets under the National Partnership Agreement on Improving Public Hospital Services: Supplementary Annexure. Canberra: DoHA, 2012. http://www.yourhealth.gov.au/internet/yourhealth/publishing.nsf/Content/Expert-Panel-Supplementary-Annexure/$File/D0515_COAG%20Supplementary%20Annexure_SECURED.pdf (accessed Dec 2012).
- 15. Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008; 188 (6 Suppl): S14-S17. <MJA full text>
- 16. Ben-Tovim DI, Bassham JE, Bennett DM, et al. Redesigning care at the Flinders Medical Centre: clinical process redesign using “lean thinking”. Med J Aust 2008; 188 (6 Suppl): S27-S31. <MJA full text>
- 17. O’Connell TJ, Bassham JE, Bishop RO, et al. Clinical process redesign for unplanned arrivals in hospital. Med J Aust 2008; 188 (6 Suppl): S18-S22. <MJA full text>
- 18. Gygi C, DeCarlo N, Williams B. Six sigma for dummies. Hoboken, NJ: Wiley Publishing Inc, 2005.
- 19. Westwood N, James-Moore M, Cooke M. Going lean in the NHS. Coventry: United Kingdom National Health Service, Institute for Innovation and Improvement, 2007. http://www. birminghamcancer.nhs.uk/uploads/document_file/document/4ff2d719358e9870fe000032/going_lean_in_the_nhs.pdf (accessed Nov 2012).
- 20. Locker TE, Mason SM. Analysis of the distribution of time that patients spend in emergency departments. BMJ 2005; 330: 1188-1189.
- 21. Mason S, Nicholl J, Locker T. Targets still lead care in emergency departments. BMJ 2010; 341: c3579.
- 22. Mason S, Weber EJ, Coster J, et al. Time patients spend in the emergency department: England’s 4-hour rule — a case of hitting the target but missing the point? Ann Emerg Med 2012; 59: 341-349.
- 23. Hauck K, Street A. Do targets matter? A comparison of English and Welsh national health priorities. Health Econ 2007; 16: 279-290.
- 24. Kelman S, Friedman JN. Performance improvement and performance dysfunction: an empirical examination of distortionary impacts of the emergency room wait-time target in the English National Health Service. J Public Adm Res Theory 2009; 19: 917-946.
- 25. Grubb J, Bevan G. Have targets done more harm than good in the English NHS? BMJ 2009; 338: 442-443.
- 26. McGrath KM, Bennett DM, Ben-Tovim DI, et al. Implementing and sustaining transformational change in health care: lessons learnt about clinical process redesign. Med J Aust 2008; 188 (6 Suppl): S32-S35. <MJA full text>





Abstract
Objective: To report the experience of implementing a 4-hour-rule program.
Design, setting and participants: A 3-year whole-of-hospital clinical service redesign program in a tertiary paediatric hospital in Western Australia, involving all patients presenting to the emergency department (ED) from 1 January 2009 to 31 December 2011.
Main outcome measures: Percentage of patients admitted, discharged or transferred from the ED within 4 hours of arrival at triage, and percentage of patients discharged from inpatient wards before 10 am.
Results: The percentage of patients admitted, discharged or transferred within 4 hours of arrival at the ED increased from 87% in 2009 to 95% in 2011. Safety and quality measures, including the admission rate from the ED, unplanned reattendances at the ED within 48 hours of discharge, patient complaints and inhospital mortality, remained unchanged. The percentage of patients discharged from inpatient wards before 10 am increased from 18% in 2009 to 30% in 2011.
Conclusions: The introduction of a 4-hour-rule program has resulted in improved timeliness of care for patients throughout the hospital, both in the ED and inpatient wards, with no adverse impact on the quality and safety of clinical care.