The known: Although equitable access to sexual and reproductive health care is a National Women's Health Strategy priority, access to abortion care in Australia is uneven.
The new: Several socio‐demographic factors were associated with a history of abortion among women giving birth in Victoria. During 2010–2019, the proportion who reported abortions declined, primarily among women in major cities. The rate was particularly low among most groups of overseas‐born women.
The implications: Medical abortion may be overcoming geographic and other barriers to abortion care. More comprehensive data on unintended pregnancies and access to reproductive health services by remoteness and migrant status would better guide reproductive health policy and practice.
In 2022, the United Nations Population Fund (UNFPA) declared unintended pregnancy a global crisis: nearly half of all pregnancies around the world are unintended.1 While some of these pregnancies are desired, about 73 million pregnancies end in abortion each year.2,3 In Australia, about 40% of pregnancies are unintended,4 and the annual abortion rate is estimated to be 17.3 per 1000 women aged 15–44 years,5 similar to rates in other high resource regions such as Europe and North America.3 Some planned pregnancies also end in abortion for medical or psychosocial reasons.6
Equitable access to sexual and reproductive health care is one of the priorities of the Australian National Women's Health Strategy.7 However, access to reproductive health care is uneven, particularly abortion care; some areas are deemed “abortion deserts” because of the lack of services.8,9 The introduction of medical abortion in Australia was expected to alleviate some access problems.10 The mifepristone–misoprostol combination (MS‐2 Step) was listed on the Pharmaceutical Benefits Scheme in 2013, subsidising its cost to women.10 Although its availability was followed by a 5.1% annual decline in surgical abortion numbers during 2014–18,5 and higher rates of medical abortion in regional and remote areas than in major cities,8 about one‐third of Australian women still live in areas where medical abortion is unavailable.8
Abortion was decriminalised in all Australian jurisdictions by 2022, but the legal situation differs between states and territories.11 There is no specific national abortion data collection, and most jurisdictions, including Victoria, do not routinely report abortion data.4,6 Information on the characteristics of women who present for abortion is particularly scarce,6 placing limits on the investigation of contributing factors and changes in abortion rates with time, as well as the evaluation of interventions and policy changes for improving access.
In Victoria, perinatal information on a range of maternal characteristics are routinely collected, including on induced abortions prior to a given birth.12,13 Although information about women who are yet to or never give birth is not included in this dataset, it is an important source when assessing factors associated with a history of induced abortion, particularly given the dearth of alternative robust population‐based abortion data. Further, the included information has policy and service delivery implications for postpartum and post‐abortion contraception, including long‐acting reversible contraception, for women who wish to avert rapid repeat pregnancies.
We therefore analysed maternity data records to assess the prevalence of a history of induced abortion among women who gave birth in Victoria during 2010–2019, a period marked by changes to abortion care in Australia associated with the introduction of medical abortion,8 and to explore the association of socio‐demographic factors with a history of induced abortion.
Methods
For our retrospective cohort study, we undertook a secondary analysis of cross‐sectional perinatal data in the Victorian Perinatal Data Collection (VPDC).14 Our report adheres to the REporting of studies Conducted using Observational Routinely‐collected health Data (RECORD) guidelines.15
Our study population included all women registered as having given birth in Victoria during 1 January 2010 – 31 December 2019. In 2020, 74 617 of 294 369 registered births in Australia were in Victoria (25%).16 Each birth (live or stillbirth after at least 20 weeks’ gestation or with a birthweight of at least 400 g) was treated as an exclusive event, and a pregnancy resulting in more than one birth as a single birth episode, as we did not assess infant outcomes. Abortion‐specific surveillance data are not collected in Victoria, but the VPDC includes mandatory items related to obstetric history, including self‐reported induced abortions.
Data collection
The collection of data for mandatory VPDC items commences at enrolment for antenatal care. The self‐reported number of induced abortions is a mandatory item for which a valid value must be entered. Birthing services are responsible for submitting data to the VPDC within 30 days of the woman leaving hospital after giving birth and must ensure that the data accurately reflect those recorded in their own information systems. Validation studies have found a high level of agreement between original medical records and VPDC data, including for the data item “previous induced abortions” (2003, 96.1%; 2011, 89.3%).13
Outcomes
The first outcome was the self‐reported number of induced abortions prior to the index birth (pregnancies that ended in induced abortion before 20 weeks’ gestation; later abortions are not recorded by the VPDC). We counted pregnancies with multiple births as one pregnancy, and coded the “history of induced abortion” as a binary variable for regression analyses. The second outcome was the outcome for the pregnancy preceding the index pregnancy (induced abortion or other: live birth, spontaneous abortion, stillbirth, neonatal death, ectopic pregnancy).
Independent variables
The socio‐demographic characteristics included in our analyses were age group (< 20, 20–24, 25–29, 30–34, 35–39, 40 years or older), parity (number of previous pregnancies that ended in live or stillbirths: 0, 1, 2, 3 or more), gravidity (number of known pregnancies, regardless of gestation time, including the index pregnancy: 1, 2, 3, 4 or more), marital status (in a couple relationship [married or de facto] or not in a couple relationship [never married, divorced, widowed, separated]), region of birth (Australia, or other countries according to the Standard Australian Classification of Countries [SACC]),17 Indigenous status (binary), and postcode‐based socio‐economic status (Index of Relative Socio‐economic Disadvantage [IRSD] quintiles18) and remoteness of residence (based on access to services) at the index birth (Australian Statistical Geography Standard Remoteness Area Structure [ASGS‐RA]: major cities, inner regional, outer regional, remote, very remote).19
Our dataset was near complete for most variables: fewer than 0.1% missing data for outcome of pregnancy preceding the index pregnancy, age, parity, gravidity, postcode, and country of birth; 0.5% missing data for Indigenous status; and 1.4% missing data for marital status.
Statistical analysis
We summarise data for characteristics as descriptive statistics. We examined associations between socio‐demographic, maternal, and reproductive characteristics and a history of induced abortion in univariate binary and multiple logistic regression analyses; we report odds ratios (ORs) and adjusted ORs (aORs) with 95% confidence intervals (CIs). Adjustment factors were selected according to previous reports6,20 and in consultation with expert clinicians (authors of this report). We also explored changes in associations between year and induced abortion, with 2010 as the reference point, in univariate and multiple logistic regression analyses; prevalence was age‐adjusted to the 2010 population of women of childbearing age in Victoria. We deemed 95% CIs that did not include 1 (one) statistically significant. All analyses were conducted in SPSS Statistics 29 (IBM).
Ethics approval
The study was approved by the La Trobe University Human Research Ethics Committee (HEC21124). The Consultative Council on Obstetric and Paediatric Mortality and Morbidity (Victoria) approved the analysis of VPDC data.
Results
A total of 766 488 births were recorded in Victoria during 2010–2019; we excluded 567 records in which data regarding induced abortions were missing (fewer than 0.1%). The proportion of women born in Australia varied by remoteness class (major cities, 55.9%; inner regional, 79.4%; outer regional/remote/very remote, 89.4%). The proportion of women under 30 years of age was smaller in major cities (32.8%; inner regional, 46.9%; outer regional/remote/very remote, 52.0%), as were the proportions living in areas in the two lowest socio‐economic status quintiles (25.8%; inner regional, 35.8%; outer regional/remote/very remote, 65.0%) or without partners at the time of the index birth (9.8%; inner regional, 15.8%; outer regional/remote/very remote, 18.9%) (Box 1).
History of induced abortion
Of the 766 488 women who gave birth in Victoria during 2010–2019, 93 251 (12.2%) reported induced abortions (93 250 of the 514 288 women who reported previous pregnancies, 18.1%). Of the 338 547 nulliparous women (ie, the index birth was their first), 36 938 (10.9%) reported induced abortions: 73 976 (79.3%) had had one, 15 016 (16.1%) two, 3261(3.5%) three, and 998 (1.1%) four or more abortions.
Of the 513 455 women who reported previous pregnancies (ie, primigravida excluded) and for whom the outcome of the most recent pregnancy prior to the index birth was known, the preceding pregnancy ended in induced abortion for 45 014 (8.8%) (Supporting Information, figure 1).
Among the 86 011 nulliparous women who reported previous pregnancies, the most recent pregnancy prior to the index birth had ended in induced abortion for 31 413 women (36.5%). Among women who had previously given birth (live or stillbirth) after pregnancies of least 20 weeks’ gestation, the most recent pregnancy prior to the index birth had ended in induced abortion for 3.2% (parity 1: 8606 of 271 064; parity 2: 3270 of 102 481; parity 3 or higher: 1719 of 53 843 women; Supporting Information, figure 2).
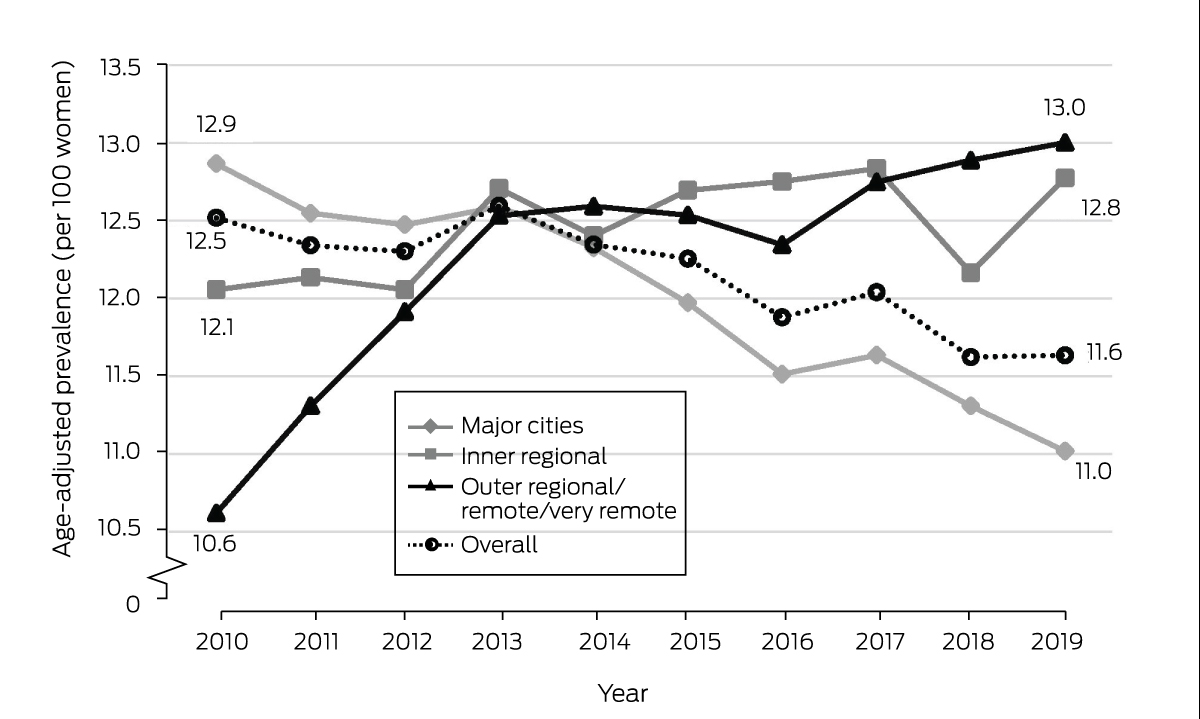
Changes in prevalence of history of induced abortion by geographic remoteness
During 2010–2019, the age‐adjusted prevalence of a history of induced abortion steadily declined among women living in major cities at the time of the index birth, from 12.9 to 11.0 per 100 women; the decline was most marked during 2013–2019. Among women in inner regional areas, it rose from 12.1 to 12.8 per 100 women; in outer regional/remote/very remote areas, the prevalence increased from 10.6 to 13.0 per 100 women, primarily during 2010–2013 (Box 2).
Socio‐demographic characteristics and history of induced abortion
Women living in inner regional (aOR, 0.94; 95% CI, 0.93–0.96) or outer regional/remote/very remote areas (aOR, 0.86; 95% CI, 0.83–0.89) were less likely than those living in major cities to report induced abortions prior to index births during 2010–2019. The adjusted odds of having had an induced abortion were 7–12% higher among women who did not live in areas in the highest socio‐economic status quintile than for those who did. The odds were higher for women born in Oceania (aOR, 1.26; 95% CI, 1.21–1.31) or North‐East Asia (aOR, 1.04; 95% CI, 1.01–1.07) than for those born in Australia, and lower for all other regions, most markedly for women born in North Africa or the Middle East (aOR, 0.42; 95% CI, 0.40–0.44) or in South‐East Asia (aOR, 0.57; 95% CI, 0.54–0.59). The adjusted odds of induced abortion increased steadily with age at the index birth and with parity. Women without partners at the time of the index birth were twice as likely as those with partners to have had abortions (aOR, 2.20; 95% CI, 2.16–2.25); the odds were also higher for Aboriginal and Torres Strait Islander than non‐Indigenous women (aOR, 1.32; 95% CI, 1.25–1.40) (Box 3).
Overall, the adjusted odds of having had an induced abortion declined across the study period (2019 v 2010: 0.93; 95% CI, 0.90–0.96). It declined among women in major cities (0.88; 95% CI, 0.84–0.91), but rose (albeit not statistically significantly) in inner regional (1.05; 95% CI, 0.99–1.12) and outer regional/remote/very remote areas (1.10; 95% CI, 0.96–1.27) (Box 4).
Discussion
We report the first Australian study to examine factors associated with a history of induced abortion in a complete population of childbearing women over ten years. We found that the likelihood of a history of induced abortion was significantly influenced by several socio‐demographic factors, and that temporal changes in the prevalence of a history of induced abortion differed by residential remoteness.
The overall decline in the proportion women giving birth who reported prior induced abortions over the 10‐year period primarily reflected its decline in major cities, where 67% of the women lived. We found that the adjusted odds of having had an abortion declined among women living in major cities who gave birth in Victoria during 2010–2019, but they rose in regional and remote areas (but not statistically significantly). PBS‐subsidised medical abortion became available in 2013,9 and telehealth consultations for abortion were available in some areas from 2015.21 The changes we report may indicate improved access to abortion services in non‐metropolitan areas, an interpretation consistent with higher medical abortion prescription rates in outer regional and remote Australia than in major cities.8 An important factor that we could not take into account in our analyses is the higher rate of unintended pregnancy in rural areas.22
The overall decline in the prior induced abortion rate we report may be linked with the increased uptake of highly effective long‐acting reversible contraception,23,24 resulting in fewer unintended pregnancies and abortions. Differences in the use of contraception in general and of more effective methods in particular have been reported in Australia, including lower rates among women born in non‐English speaking countries.23 Lower rates have also been reported for Aboriginal and Torres Strait Islander women,23 but only limited data are available.4,23 Improving equity of access to effective contraception is important for reducing the number of unintended pregnancies, including those leading to closely spaced births. Other factors that need to be taken into account include intimate partner violence, sexual coercion, and drug and alcohol use.20,25
Our finding that a history of abortion was less prevalent among childbearing women born in most regions outside Australia should be interpreted with caution. It could indicate poor access to abortion care in their countries of origin or for overseas‐born women in Australia. However, our finding could also be an artefact, as reporting of abortion in some ethnic groups is influenced by the religious or legal status of abortion in their countries of origin, by discomfort about or fear of reporting a stigmatised health behaviour, and by lower English proficiency and the need to use interpreters.
Limitations
Including all women who gave birth in Victoria during the study period eliminated the risk of selection bias. However, the presumably sizable group of women who have had one or more abortions but never given birth were not included in our analysis. The generalisability of our findings is consequently limited to women who have given birth. The socio‐demographic characteristics of the women were current at the time of the index birth, but may not have applied at the time of earlier abortions. Further, we could not assess the effects of other factors linked with induced abortion in Australia, including education and employment, use of less effective contraception, intimate partner violence, risky drinking, use of illicit drugs,25 financial security, and religious beliefs. Women who gave birth more than once during the study period were included multiple times in our study population, but each birth was treated as an exclusive observation (index birth). Finally, we do not know how many women who had had abortions did not report them.
Conclusion
Our findings indicate that access to abortion care in Victoria has improved, but the complex interplay between contraceptive use, unintended pregnancy, and induced abortion requires further exploration by remoteness of residence. Robust information about numbers of unintended pregnancies and access to reproductive health services are needed to guide national sexual and reproductive health policy and practice.
Box 1 – Socio‐demographic and pregnancy history characteristics of the women who gave birth in Victoria, 2010–2019
|
|
Geographic remoteness* |
||||||||||||||
|
Characteristic |
All locations |
Major cities |
Inner regional |
Outer regional/ remote/very remote |
|||||||||||
|
|
|||||||||||||||
|
Number of women |
766 488 |
512 669 [66.9%] |
208 473 [27.2%] |
44 916 [5.9%] |
|||||||||||
|
Age group (years) |
|
|
|
|
|||||||||||
|
Under 20 |
13 792 (1.8%) |
5946 (1.2%) |
5982 (2.9%) |
1856 (4.1%) |
|||||||||||
|
20–24 |
76 457 (10.0%) |
39 933 (7.8%) |
28 908 (13.9%) |
7561 (16.8%) |
|||||||||||
|
25–29 |
198 802 (25.9%) |
121 970 (23.8%) |
62 736 (30.1%) |
13 975 (31.1%) |
|||||||||||
|
30–34 |
280 312 (36.6%) |
196 944 (38.4%) |
69 609 (33.4%) |
13 602 (30.3%) |
|||||||||||
|
35–39 |
159 743 (20.8%) |
119 530 (23.3%) |
33 766 (16.2%) |
6377 (14.2%) |
|||||||||||
|
40 or older |
37 107 (4.8%) |
28 147 (5.5%) |
7419 (3.6%) |
1530 (3.4%) |
|||||||||||
|
Marital status |
|
|
|
|
|||||||||||
|
In a couple relationship |
665 493 (88.1%) |
458 156 (90.2%) |
171 833 (84.2%) |
35 144 (81.1%) |
|||||||||||
|
Not in a couple relationship |
89 976 (11.9%) |
49 615 (9.8%) |
32 139 (15.8%) |
8 175 (18.9%) |
|||||||||||
|
Region of birth |
|
|
|
|
|||||||||||
|
Australia |
489 665 (64.3%) |
284 894 (55.9%) |
164 713 (79.4%) |
39 962 (89.4%) |
|||||||||||
|
Oceania and Antarctica |
21 569 (2.8%) |
15 281 (3.0%) |
5344 (2.6%) |
918 (2.1%) |
|||||||||||
|
North‐West Europe |
22 357 (2.9%) |
17 133 (3.4%) |
4394 (2.1%) |
713 (1.6%) |
|||||||||||
|
Southern and Eastern Europe |
14 235 (1.9%) |
12 122 (2.4%) |
1958 (0.9%) |
142 (0.3%) |
|||||||||||
|
Americas |
10 428 (1.4%) |
8 447 (1.7%) |
1748 (0.8%) |
218 (0.5%) |
|||||||||||
|
Sub‐Saharan Africa |
13 407 (1.8%) |
10 482 (2.1%) |
2 648 (1.3%) |
266 (0.6%) |
|||||||||||
|
North Africa and the Middle East |
28 848 (3.8%) |
25 299 (5.0%) |
3324 (1.6%) |
216 (0.5%) |
|||||||||||
|
South‐East Asia |
33 147 (4.4%) |
26 867 (5.3%) |
5369 (2.6%) |
886 (2.0%) |
|||||||||||
|
North‐East Asia |
51 696 (6.8%) |
47 201 (9.3%) |
4021 (1.9%) |
443 (1.0%) |
|||||||||||
|
Southern and Central Asia |
76 633 (10.1%) |
61 819 (12.1%) |
13 801 (6.7%) |
938 (2.1%) |
|||||||||||
|
Indigenous status |
|
|
|
|
|||||||||||
|
Non‐Indigenous |
751 981 (98.6%) |
505 718 (99.2%) |
203 196 (97.9%) |
42 654 (95.4%) |
|||||||||||
|
Aboriginal or Torres Strait Islander |
10 369 (1.4%) |
3925 (0.8%) |
4363 (2.1%) |
2074 (4.6%) |
|||||||||||
|
Socio‐economic status (IRSD quintile) |
|
|
|
|
|||||||||||
|
5 (least disadvantaged) |
186 093 (24.3%) |
162 733 (31.8%) |
22 208 (10.7%) |
1151 (2.6%) |
|||||||||||
|
4 |
176 001 (23.0%) |
121 025 (23.6%) |
49 199 (23.6%) |
5777 (12.9%) |
|||||||||||
|
3 |
167 231 (21.8%) |
96 112 (18.8%) |
62 327 (29.9%) |
8 792 (19.6%) |
|||||||||||
|
2 |
124 080 (16.2%) |
61 370 (12.0%) |
46 481 (22.3%) |
16 229 (36.1%) |
|||||||||||
|
1 (most disadvantaged) |
112 037 (14.6%) |
70 928 (13.8%) |
28 145 (13.5%) |
12 964 (28.9%) |
|||||||||||
|
Parity |
|
|
|
|
|||||||||||
|
0 |
338 547 (44.2%) |
238 626 (46.5%) |
82 839 (39.7%) |
16 829 (37.5%) |
|||||||||||
|
1 |
271 370 (35.4%) |
182 017 (35.5%) |
74 105 (35.5%) |
15 129 (33.7%) |
|||||||||||
|
2 |
102 624 (13.4%) |
61 915 (12.1%) |
32 804 (15.7%) |
7872 (17.5%) |
|||||||||||
|
3 or more |
53 855 (7.0%) |
30 067 (5.9%) |
18 709 (9.0%) |
5084 (11.3%) |
|||||||||||
|
Gravidity |
|
|
|
|
|||||||||||
|
1 |
252 200 (32.9%) |
177 222 (34.6%) |
61 942 (29.7%) |
12 833 (28.6%) |
|||||||||||
|
2 |
238 468 (31.1%) |
162 584 (31.7%) |
62 812 (30.1%) |
12 950 (28.8%) |
|||||||||||
|
3 |
138 609 (18.1%) |
89 981 (17.6%) |
39 869 (19.1%) |
8701 (19.4%) |
|||||||||||
|
4 or more |
137 177 (17.9%) |
82 866 (16.2%) |
43 837 (21.0%) |
10 427 (23.2%) |
|||||||||||
|
Third or more birth at age 20–24 years |
|
|
|
|
|||||||||||
|
Yes |
7764 (10.2%) |
3417 (8.6%) |
3322 (11.5%) |
1020 (13.5%) |
|||||||||||
|
Induced abortions |
|
|
|
|
|||||||||||
|
None |
673 237 (87.8%) |
450 468 (87.9%) |
182 768 (87.7%) |
39 603 (88.2%) |
|||||||||||
|
One |
73 976 (9.7%) |
49 113 (9.6%) |
20 525 (9.8%) |
4307 (9.6%) |
|||||||||||
|
Two or more |
19 275 (2.5%) |
13 088 (2.6%) |
5180 (2.5%) |
1006 (2.2%) |
|||||||||||
|
Previous pregnancy ended in abortion† |
|
|
|
|
|||||||||||
|
Yes |
45 014/513 455 (8.8%) |
31 335/334 884 (9.4%) |
11 370/146 321 (7.8%) |
2289/32 023 (7.1%) |
|||||||||||
|
|
|||||||||||||||
|
IRSD = Index of Relative Socio‐economic Disadvantage. * The slight discrepancy between number for all locations and the sum of the numbers by category is caused by missing values for postcode (430 women, 0.06% of data). † Primigravida excluded. |
|||||||||||||||
Box 2 – Annual age‐adjusted prevalence of a history of induced abortion at index birth among 766 488 women who gave birth in Victoria, 2010–2019, by residential remoteness
Box 3 – Associations between socio‐demographic characteristics and history of induced abortion among 766 488 women who gave birth in Victoria, 2010–2019
|
Characteristic |
Induced abortion |
Odds ratio (95% CI) |
Adjusted odds ratio* (95% CI) |
||||||||||||
|
|
|||||||||||||||
|
Age group (years) |
|
|
|
||||||||||||
|
Under 20 |
973/13 792 (7.1%) |
0.59 (0.55–0.63) |
0.33 (0.31–0.36) |
||||||||||||
|
20–24 |
9026/76 457 (11.8%) |
1.04 (1.02–1.07) |
0.80 (0.78–0.82) |
||||||||||||
|
25–29 |
23 296/198 802 (11.7%) |
1.03 (1.01–1.05) |
0.97 (0.96–0.99) |
||||||||||||
|
30–34 |
31 956/280 312 (11.4%) |
1 |
1 |
||||||||||||
|
35–39 |
21 793/159 743 (13.6%) |
1.23 (1.21–1.25) |
1.23 (1.20–1.25) |
||||||||||||
|
40 or older |
6185/37 107 (16.7%) |
1.56 (1.51–1.60) |
1.51 (1.46–1.55) |
||||||||||||
|
Parity |
|
|
|
||||||||||||
|
0 |
36 938/338 547 (10.9%) |
1 |
1 |
||||||||||||
|
1 |
33 505/271 370 (12.3%) |
1.15 (1.13–1.17) |
1.15 (1.13–1.17) |
||||||||||||
|
2 |
14 154/102 624 (13.8%) |
1.31 (1.28–1.33) |
1.26 (1.24–1.29) |
||||||||||||
|
3 or more |
8637/53 885 (16.0%) |
1.56 (1.52–1.60) |
1.44 (1.40–1.48) |
||||||||||||
|
Marital status |
|
|
|
||||||||||||
|
In a couple relationship |
73 876/665 493 (11.1%) |
1 |
1 |
||||||||||||
|
Not in a couple relationship |
18 073/89 976 (20.1%) |
2.01 (1.98–2.05) |
2.20 (2.16–2.25) |
||||||||||||
|
Indigenous status |
|
|
|
||||||||||||
|
Non‐Indigenous |
90 872/751 981 (12.1%) |
1 |
1 |
||||||||||||
|
Aboriginal or Torres Strait Islander |
1815/10 369 (17.5%) |
1.54 (1.47–1.63) |
1.32 (1.25–1.40) |
||||||||||||
|
Socio‐economic status (IRSD quintile) |
|
|
|
||||||||||||
|
5 (least disadvantaged) |
21 978/186 093 (11.8%) |
1 |
1 |
||||||||||||
|
4 |
21 548/176 001 (12.2%) |
1.04 (1.02–1.06) |
1.07 (1.05–1.09) |
||||||||||||
|
3 |
20 964/167 231 (12.5%) |
1.07 (1.05–1.09) |
1.12 (1.10–1.14) |
||||||||||||
|
2 |
15 104/124 080 (12.2%) |
1.04 (1.01–1.06) |
1.09 (1.07–1.12) |
||||||||||||
|
1 (most disadvantaged) |
13 552/112 037 (12.1%) |
1.03 (1.00–1.05) |
1.08 (1.05–1.11) |
||||||||||||
|
Geographic remoteness |
|
|
|
||||||||||||
|
Major cities |
62 201/512 669 (12.1%) |
1 |
1 |
||||||||||||
|
Inner regional |
25 705/208 473 (12.3%) |
1.02 (1.003–1.03) |
0.94 (0.93–0.96) |
||||||||||||
|
Outer regional/remote/very remote |
5313/44 916 (11.8%) |
0.97 (0.94–1.001) |
0.86 (0.83–0.89) |
||||||||||||
|
Region of birth |
|
|
|
||||||||||||
|
Australia |
64 190/489 665 (13.1%) |
1 |
1 |
||||||||||||
|
Oceania and Antarctica |
3510/21 569 (16.3%) |
1.29 (1.24–1.34) |
1.26 (1.21–1.31) |
||||||||||||
|
North‐West Europe |
2807/22 357 (12.6%) |
0.95 (0.91–0.99) |
0.97 (0.93–1.01) |
||||||||||||
|
Southern and Eastern Europe |
1573/14 235 (11.1%) |
0.82 (0.78–0.87) |
0.84 (0.79–0.89) |
||||||||||||
|
Americas |
1097/10 428 (10.5%) |
0.78 (0.73–0.83) |
0.79 (0.74–0.84) |
||||||||||||
|
Sub‐Saharan Africa |
1408/13 407 (10.5%) |
0.78 (0.74–0.82) |
0.75 (0.71–0.80) |
||||||||||||
|
North Africa and the Middle East |
1694/28 848 (5.9%) |
0.41 (0.39–0.44) |
0.42 (0.40–0.44) |
||||||||||||
|
South‐East Asia |
2553/33 147 (7.7%) |
0.55 (0.53–0.58) |
0.57 (0.54–0.59) |
||||||||||||
|
North‐East Asia |
6808/51 696 (13.2%) |
1.01 (0.98–1.03) |
1.04 (1.01–1.07) |
||||||||||||
|
Southern and Central Asia |
7219/76 633 (9.4%) |
0.69 (0.67–0.71) |
0.78 (0.75–0.80) |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; IRSD = Index of Relative Socio‐economic Disadvantage. * Adjusted for age, marital status, Indigenous status, residential socio‐economic status and remoteness, region of birth, and year of index birth. |
|||||||||||||||
Box 4 – History of induced abortion, by geographic location at time of index birth and year (reference year: 2010): multiple logistic regression analyses*
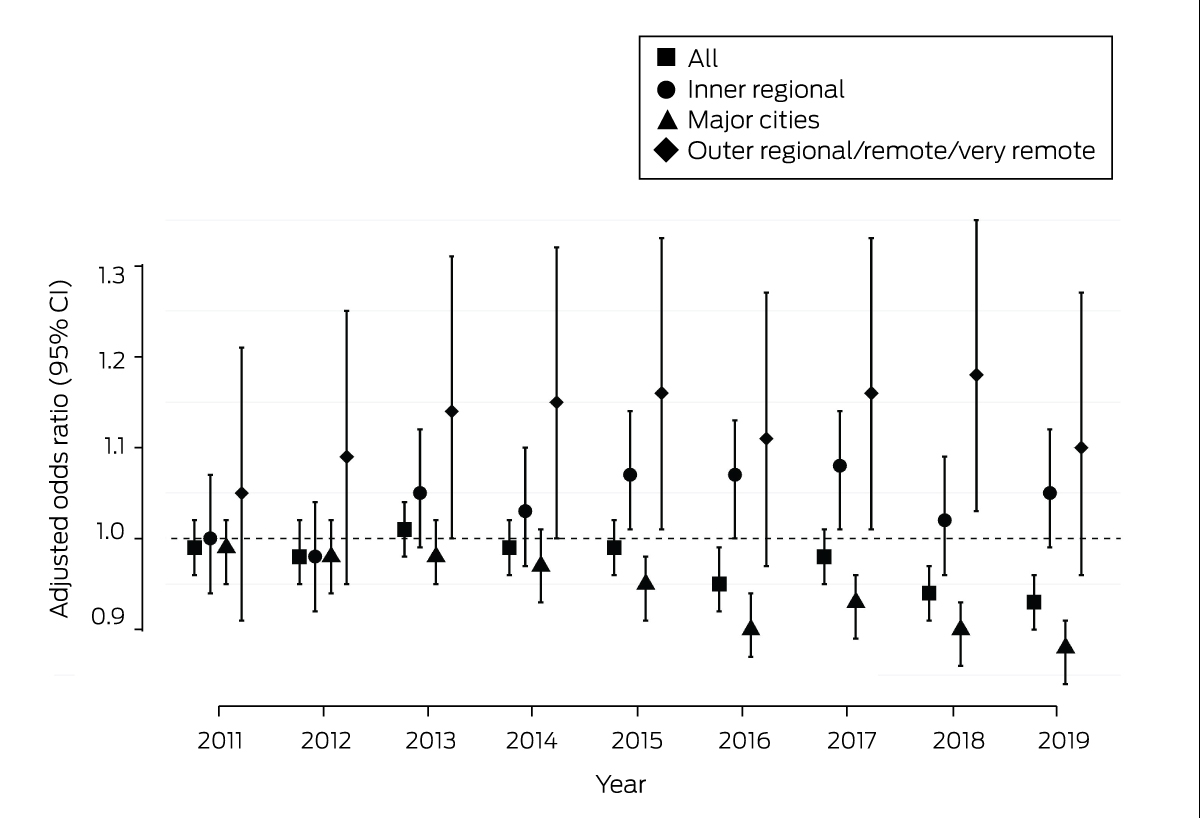
CI = confidence interval.* Adjusted for age, marital status, Indigenous status, residential socio‐economic status and remoteness, region of birth, and year of index birth. The outcomes of the univariate binary and multiple logistic regression analyses are included in the Supporting Information, table 1.
Received 21 April 2023, accepted 8 October 2023
- Kristina Edvardsson1
- Kirsten I Black2
- Deborah Bateson2
- Wendy V Norman3,4
- Mridula Shankar5
- Leesa Hooker1,6
- Xia Li7
- Angela J Taft1
- 1 Judith Lumley Centre, School of Nursing and Midwifery, La Trobe University, Melbourne, VIC
- 2 The University of Sydney, Sydney, NSW
- 3 The University of British Columbia, Vancouver, Canada
- 4 London School of Hygiene and Tropical Medicine, London, United Kingdom
- 5 Nossal Institute for Global Health, University of Melbourne, Melbourne, VIC
- 6 La Trobe Rural Health School, La Trobe University, Bendigo, VIC
- 7 La Trobe University, Melbourne, VIC
Open access:
Open access publishing facilitated by La Trobe University, as part of the Wiley – La Trobe University agreement via the Council of Australian University Librarians.
Wendy Norman is supported as an Applied Public Health Research Chair (2014–24) by the Canadian Institutes of Health Research (CPP‐329455–07837). We acknowledge members of the SPHERE Centre of Research Excellence in Sexual and Reproductive Health for Women in Primary Care (SPHERE CRE) for their contributions to this investigation, which was funded by the National Health and Medical Research Council (APP1153592). The funding sources had no role in study design, data collection, analysis or interpretation, reporting or publication.
We are grateful to the Consultative Council on Obstetric and Paediatric Mortality and Morbidity (CCOPMM) for providing access to the data analysed for this study, and for the assistance of the staff at the Consultative Councils Unit, Safer Care Victoria. The views expressed in this article do not necessarily reflect those of CCOPMM.
No relevant disclosures.
- 1. United Nations Population Fund. Seeing the unseen: the case for action in the neglected crisis of unintended pregnancy (State of World Population 2022). New York: UNFPA, 2022. https://esaro.unfpa.org/sites/default/files/pub‐pdf/en_swp22_report_0_0.pdf (viewed Sept 2023).
- 2. Taft AJ, Shankar M, Black KI, et al. Unintended and unwanted pregnancy in Australia: a cross‐sectional, national random telephone survey of prevalence and outcomes. Med J Aust 2018; 209: 407‐408. https://www.mja.com.au/journal/2018/209/9/unintended‐and‐unwanted‐pregnancy‐australia‐cross‐sectional‐national‐random
- 3. Bearak J, Popinchalk A, Ganatra B, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health 2020; 8: e1152‐e1161.
- 4. Health Technology Analysts. The impact of unintended pregnancy in Australia. Report prepared for Organon. June 2022. https://www.organon.com/australia/wp‐content/uploads/sites/16/2022/09/ORG01_Report_FINAL_28June2022.pdf (viewed Sept 2023).
- 5. Keogh LA, Gurrin LC, Moore P. Estimating the abortion rate in Australia from National Hospital Morbidity and Pharmaceutical Benefits Scheme data. Med J Aust 2021; 215: 375‐376. https://www.mja.com.au/journal/2021/215/8/estimating‐abortion‐rate‐australia‐national‐hospital‐morbidity‐and
- 6. Wright S, Bateson D, McGeechan K. Induced abortion in Australia: 2000–2020. Sydney: Family Planning NSW, 2021. https://www.fpnsw.org.au/sites/default/files/assets/Induced‐Abortion‐in‐Australia_2000‐2020.pdf (viewed Sept 2023).
- 7. Australian Department of Health. National Women's Health Strategy 2020–2030. Canberra: Department of Health, 2018. https://www.health.gov.au/sites/default/files/documents/2021/05/national‐women‐s‐health‐strategy‐2020‐2030_0.pdf (viewed Sept 2023).
- 8. Community Affairs References Committee. Ending the postcode lottery: addressing barriers to sexual, maternity and reproductive healthcare in Australia. May 2023. https://parlinfo.aph.gov.au/parlInfo/download/committees/reportsen/RB000075/toc_pdf/EndingthepostcodelotteryAddressingbarrierstosexual,maternityandreproductivehealthcareinAustralia.pdf (viewed June 2023).
- 9. Subasinghe AK, McGeechan K, Moulton JE, et al. Early medical abortion services provided in Australian primary care. Med J Aust 2021; 215: 366‐370. https://www.mja.com.au/journal/2021/215/8/early‐medical‐abortion‐services‐provided‐australian‐primary‐care
- 10. Mazza D, Burton G, Wilson S, et al. Medical abortion. Aust J Gen Pract 2020; 49: 324‐330.
- 11. de Costa C, Douglas H, Hamblin J, et al. Abortion law across Australia: a review of nine jurisdictions. Aust N Z J Obstet Gynaecol 2015; 55: 105‐111.
- 12. Victorian Department of Health and Human Services. Victorian Perinatal Data Collection (VPDC) manual, version 7.0. Section 3: data definitions. Jan 2019. https://www.health.vic.gov.au/sites/default/files/migrated/files/collections/policies‐and‐guidelines/v/vpdc‐manual‐2019‐section‐3‐‐‐data‐definitions‐vpdc‐manual.pdf (viewed Sept 2023).
- 13. Flood MM, McDonald SJ, Pollock WE, Davey MA. Data accuracy in the Victorian Perinatal Data Collection: results of a validation study of 2011 data. Health Inf Manag 2017; 46: 113‐126.
- 14. Victorian Department of Health. Victorian Perinatal Data Collection. Updated 2 Oct 2023. https://www.health.vic.gov.au/quality‐safety‐service/victorian‐perinatal‐data‐collection (viewed Oct 2023).
- 15. Benchimol EI, Smeeth L, Guttmann A, et al; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely‐collected health Data (RECORD) statement. PLoS Med 2015; 12: e1001885.
- 16. Australian Bureau of Statistics. Births, Australia. Statistics about births and fertility rates for Australia, states and territories, and sub‐state regions. Reference period 2020. 8 Dec 2021. https://www.abs.gov.au/statistics/people/population/births‐australia/2020 (viewed Dec 2023).
- 17. Australian Bureau of Statistics. Standard Australian Classification of Countries (SACC). 27 June 2016. https://www.abs.gov.au/statistics/classifications/standard‐australian‐classification‐countries‐sacc/latest‐release (viewed Aug 2023).
- 18. Australian Bureau of Statistics. How to Interpret SEIFA score distributions. In: An introduction to Socio‐Economic Indexes for Areas (SEIFA), 2006 (2039.0). 26 Mar 2008. https://www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/2039.0Main%20Features62006?opendocument&tabname=Summary&prodno=2039.0&issue=2006&num=&view= (viewed Aug 2023).
- 19. Australian Department of Health and Aged Care. Australian Statistical Geography Standard – Remoteness Area. Updated 14 Dec 2021. https://www.health.gov.au/topics/rural‐health‐workforce/classifications/asgs‐ra (viewed Aug 2023).
- 20. Shankar M, Hooker L, Edvardsson K, et al. The prevalence and variations in unintended pregnancy by socio‐demographic and health‐related factors in a population‐based cohort of young Australian women. Aust N Z J Public Health 2023; 47: 100046.
- 21. Seymour JW, Melville C, Thompson TA, Grossman D. Effectiveness and safety of a direct‐to‐patient telehealth service providing medication abortion targeted at rural and remote populations: cross‐sectional findings from Marie Stopes Australia. Contraception 2022; 115: 67‐68.
- 22. Rowe H, Holton S, Kirkman M, et al. Prevalence and distribution of unintended pregnancy: the Understanding Fertility Management in Australia National Survey. Aust N Z J Public Health 2016; 40: 104‐109.
- 23. Family Planning NSW. Contraception in Australia 2005–2018. Sydney: FPNSW, 2020. https://www.fpnsw.org.au/sites/default/files/assets/Contraception‐in‐Australia_2005‐2018_v20200716.pdf (viewed Sept 2023).
- 24. Grzeskowiak LE, Calabretto H, Amos N, et al. Changes in use of hormonal long‐acting reversible contraceptive methods in Australia between 2006 and 2018: a population‐based study. Aust N Z J Obstet Gynaecol 2021; 61: 128‐134.
- 25. Taft AJ, Powell RL, Watson LF, et al. Factors associated with induced abortion over time: secondary data analysis of five waves of the Australian Longitudinal Study on Women's Health. Aust N Z J Public Health 2019; 43: 137‐142.






Abstract
Objective: To assess the prevalence of a history of induced abortion among women who gave birth in Victoria during 2010–2019; to assess the association of socio‐demographic factors with a history of induced abortion.
Study design: Retrospective cohort study; analysis of cross‐sectional perinatal data in the Victorian Perinatal Data Collection (VPDC).
Setting, participants: All women who gave birth (live or stillborn) in Victoria, 1 January 2010 – 31 December 2019.
Main outcome measures: Self‐reported induced abortions prior to the index birth; outcome of the most recent pregnancy preceding the index pregnancy.
Results: Of the 766 488 women who gave birth during 2010–2019, 93 251 reported induced abortions (12.2%), including 36 938 of 338 547 nulliparous women (10.9%). Women living in inner regional (adjusted odds ratio [aOR], 0.94; 95% confidence interval [CI], 0.93–0.96) or outer regional/remote/very remote areas (aOR, 0.86; 95% CI, 0.83–0.89) were less likely than women in major cities to report induced abortions. The likelihood increased steadily with age at the index birth and with parity, and was also higher for women without partners at the index birth (aOR, 2.20; 95% CI, 2.16–2.25) and Aboriginal and Torres Strait Islander women (aOR, 1.32; 95% CI, 1.25–1.40). The likelihood was lower for women born in most areas outside Australia than for those born in Australia. The likelihood of a history of induced abortion declined across the study period overall (2019v 2010: 0.93; 95% CI, 0.90–0.96) and for women in major cities (0.88; 95% CI, 0.84–0.91); rises in inner regional and outer regional/remote/very remote areas were not statistically significant.
Conclusions: Access to abortion care in Victoria improved during 2010–2019, but the complex interplay between contraceptive use, unintended pregnancy, and induced abortion requires further exploration by remoteness of residence. Robust information about numbers of unintended pregnancies and access to reproductive health services are needed to guide national sexual and reproductive health policy and practice.