Dietary requirements for all nutrients are higher for women during pregnancy and lactation than when not pregnant or breastfeeding. During pregnancy, there is an increase of about 50% in maternal thyroxine production, a high rate of transfer of iodine and thyroxine from mother to fetus and increased maternal renal iodine clearance.1 Increased iodine requirements during breastfeeding allow for secretion of iodine in breastmilk. In Australia, the recommended iodine intake increases from 150 μg/day for non-pregnant adult women to 220 μg/day during pregnancy and 270 μg/day while breastfeeding2 (Box 1). The National Iodine Nutrition Survey conducted in 2003 and 2004 found that children living in south-eastern Australia were mildly iodine deficient.5 The results of several small contemporaneous studies of urinary iodine concentration in pregnant women were consistent with iodine insufficiency in pregnant women in the same states6-11 (Box 2).
Since October 2009, it has been mandatory to replace salt used in breadmaking with iodised salt, except in bread represented as organic.19 Food Standards Australia New Zealand (FSANZ) estimated that, in the general population of women aged 19–44 years, this strategy would increase mean iodine intake by 46 μg/day and reduce the proportion of women with inadequate intakes from 59% to 9%.19 Mean iodine intakes in pregnant and breastfeeding women were not calculated separately because there are too few of them in the dataset to allow separate estimation. Assuming that food consumption during pregnancy or lactation is the same as for the general population, FSANZ estimated that most of these women would still have inadequate intakes19 owing to their higher iodine requirements (Box 1).2
These concerns led to the National Health and Medical Research Council convening an expert group to consider if, and what level of, iodine supplementation should be recommended to pregnant and breastfeeding Australian women.20 As there is no nationally representative survey of iodine status in pregnant and breastfeeding women, the gap between the postfortification intake and the desirable intake was calculated using two different approaches and presented to the expert group. We describe these calculations and include more recent studies to update the information.
Except in breastfeeding women, urinary iodine excretion (μg/day) accurately reflects recent iodine intake, with about 90% of dietary iodine appearing in the urine.1 The median urinary iodine concentration (MUIC) in a population, calculated from a single sample in each participant, is well accepted as a surrogate marker for population iodine intake because variations in hydration, although influential for individual iodine concentration measurements, generally even out when calculating the population median. The formula daily iodine intake (μg) = urinary iodine concentration (μg/L) × 0.0235 × bodyweight (kg) is used for adults to estimate iodine intake from the iodine concentration in a spot urine sample.1 For example, an MUIC of 100 μg/L corresponds to an intake of 160 μg/day for a bodyweight of 68 kg. Conversely, an average population intake of 250 μg/day would give an MUIC of about 156 μg/L. This formula cannot be used to estimate iodine intake in breastfeeding women because it does not include the iodine content of breastmilk.
In addition to studies reporting MUIC data in pregnant Australian women6-11 described in earlier reviews,7,19,20 we identified four more recent studies13-16 and three reports on breastfeeding women (Box 2).13,12,17 One study (McElduff et al8) was excluded owing to the overlap of women with those of another study (Gunton et al6). Most studies took opportunistic samples from hospital clinics and did not describe whether women were using iodine supplements.
Pregnant women were recruited at stages of gestation ranging from early pregnancy to full term. Owing to lack of information about women’s weight in the studies, we applied a weight of 68 kg to all studies of pregnant women to back-calculate iodine intake from the MUIC. This allows for some of the weight gain during pregnancy compared with the reference bodyweight of 61 kg used to derive nutrient reference values for non-pregnant Australian women (Box 1).2 For simplicity, we used a target dietary intake of 250 μg (midway between the recommended daily intakes [RDIs] for pregnant and breastfeeding women) to calculate the gap in iodine intake in each study. The gap between calculated intake and the RDI of iodine for pregnant women (220 μg) or breastfeeding women (270 μg) can be determined by subtracting 30 μg from, or adding 20 μg to, respectively, the values shown in Box 2.
We performed dietary calculations using the datafile of iodine intake estimates (excluding supplements and corrected for within-person variation) generated by FSANZ during their work on iodine fortification.19 The prefortification estimate was calculated by applying the iodine content of Australian food analysed between 2001 and 2005 to the reported food consumption in the NNS. The amount of iodine in bread after mandatory replacement of salt with iodised salt (using an average of 45 mg iodine/kg salt), allowing for 10% loss of iodine with baking, was calculated for each woman based on her reported bread consumption.19
Box 3 shows the prefortification and postfortification cumulative distribution of iodine intakes for the 2960 women aged 19–44 years in the NNS estimated by FSANZ, and allows the proportion of the population with intakes greater than and less than any iodine level to be read. For example, before fortification, about 60% of women had estimated iodine intakes below 100 μg/day (therefore, about 40% had an intake greater than 100 μg/day). Box 3 shows the progressive shift in the postfortification distribution of iodine intakes in Australian women with increasing increments of 50 μg/day of iodine.
Because the data shown in the first five plots in Box 3 are not specifically for pregnant or breastfeeding women, the food-frequency data of key iodine-containing foods from a cohort study22 were also considered.
Before fortification of bread with iodine, the estimated gap between iodine intake and the target ranged from 84–172 μg/day (Box 2). Two studies were repeated after fortification. In Tasmania, after the implementation of a program that resulted in an estimated 80% of bread being made with iodised salt,18 the average gap was 113–121 μg/day compared with an average gap of 129 μg/day before the program was implemented.10 In Gippsland, there was no difference before and after the enforcement date for national mandatory fortification.16 The three small studies in breastfeeding women12,13,17 had MUICs at the lower end of the MUIC range for pregnant women.
We used the proportion with intakes less than the estimated average requirement (EAR; Box 1) to estimate the proportion of the population with inadequate iodine intakes.21 Supplementation with 100 μg of iodine per day would result in the proportion of women with intakes below the EAR for pregnant women (160 μg/day) being essentially zero, and fewer than 10% of women having intakes below the EAR for lactating women (190 μg/day). Both of these values would be zero with supplementation with 150 μg of iodine per day. Median iodine intakes would be 240 μg/day with supplementation of 100 μg/day and 290 μg/day with supplementation of 150 μg/day (Box 3). The highest iodine intake resulting from bread fortification plus supplementation with 150 μg of iodine per day would be about 580 μg/day (Box 3), which is well below the upper level of intake of 1100 μg/day for adults in Australia and New Zealand2 (Box 1).
Food-frequency data of key iodine-containing foods from a cohort study show that the intake of bread and dairy products is higher in pregnant and postpartum women, and this might increase iodine intake by about 20 μg/day compared with that of non-pregnant women.22 We added this to the 150 μg/day supplementation level in Box 3 (sixth plot) as an approximation for iodine intakes in pregnant and lactating women.
There are no urinary iodine concentration studies of pregnant or breastfeeding women in Western Australia and Queensland where the MUIC is between 100 and 150 μg/L in children.5 Studies such as those from Tasmania10,23 indicate that the MUIC in children provides an estimate of the MUIC in adults. MUIC in the range of 100–149 μg/L, while sufficient in children, indicates insufficiency in pregnant women.4 It is therefore possible that pregnant women in Western Australia and Queensland have insufficient iodine intake.
The urinary concentration data provide the basis for an estimation of the average iodine intake target for the population only. The dietary estimate allows the population iodine intake distribution to be compared with criteria for both adequacy and excessive intakes. Although advice about iodine supplementation is directed at individuals, the amount of iodine in the supplement does not need to equal the RDI. The purpose of this type of recommendation is to improve population nutrient status so that only a low proportion of the population would have inadequate intakes.24 As shown in Box 3, the median iodine intake of the population is higher than the RDI and a small proportion will have intakes below the EAR with supplementation of 100–150 μg per day.
There are few data about the dietary intakes of pregnant and breastfeeding women in Australia. Food frequency data in the 2003 Australian Longitudinal Study on Women’s Health showed similar consumption of key iodine-containing foods for both pregnant women and women after giving birth and these were slightly higher than consumption by non-pregnant women in the same cohort.22 Therefore, we believe that, in the absence of better data, the information from urinary concentration studies of pregnant women can be reasonably extrapolated to breastfeeding women to estimate their iodine intakes, and that the dietary data from the general adult female population do not substantially underestimate iodine intake in the groups of interest. Data on iodine intakes, urinary concentrations and supplement use are being collected in the 2011–2013 Australian Health Survey.25 The new data will show whether population iodine intake has changed substantially since 1995. This will allow some of the strategies aimed at improving iodine intake in the population to be assessed. Pregnant and breastfeeding women are not being oversampled which limits evaluation in these groups. A minimal effect on MUIC among pregnant women was reported after fortification.10,16 MUIC excludes additional iodine transferred to the fetus which may partly explain these results. The Tasmanian iodine fortification program achieved a smaller proportion of fortified bread than national regulation.10 The result from Gippsland16 is difficult to interpret without knowing when the samples were obtained and when bread fortification actually started during the year-long transition before the enforcement date in October 2009. Further information about current iodine status of pregnant and lactating women would be desirable.
Our calculations do not yield a single “correct” answer, but show the range of the gap in iodine intake. In addition to these numerical results (Box 2), other factors affect the supplement dose that should be recommended. A committee or organisation needs to consider what weighting should be given to each of the various non-representative studies, extrapolation of results in pregnant women to breastfeeding women and what prevalence of inadequate intake would be tolerable in the population. Other factors include whether a single recommendation to cover both groups could be made, whether the dose should be inflated to allow for missed days in supplement consumption, safety over the period of intended use for those with the highest dietary intakes, and whether it is possible to recommend a dosage that is currently available in the marketplace. A further consideration is how to factor in the uncertainty in the reference values (eg, the Food and Agriculture Organization/World Health Organization has the same recommendation for both groups [Box 1]) and the consequences of making or not making a recommendation.
1 Iodine intake recommendations for adult women
National Health and Medical Research Council and New Zealand Ministry of Health2 |
|||
Food and Agriculture Organization/World Health Organization3,4 |
|||
2 Estimated iodine intakes calculated from median urinary iodine concentrations reported in studies of pregnant or breastfeeding women and level of daily iodine supplementation needed to achieve an average intake of 250 µg/day
Supplementation required to raise median intake to 250 µg/day |
|||||||||||||||
3 Projected iodine intake of Australian women aged 19–44 years under different fortification and iodine supplement scenarios
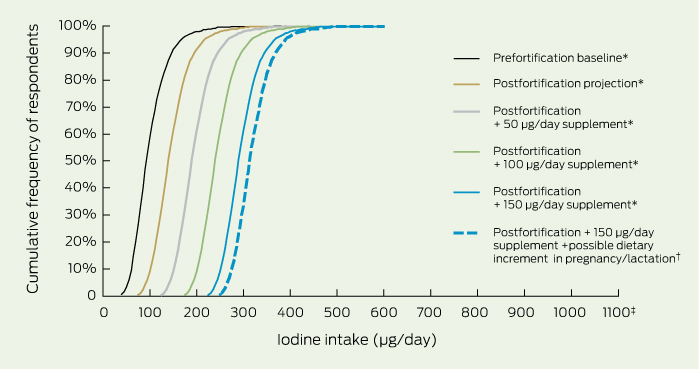
The upper level of intake recommended for adult Australian women is 1100 µg/day.2
* Food consumption data from the 1995 National Nutrition Survey with Food Standards Australia New Zealand analytical iodine concentrations and estimated postfortification iodine concentration in bread.19 † Food-frequency data of key iodine-containing foods from a cohort study22 added to the 150 µg/day level of iodine supplementation.
Received 3 February 2012, accepted 12 June 2012
- Dorothy E M Mackerras1
- Creswell J Eastman2
- 1 Office of the Chief Scientist, Food Standards Australia New Zealand, Canberra, ACT.
- 2 International Council for the Control of Iodine Deficiency Disorders, University of Sydney, Sydney, NSW.
We acknowledge permission from Food Standards Australia New Zealand to use the iodine intake datafile. Julie Boorman did the dietary modelling for the prefortification and postfortification iodine estimates that formed the basis for the current analysis.
The work for this study was done while we were both members of the National Health and Medical Research Council Expert Panel on Iodine Supplementation for Pregnant and Lactating women.
- 1. Zimmermann MB. Iodine deficiency. Endocr Rev 2009; 30: 376-408.
- 2. National Health and Medical Research Council and New Zealand Ministry of Health. Nutrient reference values for Australia and New Zealand Introduction. Canberra: NHMRC, 2006. http://www.nrv.gov.au/introduction.htm (accessed Feb 2011).
- 3. Food and Agriculture Organization of the United Nations, World Health Organization. Human vitamin and mineral requirements. Report of a Joint FAO/WHO Expert Consultation. Rome: FAO/WHO, 2002. http://www.fao.org/DOCREP/004/Y2809E/y2809e00.htm (accessed Mar 2011).
- 4. WHO Secretariat, Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr 2007; 10: 1606-1611.
- 5. Li M, Eastman CJ, Waite KV, et al. Are Australian children iodine deficient? Results of the Australian National Iodine Nutrition Study. Med J Aust 2006; 184: 165-169. <MJA full text>
- 6. Gunton JE, Hams G, Fiegert M, McElduff A. Iodine deficiency in ambulatory participants at a Sydney teaching hospital: is Australia truly iodine replete? Med J Aust 1999; 171: 467-470. <MJA full text>
- 7. Li M, Ma G, Boyages SC, Eastman CJ. Re-emergence of iodine deficiency in Australia. Asia Pac J Clin Nutr 2001; 10: 200-203.
- 8. McElduff A, McElduff P, Gunton JE, et al. Neonatal thyroid-stimulating hormone concentrations in northern Sydney: further indications of mild iodine deficiency? Med J Aust 2002; 176: 317-320.
- 9. Hamrosi MA, Wallace EM, Riley MD. Iodine status in pregnant women living in Melbourne differs by ethnic group. Asia Pac J Clin Nutr 2005; 14: 27-31.
- 10. Burgess JR, Seal JA, Stilwell GM, et al. A case for universal salt iodisation to correct iodine deficiency in pregnancy: another salutary lesson from Tasmania. Med J Aust 2007; 186: 574-576. <MJA full text>
- 11. Travers CA, Guttikonda K, Norton CA, et al. Iodine status in pregnant women and their newborns: are our babies at risk of iodine deficiency? Med J Aust 2006; 184: 617-620. <MJA full text>
- 12. Chan SS, Hams G, Wiley V, et al. Postpartum maternal iodine status and the relationship to neonatal thyroid function. Thyroid 2003; 13: 873-876.
- 13. Mackerras DE, Singh GR, Eastman CJ. Iodine status of Aboriginal teenagers in the Darwin region before mandatory iodine fortification of bread. Med J Aust 2011; 194: 126-130. <MJA full text>
- 14. Charlton KE, Gemming L, Yeatman H, Ma G. Suboptimal iodine status of Australian pregnant women reflects poor knowledge and practices related to iodine nutrition. Nutrition 2010; 26: 963-968.
- 15. Nguyen B, Baker D, Southcott E, et al. Iodine deficiency in pregnant women in the ACT. ANZ J Obstet Gynaecol 2010; 50: 539-542. doi: 10.1111/j.1479-828X.2010.01239.x.
- 16. Rahman A, Savige GS, Deacon NJ, et al. Urinary iodine deficiency in Gippsland pregnant women: the failure of bread fortification? Med J Aust 2011; 194: 240-243. <MJA full text>
- 17. Axford S, Charlton K, Yeatman H, Ma G. Improved iodine status in breastfeeding women following mandatory fortification. Aust N Z J Public Health 2011; 35: 579-580.
- 18. Seal J. The makings of the Tasmanian (interim) iodine supplementation program 2001–2004. In: Richards PAC, Stewart JC, editors. Goitre monitor: the history of iodine deficiency disorders in Tasmania. South Launceston, Tas: Myola House of Publishing, 2007: 208.
- 19. Food Standards Australia New Zealand. Proposal P1003. Mandatory iodine fortification for Australia. Approval report. Canberra: FSANZ, 2008. http://www.foodstandards.gov.au/_srcfiles/AppR_P1003_Mandatory_Iodine_Fortification_Aust%20AppR.pdf (accessed Feb 2011).
- 20. National Health and Medical Research Council. Iodine supplementation for pregnant and breastfeeding women. NHMRC public statement. Canberra: NHMRC, 2010. http://www.nhmrc.gov.au/_files_nhmrc/file/publications/synopses/new45_statement.pdf (accessed Feb 2011).
- 21. National Research Council. Dietary reference intakes: applications in dietary planning. Washington, DC: The National Academies Press, 2003. http://www.nap.edu/catalog.php?record_id=10609 (accessed Jun 2012).
- 22. Mackerras D, Powers J, Boorman J, et al. Estimating the impact of mandatory fortification of bread with iodine on pregnant and post-partum women. J Epidemiol Community Health 2011; 65: 1118-1122.
- 23. Seal JA, Doyle Z, Burgess JR, et al. Iodine status of Tasmanians following voluntary fortification of bread with iodine. Med J Aust 2007; 186: 69-71. <MJA full text>
- 24. Cockell KA, Miller DC, Lowell H. Application of the Dietary Reference Intakes in developing a recommendation for pregnancy iron supplements in Canada. Am J Clin Nutr 2009; 90: 1023-1028.
- 25. Australian Bureau of Statistics. Australian health survey. http://www.abs.gov.au/websitedbs/D3310114.nsf/Home/Australian+Health+Survey? OpenDocument (accessed Jan 2012).





Abstract
Objective: To identify a level of iodine supplementation to recommend for pregnant and breastfeeding women in Australia.
Design, setting and participants: Dietary modelling indicated that mandatory fortification of bread with iodine by replacing salt with iodised salt would still leave a gap in iodine intakes in pregnant and breastfeeding women in Australia. Iodine shortfall was estimated by two separate methods: (i) analysis of data from published studies reporting mean urinary iodine concentrations in populations of Australian women who were pregnant or had given birth in the past 6 months; and (ii) modelling based on the postmandatory fortification iodine intake estimates calculated by Food Standards Australia New Zealand using food consumption reported by women aged 19–44 years who participated in the 1995 National Nutrition Survey.
Main outcome measure: Estimated level of daily supplementation required to provide sufficient iodine to result in a low proportion of pregnant and breastfeeding women having inadequate iodine intakes.
Results: Estimations from both data sources indicate that a supplement of 100–150 μg/day would increase iodine intakes to a suitable extent in pregnant and breastfeeding women in Australia.
Conclusions: The final level of supplementation we recommend should be based on these calculations and other factors. There will be population subgroups for whom our general recommendation is not appropriate.