Induced abortion is essential health care and access to safe, affordable, high quality abortion care is a human right.1 In Australia, abortion legal reforms since 2000 have moved abortion from criminal to health law,2 closely aligned with human rights standards and best clinical practice.3 Subsidisation of mifepristone by the Pharmaceutical Benefits Scheme in 20134 established early medical abortion (at up to 63 days’ gestation) as a viable option in primary care.5 Increasing numbers of prescriptions of the combined mifepristone–misoprostol regimen (MS‐2 Step) indicate that use of this option is growing.6 Medical abortion rates are almost twice as high in regional and remote areas as in major cities,7 suggesting its value for overcoming access barriers related to geographic location.
The extension of abortion services from specialist clinics to primary care is vital for early medical abortion.8 Compared with aspiration techniques, the relative ease of medication administration has spurred telehealth models,9,10 recently supported by Medicare rebates.11 But medical abortion is not widely offered in primary care7 and geographic and financial differences in timely access persist.12,13,14 These problems are linked with structural impediments, including regulations regarding the gestational threshold for medical abortion, inadequate public funding, and the absence of a coordinated health systems approach to supporting universal access.14,15,16
Centring the provision of abortion within primary care and supportive regulatory and policy environments are crucial to achieving universal access, according to the World Health Organization (WHO).17 In Australia, some regulatory barriers that stymied expansion of medical abortion in primary care have been removed; for instance, in August 2023 the Therapeutic Goods Administration (TGA) removed the requirement that all general practitioners and pharmacists who prescribe or dispense MS‐2 Step complete mandatory online training.18 Prior to August 2023, only 7% of general practitioners and 22% of pharmacists were active MS‐2 Step providers,8,19,20 and most were in major cities.7 Other problems include general practitioners’ fears of procedural complications, the stigmatisation of abortion, and insufficient remuneration for prescribing MS‐2 Step.21 The introduction of nurse‐ and midwife‐led models of medical abortion has been slow, despite recommendations by the WHO.17 The legality of prescribing by nurse practitioners and midwifes is subject to individual state and territory legislation.22
All Australian jurisdictions have decriminalised abortion.3 The aim of our review is to synthesise primary research findings about factors that affect medical abortion provision by general practitioners, nurses, midwives, and pharmacists in Australia.
Methods
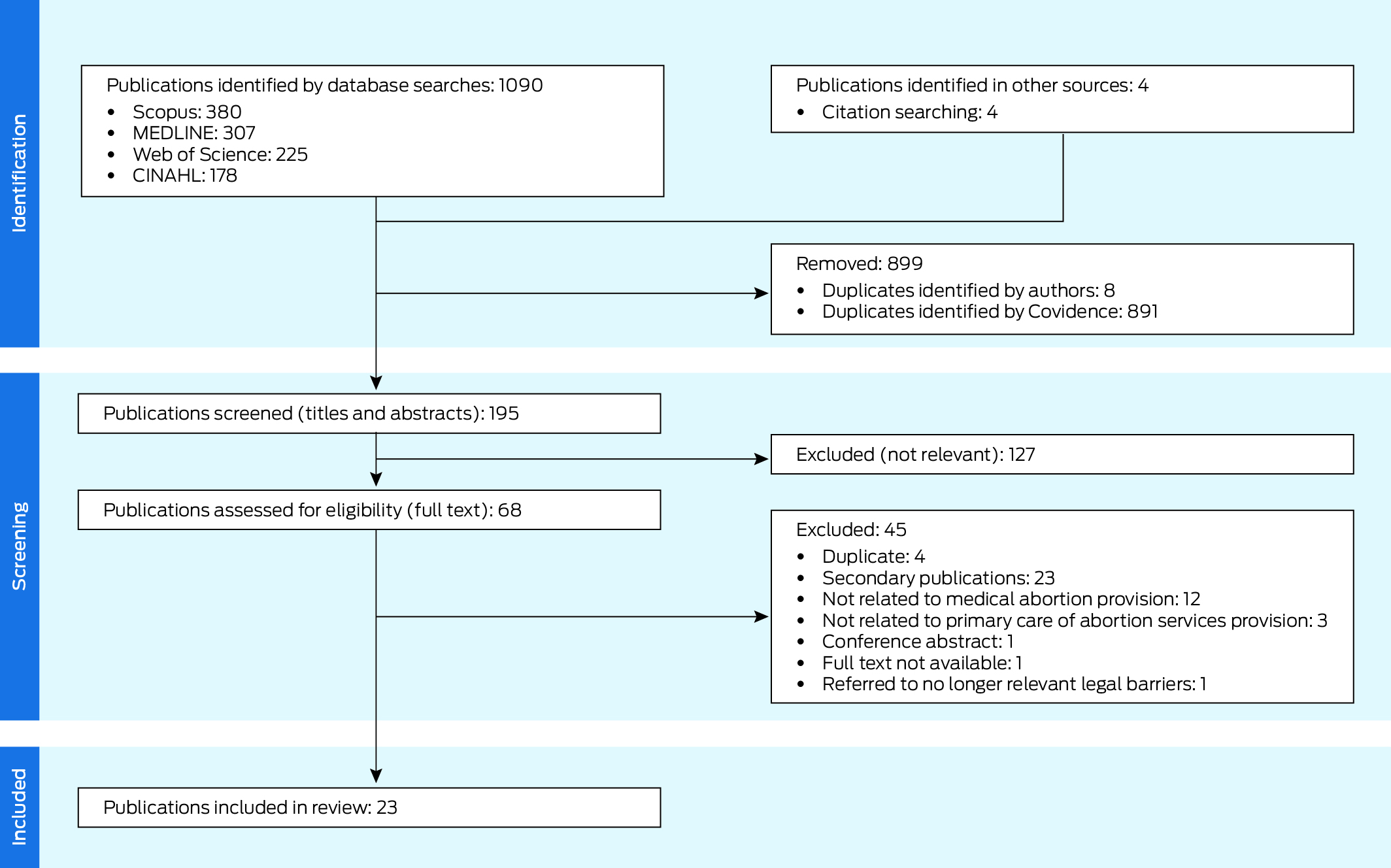
We report our systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA)23 guidelines and the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ)24 statement. The protocol was registered with the Open Science Foundation (1 July 2024; https://osf.io/9zqg2).
Study inclusion criteria
We included primary peer‐reviewed publications on qualitative, quantitative, and mixed methods research on medical abortion provision in Australian primary care published during 1 January 2013 – 18 January 2025; MS‐2 Step was registered by the TGA in August 2012.4 We defined provision broadly to include abortion experts, general practitioners, nurses, midwives, and pharmacists. We did not include secondary sources, such as editorials, letters, and commentaries (Box 1).
Search methods
We searched the MEDLINE, Scopus, Web of Science, and CINAHL (Cumulative Index to Nursing and Allied Health Literature) databases for relevant publications. In consultation with a librarian, we developed the primary search strategy in MEDLINE and adapted it for the other databases. The search terms were related to “abortion”, “primary care provision”, and “Australia” (Supporting Information, part 1).
Study selection
We screened records using Covidence (www.covidence.org). Authors GS and MS screened the titles and abstracts of all articles, then their full text. We resolved discrepancies in screening decisions by discussion. We searched reference lists of included publications to identify further publications, which then underwent the same screening process.
Data extraction
Using a standardised form, author GS extracted data from each publication, including geographic location (state or territory), study aims, methodological design, participant characteristics (gender, profession, remoteness category, provision status), sample sizes, and study findings (author‐generated themes and explanations, participant quotes, descriptive findings and relationships between independent and dependent variables). Author MS verified the extracted data.
Assessment of methodological limitations
Authors GS and MS independently appraised all studies and reached a final rating through discussion. We critically appraised the included studies with the Mixed Methods Appraisal Tool (MMAT).25 We critically appraised studies that used the Delphi methodology26 using the Guidance on Conducting and Reporting Delphi Studies (CREDES) tool.27 We did not use quality assessments to exclude studies, but these assessments contributed to assessing confidence in the review findings.
Data analysis and synthesis
We used thematic synthesis to develop findings from the qualitative data.28 Authors GS and MS independently developed line‐by‐line codes for six data‐rich records using NVivo 14. We refined codes to ensure consistency in meaning. GS coded the remaining studies, developing new codes when necessary. We then grouped and summarised codes of similar meanings into broader descriptive categories and discussed their impact on abortion provision to identify barriers and facilitators. Reviewers located these barriers and facilitators in the health care system structure and contextualised them further by gender and rurality. During discussions, we inferred higher order meanings to develop three overarching analytical themes and ten qualitative review findings.
We assessed confidence in each review finding using the GRADE–CERQual approach (https://www.cerqual.org),29 which evaluates the confidence of evidence from reviews of qualitative research according to four components: methodological limitations,30 how closely the review findings reflect the raw data (coherence),31 how applicable the raw data are to the review question (relevance),32 and the richness of data supporting the review finding (adequacy).33 We assessed the overall confidence (high, moderate, low, very low) in each review finding on component ratings of supporting evidence.
We mapped the quantitative evidence to our qualitative review findings to determine whether the quantitative data supported, extended (ie, added new detail) or contradicted the findings from our qualitative evidence synthesis.
An author reflexivity statement is included in the Supporting Information, part 2.
Results
A total of 1094 articles were identified in our database and reference list searches; after excluding 899 duplicates and 127 articles deemed not relevant after screening their titles and abstracts, the full text of 68 publications was screened. After excluding a further 45 items, 23 publications were included in our review (Box 2, Box 3; Supporting Information, part 3).34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56
Description of studies
The included publications reported used qualitative (fourteen),34,35,36,37,38,42,43,46,48,50,51,52,54,55 quantitative (four),39,45,47,49 and mixed methods studies (three);41,53,56 one study used the Delphi technique.40,44 Ten studies were conducted in Victoria, eight across Australia, three in New South Wales, and one each in Queensland and Tasmania. Fourteen studies provided data on medical abortion provision in rural areas.37,38,39,40,41,43,44,45,47,48,49,50,52,54 Eleven studies reported the perspectives of general practitioners or primary care nurses,28‐32,35,38‐40,44,47,37,39,41,43,45‐51 three studies those of pharmacists,34,52,56 and ten studies reported the views of abortion professionals, including rural abortion training providers38 and multidisciplinary abortion experts.35,36,40,42,44,52,53,54,55 Seventeen studies reported the views of medical abortion providers.34,35,36,37,39,40,42,43,44,47,49,50,51,52,53,54,56
Methodological limitations
The most frequent methodological limitations of the qualitative studies were related to analytical rigor (partially adequate or unclear in four studies), ethical considerations (partially remediated in six studies) and researcher reflexivity (not discussed in eight studies). For the quantitative studies, the major limitations were sample representativeness (in three of four studies, the samples were only partially representative of the population) and risk of non‐response bias (high or unclear in four studies). The limitations of the mixed methods studies pertained to integrating qualitative and quantitative components. The Delphi study had limitations with regard to defining consensus, participant recruitment, and coherence in design (Box 4; Supporting Information, part 4).
Themes and findings from the qualitative and quantitative study findings synthesis
The qualitative (Supporting Information, part 5) and quantitative study findings (Supporting Information, part 6) synthesis yielded three overarching themes and ten review findings (Box 4; Box 5):
- moral, legal, and regulatory influences on abortion care (three review findings);
- the absence of a systems‐based approach to abortion provision (six review findings); and
- early medical abortion belongs in primary care (one review finding).
We rated the confidence level for six of our review findings as high, for three as moderate, and for one as very low (Supporting Information, part 5).
Moral, legal, and regulatory influences on abortion care
Finding 1: Conscientious objection causes barriers to abortion care at the individual, service, and system levels (moderate confidence). Moral or religious beliefs are an individual barrier to providing abortion care for some doctors and pharmacists; colleagues who conscientiously object to abortion care greatly limit its provision and clinical training. In such cases, the service (including the dispensing of MS‐2 Step) is not offered, care is delayed, or providers must offer care clandestinely. Health services use conscientious objection legal clauses to justify institutional bans on abortion provision and education.34,36,37,41,42,43,44,46,48,50,54,56
In Victoria, section 8 of the Abortion Law Reform Act 2008 (the legal clause permitting conscientious objection) is perceived by some general practitioners as a mechanism for facilitating abortion access via referral.43 However, abortion providers are concerned that section 8 legitimises refusing to provide care without adequate justification, and that it is routinely misused by pharmacists and general practitioners who do not fulfil professional obligations and legal requirements to facilitate continuity of care by referring women seeking abortion.36,37,42,43
Quantitative studies found that some primary care clinicians conscientiously object to abortion,39,41,45,47 but personal opposition to abortion is not always a barrier to providing it.47 Conscientious objection seems to be more frequent among general practitioners trained overseas,41 and increases with time since qualification for registered nurses and midwives.47 Conscientious objection by colleagues, practice‐wide bans on abortion, and pharmacist refusal to dispense MS‐2 Step limit the provision of abortion provision by general practitioners and primary care nurses.39,40
Finding 2: Decriminalisation is crucial but insufficient for expanding abortion care (very low confidence). In Victoria, decriminalisation of abortion was viewed by providers as important for indicating that abortion care is health care. It was also understood by some as a legal mechanism for reducing unequal decisional dynamics for abortion seekers and providers of abortion care. However, in the absence of government support for service provision, including by establishing a sustainable health workforce, decriminalisation alone was considered insufficient for expanding services.36
This finding was supported by the findings of a quantitative study in Queensland which suggest that decriminalisation of abortion did not significantly alter support for the public provision of abortion care among sexual health nurses and midwives.47
Finding 3: Establishing an autonomous nurse‐led model of medical abortion requires regulatory reform and overcoming health system barriers (moderate confidence). Regulations prohibiting nurse practitioners prescribing MS‐2 Step, Medicare billing requirements for general practitioner involvement, and scarce training opportunities are systemic barriers that limit the autonomous provision of medical abortion by primary care nurses. At the service level, practice nurse involvement in medical abortion depends on their employers’ interest and approval, as well as clear protocols for task sharing. Conscientious objection by colleagues in regional and rural organisations can limit nurse involvement, although some organisations have adopted alternative approaches, including task sharing with telehealth providers. Primary care nurses have communication skills suited for abortion care, and their involvement eases the general practitioner workload. However, some may not have the physical or psychological capacity to independently provide abortions and manage complications without appropriate training, provide after‐hours support, or achieve wider medical community endorsement.35,44,48,52,53,54,55,56
Conflicting views among abortion experts about whether primary care nurses can manage abortion care and complications independently is a barrier to developing nurse‐led models. While abortion providers generally endorse the involvement of practice nurses, they see their role as being supportive rather than independent.35,44,52,55
Quantitative findings also suggest that differing views on the nursing and midwifery scope of practice, concerns about managing complications, limited abortion training opportunities, and the emotional demands of abortion work are all barriers to nurse involvement in medical abortion care.39,47,53 Abortion experts agree that nurse‐led models are needed to expand access to abortion, but have conflicting views about the required degree of general practitioner involvement.40,53 The financial and logistical feasibility of nurse‐led models requires extensive government and primary health care network support, as well as endorsement by peak nursing bodies.40
The absence of a systems‐based approach to abortion provision
Finding 4: Primary and ancillary providers of medical abortion are not well connected (high confidence). Comprehensive support by a network of ancillary services (general practitioners, pharmacists, sonographers, psychologists, referral hospitals) is essential for providing high quality abortion care. Establishing such a network, including guaranteeing the support of local hospitals for emergency and after‐hours care, is logistically difficult for general practitioners, as some services obstruct or refuse to support medical abortion provision.35,37,38,41,43,44,48,50,52,54,55,56
In the absence of systemwide support, local and virtual peer support networks and phone helplines enhance clinician knowledge, confidence, and resources, and reduce feelings of isolation.35,38,43,50,52,54,56 Such networks are especially useful for decentralised abortion services in rural areas.38,54 The MS‐2 Step 24‐hour nurse hotline was perceived to be helpful for after‐hours support and more accessible than assistance from local hospitals.43,52 In Victoria, 1800 My Options, a service for information on sexual and reproductive health care, is a vital resource for providers.52
Quantitative studies found that inadequate access to ancillary services (pathology and ultrasound), abortion medications, and tertiary support for complications are barriers to providing medical abortion.39,40,45 Primary care nurses are particularly concerned about access to surgical support.39 Service delivery models that encompass ancillary providers and provide clear referral pathways are regarded as the most important factor in service expansion.40,49
Finding 5: Preparedness and value ascribed to training, qualifications, and clinical experience (high confidence). Insufficient knowledge, training, and abortion care experience are barriers to in‐person and telehealth abortion provision for primary care clinicians. Many providers pursue external training or qualifications to compensate the limited opportunities provided by their workplaces, medical curricula, or clinical placements. Access to supervision and hands‐on learning improves general practitioners’ skills and confidence, as exposure to medical abortion in primary care is often sporadic. Some experienced providers feel that medical abortion should be provided in specialist clinics where skills and experiences in women's health are stronger and demand for the service is consistently higher.34,35,37,48,50,51,52,54,55,56
Quantitative studies also found that lack of knowledge,39,40,45,49,56 training opportunities39,45 and guidelines49 reduce clinician preparedness. Prior experience in providing abortion care is valued more by general practitioners than by primary care nurses.49 Primary care providers would like to receive abortion training,45,47 including as part of the core curriculum.47
Finding 6: The absence of a visible service system and a culture of secrecy obscure levels of abortion demand (moderate confidence). The absence of a visible primary care service system for abortion, particularly in rural areas, means referrers rely on “rumours” to identify providers offering abortion care. The stigmatisation of abortion and privacy concerns cause practitioners to operate by stealth, leading to conflicting perceptions of demand: some fear being overwhelmed, others regard demand as low. Abortion experts worry that without state or federal government support for abortion care, service expansion and workforce development will not increase.34,36,37,41,43,46,54
Quantitative studies found that the awareness of clinicians in rural areas of local abortion services is poor and believe that demand is limited by privacy concerns.41 A small minority believe that the available abortion services are adequate.39,41 Increasing public awareness of the availability of medical abortion in primary care could increase the demand for local abortion care, which could increase its provision.40
Finding 7: Inadequate resources and geographic isolation are barriers to rural abortion care (high confidence). General practitioners in rural areas who offer abortion care feel isolated, anticipate stigmatisation, and experience pressure and emotional distress, especially when working in towns or areas with conscientious objectors. Funding models do not consider these problems, and some rural providers do not have adequate resources or financial compensation to meet community needs, leading to staff burnout, poor workforce retention, and reduced quality of care (eg, delayed appointments).35,37,38,41,42,44,48,50,54,55
Geographic decentralisation of rural medical abortion services relies on the formation of partnerships with locally embedded sexual health organisations or intermediaries who facilitate training, protocol, and service development.35,38 Leveraging of telehealth and general practitioner and nurse task‐sharing approaches have helped overcome obstacles associated with conscientious objections.54
Quantitative studies have found that rural providers of medical abortion do not have access to ultrasound, allied health, surgical, and after‐hours support. Expanding rural medical abortion services requires more resources and government support to provide incentives for training and professional development.40
Finding 8: Financial disincentives and the gendered nature of abortion care contribute to work overload, service fragmentation, and gender‐based pay disparities (high confidence). The fragmented structure of public health care financing and reliance on time‐based Medicare item numbers discourage practitioners from providing abortion care. In the absence of a publicly funded supportive framework for integrating abortion services into primary care, including using telehealth, individual providers must navigate several logistical hurdles at their own cost. Coupled with the gendered nature of abortion provision and female providers often working part‐time, delays and fragmentation in care contribute to work overload and risk of burn‐out at the individual level, and gender‐related pay disparities and organisational glass ceilings at the service level.36,37,38,43,44,46,48,51,52,54,55
Offering person‐centred abortion care requires time and empathic communication that is not financially compensated by the current funding system, leaving providers feeling undervalued.48 Time and financial pressures can affect service quality, and some providers feel compelled to prioritise clinical considerations over other aspects, such as cultural safety.48,51
Quantitative studies have found that financial barriers to medical abortion provision include the time required for abortion counselling, legal restrictions of autonomous nurse provision,49 and financial unviability of the service.49 Financial considerations were more frequently a significant barrier for male than female general practitioners.45
Finding 9: Anticipated and actual stigmatisation of abortion affect its provision (high confidence). Anticipating that medical abortion provision will detrimentally affect or otherwise reduce one's professional reputation and practice is an internal barrier for general practitioners, and rural providers fear negative feedback from their communities. Some providers experience moral disapproval by friends and colleagues and choose not to advertise their service for fear of anti‐abortion activists.36,37,43,46,54,55
Some practitioners who do not provide abortion care do not believe that stigmatisation affects cases in which the patient and provider do not have negative cultural or religious beliefs about abortion, and in workplaces where women's reproductive health is a priority.37
Quantitative studies have found that primary care clinicians, particularly nurses, are concerned about being known as abortion providers because they anticipate stigmatisation by colleagues, friends, and their community,39,40,49 and fear harassment by anti‐abortion activists.39,40
Early medical abortion belongs in primary care
Finding 10: Medical abortion in primary care enhances equity and patient autonomy (high confidence). General practitioner providers are motivated by the belief that abortion care is integral to women's health care and should be financially, geographically, and socially accessible. This sense is greater among clinicians who provide care to socially marginalised, disadvantaged, or rural women for whom access to services may not be straightforward. Medical abortion provision in primary care provides greater continuity of care (eg, for follow‐up and contraception) and facilitates the tailoring of care to the needs of the woman and the community, including with telehealth.35,37,38,43,48,50,51,52,54
The risk of inadequate follow‐up is worrying for practitioners who provide or do not provide abortion care and can lead to their no longer providing medical abortion.37,43 This concern appears greatest for general practitioners who provide a low cost services to women from outside their local area.37 Provider acceptance of telehealth has grown, but barriers to uptake include difficulties with building rapport, lack of control over patients’ physical surroundings, and the inability to undertake physical examinations.52
Quantitative studies have found that recognition of abortion care as health care and the need to increase access in marginalised communities are important factors for increasing its provision by general practitioners and primary care nurses,40,47,49 but fear of loss to follow‐up is a concern.49
Discussion
Our review synthesises the findings of studies of the barriers and facilitators of medical abortion provision in Australian primary care. At the systems level, key barriers include the absence of a clear service delivery strategy, insufficient Medicare remuneration, and limited training opportunities and ancillary support. Service level barriers include resource constraints, geographic isolation, and working with conscientious objectors to abortion. Individual barriers include insufficient abortion knowledge and experience, and personal beliefs regarding abortion. Access to clinician support networks and a commitment to enhancing reproductive health care facilitate its provision.
The strengths of our study include the fact that we optimised the use of data reported by studies with different study designs. Our application of GRADE‐CERQual to each finding enhances the usability of our findings in decision making. We also discussed factors affecting telehealth and nurse‐led models of abortion care.
Our findings suggest that the decision to provide abortion care is based on core personnel values, challenging the popular view that conscientiousness is linked only with opposition to abortion.58,59 The values that underpin this conscientiousness include viewing abortion as essential health care, supporting universal access to reproductive choice, and wanting to meet community health needs.58,59,60 Values clarification workshops that enhance providers’ self‐awareness and understanding of their professional duty in abortion care is a promising strategy for supporting the Australian primary care workforce.61,62 These workshops foster supportive attitudes and reduce active opposition among providers with diverse beliefs and in different contexts.62,63 The challenges posed by conscientious objection must prompt consideration of laws that protect the right to decline involvement in pregnancy termination, which allow practitioners to avoid their professional duty to provide essential reproductive health care,64 but providing insufficient protection for practitioners who do provide it.
We found that most medical abortion providers are women, and that there are financial disincentives for engaging in sexual and reproductive health work. Recent scrutiny of the Medicare Benefits Scheme (MBS)65 affirms the existence of gender‐related biases in federal funding structures; for example, the MBS rebates for women's health procedures are smaller than for men's health procedures. This discrepancy discourages clinicians from engaging in women's health care. Widespread uptake of medical abortion services in general practice is unlikely without redressing these imbalances, and we welcome the recent announcement of a gender‐based audit of the MBS system.11
A key obstacle to medical abortion provision is the limited opportunity to gain clinical experience. This barrier is linked with the dearth of formal abortion training in medical schools,66 exacerbated by bans on abortion care education in religious training institutions, an example of abortion exceptionalism: beliefs and practices that distinguish abortion from standard medical care because it is immoral, risky, or too specialised, resulting in its systematic exclusion from training curricula.67 Integrating abortion services into primary care through a whole of system approach could shift clinical perceptions of what constitutes standard health care.
Our findings reinforce the importance of establishing communities of practice, particularly for rural providers. It has recently been reported that the Australian Contraception and Abortion Primary Care Practitioner Support Network (AusCAPPS) is widely used by general practitioners, nurses, and pharmacists to increase knowledge about abortion and to clarify questions about service provision.68 A 2023 Senate enquiry has consequently recommended to continue federal funding of the network.14
Our review emphasises the suitability of primary care for providing medical abortion, but nurses and midwives could play greater roles. Recent legislative changes in Queensland,69 the Australian Capital Territory,70 and Western Australia71 permit nurse practitioners and endorsed midwives to prescribe MS‐2 Step. Increasing the involvement of nurses and midwives in medical abortion will also require nurse‐ and midwife‐specific abortion training, improved Medicare remuneration, and overcoming the perception that medical abortion is outside their scope of care. Expanding the evidence base for nurse and midwife‐led models of medical abortion in Australia, including by task sharing,72 could change this situation.
Limitations
Only three studies examined the role of pharmacists,34,52,56 limiting our conclusions about factors that affect the dispensing of MS‐2 Step. Some studies also examined surgical abortion or included information about non‐primary care providers. Most studies were undertaken in Victoria, particularly those that investigated conscientious objection, and there were no studies from Western Australia, South Australia, or the Northern Territory.
Conclusion
Regulatory, governance, funding, and service coordination barriers need to be overcome to improve early medical abortion delivery in Australian primary care. Such care is important for supporting the National Women's Health Strategy goal of equitable access to abortion care.73
Box 1 – Factors that affect the provision of medical abortion services in Australian primary care: inclusion and exclusion criteria for our systematic review
|
Criterion |
Inclusion |
Exclusion |
|||||||||||||
|
|
|||||||||||||||
|
Population |
|
|
|||||||||||||
|
Intervention |
|
|
|||||||||||||
|
Comparison |
|
|
|||||||||||||
|
Outcomes |
|
|
|||||||||||||
|
Study design |
|
|
|||||||||||||
|
Time period |
|
— |
|||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 2 – Factors affecting the provision of medical abortion services in Australian primary care: a systematic review
Box 3 – Characteristics of the 23 publications included in our systematic review of publications of studies examining the provision of medical abortion in Australian primary care
|
Characteristic |
Number |
||||||||||||||
|
|
|||||||||||||||
|
Study design |
|
||||||||||||||
|
Quantitative |
4 |
||||||||||||||
|
Qualitative |
14 |
||||||||||||||
|
Mixed methods |
3 |
||||||||||||||
|
Delphi method |
2 |
||||||||||||||
|
Location |
|
||||||||||||||
|
Victoria |
10 |
||||||||||||||
|
New South Wales |
3 |
||||||||||||||
|
Queensland |
1 |
||||||||||||||
|
Tasmania |
1 |
||||||||||||||
|
Australia‐wide |
8 |
||||||||||||||
|
Participant remoteness categories* |
|
||||||||||||||
|
Metropolitan areas |
14 |
||||||||||||||
|
Regional areas |
13 |
||||||||||||||
|
Rural areas |
14 |
||||||||||||||
|
Unknown |
5 |
||||||||||||||
|
Participants |
|
||||||||||||||
|
General practitioners only |
6 |
||||||||||||||
|
General practitioners and nurses only |
3 |
||||||||||||||
|
Nurses and midwives only |
2 |
||||||||||||||
|
Pharmacists only |
1 |
||||||||||||||
|
General practitioners, nurses, pharmacists only |
1 |
||||||||||||||
|
Other clinical and non‐clinical experts† |
10 |
||||||||||||||
|
Medical abortion provision status |
|
||||||||||||||
|
Providers only |
9 |
||||||||||||||
|
Providers and others |
8 |
||||||||||||||
|
Unknown |
6 |
||||||||||||||
|
|
|||||||||||||||
|
* Multiple categories for individual studies possible. † Includes sexual health physicians, service managers, abortion training providers. |
|||||||||||||||
Box 4 – Systematic review of the provision of medical abortion services in Australian primary care: summary of qualitative review themes and findings, and assessment of confidence in each review finding (GRADE–CERQual 29 )
|
Themes and findings |
Overall assessment |
Explanation of overall assessment |
|||||||||||||
|
|
|||||||||||||||
|
Theme 1. Moral, legal, and regulatory influences on abortion care |
|
|
|||||||||||||
|
1. Conscientious objection causes barriers to abortion care at the individual, service, and system levels34,36,37,41,42,43,44,46,48,50,54,56 |
Moderate confidence |
|
|||||||||||||
|
2. Decriminalisation is crucial but insufficient for expanding abortion care36 |
Very low confidence |
|
|||||||||||||
|
3. Establishing an autonomous nurse‐led model of medical abortion requires regulatory reform and overcoming health system barriers35,44,48,52,53,54,55,56 |
Moderate confidence |
|
|||||||||||||
|
Theme 2. The absence of a systems‐based approach to abortion provision |
|
|
|||||||||||||
|
4. Primary and ancillary providers of medical abortion are not well connected35,37,38,41,43,44,48,50,52,54,55,56 |
High confidence |
|
|||||||||||||
|
5. Preparedness and value ascribed to training, qualifications, and clinical experience34,35,37,48,50,51,52,54,55,56 |
High confidence |
|
|||||||||||||
|
6. The absence of a visible service system and a culture of secrecy obscure levels of abortion demand34,36,37,41,43,46,54 |
Moderate confidence |
|
|||||||||||||
|
7. Inadequate resources and geographic isolation are barriers to rural abortion care35,37,38,41,42,44,48,50,54,55 |
High confidence |
|
|||||||||||||
|
8. Financial disincentives and the gendered nature of abortion care contribute to work overload, service fragmentation, and gender‐based pay disparities36,37,38,43,44,46,48,51,52,54,55 |
High confidence |
|
|||||||||||||
|
9. Anticipated and actual stigmatisation of abortion affect its provision36,37,43,46,54,55 |
High confidence |
|
|||||||||||||
|
Theme 3. Early medical abortion belongs in primary care |
|
|
|||||||||||||
|
10. Medical abortion in primary care enhances equity and patient autonomy35,37,38,43,48,50,51,52,54 |
High confidence |
|
|||||||||||||
|
|
|||||||||||||||
|
* Adequacy assessment evaluates both the quantity and richness of data contributing to a review finding. Reviewers gauge data richness by appraising the depth of information, rating excerpts from very thin to very thick based on their explanatory detail. The overall adequacy judgment combines this assessment of data richness across all contributory studies with the total data quantity.33 |
|||||||||||||||
Box 5 – Map of review findings by article and publication year*
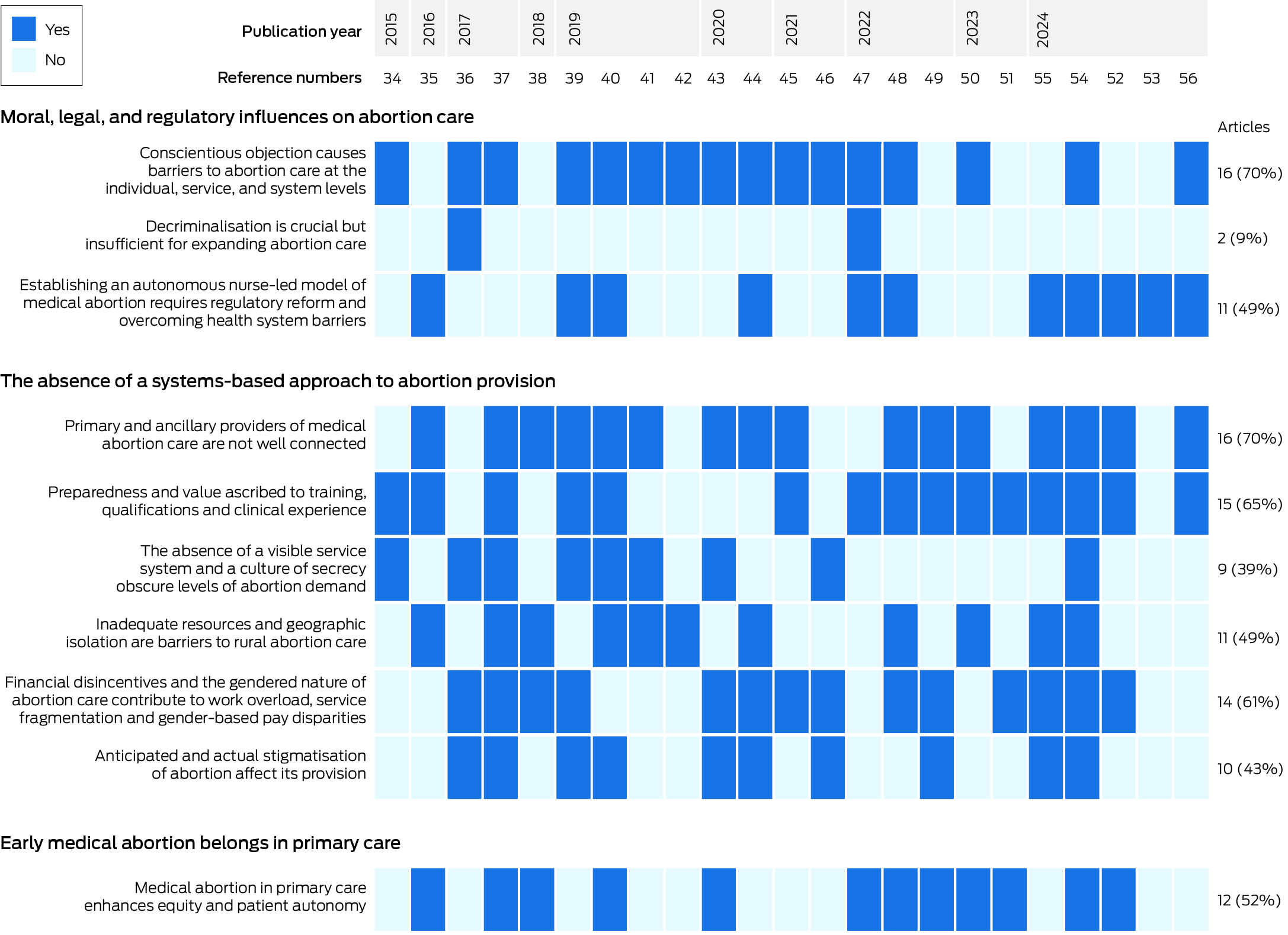
* Format adapted from figure 2 in reference 57.
Received 30 October 2024, accepted 24 February 2025
- Greta Skahill1
- Mridula Shankar2
- 1 The University of Melbourne, Melbourne, VIC
- 2 Nossal Institute for Global Health, the University of Melbourne, Melbourne, VIC
Open access:
Open access publishing facilitated by the University of Melbourne, as part of the Wiley – the University of Melbourne agreement via the Council of Australian University Librarians.
We are grateful to Rana Islamiah Zahroh (Nossal Institute for Global Health, the University of Melbourne) for training the authors in applying GRADE‐CERQual to qualitative evidence synthesis findings. We thank Alya Hazfiarini (Nossal Institute for Global Health, the University of Melbourne) for providing input on the quality appraisals. We are grateful to Shelly Makleff (Centre for Health Equity, the University of Melbourne) for her input to our discussion of values clarification workshops for health care providers.
No relevant disclosures.
Received 30 October 2024, accepted 24 February 2025
- 1. Starrs AM, Ezeh AC, Barker G, et al. Accelerate progress: sexual and reproductive health and rights for all. Report of the Guttmacher–Lancet Commission. Lancet 2018; 391: 2642‐2692.
- 2. Millar E. Abortion, decriminalisation and the medico‐legal paradigm. Soc Sci Med 2024; 355: 117098.
- 3. Melville C, Corbin B. Sexual and reproductive health rights in Australia: we have much to celebrate but must not be complacent. Med J Aust 2024; 220: 112‐114. https://www.mja.com.au/journal/2024/220/3/sexual‐and‐reproductive‐health‐and‐rights‐australia‐we‐have‐much‐celebrate‐must
- 4. Baird B. Medical abortion in Australia: a short history. Reprod Health Matters 2015; 23: 169‐176.
- 5. Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Clinical guideline for abortion care. An evidence‐based guideline on abortion care in Australia and Aotearoa New Zealand. Updated Sept 2024. https://ranzcog.edu.au/wp‐content/uploads/Clinical‐Guideline‐Abortion‐Care.pdf (viewed Oct 2024).
- 6. Keogh LA, Gurrin LC, Moore P. Estimating the abortion rate in Australia from national hospital morbidity and Pharmaceutical Benefits Scheme data. Med J Aust 2021; 215: 375‐376. https://www.mja.com.au/journal/2021/215/8/estimating‐abortion‐rate‐australia‐national‐hospital‐morbidity‐and
- 7. Subasinghe AK, McGeechan K, Moulton JE, et al. Early medical abortion services provided in Australian primary care. Med J Aust 2021; 215: 366‐370. https://www.mja.com.au/journal/2021/215/8/early‐medical‐abortion‐services‐provided‐australian‐primary‐care
- 8. Bateson D, McNamee K, Harvey C. Medical abortion in primary care. Aust Prescr 2021; 44: 187‐192.
- 9. Seymour JW, Melville C, Grossman D, et al. Examining service delivery patterns before and after implementation of a direct‐to‐patient telehealth service providing medication abortion in Australia. Aust N Z J Obstet Gynaecol 2024; 64: 647‐650.
- 10. Mazza D, Deb S, Subasinghe A. Telehealth: an opportunity to increase access to early medical abortion for Australian women. Med J Aust 2020; 213: 298‐299. https://www.mja.com.au/journal/2020/213/7/telehealth‐opportunity‐increase‐access‐early‐medical‐abortion‐australian‐women
- 11. Australian Department of Health and Aged Care. Reforming the health system to improve sexual and reproductive care [media release]. 31 May 2024. https://www.health.gov.au/ministers/the‐hon‐ged‐kearney‐mp/media/reforming‐the‐health‐system‐to‐improve‐sexual‐and‐reproductive‐care (viewed Oct 2024).
- 12. Vallury K, Kelleher D, Soffi A, et al. Systemic delays to abortion access undermine the health and rights of abortion seekers across Australia. Aust N Z J Obstet Gynaecol 2023; 63: 612‐615.
- 13. Sarder M, Mogharbel C, Kalman T. Realising access: abortion and contraception inequities and enablers in Victoria (Women's health Victoria knowledge paper 6). Women's Health Victoria, 24 Oct 2024. https://apo.org.au/node/328761 (viewed Feb 2025).
- 14. Senate Community Affairs References Committee. Ending the postcode lottery: addressing barriers to sexual, maternity and reproductive healthcare in Australia. May 2023. https://parlinfo.aph.gov.au/parlInfo/download/committees/reportsen/RB000075/toc_pdf/EndingthepostcodelotteryAddressingbarrierstosexual,maternityandreproductivehealthcareinAustralia.pdf (viewed Oct 2024).
- 15. Baird B. Abortion care is health care. Melbourne: Melbourne University Press, 2023.
- 16. Mazza D. Reimagining medical abortion in Australia: what do we need to do to meet women's needs and ensure ongoing access? Med J Aust 2023; 218: 496‐498. https://www.mja.com.au/journal/2023/218/11/reimagining‐medical‐abortion‐australia‐what‐do‐we‐need‐do‐meet‐womens‐needs‐and
- 17. World Health Organization. Abortion care guideline. Geneva: World Health Organization, 2022. https://iris.who.int/bitstream/handle/10665/349316/9789240039483‐eng.pdf?sequence=1 (viewed Oct 2024).
- 18. Therapeutic Goods Administration (Australian Department of Health and Aged Care). Amendments to restrictions for prescribing of MS‐2 Step (mifepristone and misoprostol) [media release]. 11 July 2023. https://www.tga.gov.au/news/media‐releases/amendments‐restrictions‐prescribing‐ms‐2‐step‐mifepristone‐and‐misoprostol (viewed Oct 2024).
- 19. Marie Stopes Health. MS health: June 2023 update. Melbourne: MSI Reproductive Choices, July 2023. https://resources.mshealth.com.au/20230704‐MS‐Health‐June‐2023.pdf (viewed Oct 2024).
- 20. Australian Department of Health and Aged Care. Summary statistics, allied health, all professions [dataset]. Updated 22 Oct 2024. https://hwd.health.gov.au/resources/data/summary‐all.html (viewed Oct 2024).
- 21. Mazza D, Burton G, Wilson S, et al. Medical abortion. Aust J Gen Pract 2020; 49: 324‐330.
- 22. Marie Stopes Australia. Nurse‐led medical termination of pregnancy in Australia: legislative scan. Second edition. Melbourne: Marie Stopes Australia, 2022. https://resources.msiaustralia.org.au/Nurse‐led‐MToP‐in‐Australia‐legislative‐scan.pdf (viewed Oct 2024).
- 23. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71.
- 24. Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012; 12: 181.
- 25. Hong QN, Pluye P, Fàbregues S, et al. Mixed methods appraisal tool (MMAT), version 2018. User guide. 1 Aug 2018. http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria‐manual_2018‐08‐01_ENG.pdf (viewed Oct 2024).
- 26. Hsu C, Sandford B. The Delphi technique: making sense of consensus. Practical Assessment, Research, and Evaluation 2007; 12: 10. https://doi.org/10.7275/pdz9‐th90 (viewed Oct 2024).
- 27. Jünger S, Payne SA, Brine J, et al. Guidance on conducting and reporting Delphi studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med 2017; 31: 684‐706.
- 28. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45.
- 29. Lewin S, Bohren M, Rashidian A, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings: paper 2. How to make an overall CERQual assessment of confidence and create a summary of qualitative findings table. Implement Sci 2018; 13 (Suppl 1): 11‐23.
- 30. Munthe‐Kaas H, Bohren MA, Glenton C, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings: paper 3. How to assess methodological limitations. Implement Sci 2018; 13 (Suppl 1): 25‐32.
- 31. Colvin CJ, Garside R, Wainwright M, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings: paper 4. How to assess coherence. Implement Sci 2018; 13 (Suppl 1): 33‐41.
- 32. Noyes J, Booth A, Lewin S, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings: paper 6. How to assess relevance of the data. Implement Sci 2018; 13 (Suppl 1): 51‐61.
- 33. Glenton C, Carlsen B, Lewin S, et al. Applying GRADE‐CERQual to qualitative evidence synthesis findings: paper 5. How to assess adequacy of data. Implement Sci 2018; 13 (Suppl 1): 43‐50.
- 34. Lee RY, Moles R, Chaar B. Mifepristone (RU486) in Australian pharmacies: the ethical and practical challenges. Contraception 2015; 91: 25‐30.
- 35. Newton D, Bayly C, McNamee K, et al. “… a one stop shop in their own community”: medical abortion and the role of general practice. Aust N Z J Obstet Gynaecol 2016; 56: 648‐654.
- 36. Keogh LA, Newton D, Bayly C, et al. Intended and unintended consequences of abortion law reform: perspectives of abortion experts in Victoria, Australia. J Fam Plann Reprod Health Care 2017; 43: 18‐24.
- 37. Dawson AJ, Nicolls R, Bateson D, et al. Medical termination of pregnancy in general practice in Australia: a descriptive–interpretive qualitative study. Reprod Health 2017; 14: 39.
- 38. Hulme‐Chambers A, Clune S, Tomnay J. Medical termination of pregnancy service delivery in the context of decentralization: social and structural influences. Int J Equity Health 2018; 17: 172.
- 39. de Moel‐Mandel C, Graham M, Taket A. Snapshot of medication abortion provision in the primary health care setting of regional and rural Victoria. Aust J Rural Health 2019; 27: 237‐244.
- 40. de Moel‐Mandel C, Graham M, Taket A. Expert consensus on a nurse‐led model of medication abortion provision in regional and rural Victoria, Australia: a Delphi study. Contraception 2019; 100: 380‐385.
- 41. Keogh L, Croy S, Newton D, et al. General practitioner knowledge and practice in relation to unintended pregnancy in the Grampians region of Victoria, Australia. Rural Remote Health 2019; 19: 5156.
- 42. Keogh LA, Gillam L, Bismark M, et al. Conscientious objection to abortion, the law and its implementation in Victoria, Australia: perspectives of abortion service providers. BMC Med Ethics 2019; 20: 11.
- 43. Deb S, Subasinghe AK, Mazza D. Providing medical abortion in general practice: general practitioner insights and tips for future providers. Aust J Gen Pract 2020; 49: 331‐337.
- 44. De Moel‐Mandel C, Taket A, Graham M. Identifying barriers and facilitators of full service nurse‐led early medication abortion provision: qualitative findings from a Delphi study. Aust J Adv Nurs 2020; 38: 18‐26.
- 45. Ogden K, Ingram E, Levis J, et al. Termination of pregnancy in Tasmania: access and service provision from the perspective of GPs. Aust J Prim Health 2021; 27: 297‐303.
- 46. Mazza D, Seymour JW, Sandhu MV, et al. General practitioner knowledge of and engagement with telehealth‐at‐home medical abortion provision. Aust J Prim Health 2021; 27: 456‐461.
- 47. Desai A, Maier B, James‐McAlpine J, et al. Views and practice of abortion among Queensland midwives and sexual health nurses. Aust N Z J Obstet Gynaecol 2022; 62: 219‐225.
- 48. Malatzky C, Hulme A. “I love my job … it's more the systems that we work in”: the challenges encountered by rural sexual and reproductive health practitioners and implications for access to care. Cult Health Sex 2022; 24: 735‐749.
- 49. Haas M, Church J, Street DJ, et al. How can we encourage the provision of early medical abortion in primary care? Results of a best‐worst scaling survey. Aust J Prim Health 2023; 29: 252‐259.
- 50. Mainey L, O’Mullan C, Reid‐Searl K. Working with or against the system: nurses’ and midwives’ process of providing abortion care in the context of gender‐based violence in Australia. J Adv Nurs 2023; 79: 1329‐1341.
- 51. Singh R, Mazza D, Moloney L, et al. General practitioner experiences in delivering early medical abortion services to women from culturally and linguistically diverse backgrounds: a qualitative–descriptive study. Aust J Gen Pract 2023; 52: 557‐564.
- 52. Saldanha S, Caddy C, Williams H, et al. Early medical abortion provision via telehealth in Victoria: a qualitative descriptive study. Aust J Gen Pract 2024; 53: 794‐798.
- 53. Sheeran N, Jones L, Corbin B, Melville C. Attitudes towards models of abortion care in sexual and reproductive health: perspectives of Australian health professionals. Aust J Prim Health 2024; 30: PY24100.
- 54. Noonan A, Millar E, Tomnay JE, et al. “Imagine if we had an actual service …”: a qualitative exploration of abortion access challenges in Australian rural primary care. Rural Remote Health 2024; 24: 9229.
- 55. Moulton JE, Arefadib N, Botfield JR, et al. A nurse‐led model of care to improve access to contraception and abortion in rural general practice: co‐design with consumers and providers. J Adv Nurs 2025; 81: 1019‐1037.
- 56. Srinivasan S, James SM, Kwek J, et al. What do Australian primary care clinicians need to provide long‐acting reversible contraception and early medical abortion? A content analysis of a virtual community of practice. BMJ Sex Reprod Health 2025; 51: 94‐101.
- 57. Liwanag HJ, James O, Frahsa A. A review and analysis of accountability in global health funding, research collaborations and training: towards conceptual clarity and better practice. BMJ Global Health 2023; 8: e012906.
- 58. Merner B, Haining CM, Willmott L, et al. Health providers’ reasons for participating in abortion care: a scoping review. Womens Health (Lond) 2024; 20: 17455057241233124.
- 59. Harris LH. Recognizing conscience in abortion provision. N Engl J Med 2012; 367: 981‐983.
- 60. Williams J, Mayes C. Abortion in Australia: what does the overturning of Roe v Wade have to do with it? [podcast]. Undisciplinary, 5 Aug 2022. https://undisciplinary.buzzsprout.com/1104002/episodes/11073451‐abortion‐in‐australia‐what‐does‐the‐overturning‐of‐roe‐v‐wade‐have‐to‐do‐with‐it (viewed Oct 2024).
- 61. Turner KL, Page KC. Abortion attitude transformation: a values clarification toolkit for global audiences. Chapel Hill: Ipas, 2008. https://www.ipas.org/wp‐content/uploads/2020/06/VALCLARE14‐VCATAbortionAttitudeTransformation.pdf (viewed Feb 2025).
- 62. Turner KL, Pearson E, George A, Andersen KL. Values clarification workshops to improve abortion knowledge, attitudes and intentions: a pre–post assessment in 12 countries. Reprod Health 2018; 15: 40.
- 63. Guiahi M, Wilson C, Claymore E, et al. Influence of a values clarification workshop on residents training at Catholic Hospital programs. Contracept X 2021; 3: 100054.
- 64. Emmerich N. The provision of abortion in Australia: service delivery as a bioethical concern. Monash Bioeth Rev 2024; 42: 200‐219.
- 65. Long C. Health specialists say biased Medicare rebates are costing women more [online]. ABC News (Australia), 4 Apr 2024. https://www.abc.net.au/news/2024‐04‐04/medicare‐bias‐costing‐women‐more‐mbs‐schedule/103664726?utm_campaign=abc_news_web&utm_content=link&utm_medium=content_shared&utm_source=abc_news_web (viewed Oct 2024).
- 66. Cheng HC, de Costa C. Abortion education in Australian medical schools. Aust N Z J Obstet Gynaecol 2021; 61: 793‐797.
- 67. Millar E. Abortion stigma, abortion exceptionalism, and medical curricula. Health Sociol Rev 2023; 32: 261‐276.
- 68. Srinivasan S, James SM, Kwek J, et al. What do Australian primary care clinicians need to provide long‐acting reversible contraception and early medical abortion? A content analysis of a virtual community of practice. BMJ Sex Reprod Health 2025; 51: 94‐101.
- 69. Queensland Health. Termination of pregnancy: action plan 2032. Mar 2024. https://www.health.qld.gov.au/__data/assets/pdf_file/0028/1316467/Termination‐of‐Pregnancy‐Plan_Digital.pdf (viewed Oct 2024).
- 70. Australian Capital Territory (Legislative Assembly). Health (Improved Abortion Access) Amendment Bill 2024. https://classic.austlii.edu.au/au/legis/act/bill/haaab2024383 (viewed June 2025).
- 71. Parliament of Western Australia. Abortion Legislation Reform Act 2023. https://www.legislation.wa.gov.au/legislation/statutes.nsf/law_a147399.html (viewed June 2025).
- 72. Mazza D, Shankar M, Botfield JR, et al. Improving rural and regional access to long‐acting reversible contraception and medical abortion through nurse‐led models of care, task‐sharing and telehealth (ORIENT): a protocol for a stepped‐wedge pragmatic cluster‐randomised controlled trial in Australian general practice. BMJ Open 2023; 13: e065137.
- 73. Australia Department of Health. National women's health strategy 2020–2030. Updated 31 Oct 2023. https://www.health.gov.au/sites/default/files/documents/2021/05/national‐women‐s‐health‐strategy‐2020‐2030_0.pdf (viewed Oct 2024).






Abstract
Objectives: To synthesise primary research findings about factors that affect medical abortion provision by general practitioners, nurses, midwives, and pharmacists in Australia.
Study design: Mixed methods systematic review of peer‐reviewed primary publications of qualitative, quantitative, and mixed methods studies of the provision of medical abortion in Australian primary care, 1 January 2013 – 18 January 2025.
Data sources: MEDLINE, Scopus, Web of Science, CINAHL (Cumulative Index to Nursing and Allied Health Literature).
Data synthesis: Twenty‐three publications satisfied our inclusion criteria. We undertook a thematic synthesis of the qualitative study findings to identify barriers and facilitators of medical abortion provision, and assessed the confidence of each review finding using the GRADE‐CERQual approach; we also compared the qualitative synthesis with quantitative study findings. We developed ten review findings grouped under three themes: moral, legal, and regulatory influences on abortion care (three review findings; very low to moderate confidence); the absence of a systems‐based approach to abortion provision (six review findings; moderate to high confidence); and early medical abortion belongs in primary care (one review finding; high confidence). Barriers to providing medical abortion include the absence of a supportive service delivery strategy, insufficient Medicare remuneration, geographic isolation, limited access to training, and colleagues who conscientiously object to abortion. Facilitators of its provision include clinician support networks and personal motivation to improve access to reproductive health care.
Conclusions: A range of individual, service level, and system factors exacerbate the effects of geographic location and financial considerations on the provision of medical abortion in Australian primary care. Our findings indicate that financial and structural support is needed for the geographic decentralisation of medical abortion training and services, the establishment of nurse‐led models of care, and the integration of abortion care into primary care.