About 476 million First Nations people live in more than 90 countries, about 6% of the world population.1 First Nations peoples are not a homogenous group, but include diverse communities that are among the oldest living cultures. However, most First Nations people share the experience and trauma of colonialism. Before colonisation of the traditional lands now known as Australia, Aboriginal and Torres Strait Islander people enjoyed a healthy, holistic lifestyle, co‐existing with and respecting the land and its resources.2 This lifestyle, with its rich lore, culture, and traditions, was deeply fractured by colonisation. The Aboriginal and Torres Strait Islander peoples remain strong and resilient, but the ongoing impact of colonisation has made their communities vulnerable to poor health, diminished by low levels of income, social protection, and education, inadequate housing and sanitation, unemployment, job insecurity, and poor working conditions.3
Life expectancy at birth for Aboriginal and Torres Strait Islander people is ten years lower than for non‐Indigenous Australians (in 2010–2012: 10.6 years lower for men, 9.5 years for women3); further, Indigenous people living in major cities are expected to live five years longer than Indigenous people in remote and very remote areas; the overall disease burden for Aboriginal and Torres Strait Islander people is 2.3 times as great as for non‐Indigenous Australians.4 The prevalence of diabetes is particularly high; the National Aboriginal Community Controlled Health Organisation has noted that the transition from a hunter–gatherer to a Western lifestyle was a major factor in Aboriginal and Torres Strait Islander people developing nutrition‐related diseases.5 The first national report on the health of Aboriginal and Torres Strait Islander people stated that diabetes only became a problem with the adoption of Western lifestyles.6 In 2018–19, 8% of Aboriginal and Torres Strait Islander people (64 100 people) had been diagnosed with diabetes, an incidence nearly three times that for non‐Indigenous Australians.7 Type 2 diabetes mellitus and its complications are a major cause of the gap in life expectancy between Aboriginal and Torres Strait Islander people and non‐Indigenous Australians, and the diabetes death rate is 4.4 times as high for Aboriginal and Torres Strait Islander people.7
Interventions for reducing the prevalence and impact of diabetes among Aboriginal and Torres Strait Islander people are therefore essential. Only one systematic review has evaluated the number and methodological quality of investigations of interventions for type 2 diabetes in First Nations people; it assessed studies from Australia, Canada, New Zealand, and the United States published during 1989–2008.8 This period preceded major developments in diabetes management, including new pharmacological interventions (eg, glucagon‐like peptide‐1 analogues, direct insulin delivery systems) and methods for measuring blood glucose levels (eg, continuous glucose monitoring). These advances can influence markers of disease and cardiometabolic risk factors, including blood glycated haemoglobin (HbA1c) and lipid levels, and hypertension.9,10 Understanding the impact of newer interventions on the health of Aboriginal and Torres Strait Islander people with type 2 diabetes is important for guiding clinical practice. Further, information is needed about whether interventions are tailored to the cultural, social, and historical circumstances of Aboriginal and Torres Strait Islander people, and therefore more likely to succeed. Evidence‐based, up‐to‐date information is needed to ensure that the most effective interventions are being used.
The authors of this article (Aboriginal and Torres Strait Islander and non‐Indigenous people) reviewed the literature for publications during 2000–2020 of investigations of the effectiveness of interventions for reducing the impact of type 2 diabetes in Aboriginal and Torres Strait Islander people. The primary aim was to review and summarise the characteristics and findings of the interventions. The secondary aims were to assess their effects on diabetes and cardiometabolic risk factors, including HbA1c, blood cholesterol, and triglyceride levels, body mass index, and other metabolic parameters, and to determine the proportion of people with type 2 diabetes who achieved therapeutic targets with each intervention.
Methods
We report our review according to the Preferred Reporting Items for Systematic Reviews and Meta‐analyses (PRISMA) checklist.11 The review protocol was prospectively registered with the PROSPERO International Prospective Register of Systematic Reviews (CRD42021231158; 13 February 2021).
Search strategy
Eligible for our review were publications of studies including Aboriginal or Torres Strait Islander people aged 15 years or older with diagnoses of type 2 diabetes, describing one or more diabetes interventions, and published in English during 1 January 2000 – 31 December 2020. We did not include publications about people with type 1 diabetes or gestational diabetes, or primarily about diabetes complications. We excluded qualitative studies, but did not otherwise limit the search by study design or type of intervention.
We searched eight electronic databases: MEDLINE (Ovid), Web of Science (Clarivate), the Cochrane Library, Global Health (EBSCO), Indigenous Collection (Informit), Indigenous Australia (Informit), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the World Health Organization International Clinical Trials Registry Platform (WHO‐ICTRP). Reference lists in the assessed articles were checked for further relevant publications.
We used combinations of search terms for three key themes:
- Indigenous Australians, native Australia people, Torres Strait Islander, first nations of Australia, first peoples of Australia, first Australians, Indigenous, native, tribe, aboriginal, first nation;
- medical subject headings “type 2 diabetes or type two diabetes or diabetes mellitus, type 2 or non‐insulin‐dependent diabetes”; and
- “intervention”.
During the database searching process, it was noted that including “intervention” as a keyword (first Ovid search), few articles regarding Aboriginal people with type 2 diabetes were identified; the final search strategy therefore omitted the term (second Ovid search; Supporting Information, part 1).
Search results were imported into EndNote X9, then exported to an XMLX file for import into Covidence (https://www.covidence.org); duplicates were removed automatically. The titles and abstracts of each publication were reviewed and assessed independently by two reviewers (authors CT, MAI); to resolve uncertainties, we consulted and sought decisions from the student study supervisor (author EE).
Data extraction and critical appraisal
Two authors (CT, MAI) extracted information for the key characteristics of the included articles: author, publication year, location, Aboriginal nations of the participants, study aim, study design, study duration, sample size, mean age, male participant proportion, intervention measures, nature of the control or comparison group or data, outcome measures, and findings. We summarise changes in metabolic parameters during the interventions in tables and bar charts.
Two authors (CT, MAI) independently checked and rated the studies using the quality assessment tool appropriate to the study design; disagreements were resolved by discussion (further details: Supporting Information, part 2).
Results
The database searches yielded 2546 records; after removing 1122 duplicates, 1424 records were screened by title and abstract. The full text of 55 articles deemed relevant was screened; seventeen articles that met the eligibility criteria were included in our review (Box 1): eleven cohort studies (seven retrospective audits,18,19,20,21,22,23,24 four prospective studies15,17,26,28), three randomised controlled trials,12,25,27 and three observational studies (non‐randomised follow‐up studies).13,14,16 (further details: Supporting Information, part 3).
The number of study participants ranged from 1815 to 1593;20 participant age at baseline ranged from 15 to 88 years; study duration ranged from three months27 to ten years.22 The most frequent research locations were Western Australia (three studies), the Northern Territory (three studies), and Queensland (three studies); other study locations were the Torres Strait Islands, Australian Capital Territory, New South Wales, Victoria, Northern Australia, and South Australia. Two large studies were conducted in more than one state: one in South Australia and Western Australia17 and one in 62 Aboriginal community health centres.20
Two studies included non‐Indigenous Australians as participants, but were included in our review because the proportions of Aboriginal or Torres Strait Islander participants were large (93%,23 96%21) (Supporting Information, part 3).
Overall risk of bias for the randomised controlled trials12,25,27 and the three follow‐up studies15,20,28 was low. Nine cohort studies were of good quality,15,17,18,20,21,22,23,24,26,28 two of poor quality.14,19 Eight of the seventeen studies included control groups or records for comparison;13,14,17,20,21,22,23,24 nine examined changes over time in single study groups12,15,16,18,19,25,26,27,28 (pre‐intervention/post‐intervention or post‐intervention results only); the absence of a control group may have influenced the reliability of the conclusions of these studies (Supporting Information, part 4).
Types of intervention for improving diabetes management in Aboriginal or Torres Strait Islander people
Twelve of 17 studies were site‐based (Aboriginal or Torres Strait Islander health service or diabetes clinics) rather than individual‐based diabetes interventions. Types of intervention included registers,12,13,24 recall and reminder systems,12,13,24 point‐of‐care testing services,17 diabetes care plans,13,18,21 specialist services14,21 (including community‐based or Aboriginal or Torres Strait Islander health workers,16,24,25 local health boards,13 and staff training13,24), developing clinical guidelines,13,16 undertaking audits and providing feedback,13,20 and improving the coordination of allied health services.22,24 In one study, the diabetes clinic provided cooking demonstrations and education about lifestyle and diabetes management;23 another held regular community health promotion days that included diabetes screening and education.21 Four studies found that outcomes were better when the Aboriginal or Torres Strait Islander communities were involved at all levels; for example, the involvement of Aboriginal Health Workers was independently associated with more frequent delivery of guideline‐scheduled diabetes care in remote areas.16 The presence of male Aboriginal Health Workers also improved adherence to guidelines because of the role of men in Aboriginal and Torres Strait Islander societies and the preference of people to be treated by health staff members of their own sex.16
Two studies focused on self‐management: a 5‐day diabetes residential camp study15 and the pilot of a diabetes self‐management care model.19 More recent studies used interventions that did not directly treat diabetes: laparoscopic adjustable gastric banding,26 full mouth non‐surgical periodontal scaling for people with moderate or severe periodontitis,23 and the treatment of Strongyloides stercoralis infections.18
One of the 17 studies was published in 2001,12 nine were published during 2010–202020,21,22,23,24,25,26,27,28 (mostly retrospective audits). Only three randomised controlled trials with adequate study design were reported. One evaluated a diabetes recall system combined with staff training, regular phone calls, newsletters, and workshops on basic diabetes care for Aboriginal or Torres Strait Islander people;12 another examined a community‐based, Aboriginal Health Worker‐led case management approach.25 In each study, the mean reduction in HbA1c level was greater in the intervention than the control group. The third randomised controlled trial assessed the effect of non‐surgical periodontal therapy on glycaemic control in Aboriginal or Torres Strait Islander people living with obesity and diabetes; the intervention did not significantly reduce HbA1c levels.27
Clinical outcomes
Two studies compared changes in metabolic parameters for intervention and control groups. A prospective cohort study found that laparoscopic adjustable gastric banding significantly reduced mean HbA1c level, weight, and body mass index in the intervention group;26 a randomised controlled trial found that community‐based health worker‐led management contributed to a significant decline in mean HbA1c level25 (Box 2).
Eleven studies13,14,15,17,18,19,23,24,25,27,28 reported absolute values for clinical parameters at baseline and follow‐up for the intervention and control groups. Four studies15,17,18,19 found that mean HbA1c level (expressed as percentages in most included reports) was significantly lower in the intervention group at follow‐up: 0.7 percentage points lower (P = 0.02) with point‐of‐care testing for HbA1c (results within six minutes) and urinary albumin–creatinine ratio (results within seven minutes);17 one percentage point lower (P = 0.02) with quality improvement measures for a diabetes care organisation system;18 1.1 percentage points lower three months after a 5‐day residential camp program;15 0.65 percentage points lower (P < 0.01) with the Flinders Model of diabetes self‐management care, a diabetes self‐management intervention delivered by Aboriginal or Torres Strait Islander health workers;19 1.6 percentage points lower (P < 0.01) with laparoscopic adjustable gastric banding;26 and 1.03 percentage points lower (P = 0.009) with treatment for S. stercoralis infection28 (Box 3).
Point‐of‐care testing increased the satisfaction of Aboriginal and Torres Strait Islander people with the diabetes service because of its convenience and the rapid results, which were monitored by doctors and linked with a structured chronic condition self‐management care plan.17 Point‐of‐care testing is not only a rapid assessment tool but also a management method suitable for Aboriginal or Torres Strait Islander people living in remote areas.
The rate of hospitalisation with diabetes or diabetes‐related conditions was 32% lower (P = 0.012) with a diabetes recall system in a 2001 study.12 A follow‐up study three years later that examined the sustainability of the intervention found that participants from intervention clinics were 40% less likely to have been admitted to hospital for a diabetes‐related condition; the proportion of people at the eight intervention sites who had achieved good glycaemic control (HbA1c < 53 mmol/mol) increased from 18% to 25%.14
Proportion of people who achieved therapeutic targets
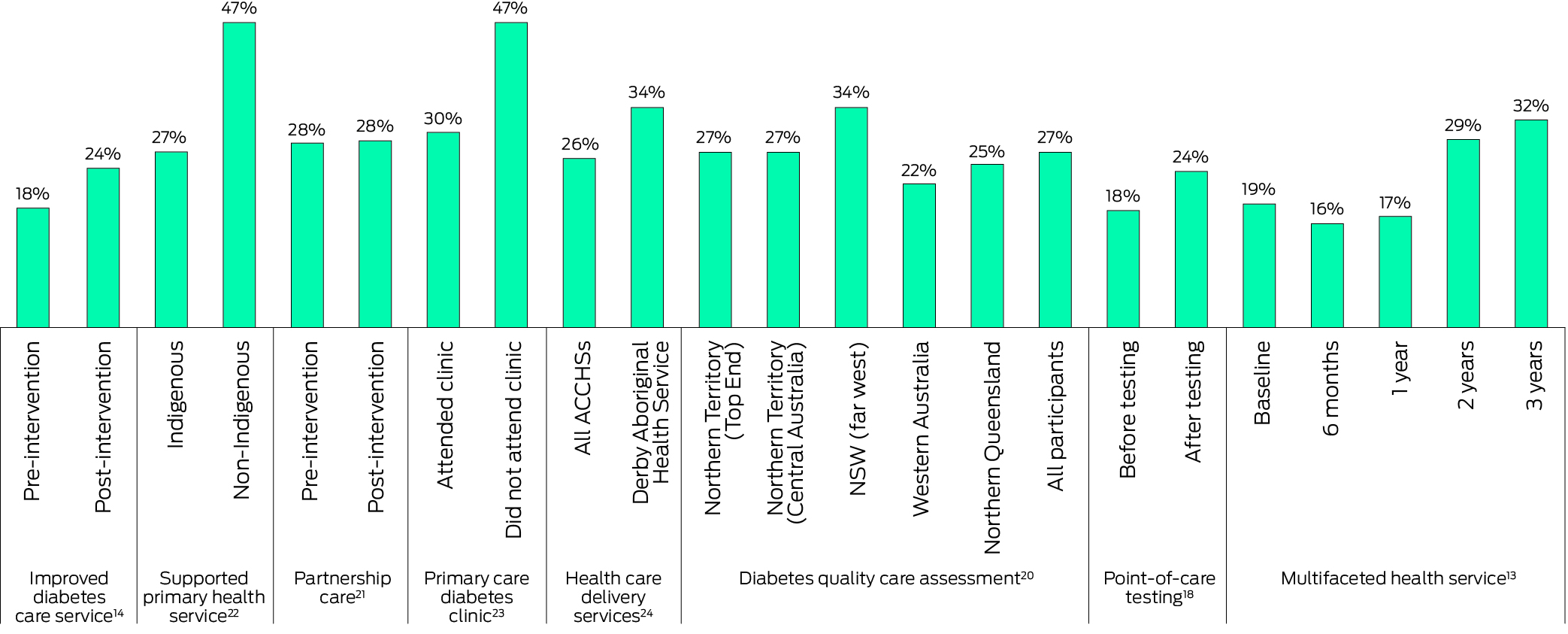
Eight studies13,14,17,20,21,22,23,24 reported the proportion of Aboriginal and Torres Strait Islander people with type 2 diabetes who achieved therapeutic targets according to various criteria (Supporting Information, part 5). The overall proportion of intervention group participants who achieved the target HbA1c level (below 53 mmol/mol) ranged from 16% to 47% (Box 4). Four studies found that improving diabetes care services increased the proportion who achieved the target: to 24% with registers, recall and reminder systems (18% prior to the intervention);14 to 34% with continued quality improvement in diabetes management at the Derby Aboriginal Health Service (26% at other Aboriginal community‐controlled health services in the Kimberley);22,24 24% after point‐of‐care testing (18% before testing);17 and 32% after three years of a multifaceted health service comprising responsibility planning by local health boards, clinical guideline development, staff training, audits and feedback (19% at baseline).13
A new model of partnership care involving regular community health promotion days and team outreach clinics increased the proportion of people who reached HbA1c and body mass index targets, and increased the number of people who met total cholesterol and triglyceride level targets.21 One study found that attending a diabetes clinic where education and management services were provided increased the proportion of people who achieved low‐density lipoprotein cholesterol targets.23 Well designed health care delivery also increased total cholesterol target achievement.24
Discussion
Our review identified few investigations of interventions for Aboriginal and Torres Strait Islander people with type 2 diabetes published during 2000–2020, and only three randomised controlled trials. Interventions reported to have statistically significant effects on HbA1c levels were laparoscopic adjustable gastric banding, a five‐day diabetes self‐management residential camp, treating S. stercoralis infections, community‐based health worker‐led management, point‐of‐care testing services, and the Flinders Model of self‐management care. Improving diabetes care services resulted in a larger proportion of people achieving the therapeutic HbA1c target (below 53 mmol/mol) and fewer hospital admissions with diabetes‐related conditions. Increasing interventional research in this area could concurrently improve the availability of intensive, sustained, and standardised diabetes services. It would also be an opportunity to consider the challenges of diabetes self‐management that result from the ongoing effects of colonisation and systemic racism on social determinants of health, including geographic isolation, stress, financial limitations, and family problems.
Of the interventions that reduced mean HbA1c levels, treating S. stercoralis infections and laparoscopic adjustable gastric banding differed in that neither directly treats diabetes or involves diabetes services. Treating these diseases had a statistically non‐significant effect on blood glucose management, and further research is needed before considering them for managing type 2 diabetes in Aboriginal and Torres Strait Islander people in general. Laparoscopic adjustable gastric banding can reduce the risk of cardiovascular disease and overall mortality and morbidity for people with obesity and type 2 diabetes,26 but it is invasive surgery that is neither appropriate nor feasible on a large scale. Treating helminth infections is essential and prevents anaemia, but such infections reflect inadequate housing and sanitation rather than an opportunity for managing diabetes.
Our review did not identify any published research regarding newer diabetes treatments and lifestyle interventions in Aboriginal or Torres Strait Islander people, including approaches linked with diabetes remission. The United Kingdom Diabetes Remission Clinical Trial (2019) found that 36% of participants in an integrated, structured weight management program had achieved diabetes remission by 24‐month follow‐up (HbA1c level below 48 mmol/mol after withdrawal of anti‐diabetes drugs at baseline); sustained remission was linked with the degree of sustained weight loss.29 This finding provides strong evidence that long term non‐pharmacological approaches can relieve type 2 diabetes or even lead to remission. Several studies are currently investigating components of this question, including a systematic review of physical activity interventions for preventing and managing type 2 diabetes in Aboriginal and Torres Strait Islander people30 and a scoping review of the characteristics of Aboriginal and Torres Strait Islander primary health care models.31
Interestingly, remission of type 2 diabetes was reported almost 40 years ago in Aboriginal people who reverted to a traditional lifestyle,32 indicating the importance of interventions that embrace cultural context, local protocols and beliefs, and taking the historical antecedents of type 2 diabetes into account.
New strategies for Aboriginal and Torres Strait Islander people must respond to a need or priority determined with community involvement and ownership. Several studies in our review found that outcomes were better when Aboriginal or Torres Strait Islander communities were involved at all levels. An earlier review also found that community‐owned and developed research and programs improved adherence to and sustainability for diabetes‐related interventions in Aboriginal and Torres Strait Islander people.9 Sports medicine studies conducted as collaborations between researchers and communities are examples of approaches that could reduce the impact of diabetes and should be a focus for future strategies.33,34,35 Working collaboratively can reduce the prevalence of inadequate glycaemic management and improve other cardiovascular risk factors and avert common diabetes‐related complications, such as diabetic nephropathy.36,37
Implications for practice, policy, and research
An international consensus regarding benchmarks for type 2 diabetes remission is required for assessing the effectiveness of new interventions. During 2019–20, the American Diabetes Association (ADA) convened an international expert group which proposed that remission be defined as a spontaneous or post‐intervention achievement of a HbA1c level below 48 mmol/mol that lasts at least three months in the absence of usual glucose‐lowering pharmacotherapy.38 None of the studies in our review examined remission, but those which reported therapeutic target data usually defined the target as a HbA1c level below 53 mmol/mol, higher than the cut‐off discussed by the ADA.
Given the high risk of type 2 diabetes in Aboriginal and Torres Strait Islander people, the paucity of randomised controlled trials was a key finding of our study. During screening in 2020, we identified four registered interventional studies including Aboriginal and Torres Strait Islander people with type 2 diabetes (Supporting Information, part 6). One39 had not recruited participants by the most recent update (2008); a cluster randomised controlled trial that had been published (co‐authored by one of the review authors) found weekly injections of exenatide (long‐acting release formulation), together with clinical review, education, and medication titration, achieved significant reductions in median HbA1c levels (–3.1%; 95% confidence interval, –5.80% to –0.38%)40 over 20 weeks in Aboriginal people in remote communities. The trial also established the feasibility of studies of diabetes treatments for Aboriginal or Torres Strait Islander people with type 2 diabetes living in remote parts of Australia. This an important finding, as remoteness has hampered diabetes research and interventions, and is one of the numerous barriers to diabetes care for Aboriginal and Torres Strait Islander people that need to be overcome (Supporting Information, part 7).
Limitations
Our review was limited by the low number of randomised controlled trials found. Many retrospective audits were identified; they illustrated the diversity of diabetes care in Aboriginal and Torres Strait Islander community health centres in Australia,18,20,24 and provided insights into health centre‐ and patient‐level characteristics. However, the longest audit (Derby Aboriginal Health Service, 1999–2009),22 was used as a comparator for the statistical analysis of retrospective audits at four Aboriginal Community Controlled Health Services in the Kimberley (2011–12).24 The audit periods and the diabetes services provided varied between studies, and the comparability of their findings is unclear. Other studies had specific limitations, including the lack of robust comparison groups or records,15,20,22 comparison data being for non‐Indigenous Australians,26 or small sample sizes (18 participants).15
Relevant research may have been reported in formats not captured by the eight databases we searched, including on Aboriginal and Torres Strait Islander websites, in government and community documents, and in the grey literature. Only a small number of relevant intervention studies were identified. All study types pertinent to the research topic were included (except qualitative studies), which may reduce the quality of some of our conclusions.
Conclusion
We found that interventions for Aboriginal and Torres Strait Islander people with type 2 diabetes that had significant impacts on mean HbA1c levels included laparoscopic adjustable gastric banding, a 5‐day diabetes self‐management residential camp, treating S. stercoralis infections, community‐based health worker‐led management, point‐of‐care testing services, and the Flinders Model of self‐management. Improved diabetes care services resulted in a larger proportion of Aboriginal and Torres Strait Islander people achieving therapeutic HbA1c targets. International benchmarks for diabetes remission are needed for assessing the effectiveness of interventions for people with type 2 diabetes. High quality interventional studies should be preferred to descriptive studies. Holistic, culturally safe interventions that take into account the social determinants of health underlying the high rates of type 2 diabetes in Aboriginal and Torres Strait Islander people are needed.
Box 1 – Identification and selection of publications of investigations of the effectiveness of interventions for reducing the impact of type 2 diabetes in Aboriginal and Torres Strait Islander communities, 2000–2020
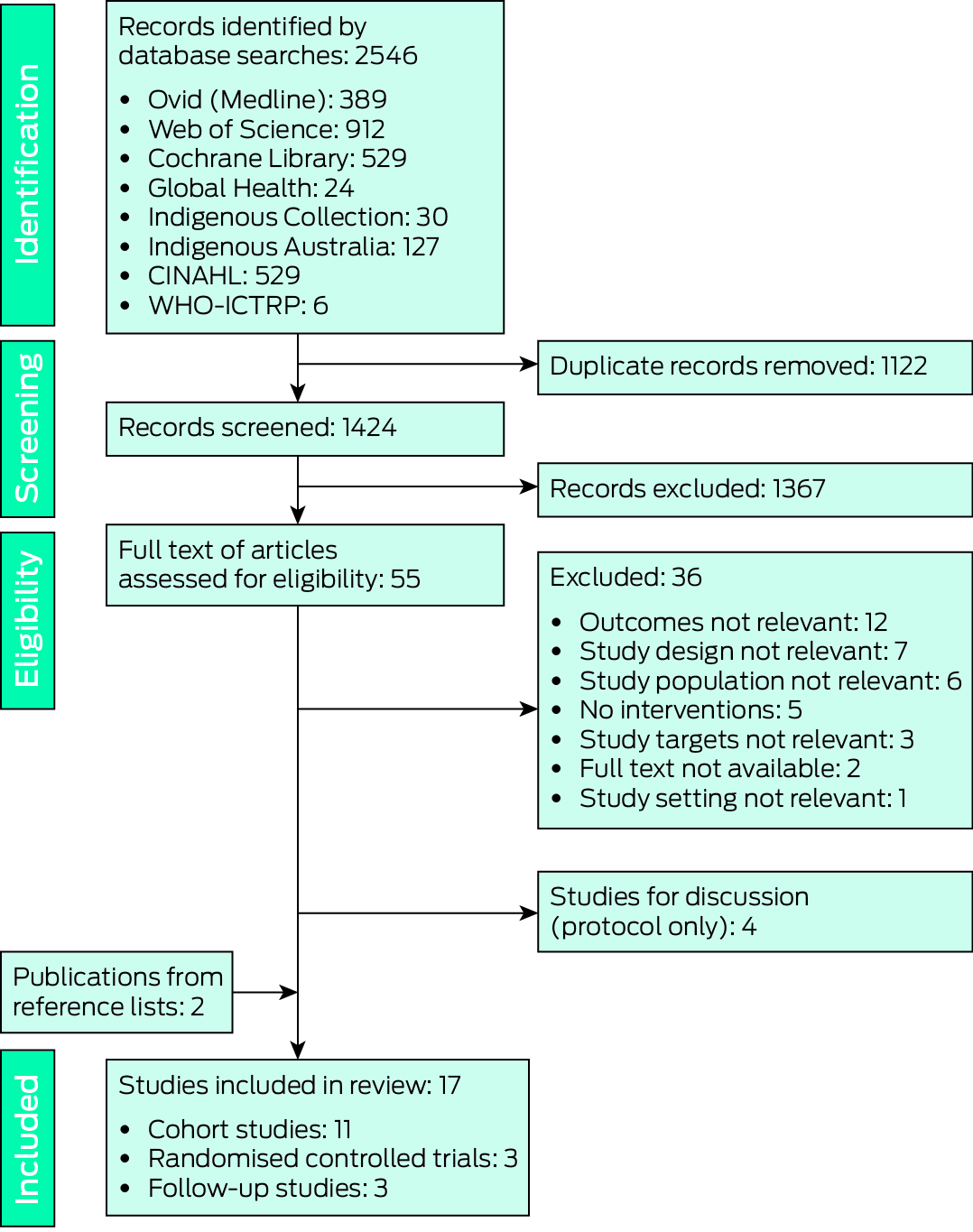
CINAHL = Cumulative Index to Nursing and Allied Health Literature; WHO‐ICTRP = World Health Organization International Clinical Trials Registry Platform.
Box 2 – Outcomes for the two studies that compared changes in metabolic parameters for intervention and control groups
|
|
|
Mean change (standard deviation) |
|||||||||||||
|
|
|
|
|
|
Blood pressure (mmHg) |
Cholesterol (mmol/L) |
|
||||||||
|
Intervention |
Participants (baseline/endpoint) |
Weight (kg) |
BMI (kg/m2) |
HbA1c (mmol/mol) |
Systolic |
Diastolic |
Total |
HDL‐C |
LDL‐C |
Triglycerides (mmol/L) |
|||||
|
|
|||||||||||||||
|
18 months with community‐based health worker25 |
|
|
|
|
|
|
|
|
|
|
|||||
|
Intervention group |
100/84 |
–0.6 (0.7) |
— |
— |
— |
— |
–0.6 (0.2) |
0.06 (0.02) |
–0.3 (0.1) |
0.2 (0.2) |
|||||
|
Control group (usual care) |
113/107 |
–1.5 (0.6) |
— |
— |
— |
— |
–0.3 (0.2) |
0.06 (0.02) |
–0.1 (0.1) |
0.1 (0.2) |
|||||
|
Two years after laparoscopic adjustable gastric banding26 |
|
|
|
|
|
|
|
|
|
|
|||||
|
Aboriginal or Torres Strait Islander participants |
30/26 |
–26.2 (14)* |
–9.9 (5.3)* |
–17.6 (14.1) |
–2.3 (17.7) |
–3.9 (9.6) |
0.4 (1.3) |
0.3 (0.3) |
–0.3 (1.2) |
–0.4 (1.3) |
|||||
|
Non‐Indigenous participants |
30/29 |
–21.1 (10.5) |
NR |
–20.0 (12.4) |
–6 (18) |
–0.7 (11) |
NR |
NR |
NR |
NR |
|||||
|
|
|||||||||||||||
|
BMI = body mass index; HbA1c = glycated haemoglobin; HDL‐C = high‐density lipoprotein cholesterol; LDL‐C = low‐density lipoprotein cholesterol; NR = not reported. * Each P < 0.001; no other differences in table were statistically significant. |
|||||||||||||||
Box 3 – Outcomes for studies that reported within‐group changes in mean values for metabolic parameters before and after interventions
|
|
Mean value (SD*): before/after the intervention |
||||||||||||||
|
|
|
|
|
Cholesterol (mmol/L) |
Blood pressure (mmHg) |
|
|||||||||
|
Study (first author)/intervention (follow‐up period) |
Weight (kg) |
BMI (kg/m2) |
HbA1c (mmol/mmol) |
Total |
HDL |
LDL |
Systolic |
Diastolic |
Triglycerides (mmol/L) |
||||||
|
|
|||||||||||||||
|
Bailie, 200413 |
|
|
|
|
|
|
|
|
|
||||||
|
Multifaceted health service: baseline |
— |
— |
75 |
— |
— |
— |
128 |
78 |
— |
||||||
|
Six months |
— |
— |
77 |
— |
— |
— |
130 |
80 |
— |
||||||
|
One year |
— |
— |
77 |
— |
— |
— |
129 |
78 |
— |
||||||
|
Two years |
— |
— |
74 |
— |
— |
— |
126 |
77 |
— |
||||||
|
Three years |
— |
— |
73 |
— |
— |
— |
128 |
80 |
— |
||||||
|
McDermott, 200414 (3 years) |
|
|
|
|
|
|
|
|
|
||||||
|
Improved diabetes care service |
86.8 (18.2)/91.3 (20.0)† |
— |
77 (24.0)/75 (25.1) |
— |
— |
— |
132.6 (17.4)/129.9 (20.2)† |
79.1 (17.1)/76.9 (11.2)† |
— |
||||||
|
Harris, 200515 |
|
|
|
|
|
|
|
|
|
||||||
|
5‐day camp (3 months) |
— |
— |
77 (21.9)/65 (18.8)† |
5.29 (1.06)/5.21 (0.89) |
— |
— |
— |
|
|
||||||
|
5‐day camp (6 months) |
— |
— |
77 (21.9)/70 (20.3) |
5.29 (1.06)/5.1 (1.08) |
— |
— |
— |
— |
3.39 (1.69)/2.66 (1.76) |
||||||
|
Shephard, 200617 |
|
|
|
|
|
|
|
|
|
||||||
|
Point‐of‐care testing (12 months) |
— |
— |
80 (22.9)/73 (20.8)† |
— |
— |
— |
— |
— |
— |
||||||
|
Point‐of‐care testing and self‐management care planning (18 months) |
83.3 (13.5)/ 83.2 (13.2) |
— |
72 (22.9)/58 (16.4)‡ |
5.92 (1.5)/4.93 (1.1)‡ |
— |
3.24 (1.2)/2.52 (0.7)‡ |
— |
— |
— |
||||||
|
Bailie, 200718 |
|
|
|
|
|
|
|
|
|
||||||
|
Improved system for diabetes care: baseline |
|
|
78 |
4.9 |
|
|
130 |
|
|
||||||
|
One year |
— |
— |
74† |
4.9 |
— |
— |
131 |
|
|
||||||
|
Two years |
— |
— |
74† |
4.9 |
— |
— |
130 |
|
|
||||||
|
Battersby, 200819 (12 months) |
|
|
|
|
|
|
|
|
|
||||||
|
Flinders Model (self‐management) |
— |
— |
72/65§ |
— |
— |
— |
139.5/136.7 |
84.6/83.8 |
— |
||||||
|
Chung, 201423 (6 months) |
|
|
|
|
|
|
|
|
|
||||||
|
Diabetes clinic attenders |
— |
37.2 |
66 |
4.4 |
1.0 |
2.3 |
134 |
80 |
2.3 |
||||||
|
Non‐attenders |
— |
36 |
65 |
4.7 |
1.1 |
2.6 |
138 |
81 |
2.4 |
||||||
|
Stoneman, 201424 |
|
|
|
|
|
|
|
|
|
||||||
|
All ACCHSs |
— |
— |
66 |
4.5 |
— |
— |
128 |
78 |
— |
||||||
|
DAHS |
— |
— |
64 |
4.5 |
— |
— |
120 |
75 |
— |
||||||
|
McDermott, 201525 (18 months) |
|
|
|
|
|
|
|
|
|
||||||
|
Health worker‐led management |
89.7 (22.6)/91.0 (23.1) |
— |
95 (23)/84 (25)‡ |
4.5 (1.3)/4.4 (1.4) |
0.9 (0.2)/0.9 (0.2) |
2.7 (1.1)/2.6 (0.9) |
127.9 (16.7)/132.5 (17.7) |
77.7 (10.4)/77.8 (9.9) |
— |
||||||
|
Control (usual care) |
91.4/87.4 |
— |
92 (20)/89 (24) |
4.6 (1.3)/4.7 (1.3) |
1.1 (0.6)/0.9 (0.2) |
2.6 (1.0)/2.6 (1.1) |
134.0 (20.9)/133.6 (19.4) |
81.0 (11.1)/81.3 (11.4) |
— |
||||||
|
Kapellas, 201727 (3 months) |
|
|
|
|
|
|
|
|
|
||||||
|
Periodontal scaling |
— |
— |
67.5 (23.9)/66.1 (22.4) |
4.8 (1.1)/4.5 (1.0) |
1.0/1.0 |
— |
— |
— |
— |
||||||
|
Control |
— |
— |
61.5 (18.8)/57.3 (18.6) |
4.6 (0.8)/4.4 (0.9 |
1.1 (0.2)/0.9 (0.2) |
— |
— |
— |
— |
||||||
|
Hays, 201728 |
|
|
|
|
|
|
|
|
|
||||||
|
Ivermectin treatment |
— |
30.5 (7.2)/30.7 (7.5) |
69.9 (24.2)/66.7 (23.4) |
— |
— |
— |
— |
— |
— |
||||||
|
Control |
— |
30.8 (6.7)/30.1 (6.4) |
68.2 (19.5)/73.1 (25.2) |
— |
— |
— |
— |
— |
— |
||||||
|
|
|||||||||||||||
|
ACCHS = Aboriginal community‐controlled health service; BMI = body mass index; DAHS = Derby Aboriginal Health Service; HbA1c = glycated haemoglobin; HDL‐C = high‐density lipoprotein cholesterol; LDL‐C = low‐density lipoprotein cholesterol. * If reported. † P < 0.05. ‡ P = 0.02. § P < 0.01. |
|||||||||||||||
Received 19 October 2023, accepted 13 February 2024
- Ciying Tan1
- Zoe Williams2
- Mohammad Ashraful Islam1
- Ray Kelly1
- Tuguy Esgin3,4
- Elif I Ekinci1,2
- 1 The Australian Centre for Accelerating Diabetes Innovations, Melbourne Medical School, the University of Melbourne, Melbourne, VIC
- 2 Austin Health, Melbourne, VIC
- 3 The University of Sydney, Sydney, NSW
- 4 Edith Cowan University, Perth, WA
We thank Anita Horvath (Medical Education, University of Melbourne) for her support and advice in the standard structure and format of the review.
Elif I Ekinci has received payment for sitting on an advisory panel for Eli Lilly Australia; and donated the money to her institution for diabetes research. She has received research support from Eli Lilly Australia, Novo Nordisk, Boehringer Ingelheim, the Eli Lilly Alliance, Versanis, Endogenex Insulet Corporation, and Medtronic.
- 1. World Bank. Indigenous Peoples. Updated 6 Apr 2023. https://www.worldbank.org/en/topic/indigenouspeoples (viewed Apr 2023).
- 2. Behrendt L. Indigenous Australians know we're the oldest living culture: it's in our dreamtime. The Guardian (Australia), 22 Sept 2016. https://www.theguardian.com/commentisfree/2016/sep/22/indigenous‐australians‐know‐were‐the‐oldest‐living‐culture‐its‐in‐our‐dreamtime (viewed Mar 2023).
- 3. Markwick A, Ansari Z, Sullivan, M, et al. Inequalities in the social determinants of health of Aboriginal and Torres Strait Islander People: a cross‐sectional population‐based study in the Australian state of Victoria. Int J Equity Health 2014; 13: 91.
- 4. Australian Institute of Health and Welfare. Indigenous health and wellbeing. 2 July 2024. https://www.aihw.gov.au/reports/australias‐health/indigenous‐health‐and‐wellbeing (viewed Mar 2023).
- 5. Education and Health Standing Committee (Western Australia Legislative Assembly). The food fix: the role of diet in type 2 diabetes prevention and management. Apr 2019. https://www.parliament.wa.gov.au/parliament/Commit.nsf/(Report+Lookup+by+Com+ID)/E65D9AAEA62B2B2C482583D800295552/$file/EHSC+Report+6+The+Food+Fix+FINAL.pdf (viewed Mar 2023).
- 6. Standing Committee on Aboriginal Affairs (House of Representatives). Aboriginal health report (Parliamentary Paper no. 60/1979). 20 Mar 1979. https://nla.gov.au/nla.obj‐2720242915 (viewed May 2021).
- 7. Australian Institute of Health and Welfare. Diabetes: Australian facts (CVD 96). Updated 17 June 2024. https://www.aihw.gov.au/reports/diabetes/diabetes (viewed June 2024).
- 8. McNamara BJ, Sanson‐Fisher R, D'Este C, Eades S. Type 2 diabetes in Indigenous populations: quality of intervention research over 20 years. Prev Med 2011; 52: 3‐9.
- 9. Sorli C, Harashima SI, Tsoukas GM, et al. Efficacy and safety of once‐weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): a double‐blind, randomised, placebo‐controlled, parallel‐group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol 2017; 5: 251‐260.
- 10. Taylor PJ, Thompson CH, Brinkworth GD. Effectiveness and acceptability of continuous glucose monitoring for type 2 diabetes management: a narrative review. J Diabetes Investig 2018; 9: 713‐725.
- 11. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71.
- 12. McDermott RA, Schmidt BA, Sinha A, Mills P. Improving diabetes care in the primary healthcare setting: a randomised cluster trial in remote Indigenous communities. Med J Aust 2001; 174: 497‐502.
- 13. Bailie RS, Si D, Togni SJ, et al. A multifaceted health‐service intervention in remote Aboriginal communities: 3‐year follow‐up of the impact on diabetes care. Med J Aust 2004; 181; 195‐200. https://www.mja.com.au/journal/2004/181/4/multifaceted‐health‐service‐intervention‐remote‐aboriginal‐communities‐3‐year
- 14. McDermott R, Tulip F, Sinha A. Sustaining better diabetes care in remote indigenous Australian communities. Qual Saf Health Care 2004; 13: 295‐298.
- 15. Harris C, Curtis O. Supporting self‐management of diabetes in Aboriginal people living with diabetes through a 5 day residential camp. Aborig Isl Health Work J 2005; 29: 4‐11.
- 16. Si D, Bailie RS, Togni SJ, et al. Aboriginal health workers and diabetes care in remote community health centres: a mixed method analysis. Med J Aust 2006; 185: 40‐45. https://www.mja.com.au/journal/2006/185/1/aboriginal‐health‐workers‐and‐diabetes‐care‐remote‐community‐health‐centres
- 17. Shephard MD, Mazzachi BC, Shephard AK, et al. Point‐of‐care testing in Aboriginal hands: a model for chronic disease prevention and management in Indigenous Australia. Point Care 2006; 5: 168‐176.
- 18. Bailie R, Si D, Dowden M, et al. Improving organisational systems for diabetes care in Australian Indigenous communities. BMC Health Serv Res 2007; 7: 67.
- 19. Battersby MW, Kit JA, Prideaux C, et al. Research implementing the Flinders Model of self‐management support with Aboriginal people who have diabetes: findings from a pilot study. Aust J Prim Health 2008; 14: 66‐74.
- 20. Si D, Bailie R, Dowden M, et al. Assessing quality of diabetes care and its variation in Aboriginal community health centres in Australia. Diabetes Metab Res Rev 2010; 26: 464‐473.
- 21. Harch S, Reeve D, Reeve C. Management of type 2 diabetes: a community partnership approach. Aust Fam Physician 2012; 41: 73‐76.
- 22. Marley JV, Nelson C, O'Donnell V, Atkinson D. Quality indicators of diabetes care: an example of remote‐area Aboriginal primary health care over 10 years. Med J Aust 2012; 197: 404‐408. https://www.mja.com.au/journal/2012/197/7/quality‐indicators‐diabetes‐care‐example‐remote‐area‐aboriginal‐primary‐health
- 23. Chung F, Herceg A, Bookallil M. Diabetes clinic attendance improves diabetes management in an urban Aboriginal and Torres Strait Islander population. Aust Fam Physician 2014; 43: 797‐802.
- 24. Stoneman A, Atkinson D, Davey M, Marley JV. Quality improvement in practice: improving diabetes care and patient outcomes in Aboriginal Community Controlled Health Services. BMC Health Serv Res 2014; 14: 481.
- 25. McDermott RA, Schmidt B, Preece C, et al. Community health workers improve diabetes care in remote Australian Indigenous communities: results of a pragmatic cluster randomized controlled trial. BMC Health Serv Res 2015; 15: 68.
- 26. O'Brien PE, DeWitt DE, Laurie C, et al. The effect of weight loss on Indigenous Australians with diabetes: a study of feasibility, acceptability and effectiveness of laparoscopic adjustable gastric banding. Obes Surg 2016; 26: 45‐53.
- 27. Kapellas K, Mejia G, Bartold PM, et al. Periodontal therapy and glycaemic control among individuals with type 2 diabetes: reflections from the PerioCardio study. Int J Dent Hyg 2017; 15: e42‐e51.
- 28. Hays R, Giacomin P, Olma L, et al. The relationship between treatment for Strongyloides stercoralis infection and type 2 diabetes mellitus in an Australian Aboriginal population: a three‐year cohort study. Diabetes Res Clin Pract 2017; 134: 8‐16.
- 29. Lean ME, Leslie WS, Barnes AC, et al. Durability of a primary care‐led weight‐management intervention for remission of type 2 diabetes: 2‐year results of the DiRECT open‐label, cluster‐randomised trial. Lancet Diabetes Endocrinol 2019; 7: 344‐355.
- 30. Evans J, Canuto K, Kelly R, et al. Physical activity interventions to prevent and manage type 2 diabetes among Aboriginal and Torres Strait Islander peoples: a systematic review protocol. JBI Evid Synth 2021; 19: 177‐183.
- 31. Harfield S, Davy C, Kite E, et al. Characteristics of Indigenous primary health care models of service delivery: a scoping review protocol. JBI Database System Rev Implement Rep 2015; 13: 43‐51.
- 32. O'Dea K. Marked improvement in carbohydrate and lipid metabolism in diabetic Australian Aborigines after temporary reversion to traditional lifestyle. Diabetes 1984; 33: 596‐603.
- 33. Esgin T, Hersh D, Rowley KG, et al. Physical activity and self‐reported metabolic syndrome risk factors in the Aboriginal population in Perth, Australia, measured using an adaptation of the Global Physical Activity Questionnaire (GPAQ). Int J Environ Res Public Health 2021; 18: 5969.
- 34. Esgin T, Hersh D, Rowley K, et al. Indigenous research methodologies: decolonizing the Australian sports sciences. Health Promot Int 2019; 34: 1231‐1240.
- 35. Esgin T, Johnston N, Rowley K, et al. Effect of 12 weeks combined aerobic and resistance training on fitness, arterial stiffness and body composition in Indigenous Australian men and women [abstract: ASICS Sports Medicine Australia Conference, Langkawi, Malaysia, 25–28 Oct 2017]. J Sci Med Sport 2017; 20 (Suppl 3): 43.
- 36. Jack S. Closing the gap on diabetes: a social determinants of health perspective. Aborig Isl Health Work J 2012; 36: 27‐30.
- 37. Bate KL, Jerums G. Preventing complications of diabetes. Med J Aust 2003; 179: 498‐503. https://www.mja.com.au/journal/2003/179/9/3‐preventing‐complications‐diabetes
- 38. Riddle MC, Cefalu WT, Evans PH, et al. Consensus report: definition and interpretation of remission in type 2 diabetes. J Clin Endocrinol Metab 2022; 107: 1‐9.
- 39. Brown LM. A randomised trial of pioglitazone versus metformin monotherapy in Indigenous Australians with type 2 diabetes: effects on metabolic and cardiovascular parameters [Trial registered on ANZCTR: ACTRN12607000135415]. Updated 25 July 2008. https://anzctr.org.au/ACTRN12607000135415.aspx (viewed Mar 2021).
- 40. Ekinci EI, Pyrlis F, Hachem M, et al. Feasibility of once weekly exenatide–LAR and enhanced diabetes care in Indigenous Australians with type 2 diabetes (Long‐acting–once‐weekly‐exenatide laR–SUGAR, “Lower SUGAR” study). Intern Med J 2021; 51: 1463‐1472.






Abstract
Objectives: To review studies of interventions for reducing the impact of type 2 diabetes in Aboriginal and Torres Strait Islander people. The primary aim was to review and summarise the characteristics and findings of the interventions. The secondary aims were to assess their effects on diabetes and cardiometabolic risk factors, and the proportions of people with type 2 diabetes who achieved therapeutic targets with each intervention.
Study design: We searched eight electronic databases for publications of studies including Aboriginal or Torres Strait Islander people aged 15 years or older with diagnoses of type 2 diabetes, describing one or more diabetes interventions, and published in English during 1 January 2000 – 31 December 2020. Reference lists in the assessed articles were checked for further relevant publications.
Data sources: MEDLINE (Ovid), Web of Science (Clarivate), the Cochrane Library, Global Health (EBSCO), Indigenous Collection and Indigenous Australia (Informit), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the World Health Organization International Clinical Trials Registry Platform (WHO‐ICTRP).
Results: The database searches yielded 1424 unique records; after screening by title and abstract, the full text of 55 potentially relevant articles were screened, of which seventeen met our eligibility criteria: eleven cohort studies (seven retrospective audits and four prospective studies), three randomised controlled trials, and three observational, non‐randomised follow‐up studies. Twelve publications reported site‐based (Aboriginal or Torres Strait Islander health service or diabetes clinic) rather than individual‐based diabetes interventions. Interventions with statistically significant effects on mean glycated haemoglobin (HbA1c) levels were laparoscopic adjustable gastric banding, a 5‐day diabetes self‐management camp, treatment ofStrongyloides stercoralis infections, community‐based health worker‐led management, point‐of‐care testing, and self‐management approaches.
Conclusions: Few interventions for Aboriginal and Torres Strait Islander people with type 2 diabetes have been reported in peer‐reviewed publications. Improving diabetes care services resulted in larger proportions of people achieving therapeutic HbA1c targets. Outcomes were better when Aboriginal and Torres Strait Islander communities were involved at all levels of an intervention. High quality studies of holistic, culturally safe and accessible interventions should be the focus of research.