In Australia, 500 000 patients present to the emergency department (ED) with chest pain each year.1 Chest pain is the second most common reason of adult ED presentation, accounting for 4.2% of all presentations, and the number of patients presenting with chest pain is increasing.2,3,4 Annually, some hospitals in Australia have over 4000 chest pain presentations, with 34–66% of these patients admitted.5 Nevertheless, up to 70–85% of these patients do not have an acute coronary syndrome (ACS), and 45–60% are deemed low or intermediate risk for cardiac chest pain.3,6,7
Hospitalisation creates direct and indirect costs for both patients and health care providers. For patients, nosocomial infections can complicate up to 4–9% of admissions.8,9,10 For the health care provider and administrators, issues include ED overcrowding leading to poorer patient outcomes, decreased potential hospital revenue, and the direct cost of a ward admission.11
Consideration of alternative outpatient pathways represent a possible “win‐win” for patients and health care services. Chest pain clinics are one such potential solution that have generated positive results internationally, mainly in the United Kingdom, demonstrating cost‐saving through avoiding hospital admission without a compromise in safety.12 The United Kingdom implemented a top‐down approach, with a national roll‐out leading to the formation of a rapid access chest pain clinic (RACC) in every National Health Service (NHS) acute trust. In contrast, Australian and New Zealand RACCs have been developed and created at local hospital network levels in response to demands across an expanding number of jurisdictions.
In this article, we review the models and experiences of these RACCs in Australia and New Zealand, considering the opportunities, challenges and benefits of developing a national framework. We searched the literature for studies exploring RACCs in the Australian and New Zealand context using terms including “chest pain clinic”, “cardiology clinic”, “rapid access cardiology service”, “Australia” and “New Zealand” through the databases PubMed, MEDLINE and EMBASE, from database inception to May 2022. We searched the grey literature using Google Scholar, and also reviewed the reference lists of identified articles. We identified 14 studies (Box 1) that explored RACCs in Australia and New Zealand, including six tertiary referral hospitals in large cities, one outer‐metropolitan hospital in New South Wales, one tertiary referral hospital in Tasmania, and one large District Health Board in Auckland. The RACCs at these centres were created between 2010 and 2018.
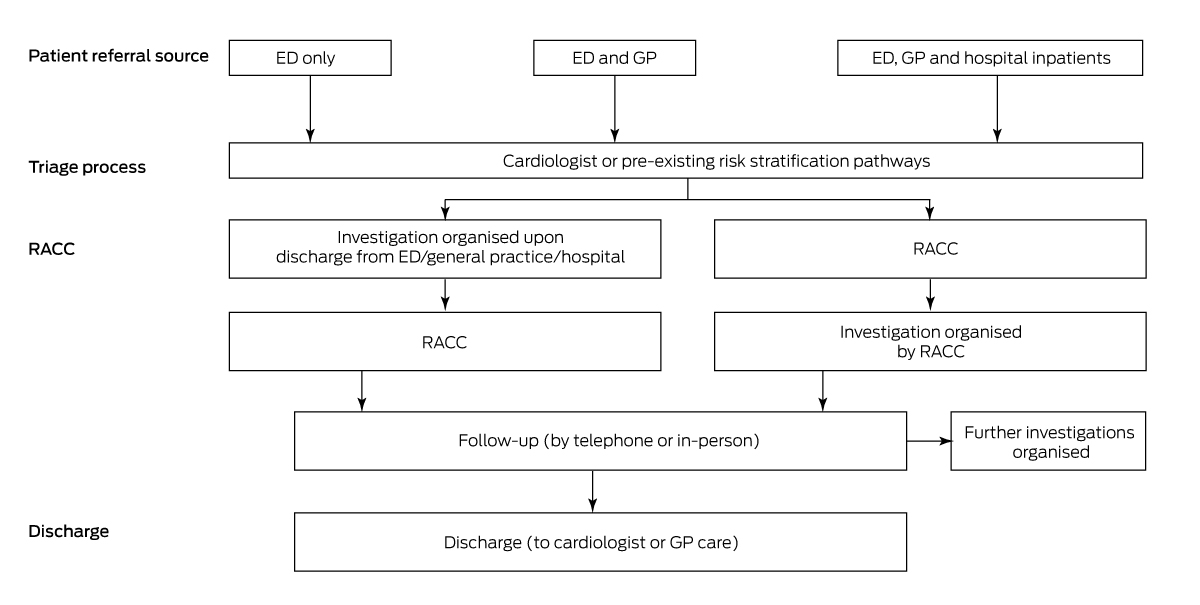
RACC models
Several RACC models exist in Australia and New Zealand (Box 2). All models in the published literature are run and supervised by cardiologists, with other additional staff including cardiology registrars,22 registrars in conjunction with clinical nurse specialists,6 a predominantly nurse‐led clinic,21 and larger clinics with registrars, junior medical officers, nursing and administrative support.2 One study explored RACCs via telehealth.18 Most RACCs reviewed patients who were referred for evaluation of chest pain, but two clinics also received referrals for investigation of dyspnoea, syncope and arrhythmia.13,20
Referral pathways were varied. Most services included patients discharged and referred from the corresponding hospital's ED (the most common pathway; five of seven clinics specified referral pathways),6,19,23 and other RACCs also received referrals from hospital physicians (least common pathway; one out of seven clinics),2 and/or from general practitioners (fairly common pathway; four out of seven clinics).2,14,20,21 Referrals were triaged and risk stratified according to either established pathways (eg, the HEART score)25 or via the clinic's cardiologist.21,22
Characteristics of patients attending RACCs
Patients attending RACCs in identified studies were predominantly men (47–78% of the cohort), with mean ages in the studies ranging from 52 to 62 years. Patients had a high burden of traditional cardiovascular risk factors, including hypertension (22–37%), dyslipidaemia (37–38%), diabetes (14–20%), tobacco use (14–41%), obesity with body mass index greater than 30 m2 (44%), and significant family history of cardiovascular disease (33–46%).6,14,16,21 The majority of patients (81–94%) had two or more cardiovascular risk factors.6,14,16,21
Clinic management and interventions
Most patients were seen within one to 12 days,2,6,13,14,17,23 although one study had a median waiting time of 18 days (interquartile range, 14–21 days).21 A variety of investigations were performed in the different clinics depending on local resources and expertise, including exercise stress testing (clinics ranged in their use between 30% and 93% of patients), computed tomography coronary angiography (CTCA; 8–67%), stress echocardiography (12–60%), and nuclear myocardial perfusion scans (9–27%), with invasive angiogram performed as the first investigation in only up to 4% of patients.2,6,13,14,19,21,23 Following non‐invasive investigations, 5–7% of RACC patients had subsequent invasive angiography, with 2–4% requiring revascularisation.2,6,13,14,19,21,23 Depending on investigation results, patients were referred for ongoing cardiology or GP follow‐up.13,14
Opportunities for primary and secondary prevention
Given the high prevalence of modifiable risk factors, health care providers have used RACCs as an opportunity to implement strategies for primary and secondary prevention of cardiovascular disease. These interventions include smoking cessation discussions, cardiac rehabilitation referrals, and statins and/or aspirin commencement, with 21–32% of clinic patients having medications added or modified.15,21,23 One randomised trial of RACC patients (n = 189)15 compared usual care with an intervention comprised of all five of the following:
- additional counselling on five‐year cardiovascular risk;
- pharmacotherapy prescribed if indicated;
- referral to a public smoking cessation service;
- lifestyle advice by a cardiac rehabilitation nurse; and
- encouragement to discuss risk factors with their GP.
Patients in the intervention group had significantly improved five‐year absolute risk scores at follow‐up (at least 12 months after baseline assessment) as measured through the Australian absolute cardiovascular disease risk calculator (www.cvdcheck.org.au/calculator) compared with the usual care chest pain clinic group (mean, −2.4 percentage points [95% CI, −1.5 to −3.4 percentage points] v + 0.4 percentage points [95% CI, −0.8 to 1.5 percentage points]).15 These findings indicate that chest pain clinics may be an ideal avenue through which patients can learn effective preventive measures to improve their cardiovascular health.
Safety
Four studies reported the operating of RACCs to be safe.2,6,14,24 Studies reported no patient mortality while awaiting follow‐up,2,6,14 with a low number of RACC patients (1%) requiring direct admission to hospital for invasive coronary angiography and 0.5% having ACS (n = 3; one with non‐ST‐elevation myocardial infarction and two with unstable angina).2 In one long term study, after adjusting for age, sex, hypertension, diabetes, smoking and dyslipidaemia, patients attending a RACC had fewer major adverse cardiovascular events at 12 months compared with a historical control (adjusted odds ratio [OR], 0.09; 95% CI, 0.02–0.46).14 Another study that explored differences in all‐cause mortality between a RACC cohort (n = 1133; mean follow‐up, 6.3 years; standard deviation, 2.6 years) against an age‐ and sex‐matched general population control (people in NSW over the same study period)24 found lower all‐cause mortality in the RACC cohort group for the patients aged 55–64 years (n = 292; mortality rate per patient‐year 0.33 v expected mortality rate per year 0.63; relative risk [RR] of death, 0.53; P = 0.01), 65–74 years (n = 182; 0.54 v 1.76; RR = 0.31; P < 0.001) and 75 years or older (n = 62; 4.33 v 7.77; RR = 0.56; P < 0.001), with no differences in all‐cause mortality for patients aged 16–54 years.24
Hospital efficiency and costs
RACC services improve hospital efficiency and costs. After a RACC was introduced, one study (n = 209) reported a mean decrease in ED length of stay of 98 minutes between the first and final 50 patients of their six‐month dataset.23 Another study (n = 63; over six months), estimated 31 inpatient days were saved due to the establishment of a RACC.13 RACCs allow patients to be discharged from the ED without the need for hospitalisation. This improves hospital efficiency and capacity via better use of services and financial savings. One study including three different RACCs in NSW calculated the average cost of patients attending a RACC to be $427–$474, with a saving per patient of $1149–$1196 by avoiding hospital admission.17
These benefits were seen in conjunction with low rates of re‐presentation. A study (n = 1133) reported that 0.4% of patients re‐presented to the ED within 48 hours (no patients with ACS), 2.1% of patients re‐presented between two and 28 days after ED presentation (no patients with ACS), and, the year after RACC implementation, one study reported a 2.3% decrease in readmissions (absolute reduction of n = 140) over the following 12‐month period.2,6 After adjusting for age, sex, hypertension, diabetes, smoking and dyslipidaemia, RACC patients had fewer ED representations over 30 days compared with historical controls without RACC attendance (adjusted OR, 0.36; 95% CI, 0.19–0.67), and fewer ED representations over 12 months compared with a historical control without RACC attendance (adjusted OR, 0.41; 95% CI, 0.28–0.58).14
Patient and referrer acceptability
Most patients reported a positive experience of RACCs. One study (n = 328) noted that 93% of patients “strongly agreed” that RACC services were useful to their community, 91% “strongly agreed” that they were comfortable with their management plan, 86% “strongly agreed” that they felt less anxious about their condition following RACC attendance, and less than 1.5% had negative responses to the RACC.2 A separate study (n = 190) reported that 82% of respondents were happy with the decision to be discharged from the ED, and only 5% were dissatisfied with the follow‐up time to the clinic.19 Most respondents had positive experiences related to the RACC, including 95% being very satisfied with the respect from health professionals in the clinic, and 76% strongly agreeing with having adequate explanation of their test results.19 Referrers also had positive experiences, with one study (n = 17) reporting that 94% of referrers were “satisfied” or “very satisfied” with the RACC.
Comparisons between RACCs in the United Kingdom and Australia and New Zealand
RACCs in the United Kingdom have been shown to reduce hospital presentation in a safe manner, thus being cost‐saving.26,27,28 This is despite a key difference between the two contexts: in the UK, RACC patients tend to be referred from GPs, whereas in the Australian and New Zealand studies, patients are predominantly referred from the ED.29 The difference in referral pathways is likely a contributing factor in divergent diagnostic rates — in the UK 4–16% of RACC patients have ACS, whereas in Australia and New Zealand these patients have been largely ruled out through their initial ED presentation.2 In addition, RACCs in the UK have implemented effective nurse practitioner‐led models.30,31
Similar to Australia and New Zealand, RACCs in the UK have a variety of first line investigations, including stress imaging modalities such as exercise stress testing, stress echocardiogram or myocardial perfusion scans and anatomical imaging such as CTCA. In the UK, with an update to the National Institute for Health and Care Excellence stable chest pain clinical guideline in 2016, there is a deliberate move towards CTCA as the first line test.32,33 International guidelines, such as the 2021 American Heart Association/American College of Cardiology guidelines on chest pain, suggest either strategy of anatomical or functional testing is reasonable for intermediate risk chest pain depending on patient characteristics, local availability and expertise.34 From our review, it is unclear if there is a shifting trend towards functional or anatomical testing in Australian and New Zealand RACCs.
Avenues for future research
There is a wide variation of RACCs in Australia and New Zealand. Not all hospital networks have RACCs, and, within RACCs, there are varied referral pathways, models of care, staffing, investigations ordered, and clinic guidelines. Future research could explore sharing data across sites or establishing a database to review existing practices at a binational level. Studies should also consider exploring RACCs in the private sector and in public clinics without current published data. Examining existing practices throughout Australia and New Zealand, combined with analysis of health economic data and outcomes, would allow for best practices and standard of care guidelines to be created.
Limitations
Articles that mentioned adverse events or re‐admission rates may have been under‐reported if patients had presented to an alternative health network, but these numbers were thought to be small.2,6,14 This review only included RACC services with published data, which may represent an academic subset of services in Australia and New Zealand. Public and private RACC services that exist without published data were not included in this review (there were at least 14 of these clinics in Australia and New Zealand at the time of writing; May 2023).
Conclusion
RACCs are a relatively new offering to now multiple cardiology services across Australia and New Zealand. Most Australian and New Zealand RACCs described in the literature have been designed as an alternative pathway to hospitalisation for patients without ACS and with chest pain at low to intermediate risk for cardiac chest pain thus avoiding investigation in hospital. The main referral source is the ED, followed by GPs. Patients attending RACCs unsurprisingly have higher levels of cardiovascular risk factors and cardiovascular events compared with community surveys, and several studies conclude they are safe. Patients report high satisfaction with the services, and reports demonstrate they reduce costs, which is driven by reduced hospitalisation. In addition to the direct benefits of reduced hospitalisation and ED length of stay, some RACCs are identifying opportunities to specifically add prevention services. There is some variation in RACC model implementation, but there are little data to indicate what the optimal approaches are. Developing a national framework may be beneficial to allow sites with equitable access to the evidence, possible models, and business cases, with involvement and education to local primary care services to strengthen referral pathways, safely avoid hospitalisation, and allow effective transitions of care. Longer term follow‐up of patients presenting to RACCs and linked data analysis may enable a better understanding and monitoring of the service.
Box 1 – Results of rapid access chest pain clinics (RACCs) in Australian New Zealand studies
|
Author (year) |
Location |
Sample size |
Sex (male) |
Age (years), mean (SD) |
Summary |
||||||||||
|
|
|||||||||||||||
|
Back et al (2019)13 |
Tertiary referral hospital, NSW |
63 |
63% |
52.7* |
|
||||||||||
|
Black et al (2019)14 |
Tertiary referral hospital, Tasmania |
1479 |
47.9% |
55.9 (13.1) |
|
||||||||||
|
Black et al (2021)15 |
Tertiary referral hospital, Tasmania |
189 |
78%† |
59 (8.1)† |
|
||||||||||
|
67%‡ |
59.5 (7.9)‡ |
||||||||||||||
|
Tertiary referral hospital, NSW |
520 |
55% |
55.2* |
|
|||||||||||
|
Kozor et al (2021)17 |
Tertiary referral hospital, NSW |
Modelling |
_ |
_ |
|
||||||||||
|
Black et al (2023)18 |
Tertiary referral hospital, Tasmania |
140 |
Unspecified |
Unspecified |
|
||||||||||
|
Lembo et al (2020)19 |
Tertiary referral hospital, NSW |
190 |
53% |
56.4 (13.6) |
|
||||||||||
|
Magdy et al (2020)20 |
Tertiary referral hospital, NSW |
1261 |
52.6% |
61.6* |
|
||||||||||
|
McLachlan et al (2019)21 |
District Health Board in Auckland |
3587 |
54% |
Unspecified |
|
||||||||||
|
Nkoane‐Kelaeng et al (2017)22 |
Tertiary referral hospital, NSW |
15 |
Unspecified |
Unspecified |
|
||||||||||
|
Said et al (2020)23 |
Outer‐metropolitan hospital, NSW |
209 |
50% |
62.3* |
|
||||||||||
|
Yu et al (2018)6 |
Tertiary referral hospital, NSW |
1133 |
61% |
54.3 (12.3) |
|
||||||||||
|
Yu et al (2021)24 |
Tertiary referral hospital, NSW |
1133 |
61% |
54.3 (12.3) |
|
||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; CTCA = computed tomography coronary angiography; ED = emergency department; GP = general practitioner; IQR = interquartile range; NSW = New South Wales; RR = relative risk; SD = standard deviation. * SD not available. † Control group. ‡ Intervention group. |
|||||||||||||||
Provenance: Not commissioned; externally peer reviewed.
- Kenneth K Cho1
- John K French1
- Gemma A Figtree2,3
- Clara K Chow3,4
- Rebecca Kozor3
- 1 Liverpool Hospital, Sydney, NSW
- 2 Royal North Shore Hospital, University of Sydney, Sydney, NSW
- 3 University of Sydney, Sydney, NSW
- 4 Westmead Applied Research Centre and Westmead Hospital, Sydney, NSW
Open access:
Open access publishing facilitated by Western Sydney University, as part of the Wiley – Western Sydney University agreement via the Council of Australian University Librarians.
No relevant disclosures.
- 1. Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Med J Aust 2016; 205: 128‐133. https://www.mja.com.au/journal/2016/205/3/national‐heart‐foundation‐australia‐and‐cardiac‐society‐australia‐and‐new
- 2. Klimis H, Khan ME, Thiagalingam A, et al. Rapid access cardiology (RAC) services within a large tertiary referral centre — first year in review. Heart Lung Circ 2018; 27: 1381‐1387.
- 3. Cullen L, Greenslade J, Merollini K, et al. Cost and outcomes of assessing patients with chest pain in an Australian emergency department. Med J Aust 2015; 202: 427‐432. https://www.mja.com.au/journal/2015/202/8/cost‐and‐outcomes‐assessing‐patients‐chest‐pain‐australian‐emergency‐department
- 4. Australian Institute of Health and Welfare. Emergency department care. Canberra: AIHW, 2021. https://www.aihw.gov.au/getmedia/433caea4‐03ff‐4569‐96ac‐042f2844f29c/Emergency‐department‐care‐2019‐20.xlsx.aspx (viewed Oct 2022).
- 5. Kozor R, Mooney J, Lowe H, et al. Rapid access chest pain clinics: an Australian cost–benefit study. Heart Lung Circ 2019; 28: S315.
- 6. Yu C, Sheriff J, Ng A, et al. A rapid access chest pain clinic (RACPC): initial Australian experience. Heart Lung Circ 2018; 27: 1376‐1380.
- 7. Chew DP, French J, Briffa TG, et al. Acute coronary syndrome care across Australia and New Zealand: the SNAPSHOT ACS study. Med J Aust 2013; 199: 185‐191. https://www.mja.com.au/journal/2013/199/3/acute‐coronary‐syndrome‐care‐across‐australia‐and‐new‐zealand‐snapshot‐acs‐study
- 8. Richards MJ, Russo PL. Surveillance of hospital‐acquired infections in Australia — one nation, many states. J Hosp Infect 2007; 65: 174‐181.
- 9. Behnke M, Aghdassi SJ, Hansen S, et al. The prevalence of nosocomial infection and antibiotic use in German hospitals. Dtsch Arztebl Int 2017; 114: 851‐817.
- 10. World Health Organization. Prevention of hospital‐acquired infections: a practical guide, 2nd ed. Geneva: WHO, 2002. https://apps.who.int/iris/bitstream/handle/10665/67350/WHO_CDS_CSR_EPH_2002.12.pdf (viewed Jan 2023).
- 11. Bayley MD, Schwartz JS, Shofer FS, et al. The financial burden of emergency department congestion and hospital crowding for chest pain patients awaiting admission. Ann Emerg Med 2005; 45: 110‐117.
- 12. Goodacre S. View from the United Kingdom: chest pain center progress. Crit Pathw Cardiol 2005; 4: 131‐133.
- 13. Back L, Indraratna P, Kushwaha V. Early results of the Prince of Wales Hospital rapid access cardiology clinic (RACC). Heart Lung Circ 2019; 28: S295.
- 14. Black JA, Cheng K, Flood JA, et al. Evaluating the benefits of a rapid access chest pain clinic in Australia. Med J Aust 2019; 210: 321‐325. https://www.mja.com.au/journal/2019/210/7/evaluating‐benefits‐rapid‐access‐chest‐pain‐clinic‐australia#:~:text=Conclusions%3A%20Patients%20were%20evaluated%20more,adverse%20cardiovascular%20events%20were%20lower
- 15. Black JA, Campbell JA, Parker S, et al. Absolute risk assessment for guiding cardiovascular risk management in a chest pain clinic. Med J Aust 2021; 214: 266‐271. https://www.mja.com.au/journal/2021/214/6/absolute‐risk‐assessment‐guiding‐cardiovascular‐risk‐management‐chest‐pain
- 16. Klimis H, Thiagalingam A, Bartlett M, et al. Rapid access cardiology clinics (RACC) — assessing cardiovascular risk. Heart Lung Circ 2017; 26: S92.
- 17. Kozor R, Mooney J, Lowe H, et al. Rapid access chest pain clinics: an Australian cost‐benefit study. Heart Lung Circ 2022; 31: 177‐182.
- 18. Black JA, Lees C, Chapman N, et al. Telehealth rapid access chest pain clinic: initial experience during COVID‐19 pandemic. Telemed J E Health 2023; https://doi.org/10.1089/tmj.2022.0493 [Epub ahead of print].
- 19. Lembo RJ, Gullick J, Chow CK, et al. A study of patient satisfaction and uncertainty in a rapid access chest pain clinic. Heart Lung Circ 2020; 29: e210‐e216.
- 20. Magdy J, Kennedy M, Back L, Pitney M. Outcomes of the first 5 years of the Sutherland heart clinic chest pain clinic (CPC). Heart Lung Circ 2020; 29: S272.
- 21. McLachlan A, Aldridge C, Lee M, et al. The development and first six years of a nurse‐led chest pain clinic. N Z Med J 2019; 132: 39‐47.
- 22. Nkoane‐Kelaeng B, Lembo R, Figtree G, et al. Initial single centre experience implementing a rapid access chest pain clinic. Heart Lung Circ 2017; 26: S82.
- 23. Said C, Lennox‐Bradley W, Coote E, Mooney J. Real world review of an Australian outer‐metropolitan rapid access cardiology clinic (RACC). Heart Lung Circ 2020; 29: S279.
- 24. Yu C, Brazete S, Gullick J, et al. Long‐term outcomes following rapid access chest pain clinic assessment: first Australian data. Heart Lung Circ 2021; 30: 1309‐1313.
- 25. Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. Int J Cardiol 2013; 168: 2153‐2158.
- 26. Tenkorang JN, Fox KF, Collier TJ, Wood DA. A rapid access cardiology service for chest pain, heart failure and arrhythmias accurately diagnoses cardiac disease and identifies patients at high risk: a prospective cohort study. Heart 2006; 92: 1084‐1090.
- 27. Fox KF, Tenkorang J, Rogers A, Wood DA. Are rapid access cardiology clinics a valued part of a district cardiology service? Int J Cardiol 2009; 137: 42‐46.
- 28. Rajpura A, Sethi S, Taylor M. An evaluation of two rapid access chest pain clinics in central Lancashire, UK. J Eval Clin Pract 2007; 13: 326‐336.
- 29. Boyle RM. Value of rapid‐access chest pain clinics. Heart 2007; 93: 415‐416.
- 30. Ingram SJ, McKee G, Quirke MB, et al. Discharge of non–acute coronary syndrome chest pain patients from emergency care to an advanced nurse practitioner–led chest pain clinic: a cross‐sectional study of referral source and final diagnosis. J Cardiovasc Nurs 2017; 32: E1‐E8.
- 31. Taylor J, Kopanska A, Cobb T. Nurse‐led chest pain hot clinics: improving patient flow in the emergency department. Br J Card Nurs 2020; 15: 1‐11.
- 32. Lee AJ, Michail M, Quaderi SA, et al. Implementation of NICE Clinical Guideline 95 for assessment of stable chest pain in a rapid access chest pain clinic reduces the mean number of investigations and cost per patient. Open Heart 2015; 2: e000151.
- 33. Timmis A, Roobottom CA. National Institute for Health and Care Excellence updates the stable chest pain guideline with radical changes to the diagnostic paradigm. Heart 2017; 103: 982‐986.
- 34. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021; 78: e187‐e285.






Summary