The known: The COVID-19 pandemic has been associated with disruptions to many aspects of health care, possibly with adverse consequences for people with other conditions.
The new: The pre-pandemic decline in in-hospital mortality among people admitted to intensive care continued for people admitted with conditions other than COVID-19 until March 2021, at which point the survival gains of the preceding five years were reversed. Changes in mortality were not correlated with the number of people admitted to intensive care with COVID-19.
The implications: Increased in-hospital mortality among people admitted to ICUs without COVID-19 may reflect changes in health care across the Australian health system that need to be identified and rectified.
The coronavirus disease 2019 (COVID-19) pandemic had deleterious effects on hospital care for patients with other medical conditions.1,2,3 Intensive care units (ICUs) were particularly affected, as increased demand and resource limitations required altered service models, including redeploying less experienced staff members, reduced staff-to-patient ratios, and discharging patients to wards earlier than usual.4,5,6 These changes may have also affected the quality of care, leading, for example, to higher incidence of pressure injuries, drug errors, and delirium.7
After the Australian government declared a national state of emergency in March 2020, it introduced a range of measures to limit the impact of the COVID-19 pandemic. The initial measures were implemented across Australia, but states and territories subsequently diverged in their responses, resulting in different case numbers.
Prior to the COVID-19 pandemic, outcomes for ICU patients had been improving for several years.8,9 However, it is unclear whether the pandemic and associated responses affected outcomes for people admitted to Australian ICUs with conditions other than COVID-19. We therefore investigated whether mortality among these patients changed during the pandemic, as this information is important for developing future health care policies, including those for dealing with pandemics.
Methods
We undertook a national, multicentre, retrospective cohort study of all adults (16 years or older) admitted with conditions other than COVID-19 to Australian ICUs that contributed data to the Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcome and Resource Evaluation (CORE) registry (https://www.anzics.com.au/dev/centre-for-outcome-resource-evaluation) during 1 January 2016 – 30 June 2022. We excluded admissions for which the primary diagnosis was COVID-19 pneumonitis or a condition associated with suspected or actual SARS-CoV-2 infection according to Acute Physiology and Chronic Health Evaluation III (APACHE III-J) groupings. We also excluded admissions for palliative care or organ donation, re-admissions within a single hospital encounter, and admissions for which outcomes data or measures required for calculating the Australian and New Zealand Risk of Death (ANZROD) were unavailable.10 The study was conducted in accordance with Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)11 and Sex and Gender Equity in Research (SAGER) guidelines.12
Data extraction
We extracted data from the Adult Patient Database (APD), a binational dataset submitted to ANZICS CORE for quality benchmarking purposes; it includes de-identified demographic, clinical, and physiological parameter data for the first 24 hours after ICU admission to 97% of Australian ICUs.9 All submitted data undergo both site- and registry-level automated data validation and data quality audits. Data extraction was authorised by ANZICS CORE.
Statistical analysis
The pandemic period was defined as commencing on 1 March 2020 and data were grouped by calendar month. Continuous variables are reported as means with standard deviations (SDs) or medians with interquartile ranges (IQRs); the statistical significance of differences was assessed in t or Wilcoxon rank-sum tests as appropriate. Categorical variables are reported as proportions and the statistical significance of differences was assessed in ?2 tests.
The primary outcome was all-cause in-hospital mortality relative to the January 2016 value, expressed as an adjusted odds ratio (aOR) with 95% confidence interval (CI). Patient-level risk-adjusted mortality was assessed in a mixed effects logistic regression model adjusted for illness severity based on ANZROD and hospital type, with ICU as a random effect. The ANZROD, derived from locally collected data and components of the APACHE scoring system,10 predicts mortality for people admitted to Australian and New Zealand ICUs. Segmental regression analysis was employed to identify points of changes in mortality trends (breakpoints), presented as locally estimated scatterplot smoothing (LOESS) regression curves. Changes in mortality before and after breakpoints were assessed using linear regression.
Secondary outcomes were unadjusted ICU mortality, ICU length of stay, and hospital length of stay.
In subgroup analyses, we separately examined all-cause in-hospital mortality in states or territories where the numbers of people admitted to ICUs with COVID-19 during the pandemic were higher (Australian Capital Territory, New South Wales, Victoria) or lower (Northern Territory, Queensland, South Australia, Tasmania, Western Australia). Further subgroup analyses assessed the influence of patient age (< 65 years v = 65 years), ANZROD (< 2% v = 2%), and whether the ICU admission was a planned admission following elective surgery.
All analyses were performed in RStudio for Windows 2022.12 (Posit), using the tidyverse, zoo, and lubridate packages for data preparation, and segmented, lme4, and broom.mixed packages for segmented and mixed effect regression analysis.
Ethics approval
The study was approved by the Alfred Hospital Ethics Committee (87/22).
Results
Data were available for 1 101 725 admissions of people without COVID-19 to 186 ICUs during 2016–22, of which 950 489 met our inclusion criteria: 603 421 admissions during the pre-pandemic period (to 29 February 2020; 12 068 per month) and 347 068 during the pandemic period (12 395 per month) (Supporting information, figure 1).
The gender distribution, median age, and proportion of planned admissions after elective surgery were similar for the pre-pandemic and pandemic periods. The proportion of admissions including non-invasive ventilation was smaller during the pandemic period (9.3% v 11.9%), the proportions including renal replacement therapy (3.2% v 2.8%) or administration of inotropic or vasopressor drugs larger (31.6% v 26.6%). The proportion of admissions with respiratory disease was smaller during the pandemic than the pre-pandemic period (14.5% v 16.7%) (Box 1).
During the pandemic period, the median age of patients in states or territories with higher numbers of COVID-19-related ICU admissions was higher than in those with lower numbers (66.5 [IQR, 52.5–76.2] years v 65.1 [IQR, 50.6–74.9] years), as was the mean ANZROD (8% [SD, 0.15] v 7% [SD, 0.14]); the proportion of planned admissions after elective surgery was smaller (85 526, 39.6% v 62 490, 47.7%) (Supporting information, table 1).
Outcomes
During the pre-pandemic period, 41 278 people died in hospital (6.8%), and 22 249 (6.4%) during the pandemic period (pandemic v pre-pandemic: aOR, 0.91; 95% CI, 0.89–0.93). Time series analysis of mortality identified a gradual decline in both the unadjusted rate and the adjusted odds of mortality since 2018 until early 2021, at which point they rose, and they continued to do so after the number of COVID-19-related admissions declined (Box 2).
Segmental regression analysis identified a breakpoint in mortality trend in March 2021 (95% CI, October 2020 – July 2021). Time series regression analysis identified a 0.3% monthly decline in the adjusted odds of mortality from January 2016 to March 2021 (P < 0.001; March 2021 v January 2016: aOR, 0.70; 95% CI, 0.62–0.80), followed by a 1.4% monthly increase during March 2021 – June 2022 (P < 0.001; June 2022 v January 2016: aOR, 1.03; 95% CI, 0.90–1.17) (Box 2; Supporting information, table 2).
Subgroup analyses
In the states and territories with higher numbers of COVID-19-related ICU admissions, a breakpoint was identified in March 2021 (95% CI, November 2020 – July 2021). Time series regression analysis identified a 0.4% monthly decline in the adjusted odds of mortality during January 2016 – March 2021 (P < 0.001), followed by a 1.4% monthly increase during March 2021 – June 2022 (P < 0.001) (Box 3).
In states and territories with lower numbers of COVID-19-related ICU admissions, two breakpoints were identified: in July 2018 (95% CI, July 2017 – July 2018) and January 2021 (95% CI, April 2020 – October 2021). Time series regression analysis identified no significant monthly change in adjusted odds for mortality to July 2018 (P = 0.24), a 0.7% monthly decline during July 2018 – January 2021 (P = 0.007), and a 1.0% monthly increase from February 2021 (P = 0.015) (Box 3).
Rises in adjusted mortality during the COVID-19 pandemic were also noted for other subgroups. The pre-pandemic decline in mortality had been negligible for people under 65 years of age, but mortality increased during 2021 for both people under 65 and people aged 65 years or more (Supporting information, figure 2). The pre-pandemic decline and pandemic period increase in mortality were more marked for people with an ANZROD of 2% or more than for those with risk below 2% (Supporting information, figure 3) and for unplanned ICU admissions than planned admissions after elective surgery (Supporting information, figure 4).
Secondary outcomes
Unadjusted ICU mortality, ICU length of stay, and hospital length of stay were each similar during the pre-pandemic and pandemic periods (Box 4). Median ICU and hospital lengths of stay were not markedly different in the three jurisdictions with higher numbers of COVID-19-related ICU admissions, but the proportions of patients who died in intensive care (4.0% v 3.8%) or in hospital (6.7% v 5.9%) were larger (Supporting information, table 3).
Discussion
We found that the pre-pandemic decline in hospital mortality among ICU patients continued for people admitted to ICUs with conditions other than COVID-19 during the first year of the COVID-19 pandemic. However, in-hospital mortality rose from March 2021, even in states and territories where the numbers of COVID-19-related ICU admissions were relatively small, cancelling the improvement since January 2016. Further, the rise continued after the number of COVID-19-related ICU admissions declined in early 2022. The increase was particularly marked for people with unplanned ICU admissions or ANZROD of 2% or more.
The few studies of people admitted to ICUs without COVID-19 during the COVID-19 pandemic have consistently reported greater mortality correlated with the number of ICU patients admitted with COVID-19. In a multicentre study in Brazil, for example, adjusted mortality increased, time series analysis identifying a reversal of the pre-pandemic decline in mortality.13 A national registry-based study in India found that unadjusted mortality increased during the pandemic, and a notable increase in overall illness severity.14 In a single-centre, propensity score-matched study in Vienna, the rise in mortality among ICU patients without COVID-19 was not statistically significant, but the number of patients was relatively small.15 No comparable studies undertaken during the current period of very low COVID-19-related ICU admission numbers have been reported.
Our study provides a unique perspective on the systemic impact of the pandemic on a resource-rich health system with a high normal and surge ICU capacity16 that was relatively unchallenged by COVID-19 during most of the pandemic period.17 This situation enabled us to assess the impact of the pandemic beyond direct effects on the demand for physical resources.
Our findings suggest that pandemic-related changes in the delivery of care to ICU patients without COVID-19 were associated with a rise in mortality that persisted until at least the end of the study period (June 2022); that is, after the number of COVID-19-related ICU admissions had declined. We would expect that changes attributable to pandemic-induced system strain would be correlated with the number of COVID-19-related ICU admissions, but this was not the case. Our risk adjustment methods, which have been validated for an Australian population,10 also exclude changes in the demographic and illness severity of ICU patients as explanations for the increase in mortality.
Although the observational nature of our study limits conclusions about why mortality increased during the pandemic, the fact that the patterns of change were similar in states and territories where ICU admissions with COVID-19 were higher or lower suggests national changes in health care delivery. The more marked increases in mortality for patients with unplanned ICU admissions or more severe illness suggest that delivering timely acute care to patients with complex needs was more difficult during the pandemic. This interpretation is consistent with evidence that the pandemic has been associated with disruptions to a range of health care services, both overseas and in Australia, including reduced access to primary, hospital, and emergency care.18,19,20,21
Specific changes that may have contributed to increased mortality include system-level factors, such as the withdrawal of strain mitigation strategies (eg, staff redeployment), increased demand for ICU services, and changes in the availability of experienced staff following losses to burnout or leave.22,23 Unmeasured changes in disease epidemiology not fully accounted for by ANZROD and alterations in health care use patterns during the pandemic may also have contributed to poorer patient outcomes.24
Our findings highlight the need to evaluate elements of health service delivery that could underlie the increase in ICU patient mortality, particularly in acute and emergency care. Health system strain and staff shortages have been documented in the lay press, but the extent of these problems has not been systematically examined. Contemporaneous monitoring of system performance and patient outcomes across a range of health care settings and close monitoring of model performance in the context of changing system characteristics are needed.25
Limitations
Our time series analysis identified mortality changes that might have been masked in cross-sectional summary statistics by overall improvements in recent years. Our analysis of data from 97% of Australian ICUs before and during the COVID-19 pandemic, adjusted for patient risk using methods specific to and validated for the Australian population, delivers findings generalisable across Australia and to countries with similar health care systems and numbers of COVID-19 cases. However, causal relationships cannot be derived from a retrospective study based on observational data, and unidentified factors could have influenced mortality, although assuming that systemic changes related to the pandemic were dominant is reasonable in the absence of other known major shifts in ICU standards of treatment. Secondly, ANZICS APD data submission quality could have declined during periods of high demand, biasing the dataset, but various data quality checks indicate that comprehensive data submission was maintained. Thirdly, our study did not take into account people with disorders other than COVID-19 who were referred for but declined ICU admission, including people who would normally have been admitted to high dependency units but were instead admitted to wards because of capacity limitations. Fourthly, our study was limited to ICU services, a single component of the Australian health care system. Also examining outcomes for inpatients, for example, would provide a broader perspective of outcomes across the entire system and better inform decision-making.
Conclusion
Mortality among people admitted to Australian ICUs with conditions other than COVID-19, following a period of decline prior to the COVID-19 pandemic, began to rise in March 2021, reversing the accumulated improvements of the preceding five years. Its geographic and temporal characteristics suggest that a confluence of factors beyond the direct burden of COVID-19-related ICU admissions contributed to this reversal. National outcome monitoring programs and further investigation of changes in health care delivery and quality during the pandemic are needed.
Box 1 – Characteristics of 950 489 adults admitted to 186 Australian intensive care units (ICUs) for reasons other than COVID-19, January 2016 – June 2022
|
Characteristic |
Pre-pandemic period: 1 Jan 2016 – 29 Feb 2020 |
Pandemic period: 1 Mar 2020 – 30 June 2022 |
|||||||||||||
|
|
|||||||||||||||
|
Admissions |
603 421 |
347 068 |
|||||||||||||
|
Gender |
|
|
|||||||||||||
|
Women |
263 681 (43.7%) |
152 905 (44.1%) |
|||||||||||||
|
Men |
339 416 (56.2%) |
193 890 (55.9%) |
|||||||||||||
|
Other |
324 (0.1%) |
273 (0.1%) |
|||||||||||||
|
Age (years), median (IQR) |
66.0 (51.9–75.7) |
66.0 (51.8–75.7) |
|||||||||||||
|
Planned ICU admission after elective surgery |
263 184 (43.6%) |
149 237 (43.0%) |
|||||||||||||
|
APACHE II score, median (IQR) |
14.0 (10.0–18.0) |
14.0 (10.0–18.0) |
|||||||||||||
|
APACHE II score, mean (SD) |
14.8 (7.2) |
14.7 (7.1) |
|||||||||||||
|
APACHE III score, median (IQR) |
46.0 (34.0–61.0) |
46.0 (34.0–60.0) |
|||||||||||||
|
APACHE III score, mean (SD) |
49.8 (23.4) |
49.1 (22.8) |
|||||||||||||
|
ANZROD, median (IQR) |
0.02 (0.00–0.06) |
0.01 (0.00–0.06) |
|||||||||||||
|
ANZROD, mean (SD) |
0.07 (0.15) |
0.07 (0.15) |
|||||||||||||
|
Interventions (from 1 January 2018)* |
|
|
|||||||||||||
|
Extracorporeal membrane oxygenation |
476 (0.1%) |
527 (0.2%) |
|||||||||||||
|
Invasive ventilation |
90 205 (27.2%) |
94 501 (27.2%) |
|||||||||||||
|
Non-invasive ventilation |
31 285 (9.4%) |
28 530 (9.3%) |
|||||||||||||
|
Continuous renal replacement therapy |
9288 (2.8%) |
11 094 (3.2%) |
|||||||||||||
|
Inotropic or vasopressor agents |
88 162 (26.6%) |
109 693 (31.6%) |
|||||||||||||
|
Admission diagnostic category |
|
|
|||||||||||||
|
Gastrointestinal |
102 307 (19.3%) |
61 128 (20.2%) |
|||||||||||||
|
Respiratory |
88 770 (16.7%) |
43 976 (14.5%) |
|||||||||||||
|
Cardiac surgery |
81 538 (15.4%) |
45 433 (15.0%) |
|||||||||||||
|
Neurological |
77 395 (14.6%) |
46 157 (15.2%) |
|||||||||||||
|
Cardiovascular |
57 638 (10.9%) |
34 552 (11.4%) |
|||||||||||||
|
Sepsis |
42 030 (7.9%) |
23 884 (7.9%) |
|||||||||||||
|
Metabolic |
38 910 (7.3%) |
23 783 (7.9%) |
|||||||||||||
|
Trauma |
26 044 (4.9%) |
15 921 (5.3%) |
|||||||||||||
|
Renal |
8112 (1.5%) |
4729 (1.6%) |
|||||||||||||
|
Other |
7308 (1.4%) |
3250 (1.1%) |
|||||||||||||
|
|
|||||||||||||||
|
ANZROD = Australian and New Zealand Risk of Death; APACHE = Acute Physiology and Chronic Health Evaluation; COVID-19 = coronavirus disease 2019. * The denominator for the pre-pandemic period is 331 848. |
|||||||||||||||
Box 2 – Adults admitted to 186 Australian intensive care units (ICUs) for reasons other than COVID-19, January 2016 – June 2022: unadjusted monthly mortality and adjusted odds ratios with 95% confidence intervals (reference: January 2016)*
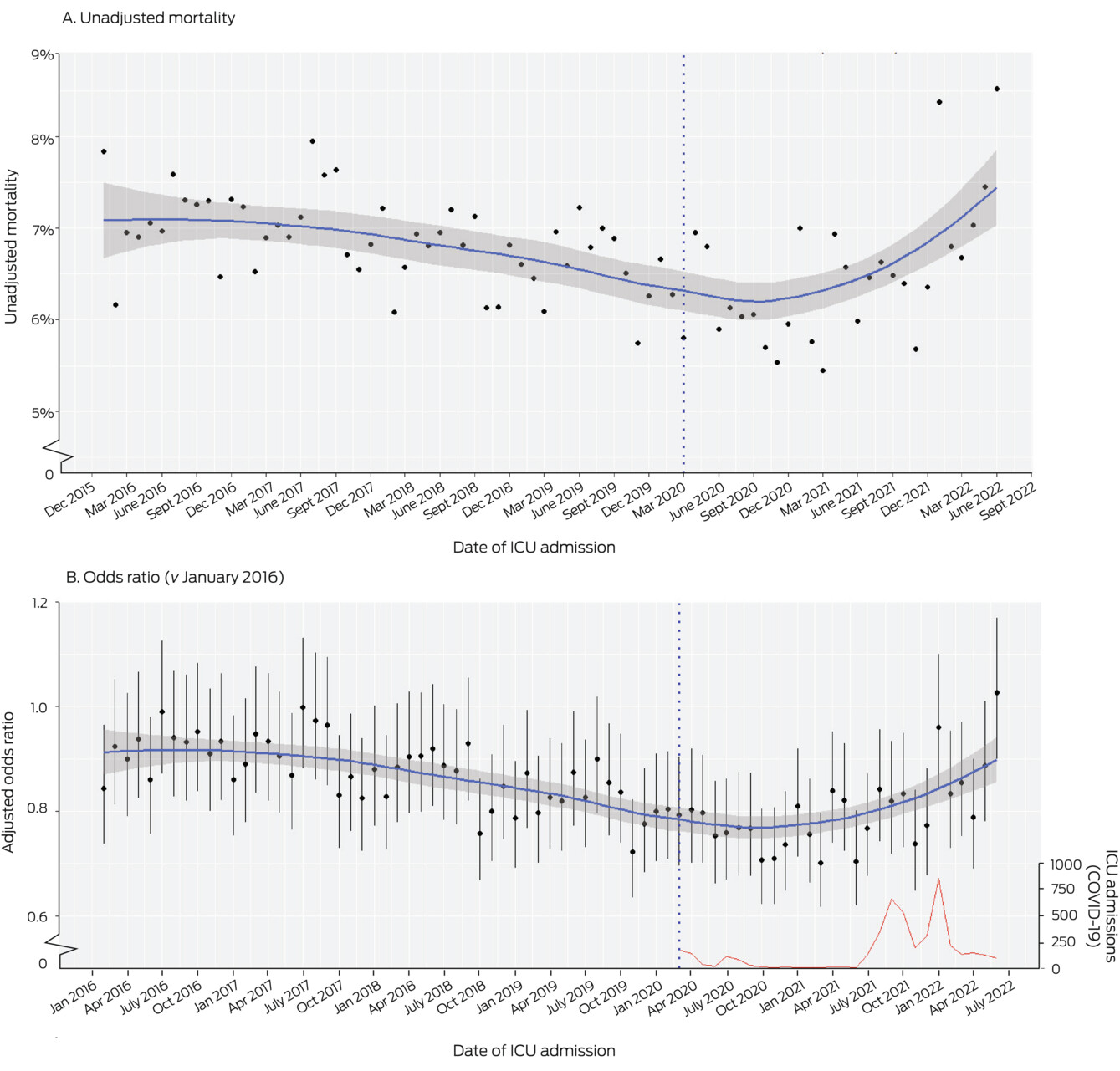
COVID-19 = coronavirus disease 2019.* Blue curves: locally estimated scatterplot smoothing (LOESS) curves; red curves: monthly ICU admissions of people with COVID-19 (suspected or confirmed); vertical dotted line: beginning of pandemic period.
Box 3 – Adults admitted to 186 Australian intensive care units (ICUs) for reasons other than COVID-19, January 2016 – June 2022, for states/territories with higher or lower numbers of COVID-19-related ICU admissions: adjusted odds ratios with 95% confidence intervals (reference: January 2016)*
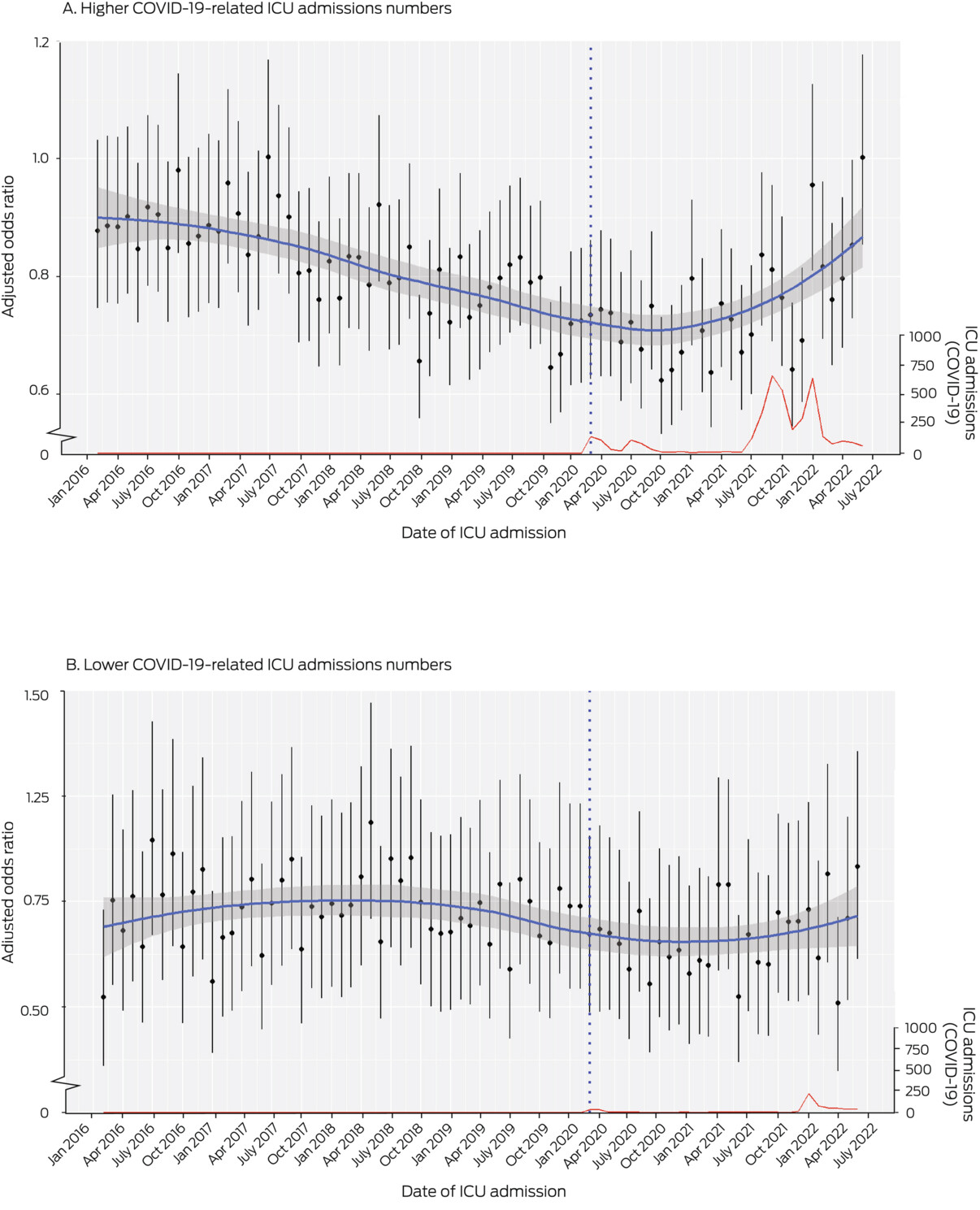
* Blue curves: locally estimated scatterplot smoothing (LOESS) curves; red curves: monthly ICU admissions of people with COVID-19 (suspected or confirmed); vertical dotted line: beginning of pandemic period. Higher COVID-19-related ICU admission numbers: Australian Capital Territory, New South Wales, Victoria; lower COVID-19-related ICU admission numbers: Northern Territory, Queensland, South Australia, Tasmania, Western Australia.
Box 4 – Unadjusted outcomes for adults admitted to 186 Australian intensive care units for reasons other than COVID-19, January 2016 – June 2022
|
Outcomes |
Pre-pandemic period: 1 Jan 2016 – 29 Feb 2020 |
Pandemic period: 1 Mar 2020 – 30 June 2022 |
|||||||||||||
|
|
|||||||||||||||
|
Admissions |
603 421 |
347 068 |
|||||||||||||
|
Intensive care unit stay |
|
|
|||||||||||||
|
Length (hours), median (IQR) |
40.6 (21.7–72.6) |
40.4 (21.7–72.6) |
|||||||||||||
|
Deaths in ICU |
25 364 (4.2%) |
13 602 (3.9%) |
|||||||||||||
|
Hospital stay |
|
|
|||||||||||||
|
Length (days), median (IQR) |
7.9 (4.2–14.1) |
7.6 (4.1–13.8) |
|||||||||||||
|
Deaths in hospital |
41 278 (6.8%) |
22 249 (6.4%) |
|||||||||||||
|
|
|||||||||||||||
|
COVID-19 = coronavirus disease 2019; IQR = interquartile range. |
|||||||||||||||
Received 4 November 2022, accepted 27 March 2023
- Sing Chee Tan1,2
- Tess Evans3
- Matthew L Durie4
- Paul J Secombe5,6
- David Pilcher7,8
- 1 Northern Hospital Epping, Melbourne, VIC
- 2 The University of Melbourne, Melbourne, VIC
- 3 Fiona Stanley Hospital, Perth, WA
- 4 Melbourne Health, Melbourne, VIC
- 5 Alice Springs Hospital, Alice Springs, NT
- 6 Monash University, Melbourne, VIC
- 7 The Alfred Hospital, Melbourne, VIC
- 8 Centre for Outcome and Resource Evaluation Australian and New Zealand Intensive Care Society, Melbourne, VIC
Open access:
Open access publishing facilitated by The University of Melbourne, as part of the Wiley ‐ The University of Melbourne agreement via the Council of Australian University Librarians.
We thank the Australia New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE) for providing the data we analysed. The authors and the management committees of ANZICS CORE also thank the clinicians, data collectors, and researchers at the contributing sites.
No relevant disclosures.
- 1. Riley B, Packer M, Gallier S, et al. Acute, non‐COVID related medical admissions during the first wave of COVID‐19: A retrospective comparison of changing patterns of disease. Acute Med 2020; 19: 176‐182.
- 2. Chan DZ, Stewart RA, Kerr AJ, et al. The impact of a national COVID‐19 lockdown on acute coronary syndrome hospitalisations in New Zealand. Lancet Reg Health West Pac 2020; 5: 100056.
- 3. Corrigan C, Duke G, Millar J, et al; Australian and New Zealand Intensive Care Society Pediatric Study Group; ANZICS Center for Outcome and Resource Evaluation. Admissions of children and adolescents with deliberate self‐harm to intensive care during the SARS‐COV‐2 outbreak in Australia. JAMA Netw Open 2022; 5: e2211692.
- 4. Fjølner J, Haaland ØA, Jung C, et al. Who gets the ventilator? A multicentre survey of intensivists’ opinions of triage during the first wave of the COVID‐19 pandemic. Acta Anaesthesiol Scand 2022; 66: 859‐868.
- 5. Vidal‐Cortés P, Martín MC, Díaz E, et al. Impact of one year of pandemic on Spanish Intensive Care Units. Rev Esp Quimioter 2022; 35: 392‐400.
- 6. Topple M, Jaspers R, Watterson J, et al. Nursing workforce deployment and intensive care unit strain during the COVID‐19 pandemic in Victoria, Australia. Aust Crit Care 2022; 36: 84‐91.
- 7. Rewa OG, Stelfox HT, Ingolfsson A, et al. Indicators of intensive care unit capacity strain: a systematic review. Crit Care 2018; 22: 86.
- 8. Kaukonen KM, Bailey M, Suzuki S, et al. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA 2014; 311: 1308‐1316.
- 9. Australian and New Zealand Intensive Care Society. ANZICS Centre for Outcomes and Resource Evaluation: 2019 annual report. Melbourne, 2020. https://www.anzics.com.au/wp‐content/uploads/2020/11/2019‐CORE‐Report.pdf (viewed Sept 2022).
- 10. Paul E, Bailey M, Kasza J, Pilcher D. The ANZROD model: better benchmarking of ICU outcomes and detection of outliers. Crit Care Resusc 2016; 18: 25‐36.
- 11. von Elm E, Altman DG, Egger M, et al; STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806.
- 12. Heidari S, Babor TF, De Castro P, et al. Sex and Gender Equity in Research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev 2016; 1: 2.
- 13. Zampieri FG, Bastos LSL, Soares M, et al. The association of the COVID‐19 pandemic and short‐term outcomes of non‐COVID‐19 critically ill patients: an observational cohort study in Brazilian ICUs. Intensive Care Med 2021; 47: 1440‐1449.
- 14. Indian Registry of IntenSive care (IRIS); Kj Adhikari N, Beane A, Devaprasad D, et al. Impact of COVID‐19 on non‐COVID intensive care unit service utilization, case mix and outcomes: a registry‐based analysis from India. Wellcome Open Res 2021; 6: 159.
- 15. Bologheanu R, Maleczek M, Laxar D, Kimberger O. Outcomes of non‐COVID‐19 critically ill patients during the COVID‐19 pandemic : a retrospective propensity score‐matched analysis. Wien Klin Wochenschr 2021; 133: 942‐950.
- 16. Litton E, Bucci T, Chavan S, et al. Surge capacity of Australian intensive care units associated with COVID‐19 admissions. Med J Aust 2020; 212: 463‐467. https://www.mja.com.au/journal/2020/212/10/surge‐capacity‐intensive‐care‐units‐case‐acute‐increase‐demand‐caused‐covid‐19
- 17. Begum H, Neto AS, Alliegro P, et al. People in intensive care with COVID‐19: demographic and clinical features during the first, second, and third pandemic waves in Australia. Med J Aust 2022; 217: 352‐360. https://www.mja.com.au/journal/2022/217/7/people‐intensive‐care‐covid‐19‐demographic‐and‐clinical‐features‐during‐first
- 18. Mogharab V, Ostovar M, Ruszkowski J, et al. Global burden of the COVID‐19 associated patient‐related delay in emergency healthcare: a panel of systematic review and meta‐analyses. Glob Health 2022; 18: 58.
- 19. Tan SC, Cross A, Ghosh A. Impact of lockdowns on critical care service demand in a metropolitan hospital in Melbourne, Australia. Emerg Med Australas 2022; 34: 52‐57.
- 20. Halcomb E, Fernandez R, Ashley C, et al. The impact of COVID‐19 on primary health care delivery in Australia. J Adv Nurs 2022; 78: 1327‐1336.
- 21. Sutherland K, Chessman J, Zhao J, et al. Impact of COVID‐19 on healthcare activity in NSW, Australia. Public Health Res Pract 2020; 30: 3042030.
- 22. Mannix K. The future of Australia's nursing workforce: COVID‐19 and burnout among nurses. University of Melbourne, Dec 2021. https://www.unimelb.edu.au/__data/assets/pdf_file/0004/4085194/katelyn_mannix_report.pdf (viewed Sept 2022).
- 23. Litton E, Huckson S, Chavan S, et al. Increasing ICU capacity to accommodate higher demand during the COVID‐19 pandemic. Med J Aust 2021; 215: 513‐517. https://www.mja.com.au/journal/2021/215/11/increasing‐icu‐capacity‐accommodate‐higher‐demand‐during‐covid‐19‐pandemic
- 24. Lyall MJ, Lone NI. Higher clinical acuity and 7‐day hospital mortality in non‐COVID‐19 acute medical admissions: prospective observational study. Emerg Med J 2021; 38: 366‐370.
- 25. Pilcher D, Coatsworth NR, Rosenow M, McClure J. A national system for monitoring intensive care unit demand and capacity: the Critical Health Resources Information System (CHRIS). Med J Aust 2021; 214: 297‐298. https://www.mja.com.au/journal/2021/214/7/national‐system‐monitoring‐intensive‐care‐unit‐demand‐and‐capacity‐critical






Abstract
Objective: To investigate in‐hospital mortality among people admitted to Australian intensive care units (ICUs) with conditions other than coronavirus disease 2019 (COVID‐19) during the COVID‐19 pandemic.
Design: National, multicentre, retrospective cohort study; analysis of data in the Australian and New Zealand Intensive Care Society Centre for Outcome and Resource Evaluation (ANZICS CORE) Adult Patient Database.
Setting, participants: Adults (16 years or older) without COVID‐19 admitted to Australian ICUs, 1 January 2016 – 30 June 2022.
Main outcome measures: All‐cause in‐hospital mortality, unadjusted and relative to the January 2016 value, adjusted for illness severity (Australian and New Zealand Risk of Death [ANZROD] and hospital type), with ICU as a random effect. Points of change in mortality trends (breakpoints) were identified by segmental regression analysis.
Results: Data for 950 489 eligible admissions to 186 ICUs were available. In‐hospital mortality declined steadily from January 2016 to March 2021 by 0.3% per month (P < 0.001; March 2021 v January 2016: adjusted odds ratio [aOR], 0.70; 95% confidence interval [CI], 0.62–0.80), but rose by 1.4% per month during March 2021 – June 2022 (P < 0.001; June 2022 v January 2016: aOR, 1.03; 95% CI, 0.90–1.17). The rise in mortality continued after the number of COVID‐19‐related ICU admissions had declined; mortality increased in jurisdictions with lower as well as in those with higher numbers of COVID‐19‐related ICU admissions.
Conclusion: The rise in in‐hospital mortality among people admitted to Australian ICUs with conditions other than COVID‐19 from March 2021 reversed the improvement of the preceding five years. Changes to health service delivery during the pandemic and their consequences should be investigated further.