The known: The capability of Australian intensive care units (ICUs) to respond to the expected increase in demand associated with COVID‐19 is unknown.
The new: A survey of ICU directors found that intensive care bed capacity could be increased by as much as 191%, but invasive ventilator numbers by only 120%, and the surge would also require large numbers of additional senior medical and nursing staff (250% increase).
The implications: Assuring intensive care bed surge capability will require increases in the numbers of invasive ventilators, as well as in clinical and, in particular, nursing staff levels. New staffing models and strategies for reducing local variability in surge capability are urgently needed.
The burden on health care resources associated with the coronavirus disease 2019 (COVID‐19) pandemic is unparalleled in recent times. The early experience in severely affected countries is that 5–16% of patients with laboratory‐confirmed COVID‐19 require admission to intensive care units (ICUs).1,2
While public health measures that limit virus transmission are the primary means for reducing the disease burden and the need for ICU care, Australian and New Zealand Intensive Care Society (ANZICS) guidelines recommend that ICUs have coordinated local and regional staged surge plans for responding to increased demand.3
The primary aim of our study was to assess the intensive care bed and invasive ventilation surge capability in Australia. A secondary aim was to describe variation in surge capability by ICU type (tertiary, metropolitan, regional/rural, private) and jurisdiction, as well as surge capability with respect to other ICU equipment and clinical and nursing staffing levels.
Methods
Data were primarily obtained from the ANZICS Critical Care Resources (CCR) registry. We analysed unpublished data extracted from the ANZICS CCR 2018–19 survey or, when these were not available, from the 2017–18 CCR report,4 including baseline number of available beds for all ICUs in Australia, workforce data (numbers of senior medical staff and nursing staff), and numbers of elective surgery, mechanical ventilation, and total ICU bed‐days.
The ANZICS CCR data were supplemented by data from a survey of ICU surge capacity distributed to all ICU directors in Australia (Supporting Information, table 1). The survey was designed by the study investigators, with feedback from other critical care clinicians and health policy makers, with the aim of obtaining information on local, jurisdictional, and national critical care capacity. The survey included questions on the baseline number of available ICU beds, and on the incremental capacity to increase ICU bed numbers with additional physical ICU beds not staffed or operational during baseline activity, surge beds already configured to ICU standards, and other beds that could be rapidly converted to meet the minimal standards required for intensive care.5 The survey also included questions about equipment for invasive mechanical ventilation (standard ICU ventilators and other ventilators, including transport ventilators, anaesthetic machine ventilators, and non‐invasive ventilators capable of providing invasive ventilation), dialysis machines, extracorporeal membrane oxygenation (ECMO) machines, and intravenous infusion pumps, as well as about staffing numbers (senior doctors, defined as consultants working in ICUs, and ICU‐registered nursing staff).
The survey was distributed by email (ANZICS registries mailing list) during 13–24 March 2020. The ICU director or, if they were unavailable, the nurse unit manager could complete and return the survey online, or by email as a Microsoft Word document. Non‐responding ICUs were followed up twice by email. Responses were collated in a spreadsheet by ANZICS Centre for Outcome and Resource Evaluation (CORE) staff. With the assistance of the Australasian Veterinary Boards Council, each state veterinary board also surveyed the superintendents of veterinary hospitals about the models, numbers, and locations of all machines capable of invasive ventilation in their facilities.
Data were collated and analysed in Excel (Microsoft) and summarised as descriptive statistics: parametric variables as means and standard deviations (SDs), non‐parametric variables as medians and interquartile ranges (IQRs). The incremental increase in ICU bed capacity for each surge level was compared with the available number of ventilators, and the results reported both as mean (with SDs) and median values (with IQRs).
To estimate the number of additional staff required by a surge, we extrapolated ANZICS CCR data from the respondent ICUs to all 2378 available Australian ICU beds, providing estimated baseline numbers of senior medical and registered nursing staff. For senior medical staff, the best case estimate assumed that absenteeism did not increase and that the need for additional staffing could be reduced by 20% in the short term by increasing the available clinical full‐time equivalent (FTE) staff level by reducing leave, increasing the work hours of part‐time employees, and by temporarily delegating certain roles outside the ICU to ward staff (eg, follow‐up clinics, tracheostomy, and total parenteral nutrition rounds). Conversely, worst case estimates assumed no increase in the work hours of existing staff and that a 30% increase in staff numbers would be required to compensate absenteeism. The worst case estimate for nursing staff included a further 10% increase to account for the proportion of patients receiving mechanical ventilation (requiring one‐to‐one nursing care) increasing from 50% to 70% under pandemic conditions.
Ethics approval
The study was approved by the Central Australian Human Research Ethics Committee (reference, CAHREC‐20‐3687).
Results
Physical intensive care beds
A total of 191 ICUs in Australia (119 public and 72 private) are recorded in the ANZICS CCR database, with 2378 ICU beds available during baseline activity, or 9.3 ICU beds per 100 000 population. Responses to the surge survey were received from 175 ICUs (92%) with 2228 available beds (94% of all available ICU beds), including all tertiary ICUs (Box 1; Supporting Information, table 2).
The 175 respondent ICUs had access to a total of 4258 additional physical intensive care beds, surge beds outside the ICU configured according to intensive care standards, and other beds that could be rapidly converted to meet the minimal requirements of intensive care, almost tripling intensive care bed capacity (191% increase) (Box 2). The estimated total number of surge beds for all Australian ICUs, extrapolated from the 191% increase for respondent ICUs, was 6923 (Box 3, Box 4), or 27.2 ICU beds per 100 000 population.
Ventilators
The 175 respondent sites have 2184 standard ICU invasive ventilators. During a surge, the number of units could be increased by 2631 units (120% increase), comprising 532 other ICU ventilators (including transport ventilators), 1476 anaesthetic machine ventilators, and 471 non‐invasive ventilators capable of invasive ventilation. That is, at higher surge levels there will be fewer available ventilators than intensive care beds: 2631 extra ventilators for the 4259 extra beds (61%) (Box 5; ventilator numbers and ventilators per bed by ICU category and jurisdiction: Supporting Information, tables 3–5).
Ventilators in veterinary facilities
A total of 188 invasive ventilators were identified in 120 Australian veterinary facilities (147 in metropolitan areas, 41 in rural or regional areas; Supporting Information, table 6), of which 179 were human model ventilators.
Other intensive care equipment
The availability of other equipment (renal replacement therapy machines, ECMO equipment, intravenous infusion pumps) is reported in the Supporting Information, tables 7–9.
Staffing levels
Based on data for the 175 respondent ICUs, the maximal surge would require an additional 2623–4092 senior medical staff and an additional 24 895–42 720 registered nursing staff (157–269% increase on baseline staffing) across all 191 ICUs (Box 6).
Elective surgery
In the 157 ICUs for which annual elective surgery data were available in the ANZICS CCR, elective surgery accounted for 62 340 ICU admissions (38% of all ICU admissions) and 2 801 310 ICU bed‐days (25% of all ICU bed‐days). Elective surgery accounts for a substantially greater proportion of ICU admissions to tertiary than to other public ICU types (Supporting Information, table 10).
Discussion
The 191 ICUs in Australia provide 2378 intensive care beds during baseline activity (9.3 per 100 000 population). The 175 ICUs that responded to our surge survey reported they could increase their intensive care physical bed capacity by a total of 4258 beds (191% increase, corresponding to 6923 extra beds across all Australian ICUs), and invasive mechanical ventilation capacity by 2631 machines (120% increase).
Baseline ICU bed numbers per capita are substantially lower in China (3.6 per 100 000) and the United Kingdom (6.6 per 100 000 population), but higher in the United States (25.8 per 100 000 population).6,7 Our survey indicates that the physical bed capacity of intensive care could be substantially increased in Australia during a surge, to 27.2 beds per 100 000 population on the basis of added beds at the respondent sites alone. This capability, compared with the remarkable but lower immediate surge capacity demonstrated in the Lombardy in northern Italy — where an additional 482 ICU beds were made available over an 18‐day period (from a baseline of 720 ICU beds) in response to the unexpectedly high number of acute presentations with COVID‐192 — highlights the value of the longer time available for planning in Australia. International comparisons are, of course, complex and require consideration of additional factors, including access to suitably trained specialists and the possibility of deferring elective surgery. Intensive care specialists are available in nearly all Australian ICUs, but only in 48% of US acute care hospitals.8,9 Our data also indicate that tertiary ICUs have substantially greater capacity than metropolitan or rural and regional ICUs to make beds available for increased numbers of unplanned admissions by cancelling elective surgery.
Our study provides further important information. First, staffing is required for additional ICU beds. Even in the best case scenario, the staffing requirements associated with maximal surge intensive care bed capacity are extremely high. This applies in particular to the increased demand for nursing staff, as a bedside nurse is required for each additional surge patient receiving mechanical ventilation. Strategies and resources for rapidly preparing registered nurses to manage mechanically ventilated patients are urgently required. Similarly, senior ICU doctors may be required to act as supervisors for several groups of patients, assisted by other senior clinicians with overlapping skill sets, such as anaesthetists, in order to maintain safe patient‐to‐physician ratios. The optimal modifications of standard ICU staffing models during a surge will differ between sites and according to local capabilities. Their impacts on resource use and patient outcomes are uncertain and will require investigation.
Second, cross‐disciplinary collaboration allowed identification of additional ventilators in veterinary hospitals, most of which were models already used in Australian ICUs. With appropriate preparation, the risk associated with using these ventilators would be lower than for ventilators not normally used in ICUs or equipment unfamiliar to critical care staff. In addition, the veterinary sector may also provide additional physical capacity, pharmaceutical resources, and staff who could assist with intensive care.
Finally, our survey found substantial differences by ICU category and jurisdiction. Surge capability is relatively limited for paediatric ICUs; it is greater for rural and regional ICUs than for metropolitan ICUs, but much lower than for private and tertiary ICUs. Rural and regional ICUs have high proportions of vulnerable patients and rely on inter‐hospital transfer systems that may be overwhelmed in a crisis.10 It is unlikely that patients with COVID‐19 would be transferred interstate, but we found that equipment and staffing levels may be rate‐limiting factors. Establishing national, real time monitoring of ICU bed capacity could facilitate the rapid redeployment of resources to areas of need.
Limitations
The response rate to our surge survey (92%, including all tertiary ICUs) means that our results are probably nationally representative. However, surge capability in our study reflected the numbers of beds identified by respondents at the time of the survey. The reported capacity for an institution may not be accurate. Equally importantly, further beds could potentially be made available over time, and additional facilities explored for managing urgent elective surgical ICU and other critical care admissions. Estimation of invasive ventilator capacity did not include state, federal, or Australian Defence Force stores stockpiled to assist with disaster response, or health care facilities without ICUs.
Conclusion
The directors of Australian ICUs report that overall intensive care physical bed capacity could be near tripled in response to the increased demand caused by the COVID‐19 pandemic. However, maximal surge would require a potential shortfall in invasive ventilators to be remedied, and would also require a large increase in senior clinician and nursing staff numbers. The potential for increasing capacity differs by jurisdiction, and is greatest in tertiary ICUs.
Box 1 – Characteristics of intensive care units that responded to the surge survey
|
|
Total |
Tertiary |
Metropolitan |
Rural/regional |
Private |
Paediatric |
|||||||||
|
|
|||||||||||||||
|
Survey respondents |
175/191 (92%) |
35/35 (100%) |
31/32 (97%) |
36/43 (84%) |
65/72 (90%) |
8/9 (89%) |
|||||||||
|
Admissions per year, mean (SD) |
1058 (744) |
1914 (905) |
770 (428) |
773 (404) |
896 (597) |
1031 (614) |
|||||||||
|
Bed‐days per year, mean (SD) |
3118 (3001) |
6825 (4045) |
2322 (2475) |
2113 (1427) |
1932 (1381) |
4146 (3039) |
|||||||||
|
Mechanical ventilation days per year, mean (SD) |
752 (1204) |
2188 (1677) |
550 (492) |
367 (540) |
195 (246) |
1509 (1270) |
|||||||||
|
|
|||||||||||||||
|
SD = standard deviation |
|||||||||||||||
Box 2 – Intensive care unit (ICU) bed capacity of the 175 surge survey respondent units, by category and jurisdiction
|
|
|
Numbers of ICU beds available |
|
||||||||||||
|
Currently available ICU beds |
Additional physical beds |
Additional bed spaces outside ICU |
Other surge beds |
Total surge beds |
Total beds available |
||||||||||
|
|
|||||||||||||||
|
Category |
|
|
|
|
|
|
|||||||||
|
Tertiary |
799 |
257 |
711 |
380 |
1348 |
2147 |
|||||||||
|
Metropolitan |
285 |
127 |
321 |
114 |
562 |
847 |
|||||||||
|
Rural/regional |
291 |
105 |
398 |
270 |
773 |
1064 |
|||||||||
|
Private |
725 |
58 |
947 |
436 |
1441 |
2166 |
|||||||||
|
Paediatric |
128 |
40 |
46 |
48 |
134 |
262 |
|||||||||
|
Jurisdiction |
|
|
|
|
|
|
|||||||||
|
Australian Capital Territory |
52 |
17 |
67 |
95 |
179 |
231 |
|||||||||
|
New South Wales |
854 |
179 |
1034 |
512 |
1725 |
2579 |
|||||||||
|
Northern Territory |
24 |
4 |
9 |
10 |
23 |
47 |
|||||||||
|
Queensland |
376 |
154 |
262 |
99 |
515 |
891 |
|||||||||
|
South Australia |
193 |
41 |
93 |
21 |
155 |
348 |
|||||||||
|
Tasmania |
51 |
12 |
60 |
41 |
113 |
164 |
|||||||||
|
Victoria |
499 |
149 |
666 |
351 |
1166 |
1665 |
|||||||||
|
Western Australia |
179 |
31 |
232 |
119 |
382 |
561 |
|||||||||
|
Total |
2228 |
587 |
2423 |
1248 |
4258 |
6486 |
|||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 3 – Intensive care unit (ICU) bed capacity in Australia, by category*
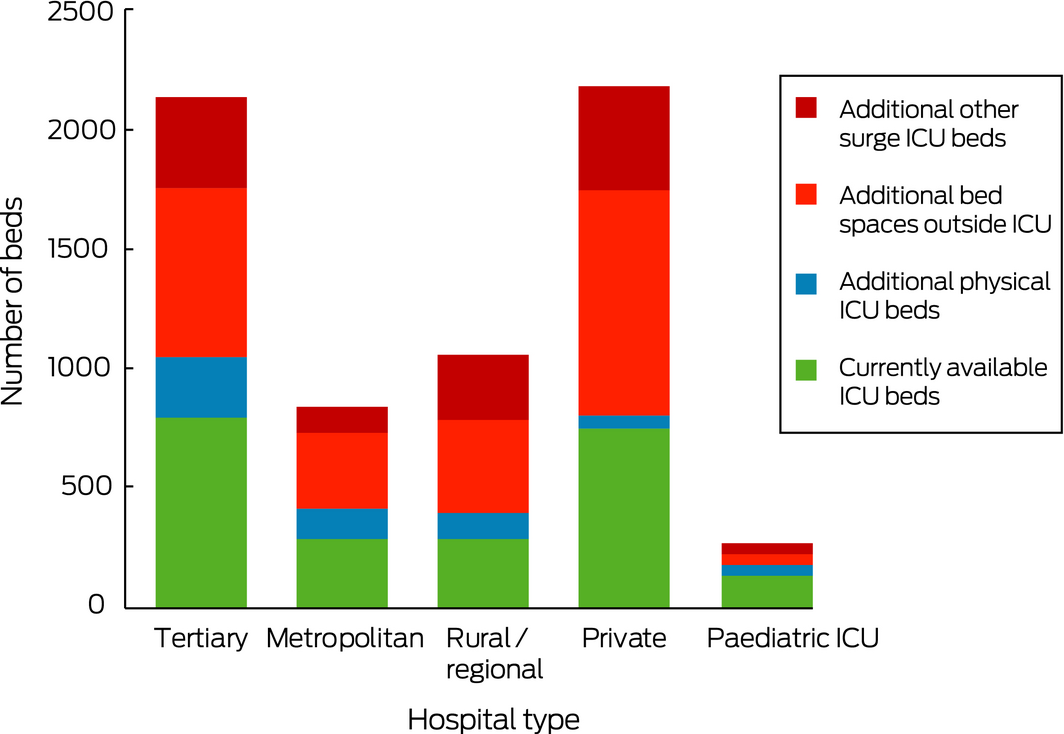
* Baseline (currently available) beds at all 191 ICUs and surge beds at 175 respondent ICUs.
Box 4 – Intensive care unit (ICU) beds per 100 000 population, by jurisdiction*
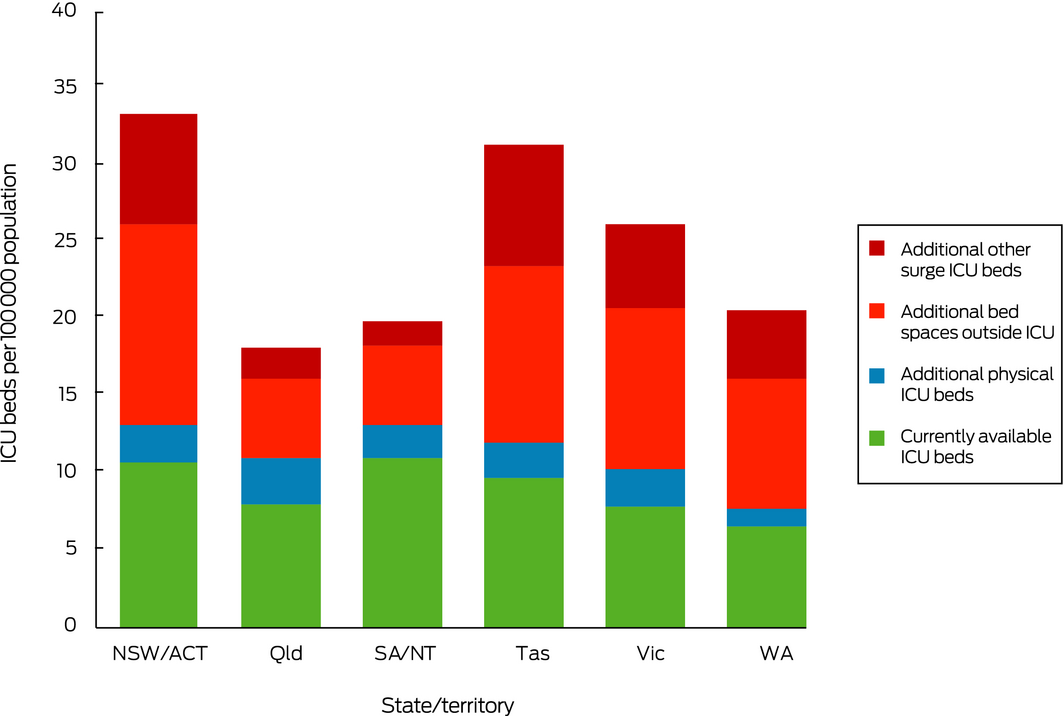
* Baseline (currently available) beds at all 191 ICUs and surge beds at 175 respondent ICUs.
Box 5 – Available ventilators per bed at the 175 respondent surge survey intensive care units (ICUs)
|
|
|
Ventilators per bed |
|||||||||||||
|
Number of ventilators |
ICU beds |
ICU beds + additional physical beds |
ICU beds + additional physical beds + bed spaces outside ICU |
ICU beds + additional physical beds + bed spaces outside ICU + others |
|||||||||||
|
|
|||||||||||||||
|
Total number of beds |
|
2228 |
2815 |
5238 |
6486 |
||||||||||
|
Standard ICU ventilators |
2184 |
|
|
|
|
||||||||||
|
Mean (SD) |
|
1.0 (0.7) |
0.8 (0.4) |
0.4 (0.3) |
0.3 (0.3) |
||||||||||
|
Median (IQR) |
|
0.9 (0.5–1.1) |
0.6 (0.4–0.9) |
0.4 (0.2–0.6) |
0.3 (0.2–0.5) |
||||||||||
|
Standard ICU ventilators+ other ICU ventilators |
2716 |
|
|
|
|
||||||||||
|
Mean (SD) |
|
1.2 (0.8) |
1.0 (0.4) |
0.5 (0.3) |
0.4 (0.3) |
||||||||||
|
Median (IQR) |
|
1.0 (0.7–1.4) |
0.8 (0.6–1.1) |
0.5 (0.3–0.7) |
0.4 (0.2–0.6) |
||||||||||
|
Standard ICU ventilators + other ICU ventilators + anaesthetic machine ventilators |
4192 |
|
|
|
|
||||||||||
|
Mean (SD) |
|
1.9 (1.3) |
1.5 (0.7) |
0.8 (0.4) |
0.6 (0.4) |
||||||||||
|
Median (IQR) |
|
1.7 (1.2–2.2) |
1.4 (1.0–1.8) |
0.8 (0.5–1.0) |
0.6 (0.4–0.9) |
||||||||||
|
Standard ICU ventilators + other ICU ventilators + anaesthetic machine ventilators + non‐invasive ventilators |
4663 |
|
|
|
|
||||||||||
|
Mean (SD) |
|
2.1 (1.5) |
1.7 (0.8) |
0.9 (0.5) |
0.7 (0.5) |
||||||||||
|
Median (IQR) |
|
1.9 (1.4–2.5) |
1.5 (1.1–2.0) |
0.8 (0.6–1.1) |
0.7 (0.5–1.0) |
||||||||||
|
Standard ICU ventilators + other ICU ventilators + anaesthetic machine ventilators + non‐invasive ventilators + other non‐ICU ventilators |
4815 |
|
|
|
|
||||||||||
|
Mean (SD) |
|
2.2 (1.6) |
1.7 (0.9) |
0.9 (0.5) |
0.7 (0.5) |
||||||||||
|
Median (IQR) |
|
1.9 (1.4–2.7) |
1.5 (1.1–2.1) |
0.9 (0.6–1.1) |
0.7 (0.5–1.0) |
||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range; SD = standard deviation. Bold: mean or median ventilator‐too‐bed ratio below 1.0. |
|||||||||||||||
Box 6 – Estimated numbers of additional intensive care staff required by surge level (all Australian intensive care units)
|
|
Surge level (beds required) |
||||||||||||||
|
Additional physical ICU beds |
Additional physical beds and bed spaces outside ICU |
All identified surge beds |
|||||||||||||
|
|
|||||||||||||||
|
Additional senior medical staff required (baseline number: 1671*) |
|
|
|
||||||||||||
|
Best case (increase from baseline staffing) |
363 (22%) |
1856 (111%) |
2623 (157%) |
||||||||||||
|
Worst case (increase from baseline staffing) |
568 (34%) |
2896 (173%) |
4092 (245%) |
||||||||||||
|
Additional registered nurses required (baseline number: 15 857*) |
|
|
|
||||||||||||
|
Best case (increase from baseline staffing) |
3449 (22%) |
17 614 (111%) |
24 895 (157%) |
||||||||||||
|
Worst case (increase from baseline staffing) |
5918 (37%) |
30 158 (190%) |
42 720 (269%) |
||||||||||||
|
|
|||||||||||||||
|
* Estimated by extrapolating Australian and New Zealand Intensive Care Society Critical Care Resources registry data for the respondent ICUs to all 2378 available Australian ICU beds. For assumptions underlying best and worst case scenarios, see Methods. |
|||||||||||||||
Received 30 March 2020, accepted 3 April 2020
- Edward Litton1,2
- Tamara Bucci2
- Shaila Chavan2
- Yvonne Y Ho3
- Anthony Holley4,5
- Gretta Howard6
- Sue Huckson2,7
- Philomena Kwong8
- Johnny Millar9
- Nhi Nguyen10,11
- Paul Secombe12,13
- Marc Ziegenfuss14,15
- David Pilcher2,16
- 1 Fiona Stanley Hospital, Perth, WA
- 2 Centre for Outcome and Resource Evaluation, Australian and New Zealand Intensive Care Society, Melbourne, VIC
- 3 Royal Australian and New Zealand College of Radiologists, Sydney, NSW
- 4 Royal Brisbane and Women's Hospital, Brisbane, QLD
- 5 Australian and New Zealand Intensive Care Society, Melbourne, VIC
- 6 Turramurra Veterinary Hospital, Sydney, NSW
- 7 Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne, VIC
- 8 Animal Emergency Service, Brisbane, QLD
- 9 Royal Children's Hospital Melbourne, Melbourne, VIC
- 10 NSW Agency for Clinical Innovation, Sydney, NSW
- 11 Nepean Hospital, Penrith, NSW
- 12 Alice Springs Hospital, Alice Springs, NT
- 13 Northern Territory School of Medicine, Flinders University, Darwin, NT
- 14 Prince Charles Hospital, Brisbane, QLD
- 15 Queensland Statewide Intensive Care Clinical Network, Brisbane, QLD
- 16 Alfred Hospital, Melbourne, VIC
We thank all data collectors and clinicians, and in particular the directors of the Australian intensive care units who responded to our survey (Supporting Information). Anthony Delaney (intensive care specialist, Royal North Shore Hospital, Sydney) critically appraised the manuscript. Julie Strous (executive director, Australasian Veterinary Boards Council), Colin Dunlop (director, Advanced Anaesthesia Specialists) and Sarah Zaman (interventional cardiologist, MonashHEART and Monash Cardiovascular Research Centre, Monash University) assisted with collecting veterinary data. Jan Alexander (Australian and New Zealand Paediatric Intensive Care registry manager) contributed paediatric hospital data.
No relevant disclosures.
- 1. Guan WJ, Ni ZY, Hu Y, et al; China Medical Treatment Expert Group for Covid‐19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; https://doi.org/10.1056/nejmoa2002032 [Epub ahead of print].
- 2. Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID‐19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020; https://doi.org/10.1001/jama.2020.4031 [Epub ahead of print].
- 3. Australian and New Zealand Intensive Care Society. ANZICS COVID‐19 guidelines, version 1. 16 Mar 2020. https://www.anzics.com.au/coronavirus-guidelines (viewed Mar 2020).
- 4. Australia and New Zealand Intensive Care Society. Intensive care resources and activity in Australia and New Zealand: activity report 2017/18. Melbourne: ANZICS, 2020. https://www.anzics.com.au/wp-content/uploads/2020/02/2018-CCR-Report.pdf (viewed Mar 2020).
- 5. College of Intensive Care Medicine. Minimum standards for intensive care units. 1994, reviewed 2011. https://www.cicm.org.au/CICM_Media/CICMSite/CICM-Website/Resources/Professional%20Documents/IC-1-Minimum-Standards-for-Intensive-Care-Units.pdf (viewed Mar 2020).
- 6. Halpern NA, Tan KS. United States resource availability for COVID‐19 (Society of Critical Care Medicine). Updated 19 Mar 2020. https://sccm.org/Blog/March-2020/United-States-Resource-Availability-for-COVID-19 (viewed Mar 2020).
- 7. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid‐19. N Engl J Med 2020; https://doi.org/10.1056/nejmsb2005114 [Epub ahead of print].
- 8. Halpern NA, Tan KS, DeWitt M, Pastores SM. Intensivists in US acute care hospitals. Crit Care Med 2019; 47: 517–525.
- 9. Litton E, Bucci T. Intensive care resources and activity in Australia and New Zealand: activity report 2017/18, Melbourne: ANZICS Centre for Outcome and Resource Evaluation, 2020. https://www.anzics.com.au/wp-content/uploads/2020/02/2018-CCR-Report.pdf (viewed Mar 2020).
- 10. Secombe P, Brown A, McAnulty G, Pilcher D. Aboriginal and Torres Strait Islander patients requiring critical care: characteristics, resource use, and outcomes. Crit Care Resusc 2019; 21: 200–211.





Abstract
Objectives: To assess the capacity of intensive care units (ICUs) in Australia to respond to the expected increase in demand associated with COVID‐19.
Design: Analysis of Australian and New Zealand Intensive Care Society (ANZICS) registry data, supplemented by an ICU surge capability survey and veterinary facilities survey (both March 2020).
Settings: All Australian ICUs and veterinary facilities.
Main outcome measures: Baseline numbers of ICU beds, ventilators, dialysis machines, extracorporeal membrane oxygenation machines, intravenous infusion pumps, and staff (senior medical staff, registered nurses); incremental capability to increase capacity (surge) by increasing ICU bed numbers; ventilator‐to‐bed ratios; number of ventilators in veterinary facilities.
Results: The 191 ICUs in Australia provide 2378 intensive care beds during baseline activity (9.3 ICU beds per 100 000 population). Of the 175 ICUs that responded to the surge survey (with 2228 intensive care beds), a maximal surge would add an additional 4258 intensive care beds (191% increase) and 2631 invasive ventilators (120% increase). This surge would require additional staffing of as many as 4092 senior doctors (245% increase over baseline) and 42 720 registered ICU nurses (269% increase over baseline). An additional 188 ventilators are available in veterinary facilities, including 179 human model ventilators.
Conclusions: The directors of Australian ICUs report that intensive care bed capacity could be near tripled in response to the expected increase in demand caused by COVID‐19. But maximal surge in bed numbers could be hampered by a shortfall in invasive ventilators and would also require a large increase in clinician and nursing staff numbers.