Building resilience to environmental disasters requires transformative action to tackle climate change and health inequities
As the flood waters are receding in parts of New South Wales and Queensland and new forecasts of heavy rain are released, important questions emerge about the resilience of the Australian health system, and ultimately of our communities, to the intensifying extreme events we have experienced in recent years in the context of climate change.
Recurrent climate disasters and health emergencies
Unprecedented floods in Northern Rivers, NSW, and in south‐east Queensland have caused deaths and devastation and disrupted health and other services and facilities. Deaths from drowning, injuries, poisonings and infections are typically the immediate health impacts of floods.1 However, these direct impacts are only the tip of the health iceberg. Flood‐affected communities in Australia and other parts of the world have experienced long‐lasting mental health effects, such as depression, anxiety and post‐traumatic stress disorder.2,3
Underlying vulnerabilities, including obesity, diabetes, cancer, mental illness and other non‐communicable diseases (NCDs), complicate disaster recovery efforts in communities affected by extreme events. Climate disasters interrupt treatment and overall health care, exacerbating conditions or even causing deaths.4 Interruption may be caused by loss of belongings including medication, damaged transport routes, reduced health services, disrupted telecommunications, loss of power, and evacuations, often compounded by disrupted sleep, stress and reduced access to healthy food and safe water.
Importantly, flooding exacerbates health inequities in affected populations.2 In a previous flooding event that affected north‐eastern NSW in 2017, Aboriginal communities and people from low socio‐economic households were more likely to have their homes flooded and to be displaced, which exacerbated their mental health risk.5 Furthermore, people with a disability were more likely to have their homes flooded and be evacuated, still be displaced 6 months after the event, and experience disrupted access to food, support networks, health care and social services.6
Floods are generally associated with increased incidence of vector‐, food‐ and water‐borne diseases due to increased abundance of mosquitoes, water and food contamination, and compromised hygiene and sanitation services.1,7 For example, gastrointestinal disease and leptospirosis cases were recorded after floods in England and Hawaii.1 River flow and height (which are surrogates of flooding) were positively associated with Ross River virus disease spread by mosquitoes in the Murray River in eastern Australia.8 Ongoing rain and flooding in eastern Australia provide suitable environmental conditions for the spread of mosquito‐borne flaviviruses, which have recently caused several cases of acute encephalitis in animals and humans, including 42 human cases of Japanese encephalitis in NSW, Queensland, South Australia and Victoria (as at 18 May 2022).9
There has been widespread criticism of the handling of the flooding crisis in NSW after residents were left stranded on roofs in Lismore during the record floods of February 2022. An independent inquiry on the causes of, and factors contributing to, the frequency, intensity, timing and location of floods, as well as the preparation and planning for floods by the agencies and the community, has been announced by the NSW Government.10 This inquiry will scrutinise not only the emergency response, but also the transition from incident response to recovery, and consider land use planning and building standards in flood prone areas, appropriate action to adapt to future flood risks, and coordination and collaboration between all levels of government.
Building resilience to converging health and climate crises
Heavy rainfall, river floods, extreme heat and fire weather events are all projected to increase throughout Australia.11,12 Although we cannot fully attribute single weather events to climate change, extreme events such as the recent floods in NSW and Queensland, or the devastating 2020 Black Summer bushfires in eastern Australia, are projected to increase in frequency, intensity and duration for global warming scenarios from 1.5°C to 4°C.11
The recent report of the Intergovernmental Panel on Climate Change (IPCC) on impacts, adaptation and vulnerability12 identified the inability of institutions and governance systems to manage climate risks, such as those posed by floods, as a key risk for Australia. In this context of intensifying and more frequent extreme events, strengthening the long term resilience of health and social services and local communities to climate disasters becomes crucial. The IPCC report also highlighted the value of diverse knowledges including scientific, local and Indigenous knowledges in understanding and responding to climate risks.
The Sendai Framework for Disaster Risk Reduction 2015–2030 outlines four priorities for action to prevent new and reduce existing disaster risks:
- • understanding disaster risk;
- • strengthening disaster risk governance to manage disaster risk;
- • investing in disaster reduction for resilience; and
- • enhancing disaster preparedness for effective response and to “build back better” in recovery, rehabilitation and reconstruction.13
Resilience is not only the ability to maintain essential function, identity and structure but also the capacity for transformation.12 Building back better should not be interpreted as just engineering interventions of rebuilding residential areas in floodplains or bushfire prone areas with stronger flood‐ and fire‐resistant structures, but as an opportunity for more fundamental structural changes in our health system, society and economy that will strengthen community cohesion and resilience. In Australia, effective long term disaster management and resilience across multiple sectors is strongly influenced by geography, and should be informed by meaningful engagement with rural health services and Aboriginal and Torres Strait Islander and other local communities in rural and urban areas.14
The coronavirus disease 2019 (COVID‐19) pandemic and underlying NCDs present a challenge for disaster and health systems, especially when public health and health care infrastructure is inaccessible or damaged. People with cardiovascular and respiratory diseases, unstable diabetes, or renal and mental health diseases, and those who are undergoing cancer treatment are at greatest risk.15
Displacement and temporary relocation of families in crowded evacuation centres increase the risk of transmission of respiratory diseases, including COVID‐19. Fundamental shifts in preparedness planning are required to ensure health, safety, and smooth operations during emergencies in the context of the COVID‐19 pandemic.16 This includes revising evacuation plans, shelter design and staffing, health care operations for evacuees, and public health messaging. Developing effective public health messaging for floods during the pandemic is critical and requires careful planning and familiarity with the needs and characteristics of the affected communities.16
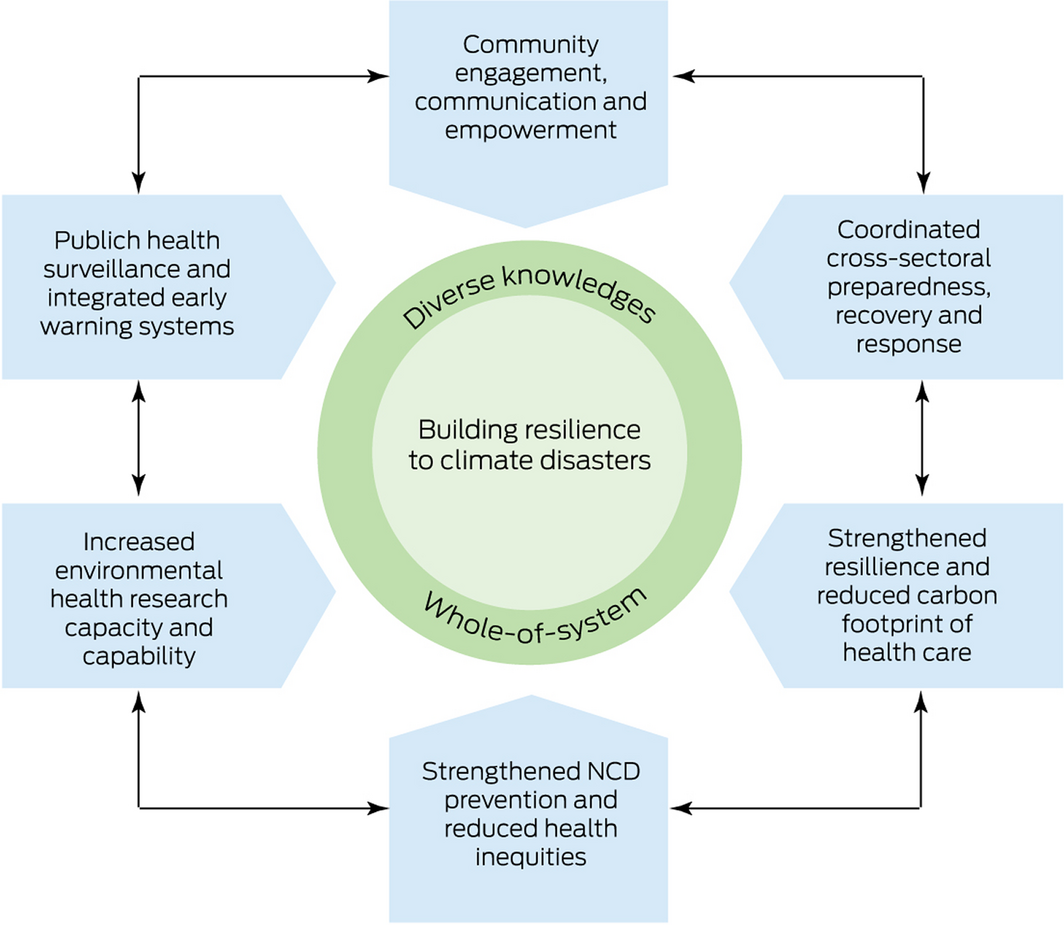
The converging impacts of climate change, extreme events, COVID‐19, NCDs, socio‐economic inequities, population ageing and urban growth require an integrated whole‐of‐system response. This should focus on flood‐ and fire‐resilient land‐use planning that will reduce community exposure to climate‐related risks and systemic vulnerability in the long term,17 improved housing conditions for low socio‐economic households, agile and high value health care, strengthened public health surveillance and emergency warning systems, and a net‐zero carbon economy.
In the broader health sector, transformative action should involve two key aspects:
- • increasing the resilience of health and social care services through stronger focus on NCD prevention, particularly on mental health and wellbeing, as well as on improvements in the structural and operational resilience of health care infrastructure; and
- • drastically reducing the carbon footprint of the health sector, which represents 7% of the national carbon emissions,18 through reduction of wasteful clinical care (low value care), health care‐related transport, water and energy consumption.19
The response of health professionals to COVID‐19, catastrophic bushfires and floods over the past 2 years has been heroic, but it is not sustainable in the long run. Extreme events, pandemic fatigue, overstretched clinical services, spiralling demand for mental health services, and staff burnout could drive the health care workforce to collapse.20 Beyond the health system, the COVID‐19 pandemic has altered the social capital (ie, community attachment, solidarity and social trust) and exposed health inequities in our communities.21
Health practitioners have the opportunity to contribute their expertise to help reduce the health consequences of climate disasters across the prevention, preparedness, response and recovery phases of disaster management.22 Disaster preparedness and recovery plans should be developed in partnership with disability organisations and community grassroots, including Aboriginal and Torres Strait Islander communities, to ensure that scientific knowledge is combined with local knowledge gained from experience and built from the ground up.23
Proactive adaptation through better planning in the built environment is essential. The initial focus on recovery should shift towards long term planning of more resilient urban and rural infrastructure, housing, digital communications, and health and social services. In addition, effective prevention of infectious diseases outbreaks related to extreme weather events requires strengthened public health surveillance and integrated early warning systems.24 Similarly, early detection and treatment of mental health problems triggered or exacerbated by extreme events is essential to prevent impacts that could be prolonged over years.2
Response and recovery efforts during and after climate disasters, such as the recent floods in NSW and Queensland are essential, but long term planning and public health prevention are equally or even more important in the face of converging health and climate crises. To build this urgently needed long term resilience (Box), we call for:
- • developing a coordinated cross‐sectoral whole‐of‐system response (health, environment, land‐use planning, social housing) to floods, strongly focusing on long term public health prevention and preparedness for more frequent and intense extreme events; this should incorporate meaningful community engagement, including Aboriginal and Torres Strait Islander, culturally and linguistically diverse, and socio‐economically marginalised communities, to build social cohesion, reduce inequities and develop culturally appropriate risk communication strategies and person‐centred adaptation plans;
- • strengthening NCD prevention, including mental health and wellbeing services, particularly for rural and remote communities disproportionally affected by environmental change and extreme events;
- • implementing a stronger environmental public health surveillance for infectious diseases and NCDs, and climate‐informed predictive models and early warning systems linked to emergency, public and mental health services;
- • establishing a sustainable health unit (similar to Greener NHS in England25) that will help improve the health sector’s resilience to climate and health emergencies, and monitor and reduce the carbon footprint of health services; and
- • increasing research capacity and capability and identifying gaps in local service delivery, communication and coordination, with a strong focus on the evaluation of interventions aiming to increase health sector and community resilience, particularly of at‐risk populations, to floods and other climate disasters.
Provenance: Not commissioned; externally peer reviewed.
- 1. Alderman K, Turner LR, Tong S. Floods and human health: a systematic review. Environ Int 2012; 47: 37‐47.
- 2. Mulchandani R, Armstrong B, Beck CR, et al. The English National Cohort Study of Flooding and Health: psychological morbidity at three years of follow up. BMC Public Health 2020; 20: 321.
- 3. Fernandez A, Black J, Jones M, et al. Flooding and mental health: a systematic mapping review. PLoS One 2015; 10: e0119929.
- 4. Ryan B, Franklin RC, Burkle FM, et al. Identifying and describing the impact of cyclone, storm and flood related disasters on treatment management, care and exacerbations of non‐communicable diseases and the implications for public health. PLoS Curr 2015; 7: ecurrents.dis.62e9286d152de04799644dcca47d9288.
- 5. Matthews V, Longman J, Berry HL, et al. Differential mental health impact six months after extensive river flooding in rural Australia: a cross‐sectional analysis through an equity lens. Front Public Health 2019; 7: 367.
- 6. Longman JM, Bennett‐Levy J, Matthews V, et al. Rationale and methods for a cross‐sectional study of mental health and wellbeing following river flooding in rural Australia, using a community‐academic partnership approach. BMC Public Health 2019; 19: 1255.
- 7. Coalson JE, Anderson EJ, Santos EM, et al. The complex epidemiological relationship between flooding events and human outbreaks of mosquito‐borne diseases: a scoping review. Environ Health Perspect 2021; 129: 96002.
- 8. Tall JA, Gatton ML, Tong S. Ross River virus disease activity associated with naturally occurring nontidal flood events in australia: a systematic review. J Med Entomol 2014; 51: 1097‐1108.
- 9. Australian Government Department of Health. Japanese encephalitis virus (JEV), 2022. https://www.health.gov.au/health‐alerts/japanese‐encephalitis‐virus‐jev/about (viewed May 2022).
- 10. NSW Government. 2022 NSW Flood Inquiry. https://www.nsw.gov.au/nsw‐government/projects‐and‐initiatives/floodinquiry (viewed May 2022).
- 11. Intergovernmental Panel on Climate Change. Climate change 2021: the physical science basis. https://www.ipcc.ch/report/sixth‐assessment‐report‐working‐group‐i (viewed May 2022).
- 12. Intergovernmental Panel on Climate Change. Climate change 2022: impacts, adaptation and vulnerability. https://www.ipcc.ch/report/sixth‐assessment‐report‐working‐group‐ii (viewed May 2022).
- 13. United Nations Office for Disaster Risk Reduction. Sendai Framework for Disaster Risk Reduction 2015–2030. https://www.undrr.org/publication/sendai‐framework‐disaster‐risk‐reduction‐2015‐2030 (viewed May 2022).
- 14. Parsons M, Reeve I, McGregor J, et al. Disaster resilience in Australia: a geographic assessment using an index of coping and adaptive capacity. Int J Disaster Risk Reduct 2021; 62: 102422.
- 15. Ryan BJ, Franklin RC, Burkle FM, et al. Reducing disaster exacerbated non‐communicable diseases through public health infrastructure resilience: perspectives of Australian disaster service providers. PLoS Curr 2016; 8: ecurrents.dis.d142f36b6f5eeca806d95266b20fed1f.
- 16. National Academies of Sciences, Engineering, and Medicine. Emergency evacuation and sheltering during the COVID‐19 pandemic. NASEM, 2021. https://nap.nationalacademies.org/catalog/26084/emergency‐evacuation‐and‐sheltering‐during‐the‐covid‐19‐pandemic (viewed May 2022).
- 17. Australian Institute for Disaster Resilience. Land use planning for disaster resilient communities. https://knowledge.aidr.org.au/resources/handbook‐land‐use‐planning (viewed May 2022).
- 18. Malik A, Lenzen M, McAlister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health 2018; 2: e27‐e35.
- 19. Barratt AL, Bell KJ, Charlesworth K, et al. High value health care is low carbon health care. Med J Aust 2022; 216: 67‐68. https://www.mja.com.au/journal/2022/216/2/high‐value‐health‐care‐low‐carbon‐health‐care
- 20. Ong O. How pandemic fatigue could drive a medical workforce collapse. InSight+ 2021; 15 Nov. https://insightplus.mja.com.au/2021/43/how‐pandemic‐fatigue‐could‐drive‐a‐medical‐workforce‐collapse
- 21. de Leeuw E, Fatema K, Sitas F, et al. Work, income and health inequity: a snapshot of the evidence [ACOSS/UNSW Sydney Poverty and Inequality Partnership Report No. 8]. Sydney: UNSW Sydney, 2021. https://povertyandinequality.acoss.org.au/wp‐content/uploads/2021/08/Work‐income‐and‐health‐inequity_August‐2021.pdf (viewed May 2022).
- 22. Burns PL, Douglas KA, Hu W. Primary care in disasters: opportunity to address a hidden burden of health care. Med J Aust 2019; 210: 297‐299. https://www.mja.com.au/journal/2019/210/7/primary‐care‐disasters‐opportunity‐address‐hidden‐burden‐health‐care
- 23. Villeneuve M. Building a roadmap for inclusive disaster risk reduction in Australian communities. Prog Disaster Sci 2021; 10: 100166.
- 24. McClymont H, Bambrick H, Si X, et al. Future perspectives of emerging infectious diseases control: a One Health approach. One Health 2022; 14: 100371.
- 25. National Health Service. Greener NHS, 2022. https://www.england.nhs.uk/greenernhs (viewed May 2022).






Open access
Open access publishing facilitated by Australian National University, as part of the Wiley ‐ Australian National University agreement via the Council of Australian University Librarians.
We acknowledge the HEAL (Healthy Environments And Lives) National Research Network, which receives funding from the National Health and Medical Research Council (Grant No. 2008937).
No relevant disclosures.