The known: Individual and neighbourhood socio‐economic status each influence the prevalence of cardiovascular risk factors and clinical events, particularly during adulthood.
The new: Greater socio‐economic disadvantage at birth was associated with lower BMI, systolic blood pressure, and LDL‐ and HDL‐cholesterol levels at ages 11, 18 and 25 years. Children of mothers in remote locations at the time of birth had lower mean BMI and HDL‐cholesterol levels, and higher triglyceride levels.
The implications: Strategies for preventing cardiovascular disease in Indigenous Australian communities must take their individual perspectives and socio‐economic conditions into account.
Both the age‐adjusted prevalence and mortality of atherosclerotic cardiovascular disease (CVD) have markedly declined in developed countries since the 1960s. Reduced population levels of cardiovascular risk factors, particularly the lower prevalence of elevated serum lipid levels and high blood pressure, explain more than over 40% of the drop in CVD mortality.1 However, these improvements have not been as evident among Indigenous Australians, for whom mean life expectancy is still about ten years lower than for other Australians and the most frequent cause of death is CVD.2
Although the prevalence of CVD and of its main risk factors has declined worldwide, socio‐economic differences in risk levels have not.3,4 Their prevalence is influenced both by the socio‐economic characteristics of individuals and those of their neighbourhoods.5,6,7 However, information about the association between socio‐economic status and CVD risk factors across the life course is scarce, especially for early life. In particular, longitudinal data for Indigenous Australian children and young adults have not been reported.
We therefore analysed longitudinal risk factor data for 570 participants in the Aboriginal Birth Cohort (ABC) study in the Northern Territory. Our aim was to determine whether socio‐economic features at birth are associated with differences in body mass index (BMI), blood lipid levels, and blood pressure during the first 25 years of life.
Methods
Participants
Details of the ABC study have been published previously.8,9 Briefly, 686 of the 1238 children born to Indigenous Australian mothers at the Royal Darwin Hospital during 1987–1990 were recruited for the study; the mean birthweights and sex ratio of the recruited children were similar to those for the children not recruited. Three clinical follow‐ups have since been conducted: Wave 2 in 1998–2001 (570 of 668 living participants; mean age, 11 years; range, 8–14 years), Wave 3 in 2006–2008 (442 of 659 living participants; mean age, 18 years; range, 16–20 years), and Wave 4 in 2014–2016 (423 of 647 living participants [65%]; mean age, 25 years; range, 23–28 years). Participants resided in 46 urban and remote communities across the NT; 428 participants (75%) lived in remote communities (including the Arnhem, Victoria Daly, and Tiwi regions) and 142 (25%) in urban Darwin and its immediate surrounds (Supporting Information, figure 1).
Socio‐economic variables
Area‐level socio‐economic disadvantage was defined according to the Indigenous Relative Socioeconomic Outcomes (IRSEO) index. The IRSEO score is calculated at the Indigenous Area level from data for nine variables (three related to employment, three to education, two to housing, one to income) derived from the 2011 Census of Population and Housing; each area is assigned to one of 100 percentiles (from 1, the most advantaged, to 100, the most disadvantaged).10 Participants were assigned IRSEO scores according to their reported residential addresses at birth. Scores were categorised into four groups: least disadvantage (range, 13–40), moderate disadvantage (range, 41–80), high disadvantage (range, 81–90), and highest disadvantage (range 91–99). Families were classified as urban or remote according to location of residence of the participant at birth. Parity of the mother at the time of birth of the participant was categorised as one, 2–3, 4–5, or 6 or more children.
Blood lipid levels, blood pressure, body mass index
Venous blood samples were collected for assessing lipid levels (low density lipoprotein [LDL]‐cholesterol, high density lipoprotein [HDL]‐cholesterol, triglycerides) by enzymatic methods (analytic devices employed: Waves 2 and 3, Hitachi 917, Roche; Wave 4, XPand Plus, Siemens). Blood pressure was measured three times during each wave (right arm, sitting after resting) with an automatic oscillatory unit (LifeSign 420, Welch Allyn); the mean systolic and diastolic values were included in analyses. BMI was calculated from weight, measured to 0.1 kg with a digital scale (TBF‐521, Tanita) while the participant was barefoot and in light clothing, and height, measured with a portable stadiometer to the nearest millimetre.
Statistical analyses
Characteristics of study participants are reported as means with standard deviations (SDs) for continuous variables and as proportions for categorical variables. Attrition analyses compared baseline characteristics for participants and non‐participants in each follow‐up (Student t tests for continuous variables, χ2 tests for categorical variables).
The main analyses examined whether associations between socio‐economic factors at birth and longitudinal data on cardiovascular risk factors were statistically significant. To assess these associations and to calculate point estimates (with 95% confidence intervals [CIs]) of risk factor levels for each study wave, we used linear mixed models to account for intra‐subject correlation arising from the repeated measures. Models included one of the socio‐economic variables (IRSEO score, residence, mother's parity at the birth of the participant) as the variable of interest, and sex, BMI (except in BMI models), and study wave as covariates. To provide least square means (with 95% CIs) for each follow‐up wave, terms for interactions between the socio‐economic variables and study wave were also included. Age was not included as a factor in the main analyses because it was collinear with study wave (variance inflation factor, 30); as age variability in each wave was limited, study wave was included as a factor in the models rather than continuous age. However, we also performed sensitivity analyses that included age as a factor. To assess the influence of missing data, we also analysed data limited to participants who had participated in all three follow‐ups. All analyses were performed in SAS 9.4 (SAS Institute); P < 0.05 (two‐tailed) was deemed statistically significant.
Ethics approval
This study was approved by the Human Research Ethics Committee of the Northern Territory Department of Health and Menzies School of Health Research, including the Aboriginal Ethics Sub‐committee with the power of veto (reference, 2013‐2022). The investigation complied with the National Health and Medical Research Council National Statement on Ethical Conduct in Human Research (2007) and the Helsinki Declaration of 1975 (2008 revision). Informed written consent was obtained from all participants or (until the age of 18 years) their mothers.
Results
The characteristics of the study participants are summarised in Box 1. During Wave 4, 75 of the 423 participants (18%) reported have lived in another community at some point in their lives; 30 of 343 participants (8.7%) who had lived in remote areas at Wave 2 had moved to urban areas by Wave 4, and 15 of 80 participants (19%) who had lived in urban areas had moved to remote areas.
Attrition analyses are summarised in the table in the Supporting Information. Larger proportions of non‐participants than of participants in Waves 3 and 4 were male, lived at birth in areas of least disadvantage, and lived in urban areas. The mean age (at Wave 2) of non‐participants in Wave 3 was slightly higher than that of participants; in Wave 4, the maternal parity for non‐participants was shifted to slightly lower numbers of children than for participants (three or fewer children: 80% v 71%).
Body mass index
IRSEO of residence at birth (P < 0.001), remoteness of residence (P < 0.001), and parity at birth (P = 0.039) each influenced mean BMI levels (Box 2).
Blood pressure
IRSEO of residence at birth influenced systolic blood pressure level (P = 0.024); remoteness of residence (P = 0.32) and parity (P = 0.54) did not (Box 3). There were no significant associations between socio‐economic variables and diastolic blood pressure: IRSEO, P = 0.07; remoteness, P = 0.93; parity, P = 0.23 (Supporting Information, figure 2).
Lipid levels
IRSEO of residence at birth influenced LDL‐cholesterol (P = 0.010) (Box 4) and HDL‐cholesterol levels (P < 0.001) (Box 5). LDL‐cholesterol level was influenced neither by remoteness of residence (P = 0.21) nor by parity (P = 0.30) (Box 4); HDL‐cholesterol level was influenced by remoteness of residence (P < 0.001), but not by parity (P = 0.53) (Box 5). Triglyceride levels were influenced by remoteness of residence (P = 0.043), but not by IRSEO (P = 0.42) or parity (P = 0.25) (Box 6).
Sensitivity analyses
The results of analyses also adjusted for age were similar to those of the main analysis (data not shown). The results of analyses restricted to data for participants who participated in all three follow‐ups were also similar, except that the associations between IRSEO and LDL‐cholesterol level (P = 0.17) and between remoteness and triglyceride level (P = 0.13) were not statistically significant.
Discussion
We found that socio‐economic factors at the time of birth are statistically associated with differences in the prevalence of CVD risk factors among Indigenous Australians in the Northern Territory. In particular, higher HDL‐cholesterol levels were associated with having a mother living in an area of low disadvantage or in an urban area at the time of birth. Of the three socio‐economic measures examined, IRSEO grouping was associated with more differences in outcomes than remoteness of residence or maternal parity at birth.
Earlier studies have consistently found that neighbourhood factors influence the prevalence among adults of CVD and its risk factors.7,11 A Canadian study reported that children from disadvantaged neighbourhoods were more likely than those from less disadvantaged areas to have CVD risk factors or events during 34 years of follow‐up.11 In the Cardiovascular Risk in Young Finns study, neighbourhood socio‐economic disadvantage across life was associated with higher blood pressure and triglyceride levels in midlife.7 We found, in contrast, that systolic blood pressure and LDL‐cholesterol levels were lower among people from areas of highest disadvantage. However, the prevalence among Indigenous Australians of small, dense LDL particles is high;12 we did not have data for evaluating this phenomenon. Our findings regarding HDL‐cholesterol and triglyceride levels were consistent with previous reports7,13 that they are most favourable in people from least disadvantaged areas (HDL‐cholesterol) and from urban places of residence (triglycerides).
Our findings have several potential explanations. Dietary factors are important, and poor diet is one of the main reasons for health gaps between Indigenous and non‐Indigenous Australians.14 Relatively high food prices in remote communities, combined with low incomes, cause food insecurity.15 In American studies, food insecurity has been associated with lower blood pressure and cholesterol levels.16,17 Even short periods of low income reduce dietary quality among remote Indigenous Australians; the most notable differences between periods of high and low money availability are in energy intake, the proportions of energy provided by fats and carbohydrates, and the ratio of sodium to potassium intake.18 Structural factors, such as limited food storage facilities and transport, affect dietary choices.19 Complex food‐sharing networks also influence food choices, and consuming traditional bush foods may affect diet quality, but information on the health effects of these factors is sparse.
For Indigenous Australians, neighbourhood disadvantage is inversely and urban residence directly associated with positive scores on an American Heart Association index of ideal cardiovascular health.20 As we have found that greater neighbourhood disadvantage and remoteness were favourably associated with some characteristics (blood pressure, LDL‐cholesterol levels) and unfavourably with others (HDL‐cholesterol, triglyceride levels), the underlying reasons for these associations probably include non‐dietary factors. The importance of social factors — education, inequities in resource allocation, employment opportunities, physical infrastructure — must also be taken into account.21 Finally, genetic and inflammatory factors play important roles in determining serum lipid levels in Indigenous Australians.22 In a medium‐sized study in southeast Queensland (N = 155), apolipoprotein E4 polymorphisms associated with high triglyceride and low HDL‐cholesterol levels were 80% more frequent among Indigenous than among non‐Indigenous participants.23
From the clinical and public health points of view, our findings provide novel information about the effects of socio‐economic factors on cardiovascular risk in an Indigenous community. It has been estimated that each 20 mmHg rise in systolic blood pressure in people aged 40–69 years is associated with a doubling of cardiovascular mortality;24 an increase of 1 mmol/L in LDL‐cholesterol levels has been associated with a 62% prospective increase in coronary disease.25 The largest differences by IRSEO group we found were 3.5 mmHg for systolic blood pressure and 0.6 mmol/L for LDL‐cholesterol (in Wave 4). From the public health perspective, our data indicate that intervention strategies for preventing CVD in Indigenous Australian communities must take the perspectives and socio‐economic conditions of the residents into account.
Limitations
The strengths of our study include its longitudinal design commencing in childhood, and the structured follow‐ups with good retention rates (of the participants in Wave 2, 78% participated in Wave 3 and 75% in Wave 4), particularly given the accessibility problems that hamper data collection in remote areas. The study population, however, was quite small, which limits extrapolation of our findings. Further, attrition analyses identified differences between non‐participants and participants in Waves 3 and 4. Another limitation to generalising our findings is our definition of socio‐economic disadvantage. For studies of non‐Indigenous neighbourhoods, authors have assessed income, education level, occupation, unemployment rates, and the proportions of people living in owned and rental housing,3,4,7 but data for these variables were not available for our study; moreover, they would not be appropriate for assessing remote communities. The IRSEO scores we employed refer to area‐level socio‐economic status and do not necessarily reflect the socio‐economic status of individual participants. Finally, the participants were still young adults at the most recent follow‐up, prohibiting the investigation of associations between socio‐economic measures and CVD morbidity.
Conclusion
Our longitudinal life course analysis provides evidence for associations between area‐level socio‐economic status at birth and the prevalence of major cardiovascular disease risk factors among Indigenous Australians. Mean BMI, blood pressure, and LDL‐cholesterol were at healthier levels among individuals born in highly disadvantaged and remote areas, whereas mean HDL‐cholesterol and triglyceride levels were least favourable in these people.
Box 1 – Characteristics of the study participants
|
Variable |
|
||||||||||||||
|
|
|||||||||||||||
|
Number of participants |
|
||||||||||||||
|
Wave 2 |
570 |
||||||||||||||
|
Wave 3 |
442 |
||||||||||||||
|
Wave 4 |
423 |
||||||||||||||
|
Age (years), mean (SD) |
|
||||||||||||||
|
Wave 2 |
11.0 (1.2) |
||||||||||||||
|
Wave 3 |
17.8 (1.1) |
||||||||||||||
|
Wave 4 |
25.3 (1.2) |
||||||||||||||
|
Sex (male) |
|
||||||||||||||
|
Wave 2 |
303 (53.2%) |
||||||||||||||
|
Wave 3 |
221 (50.0%) |
||||||||||||||
|
Wave 4 |
207 (48.9%) |
||||||||||||||
|
IRSEO (at birth) |
|
||||||||||||||
|
Least disadvantage |
120 (21.1%) |
||||||||||||||
|
Moderate disadvantage |
30 (5.3%) |
||||||||||||||
|
High disadvantage |
201 (35.2%) |
||||||||||||||
|
Highest disadvantage |
219 (38.4%) |
||||||||||||||
|
Residence at birth |
|
||||||||||||||
|
Urban |
101 (17.7%) |
||||||||||||||
|
Remote |
469 (82.3%) |
||||||||||||||
|
Mother's parity at birth |
|
||||||||||||||
|
One child |
190 (33.5%) |
||||||||||||||
|
2–3 children |
227 (39.8%) |
||||||||||||||
|
4–5 children |
110 (19.3%) |
||||||||||||||
|
6 or more children |
43 (7.5%) |
||||||||||||||
|
|
|||||||||||||||
|
IRSEO = Indigenous Relative Socioeconomic Outcomes; SD = standard deviation. |
|||||||||||||||
Box 2 – Relationship between body mass index and socio‐economic variables in the Australian Aboriginal Birth Cohort study.* A. Residence at birth: IRSEO; B. Residence at birth: remoteness; C. Mother's parity at birth
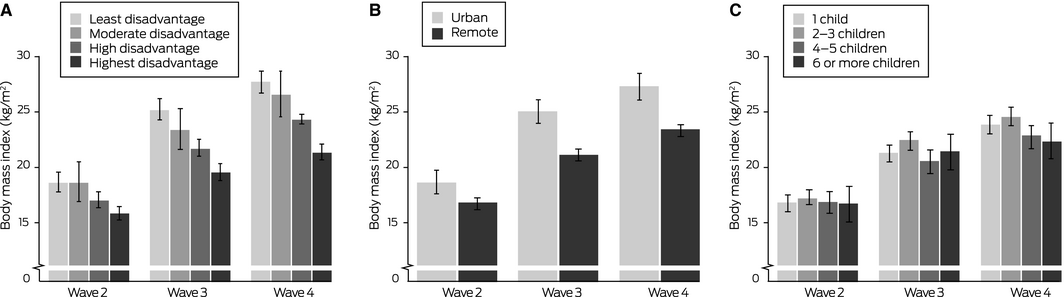
IRSEO = Indigenous Relative Socioeconomic Outcomes. * Least square means with 95% confidence intervals. Linear mixed models also included sex and study wave as variables. Interactions: wave*IRSEO, P < 0.001; wave*remoteness, P < 0.001; wave*parity, P = 0.036.
Box 3 – Relationship between systolic blood pressure and socio‐economic variables in the Australian Aboriginal Birth Cohort study.* A. Residence at birth: IRSEO; B. Residence at birth: remoteness; C. Mother's parity at birth
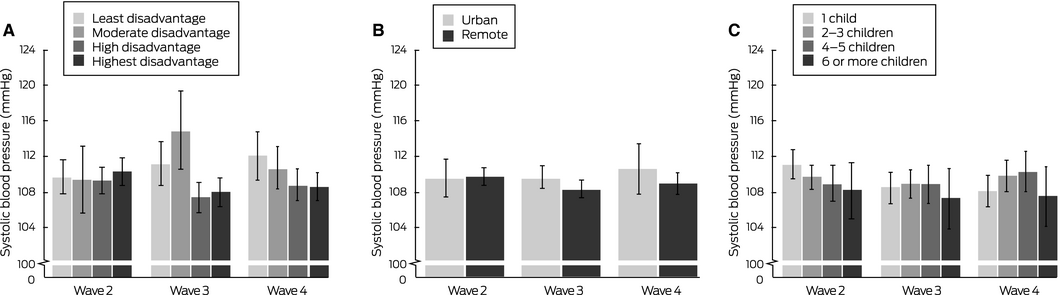
IRSEO = Indigenous Relative Socioeconomic Outcomes. * Least square means with 95% confidence intervals. Linear mixed models also included sex, study wave, and body mass index as variables. Interactions: wave*IRSEO, P = 0.022; wave*remoteness, P = 0.46; wave*parity, P = 0.17.
Box 4 – Relationship between LDL‐cholesterol level and socio‐economic variables in the Australian Aboriginal Birth Cohort study.* A. Residence at birth: IRSEO; B. Residence at birth: remoteness; C. Mother's parity at birth
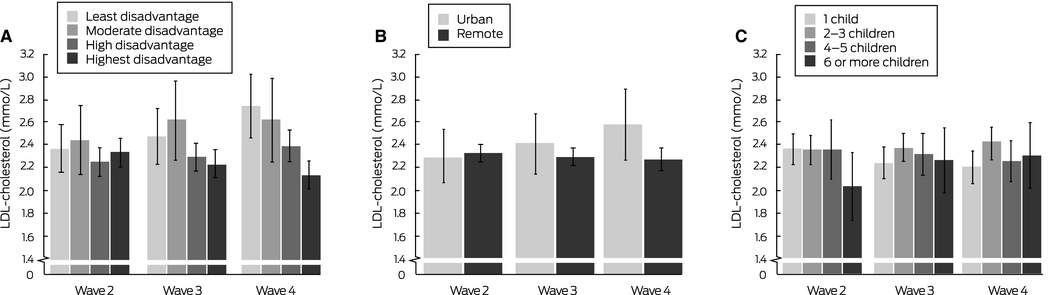
IRSEO = Indigenous Relative Socioeconomic Outcomes; LDL‐cholesterol = low density lipoprotein cholesterol. * Least square means with 95% confidence intervals. Linear mixed models also included sex, study wave, and body mass index as variables. Interactions: wave*IRSEO, P < 0.001; wave*remoteness, P = 0.13; wave*parity, P = 0.17.
Box 5 – Relationship between HDL‐cholesterol level and socio‐economic variables in the Australian Aboriginal Birth Cohort study.* A. Residence at birth: IRSEO; B. Residence at birth: remoteness; C. Mother's parity at birth
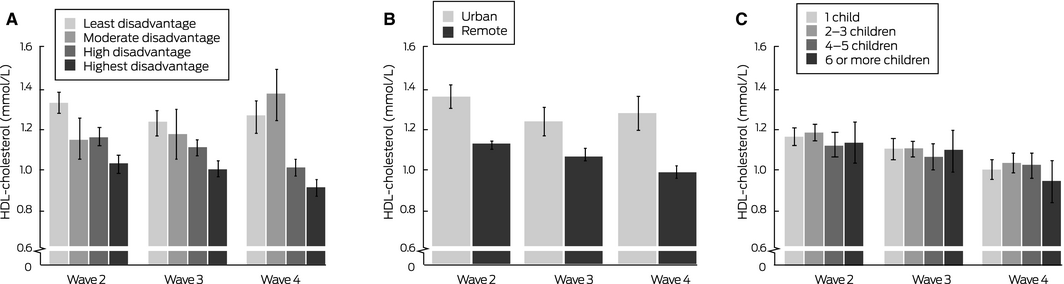
HDL‐cholesterol = high density lipoprotein cholesterol; IRSEO = Indigenous Relative Socioeconomic Outcomes. * Least square means with 95% confidence intervals. Linear mixed models also included sex, study wave, and body mass index as variables. Interactions: wave*IRSEO, P < 0.001; wave*remoteness, P = 0.014; wave*parity, P = 0.60.
Box 6 – Relationship between triglyceride level and socio‐economic variables in the Australian Aboriginal Birth Cohort study.* A. Residence at birth: IRSEO; B. Residence at birth: remoteness; C. Mother's parity at birth
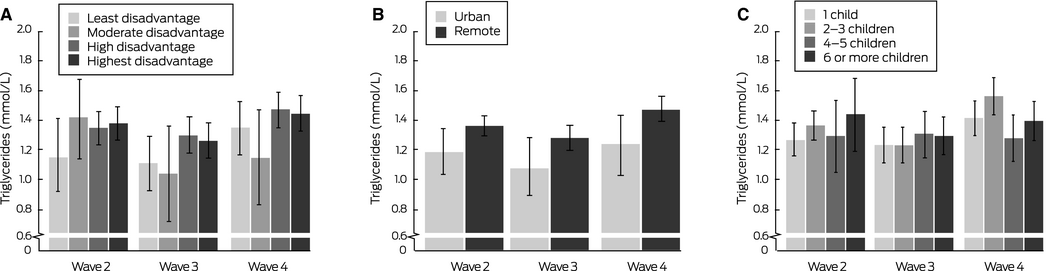
IRSEO = Indigenous Relative Socioeconomic Outcomes. * Least square means with 95% confidence intervals. Linear mixed models also included sex, study wave, and body mass index as variables. Interactions: wave*IRSEO, P = 0.36; wave*remoteness, P = 0.85; wave*parity, P = 0.022.
Received 19 October 2018, accepted 12 April 2019
- Markus Juonala1,2,3
- Pauline Sjöholm1
- Katja Pahkala1
- Susan Ellul3
- Noora Kartiosuo4
- Belinda Davison5
- Gurmeet R Singh5
- 1 Turun Yliopisto (University of Turku), Turku, Finland
- 2 Turku University Hospital, Turku, Finland
- 3 Murdoch Children's Research Institute, Melbourne, VIC
- 4 Research Centre of Applied and Preventive Cardiovascular Medicine, Turun Yliopisto, Turku, Finland
- 5 Menzies School of Health Research, Darwin, NT
We acknowledge past and present study team members, particularly the late Susan Sayers AO, founder of the Aboriginal Birth Cohort study. We especially thank the young adults in the Aboriginal Birth Cohort and their families and communities for their cooperation and support, and all the individuals who helped in urban and rural locations. The investigation was supported by the National Health and Medical Research Council, the Channel 7 Children's Research Foundation of South Australia, the National Heart Foundation, a Northern Territory Government Research and Innovation Grant, the Juho Vainio Foundation, the Turku University Hospital, and the Finnish Foundation for Cardiovascular Research. The sponsors had no role in preparing the manuscript.
No relevant disclosures.
- 1. Capewell S, O'Flaherty M. What explains declining coronary mortality? Lessons and warnings. Heart 2008; 94: 1105–1108.
- 2. Australian Institute of Health and Welfare. The health and welfare of Australia's Aboriginal and Torres Strait Islander Peoples: 2015 (Cat No. IHW 147). Canberra: AIHW, 2015.
- 3. Naska A, Katsoulis M, Trichopoulos D, Trichopoulou A. The root causes of socioeconomic differentials in cancer and cardiovascular mortality in Greece. Eur J Cancer Prev 2012; 21: 490–496.
- 4. Pujades‐Rodriguez M, Timmis A, Stogiannis D, et al. Socioeconomic deprivation and the incidence of 12 cardiovascular diseases in 1.9 million women and men: implications for risk prediction and prevention. PLoS One 2014; 9: e104671.
- 5. Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. New Engl J Med 2001; 345: 99–106.
- 6. Halonen JI, Stenholm S, Pentti J, et al. Childhood psychosocial adversity and adult neighborhood disadvantage as predictors of cardiovascular disease: a cohort study. Circulation 2015; 132: 371–379.
- 7. Kivimäki M, Vahtera J, Tabák AG, et al. Neighbourhood socioeconomic disadvantage, risk factors, and diabetes from childhood to middle age in the Young Finns Study: a cohort study. Lancet Public Health 2018; 3: e365–e373.
- 8. Sayers SM, Mackerras D, Singh G, et al. An Australian Aboriginal birth cohort: a unique resource for a life course study of an Indigenous population. A study protocol. BMC Int Health Hum Rights 2003; 3: 1.
- 9. Sayers S, Singh G, Mackerras D, et al. Australian Aboriginal Birth Cohort study: follow‐up processes at 20 years. BMC Int Health Hum Rights 2009; 9: 23.
- 10. Biddle N. Socioeconomic outcomes (CAEPR Indigenous Population Project 2011 census papers, paper 13). Canberra: Centre for Aboriginal Economic Policy Research, Australia National University, 2013. http://caepr.cass.anu.edu.au/research/publications/socioeconomic-outcomes (viewed June 2019).
- 11. Kakinami L, Serbin LA, Stack DM, et al. Neighbourhood disadvantage and behavioural problems during childhood and the risk of cardiovascular disease risk factors and events from a prospective cohort. Prev Med Rep 2017; 8: 294–300.
- 12. O'Neal DN, Piers LS, Iser DM, et al. Australian Aboriginal people and Torres Strait Islanders have an atherogenic lipid profile that is characterised by low HDL‐cholesterol level and small LDL particles. Atherosclerosis 2008; 201: 368–377.
- 13. McCarthy K, Cai LB, Xu FR, et al. Urban–rural differences in cardiovascular disease risk factors: a cross‐sectional study of schoolchildren in Wuhan, China. PLoS One 2015; 10: e0137615.
- 14. Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012; 70: 3–21.
- 15. Brimblecombe JK, O'Dea K. The role of energy cost in food choices for an Aboriginal population in northern Australia. Med J Aust 2009; 190: 549–551. https://www.mja.com.au/journal/2009/190/10/role-energy-cost-food-choices-aboriginal-population-northern-australia
- 16. Saiz AM, Aul AM, Malecki KM, et al. Food insecurity and cardiovascular health: findings from a statewide population health survey in Wisconsin. Prev Med 2016; 93: 1–6.
- 17. Shin JI, Bautista LE, Walsh MC, et al. Food insecurity and dyslipidemia in a representative population‐based sample in the US. Prev Med 2015; 77: 186–190.
- 18. Wycherley TP, Pekarsky BA, Ferguson MM, et al. Fluctuations in money availability within an income cycle impacts diet quality of remote Indigenous Australians. Public Health Nutr 2017; 20: 1431–1440.
- 19. Brimblecombe J, Maypilama E, Colles S, et al. Factors influencing food choice in an Australian Aboriginal community. Qual Health Res 2014; 24: 387–400.
- 20. Sjöholm P, Pahkala K, Davison B, et al. Early life determinants of cardiovascular health in adulthood. The Australian Aboriginal Birth Cohort study. Int J Cardiol 2018; 269: 304–309.
- 21. Smith KB, Humphreys JS, Wilson MG. Addressing the health disadvantage of rural populations: how does epidemiological evidence inform rural health policies and research? Aust J Rural Health 2008; 16: 56–66.
- 22. Lyons JG, O'Dea K, Walker KZ. Evidence for low high‐density lipoprotein cholesterol levels in Australian indigenous peoples: a systematic review. BMC Public Health 2014; 14: 545.
- 23. Shaw JT, Tate J, Kesting JB, et al. Apolipoprotein E polymorphism in indigenous Australians: allelic frequencies and relationship with dyslipidaemia. Med J Aust 1999; 170: 161–164.
- 24. Lewington S, Clarke R, Qizilbash N, et al. Age‐specific relevance of usual blood pressure to vascular mortality: a meta‐analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360: 1903–1913.
- 25. Emerging Risk Factors Collaboration; Di Angelantonio E, Sarwar N, Perry P, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009; 302: 1993–2000.





Abstract
Objectives: To determine whether socio‐economic status at birth is associated with differences in risk factors for cardiovascular disease — body mass index (BMI), blood pressure, blood lipid levels — during the first 25 years of life.
Design: Analysis of prospectively collected data.
Setting, participants: 570 of 686 children born to Aboriginal mothers at the Royal Darwin Hospital during 1987–1990 and recruited for the Aboriginal Birth Cohort Study in the Northern Territory. Participants resided in 46 urban and remote communities across the NT. The analysed data were collected at three follow‐ups: Wave 2 in 1998–2001 (570 participants; mean age, 11 years), Wave 3 in 2006–2008 (442 participants; mean age, 18 years), and Wave 4 in 2014–2016 (423 participants; mean age, 25 years).
Main outcome measures: Cardiovascular disease risk factors by study wave and three socio‐economic measures at the time of birth: area‐level Indigenous Relative Socioeconomic Outcomes (IRSEO) index score and location (urban, remote) of residence, and parity of mother.
Results: Area‐level IRSEO of residence at birth influenced BMI (P < 0.001), systolic blood pressure (P = 0.024), LDL‐cholesterol (P = 0.010), and HDL‐cholesterol levels (P < 0.001). Remoteness of residence at birth influenced BMI (P < 0.001), HDL‐cholesterol (P < 0.001), and triglyceride levels (P = 0.043). Mother's parity at birth influenced BMI (P = 0.039).
Conclusions: Our longitudinal life course analyses indicate that area‐level socio‐economic factors at birth influence the prevalence of major cardiovascular disease risk factors among Indigenous Australians during childhood and early adulthood.