The known Rural background, rural interest, and rural exposure during medical training have each been associated with increased likelihood of medical students entering rural practice after graduation.
The new Pre-existing interest does not reliably translate into rural practice by graduates who have not participated in a rural clinical school during training.
The implications Rural clinical schools are critical to any effective strategy for increasing the proportion of local graduates participating in the rural workforce.
Whether their rural origin, their initial intention to practise in a rural location, or their rural experience is most important for enticing medical graduates into the rural medical workforce is of critical interest. If a medical student’s intention when entering medical school is the primary determinant, expensive immersion programs during training may be less important than careful selection and rural streaming after graduation.
International studies suggest that both nature (rural origin and pre-existing rural interest) and nurture (rural experience) could be important, but the data are contradictory. A study in the United States found that factors known at medical school entry (rural origin, general practice intention, rural intention) were strongly associated with rural practice three decades after graduation.1 In contrast, an Australian study found that graduates who had undertaken an extended rural placement were more than three times as likely to express interest and twice as likely to enter a rural internship as rural background medical students from the same school,2 suggesting that experience is the key factor. Other investigators have reported that rural background and exposure are independent predictors of later rural practice.3,4
It is therefore not clear how rural background, rural intention, and medical school experience interact when medical students eventually decide to practise in a rural location. Nor is it clear whether students who enter rural medical school programs do so because of an existing rural intention that commits them to rural work, or whether an ambivalent interest might be converted during medical training into practice.
This question was partly addressed by an Australian study5 which found that the rural work choices of students who had expressed interest in rural immersion by applying to a rural clinical school (RCS) but did not progress to rural placement were indistinguishable from those of students who were not interested or did not apply. This suggested that interest alone was not sufficient, and that longitudinal rural experience was necessary for converting interest into practice.
The Australian Medical Deans Outcomes Database (MSOD) project (http://www.medicaldeans.org.au/projects-activities/msodproject) can provide more robust evidence. During 2006–2012, name-identified demographic and intentions data were routinely collected from all students entering Australian medical schools, 25% of whom later entered an RCS. The Australian Health Practitioner Regulation Agency (AHPRA; http://www.ahpra.gov.au) maintains an annually updated record of principal place of practice for all health practitioners, and workforce choices can be identified for each graduate in its registry. Linking the MSOD and AHPRA databases provides a seamless overview of intentions, experience, and practice over time.
On the basis of MSOD data, Jones and colleagues6 found that students with a rural intention were more likely to be interested in general practice (odds ratio [OR], 5.5), to come from a rural background (OR, 2.5), and to be rurally bonded (OR, 2.0), and argued that these students were likely to exhibit workforce choices consistent with their initially expressed interest. These findings were confirmed by an analysis of entry demographic data and postgraduate survey data for 4038 respondents from 20 Australian medical schools.7 The authors found that medical students with positive rural intentions at entry were six times as likely to be interested in rural work, and more likely to actually work rurally at postgraduate year (PGY) 1 (OR, 1.38) or PGY 3 (OR, 1.86) than those without an initial rural intention. The authors concluded that medical school selection is a key workforce factor.
The relative contributions of rural background, intention, and experience to actual rural practice outcomes have not previously been assessed concurrently. Our study is therefore the first to examine all three variables in a representative medical school.
Methods
Participants
The participants were University of Western Australia medical students who completed the MSOD Commencing Medical School Questionnaire (CMSQ) during 2006–2010 and had graduated by the end of 2014, ensuring that by 2016 they were in at least their second year in the workforce.
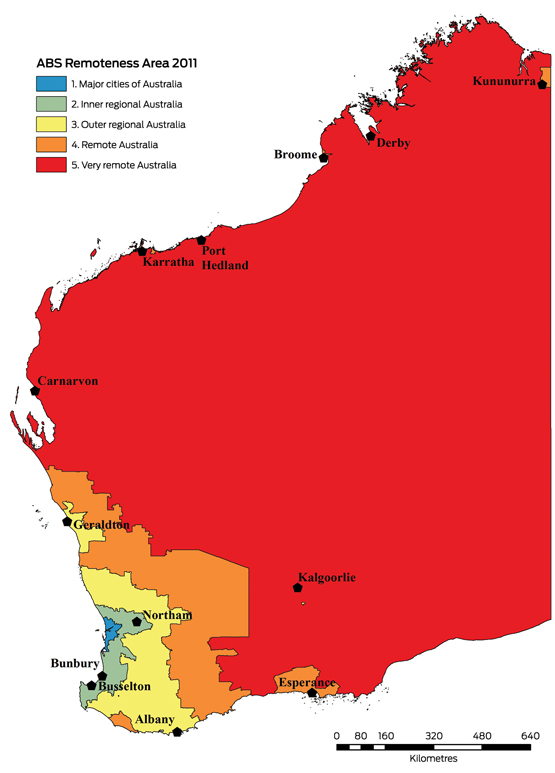
To obtain an RCS position, undergraduate medical students were required to submit a written application and to undergo a standardised interview. All students who had passed the preceding academic year and were not international students were eligible; academic results were not otherwise relevant to selection. RCS students were distributed in groups of 3–12 to sites in areas classified as Australian Standard Geographical Classification – Remoteness Areas (ASGC-RAs)8 2–5 (Box 1), where they remained in a longitudinal integrated clerkship9 for one academic year in the penultimate year of their training program.
Socio-demographic factors
Variables previously shown to be significantly related to rural work in this cohort10 were retained for analysis, including rural background, country of birth, sex, age at completion of training, and socio-economic status of home town.
Students were identified as being of rural origin if their principal home address had been in an ASGC-RA 2–5 for at least 5 years (consecutive or cumulative) from the commencement of primary school.11 As a socio-economic indicator, the correspondence postcode at entry for each student was linked with the Index of Relative Socio-economic Advantage and Disadvantage (IRSAD) score from the 2006 Socio-Economic Indices for Areas (SEIFA).12 A substantial proportion of the medical student cohort were born overseas but entered the course with Australian citizenship or permanent residency, and were therefore eligible to apply for placement in the RCS. Students’ countries of birth were classified according to the major regional groups outlined in the Standard Australian Classification of Countries,13 dichotomised into Oceania (Australia, New Zealand, Papua New Guinea, proximate Pacific islands) and Other. A number of students were enrolled in one of two schemes that obliged them to a return of service after graduation in either a rural, regional or remote area (the Medical Rural Bonded Scholarship Scheme, MRBS) or in a “district of workforce shortage” (the Bonded Medical Places Scheme, BMP).
Outcome variable: participation in the rural workforce
In April 2016, each graduate’s current principal workplace location was identified in the AHPRA database, and designated rural (ASGC-RA 2–5) or urban (ASGC-RA 1). All students who completed the CMSQ and were currently practising in Australia were cross-matched with their AHPRA registration status.
Statistical analysis
Data were analysed in SPSS Statistics 20.0 (IBM) and SAS 9.4 (SAS Institute). The socio-demographic profiles of students who did or did not complete the CMSQ were compared in χ2 tests for categorical variables. The statistical significance of key demographic variables for predicting current location of practice (ASGC-RA 1 v ASGC-RA 2–5) were assessed by univariate logistic regression. Statistically significant predictors were then entered into a multivariate logistic regression model. Backward stepwise elimination removed non-significant factors (P > 0.2). Interactions between independent variables were assessed to ensure that multi-collinearity was not a problem. Interaction between the three key variables of rural origin, rural intent, and RCS participation on rural workforce outcome was also examined.
Ethics approval
The study was approved by the University of Western Australia Human Research Ethics Committee (reference, RA/4/1/1627).
Results
Of 885 students from the University of Western Australia who commenced medical school during 2006–2010 and completed the CMSQ (82 students did not complete the questionnaire), 13 graduates could not be identified in the AHPRA database, two were overseas or not practising medicine, 69 had withdrawn from medical school, 111 were international medical students, and 121 were provisionally registered; 569 eligible graduates were therefore included in our study. Not all participants who completed the CMSQ answered the questions about rural intent or general practice intent, so that 508 graduates were included in the final multivariate analysis.
There were no statistically significant differences between students who were currently working (according to AHPRA) who did or did not complete the CMSQ during 2006–2010 for any variable previously found to be related to rural work (data not shown). Marital status and entry intentions regarding general or rural practice were available only in the CMSQ data, and could therefore not be compared.
Rural clinical school students
Differences between RCS and non-RCS graduates previously reported10 were confirmed (Box 2), suggesting that our CMSQ subset included valid samples of the two groups. There was a strong relationship between rural origin and socio-economic disadvantage (P < 0.001).
Rural practice outcome
In the univariate analysis, students of rural origin were four times as likely as urban origin students to practise rurally after graduation (OR, 4.3; 95% confidence interval [CI], 2.4–7.8); those from the most advantaged backgrounds were less likely to do so (for each IRSAD quintile: OR, 0.6; 95% CI, 0.4–0.7). RCS participants were more than twice as likely as other students to work rurally (OR, 2.3; 95% CI, 1.3–4.1), while those with an entry intention to work rurally were more than three times as likely to actually do so (OR, 3.4; 95% CI, 1.8–6.4) (Box 3).
After backward stepwise logistic regression, only two variables significantly predicted rural workforce participation: graduates from a rural background were almost four times as likely as urban origin graduates (OR, 3.9; 95% CI, 2.1–7.2) and RCS participants nearly twice as likely as non-RCS participants (OR, 1.9; CI, 1.0–3.5) to practise rurally (Box 3).
When the data were re-analysed using the Modified Monash Model14 instead of ASGC-RA categories to define urban and rural locations, the results were similar (online Appendix).
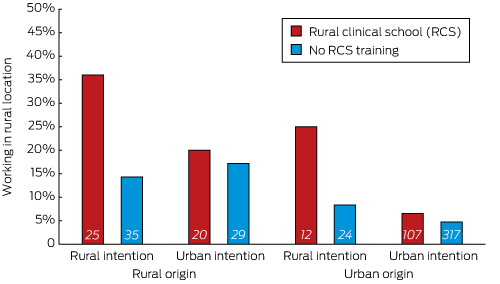
Interaction between entry intention and RCS experience on rural practice outcome
When entry intention was taken into account, the interaction between the effects of intention, RCS training and rural work on practice location became apparent. Both rural and urban origin students with rural intention at entry were more likely to work rurally only if they had also trained in an RCS (Box 4).
All three factors were therefore examined concurrently in the multivariate model for rural workforce outcome. The interaction between intention and RCS participation was significant (P < 0.001), and was not influenced by the background of the students (P = 0.54).
For students with a rural intention at the start of medical school, RCS training significantly increased the likelihood of later rural practice (OR, 3.57; 95% CI, 1.25–10.2; P = 0.017). For students without a rural intention, however, RCS participation did not significantly affect their practising rurally (OR, 1.38; 95% CI, 0.61–3.16; P = 0.44).
Conversely, RCS students who had a rural intention at entry were more than five times as likely to practise rurally as those who did not have this intention (OR, 5.29; 95% CI, 2.00–13.9). In contrast, rural intention had no statistically significant additive effect in predicting rural work for non-RCS students (OR, 2.05; 95% CI, 0.82–5.12).
Discussion
We found that the strong association between entry intention and final workplace location identified in other studies7 appears to be mediated for both urban and rural origin graduates by participation in an RCS. Indeed, the significant association between entry rural intention and participation in an RCS in our univariate analysis indicates that the RCS essentially recruits students who entered medical school with rural practice intentions. Further, RCS experience increases fivefold the likelihood that those with a pre-existing intention later choose rural practice. RCS participation thus appears to be the decisive factor in deciding to practise in a rural location. These findings are consistent with our earlier study,5 which found that the rural practice choices of students who applied for RCS training but did not progress to rural placement did not differ from those of students who did not apply.
RCS experience did not affect the workforce choices of students without an initial rural intention. This group may include students, of rural or urban origin, who apply for RCS training because of its educational benefit (hands-on experience, close longitudinal supervision).15
We found that only rural origin and RCS participation independently predicted a rural location for practice during PGY 2–5, consistent with other reports of additive effects of rural background and longitudinal, integrated immersion in rural practice during training.3,4 Contrary to the conclusions of Rabinowitz and colleagues,1 this indicates that more is needed to encourage rural practice than strategic selection into medical school. Although selecting students with rural intent is important, additional rural exposure during training increases the likelihood of taking up rural practice. Our data are consistent with other findings that participation in an RCS is strongly correlated with future rural work,2 but also suggest more complex interactions with entry intention and rural background.
Reviews of rural medical workforce distribution programs by the Australian Department of Health report that 20% of medical practitioners work in areas categorised as ASGC-RA 2–5.16 However, a substantial proportion of these practitioners are international medical graduates (IMGs), and this proportion has been growing more rapidly in Western Australia than in any other state. In the eight years to 2008, the number of IMGs working in rural areas increased by 38%; while they comprised 5% of all GPs in ASGC-RA 1 areas, 25% of those in ASGC-RA 4–5 regions were IMGs.16 The 2008 report for the federal Department of Health and Ageing noted that Rural Health Workforce Australia “estimates that from the 2011 medical student pool of approximately 3000 graduates, only 80 (or 2.7%) will pursue rural careers.”16 That nearly 9% of the PGY 2–5 graduates in our study resided in rural locations is therefore encouraging.
It should also be noted that MRBS and BMP recipients comprise a substantial subgroup of students who will potentially join the rural workforce, and their contribution is likely to become significant when they reach a more advanced stage in their training and begin their return-of-service obligations to rural and districts of workforce shortage locations.
The strong rural background effect we identified is a universal finding.1,3,4 In contrast to Jones and colleagues, who found no locality-specific social, environmental or economic factor effects on intention, and suggested that the rural background effect was reduced for those from lower socio-economic backgrounds,17 we found that socio-economic disadvantage was strongly related to both rural background and subsequent rural work. This connection has been discussed, although not demonstrated, by other investigators in Australia,18 the United States,19 and the United Kingdom;20 in an American study, it was found that graduates who had grown up in underserved areas were 1.6 times as likely to work with underserved populations.21 Our findings suggest that medical students’ experience of disadvantage in a rural environment before medical school may be a powerful personal motivator that influences medical school and graduate work choices.
Only graduates who had completed the MSOD CMSQ were included in our study, but 78% of the potentially eligible cohort — 508 of 651 students, after excluding international students (who could not enrol in the RCS) and those who subsequently withdrew from the course — provided full responses. As there were no significant differences between the demographic features of our cohort and those who did not complete the questionnaire, there is no reason to suspect a selection bias. Our data are drawn from a single clinical school offering a range of longitudinal integrated clerkship typologies;11 further studies are required to examine the effects of specific RCS types. Finally, our study focused on a single point in time, but longitudinal analysis suggests that graduates who have recently entered the rural workforce are highly mobile.22,23 Further investigations of their work patterns are needed, studies which might also assess additional factors that have been related to rural work choices, such as their partners’ backgrounds.24
In conclusion, we found that, in addition to the effect of rural background, there is an interaction between interest and participation in an RCS that influences later decisions about working in a rural location. Rural background, rural intention and rural experience during medical school all need to be factored into programs for redressing deficits in rural workforce levels.
Box 1 – Rural Clinical School of Western Australia sites and Australian Bureau of Statistics (ABS) Standard Geographical Classification – Remoteness Areas, 2011
Box 2 – Demographic data for medical students who commenced medical studies and completed the Commencing Medical School Questionnaire (2006–2010), whose location of work in 2016 was registered with the Australian Health Practitioner Regulation Agency
|
|
Location in penultimate year of study |
P* |
|||||||||||||
|
Rural clinical school |
Urban clinical school |
||||||||||||||
|
|
|||||||||||||||
|
Number of students |
164 |
405 |
|
||||||||||||
|
Country of birth (Oceania) |
141 (86.0%) |
293 (72%) |
< 0.001 |
||||||||||||
|
Sex (women) |
114 (69.5%) |
229 (56%) |
0.005 |
||||||||||||
|
Rural origin |
45 (27%) |
64 (16%) |
0.002 |
||||||||||||
|
Home town IRSAD (quintile) |
|
|
0.002 |
||||||||||||
|
1–2 |
1 (0.6%) |
4 (1%) |
|
||||||||||||
|
3–4 |
11 (6.7%) |
8 (2%) |
|
||||||||||||
|
5–6 |
39 (24%) |
60 (15%) |
|
||||||||||||
|
7–8 |
19 (12%) |
73 (18%) |
|
||||||||||||
|
9–10 |
94 (57%) |
260 (64%) |
|
||||||||||||
|
Medical Rural Bonded Scholarship recipient |
9 (6%) |
16 (4.0%) |
0.50 |
||||||||||||
|
Bonded Medical Place recipient |
34 (21%) |
88 (22%) |
0.82 |
||||||||||||
|
Entry intention to practise rurally |
37† (26%) |
59‡ (16%) |
0.017 |
||||||||||||
|
Entry intention to practise in a general practice or Aboriginal Health Service |
20§ (12%) |
35¶ (8.8%) |
0.22 |
||||||||||||
|
Aged 25 or more at completion of medical degree |
80 (49%) |
205 (51%) |
0.71 |
||||||||||||
|
Rural practice location, 2016 |
23 (14%) |
27 (6.7%) |
0.008 |
||||||||||||
|
Inner regional |
7 |
11 |
|
||||||||||||
|
Outer regional |
9 |
11 |
|
||||||||||||
|
Remote |
7 |
5 |
|
||||||||||||
|
|
|||||||||||||||
|
IRSAD = Index of Relative Socio-economic Advantage and Disadvantage; 1 = most disadvantaged, 10 = most advantaged. * χ2 test. Missing values (no answer provided): † 19; ‡ 38; § 3; ¶ 5. |
|||||||||||||||
Box 3 – Univariate and multivariate analyses of predictors of rural practice (ASGC-RA 2–5)
|
Characteristic |
Univariate analysis |
Multivariate analysis |
|||||||||||||
|
Odds ratio (95% CI) |
P |
Odds ratio (95% CI) |
P |
||||||||||||
|
|
|||||||||||||||
|
Country of birth: Oceania (v other) |
2.11 (0.88–4.58) |
0.10 |
|
|
|||||||||||
|
Sex: women (v men) |
1.45 (0.81–2.59) |
0.21 |
|
|
|||||||||||
|
Origin: rural (v urban) |
4.29 (2.35–7.83) |
< 0.001 |
3.91 (2.12–7.21) |
< 0.001 |
|||||||||||
|
Home town IRSAD: per quintile |
0.57 (0.44–0.74) |
< 0.001 |
|
|
|||||||||||
|
Scholarship |
|
|
|
|
|||||||||||
|
Medical Rural Bonded Scholarship |
2.06 (0.68–6.24) |
0.20 |
|
|
|||||||||||
|
Bonded Medical Place |
1.48 (0.77–2.84) |
0.24 |
|
|
|||||||||||
|
Clinical school: rural medical school (v other) |
2.28 (1.27–4.12) |
0.006 |
1.93 (1.05–3.54) |
0.034 |
|||||||||||
|
Entry intention to practise rurally (v none) |
3.42 (1.82–6.43) |
< 0.001 |
|
|
|||||||||||
|
Entry intention to practise in a general practice or Aboriginal Health Service (v none) |
3.39 (1.94–7.95) |
< 0.001 |
|
|
|||||||||||
|
Age at completion of training: ≥ 25 years (v ≤ 24 years) |
1.42 (0.79–2.55) |
0.24 |
|
|
|||||||||||
|
|
|||||||||||||||
|
ASGC-RA = Australian Standard Geographical Classification – Remoteness Areas; IRSAD = Index of Relative Socio-economic Advantage and Disadvantage; 1 = most disadvantaged, 10 = most advantaged. |
|||||||||||||||
Received 30 November 2016, accepted 9 May 2017
- Denese Playford1
- Hanh Ngo1
- Surabhi Gupta1
- Ian B Puddey2
- 1 The Rural Clinical School of Western Australia, University of Western Australia, Perth, WA
- 2 University of Western Australia, Perth, WA
We acknowledge the statistical advice of Sharon Evans, senior biostatistician, and the support of David Atkinson, head of the Rural Clinical School of Western Australia.
No relevant disclosures.
- 1. Rabinowitz H, Diamond J, Markham F, et al. The relationship between entering medical students’ backgrounds and career plans and their rural practice outcomes three decades later. Acad Med 2012; 87: 493-497.
- 2. Clark T, Freedman SB, Croft AJ, et al. Medical graduates becoming rural doctors: rural background versus extended rural placement. Med J Aust 2013; 199: 779-782. <MJA full text>
- 3. Playford D, Evans S, Atkinson D, et al. Impact of the Rural Clinical School of Western Australia on work location of medical graduates. Med J Aust 2014; 200: 104-107. <MJA full text>
- 4. Kondalsamy-Chennakesavan S, Eley DS, Ranmuthugal G, et al. Determinants of rural practice: positive interaction between rural background and rural undergraduate training. Med J Aust 2015; 202: 41-45. <MJA full text>
- 5. Playford DE, Puddey IB. Interest in Rural Clinical School is not enough: participation is necessary to predict an ultimate rural practice location. Aust J Rural Health 2016; doi: http://dx.doi.org/10.1111/ajr.12324 [Epub ahead of print].
- 6. Jones M, Humphreys J, Prideaux D. Predicting medical students’ intentions to take up rural practice after graduation. Med Educ 2009; 43: 1001-1009.
- 7. Herd MS, Bulsara MK, Jones MP, et al. Preferred practice location at medical school commencement strongly determines graduates’ rural preferences and work locations. Aust J Rural Health 2016; 25: 15-21.
- 8. Australian Bureau of Statistics. 1216.0 Australian Standard Geographical Classification (ASGC), Jul 2008. Updated Sept 2009. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/1216.0Jul%202008?OpenDocument (accessed Feb 2016).
- 9. Worley P, Couper I, Strasser R, et al; Consortium of Longitudinal Integrated Clerkships (CLIC) Research Collaborative. A typology of longitudinal integrated clerkships. Med Educ 2016; 50: 922-932.
- 10. Puddey IB, Mercer A, Playford DE, Riley GJ. Medical student selection criteria and socio-demographic factors as predictors of ultimately working rurally after graduation. BMC Med Educ 2015; 15: 74.
- 11. Australian Government, Department of Health. Rural Health Multidisciplinary Training (RHMT) 2016-2018 — Programme Framework. http://www.health.gov.au/internet/main/publishing.nsf/content/rural-health-multidisciplinary-training-program-framework (accessed Feb 2017).
- 12. Australian Bureau of Statistics. 2039.0. 2039. Information paper: an introduction to Socio-Economic Indexes for Areas (SEIFA), 2006. Updated Mar 2009. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/2039.0Main+Features12006?OpenDocument (accessed Feb 2017).
- 13. Australian Bureau of Statistics. 1269.0. Standard Australian Classification of Countries (SACC), 2011. Updated May 2015. http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/1269.0main+features102011 (accessed Feb 2016).
- 14. Australian Government, Department of Health. Rural classification reform: frequently asked questions [webpage]. DoctorConnect; no date. http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/Classification-changes (accessed June 2017).
- 15. Walters L, Greenhill J, Richards J, et al. Outcomes of longitudinal integrated clinical placements for students, clinicians and society. Med Educ 2012; 46: 1028-1041.
- 16. Deloitte Access Economics. Review of the rural medical workforce distribution programs and policies. Report for the Department of Health and Ageing; Aug 2011. https://www.health.gov.au/internet/main/publishing.nsf/Content/foi-disc-log-2011-12/$File/FOI%20235-1011%20document%201.pdf (accessed Mar 2017).
- 17. Jones M, Humphreys JS, McGrail MR. Why does a rural background make medical students more likely to intend to work in rural areas and how consistent is the effect? A study of the rural background effect. Aust J Rural Health 2012; 20: 29-34.
- 18. Larkins S, Michielsen K, Iputo J, et al. Impact of selection strategies on representation of underserved populations and intention to practise: international findings. Med Educ 2015; 49: 60-72.
- 19. Odom Walker K, Ryan G, Ramey R, et al. Recruiting and retaining primary care physicians in urban underserved communities: the importance of having a mission to serve. Am J Public Health 2010; 100: 2168-2175.
- 20. Tiffin PA, Dowell JS, McLachlan JC. Widening access to UK medical education for under-represented socioeconomic groups: modelling the impact of the UKCAT in the 2009 cohort. BMJ 2012; 344: e1805.
- 21. Rabinowitz HK, Diamond JJ, Veloski JJ, et al. The impact of multiple predictors on generalist physicians’ care of underserved populations. Am J Public Health 2000; 9: 1225-1228.
- 22. Playford D, Ng W, Burkitt T. Redistributing the medical workforce: creation of a mobile rural workforce following undergraduate longitudinal rural immersion. Med Teach 2016; 38: 498-503.
- 23. McGrail M, Russell DJ, Campbell DG. Vocational training of general practitioners in rural locations is critical for the Australian rural medical workforce. Med J Aust 2016; 205: 216-221. <MJA full text>
- 24. Laven G, Beilby JJ, McElroy HJ, Wilkinson D. Factors associated with rural practice among Australian-trained general practitioner. Med J Aust 2003; 179: 75-79. <MJA full text>





Abstract
Objective: To compare the influence of rural background, rural intent at medical school entry, and Rural Clinical School (RCS) participation on the likelihood of later participation in rural practice.
Design: Analysis of linked data from the Medical School Outcomes Database Commencing Medical Students Questionnaire (CMSQ), routinely collected demographic information, and the Australian Health Practitioner Regulation Agency database on practice location.
Setting and participants: University of Western Australia medical students who completed the CMSQ during 2006–2010 and were practising medicine in 2016.
Main outcome measures: Medical practice in rural areas (ASGC-RAs 2–5) during postgraduate years 2–5.
Results: Full data were available for 508 eligible medical graduates. Rural background (OR, 3.91; 95% CI, 2.12–7.21; P < 0.001) and experience in an RCS (OR, 1.93; 95% CI, 1.05–3.54; P = 0.034) were significant predictors of rural practice in the multivariate analysis of all potential factors. When interactions between intention, origin, and RCS experience were included, RCS participation significantly increased the likelihood of graduates with an initial rural intention practising in a rural location (OR, 3.57; 95% CI, 1.25–10.2; P = 0.017). The effect of RCS participation was not significant if there was no pre-existing intention to practise rurally (OR, 1.38; 95% CI, 0.61–3.16; P = 0.44).
Conclusion: For students who entered medical school with the intention to later work in a rural location, RCS experience was the deciding factor for realising this intention. Background, intent and RCS participation should all be considered if medical schools are to increase the proportion of graduates working rurally.