Cardiovascular disease remains a major cause of premature death in Aboriginal and Torres Strait Islander (Indigenous) people,1 accounting for almost a third of the gap in life expectancy between Indigenous and non-Indigenous Australians. A much higher burden of cardiovascular disease in Indigenous people has been well documented, as well as significant disparities in and barriers to cardiac care, compared with the non-Indigenous population. The reasons for these disparities are complex and multifactorial and include the burden of social determinants of health, cultural safety, communication problems and systemic problems of poor access to care.2 These factors have been discussed elsewhere in this issue and in previous publications in the Journal.3
Despite these challenges, clinicians committed to improving Indigenous health outcomes can play an important role in facilitating and delivering evidence-based and culturally appropriate clinical care for Indigenous people who are at high risk of, or already experiencing, cardiac conditions. In this review, we focus on practical considerations based on our own experience and that of others who have been delivering cardiac care for Indigenous people in urban, rural and remote settings.
Ischaemic heart disease
An understanding of the clinical and social context is important in delivering optimal care to any target population. Compared with non-Indigenous Australians, Indigenous people have a very high burden of cardiovascular risk factors, including higher prevalences of smoking (40% v 18%), diabetes (18% v 5%) and living in remote areas (28% v 5%). Other more common risk factors include hypertension, obesity, chronic kidney disease and psychosocial stress.1,3 This risk factor burden is directly related to the low socio-economic status of the Indigenous population.1 It translates into a significantly higher incidence of ischaemic heart disease (IHD), with associated increases in morbidity and mortality, compared with the non-Indigenous population (Box 1).4 Control of risk factors is challenging and requires an empowered and supported primary care team working together with specialists through outreach services or telehealth.
Care considerations
Early diagnosis of IHD and provision of evidence-based therapy are essential to improving clinical outcomes for Indigenous people, but they can be hindered by several barriers.
Indigenous patients are at risk of premature coronary artery disease and it is not unusual for this to present in patients in their late 20s or early 30s.5 Therefore, even in young patients, all cardiac symptoms such as chest discomfort should be taken seriously and investigated. Given that Indigenous patients with IHD are often young, their symptom tolerance is relatively high. A young patient with severe disease may deny symptoms until very late, resulting in late presentation, delayed treatment and a poor outcome. Routine functional testing, such as the 6 minute walk test or exercise stress testing, should be considered to objectively assess exercise tolerance for age.
Further, as Indigenous patients can be quiet and reluctant to talk about their symptoms, traditional history-taking methods may underestimate symptom severity and mask diagnosis. Clarification may be better achieved through indirect assessment using questions about lifestyle activities, such as ability to play football or participate in hunting, or through collateral history from family members.
Continuity of care from the same care providers is important in developing rapport with Indigenous patients. Positive therapeutic relationships can be achieved by arranging for the same cardiologist or physician to provide outreach clinics to a region for a prolonged period, with effective examples being described in specialist outreach programs in the Northern Territory.6
Use of local cardiac nurse coordinators for education, care coordination and case management of patients who have complex, high risk cardiovascular disease has reduced the likelihood of these patients being lost to follow-up. Primary care practitioners need access to a clinical support network infrastructure, such as the South Australian and NT acute coronary syndrome (ACS) support network, to provide early specialist advice for patients presenting with suspected IHD.7
Diagnosis
Diagnosis of IHD usually requires investigations beyond history, physical examination and a resting electrocardiogram (ECG). Stress electrocardiography8 or stress echocardiography are the minimal investigations needed to confirm or exclude significant IHD. Stress testing may not be suitable for Indigenous patients who are obese or who have musculoskeletal conditions or other comorbidities. Alternative diagnostic investigations, such as computed tomography coronary angiography, stress myocardial perfusion scanning or dobutamine stress cardiac ultrasound imaging, should be considered in these circumstances. Facilities for these investigations are usually located in metropolitan and major regional centres, presenting a further barrier to appropriate and timely investigations for Indigenous people living in remote areas. Issues of cost, transport and family responsibilities may prevent patients travelling for these investigations.2 The first presentation of IHD in Indigenous patients is therefore often when they present to hospital with an ACS.9,10
Management
Updated Australian clinical guidelines for the management of ACS, published in 2016, apply to all patients regardless of ethnicity or cultural background.11 However, disparities in ACS care for Indigenous people are well documented.12 Here, we present a practical application of the guidelines for use in the Indigenous setting.13
Indigenous patients who present to a health care facility with a suspected ACS must have access to a digital 12-lead ECG, which can, if necessary, be transmitted to a referral centre for assistance with decision making. Access to point-of-care troponin testing is also important for risk stratification and therapeutic decision making.
All patients with ST-segment elevation ACS presenting within 12 hours of symptom onset should receive reperfusion therapy with either percutaneous coronary intervention (PCI) or fibrinolytic therapy. PCI is preferred over fibrinolysis in patients with ST-segment elevation myocardial infarction if it can be performed within 90 minutes of first clinical contact. As Indigenous people frequently delay their presentation and may live remotely, fibrinolytic therapy may be the only therapeutic option. If systems are in place, prehospital fibrinolysis should be administered when timely access to a hospital is not possible.
All patients who present to a hospital without PCI capability should be transferred within 24 hours, if possible, to a PCI-capable hospital for angiography. Patients with non-ST-segment elevation ACS classified as high risk, with elevated troponin levels, dynamic ECG changes or ongoing symptoms, should undergo coronary angiography as soon as possible, with a view to revascularisation. There is considerable evidence that Indigenous people with ACS have lower rates of angiography and PCI than the non-Indigenous population.5,14 Factors responsible for this disparity include communication and language barriers, lack of coordinated care, failure to engage family members in discussions about recommended interventions, and a lack of cultural safety among health care providers. Clinicians should take time to explain invasive cardiac procedures, such as angiography, to Indigenous patients, and consider obtaining assistance from Aboriginal health workers and interpreters, with the use of visual charts and videos. Family meetings often aid therapeutic decision making.
It is important to respect the choices that Indigenous patients may make outside the recommendations of evidence-based guidelines. For example, an Indigenous patient may refuse to have cardiac surgery or PCI after an ACS episode because of anxiety relating to the procedure or social dislocation. It is not unusual for such patients, if given time for better understanding, to reconsider their decision and subsequently undergo delayed but appropriate therapy. Patient support should therefore continue through optimal medical therapy and subsequent close monitoring and follow-up.
Rehabilitation
Enrolment in cardiac rehabilitation programs is beneficial after ACS,13 but participation rates of Indigenous people are low. Reasons for this include distance, extended family responsibilities, socio-cultural inappropriateness of programs, poor understanding of cardiac rehabilitation and the younger age of the Indigenous population with ACS (as patients in their 20s or 30s are less compliant and less likely to accept clinical recommendations). Cardiac rehabilitation programs are not always available in outer regional and remote communities. When they are not accessible, provision of culturally appropriate education about necessary lifestyle changes can be effective. Better secondary prevention can also be achieved through innovative telehealth cardiac rehabilitation models of care, such as the use of text messaging.15,16
Rheumatic fever and rheumatic heart disease
With rising living standards, rheumatic fever has virtually disappeared among non-Indigenous Australians, but acute rheumatic fever (ARF) and secondary rheumatic heart disease (RHD) remain major problems in the Indigenous community17 and, to a lesser degree, urban Maori and Pacific Islander populations in Australia. The Indigenous population in the NT has the highest rates of ARF and RHD in the Western world.18 Rheumatic fever is a disease of disadvantage and is more likely to occur in Indigenous communities with a higher rate of poverty, inadequate housing with overcrowding, and lack of ready access to primary care. The diagnosis of ARF may be difficult unless significant valve disease is manifest at presentation. Echocardiography is essential to detect any cardiac involvement.
Clinical features
Many cases of ARF are subclinical, and the first presentation may be valvular heart disease manifesting as a heart murmur. ARF and RHD affect Indigenous Australians at a young age (in childhood and adolescence) and should be included in the differential diagnosis when evaluating all Indigenous patients with cardiac symptoms. Patients may downplay their symptoms for fear of hospitalisation and invasive treatments. For example, joint pains may be attributed to trauma rather than ARF to avoid long term benzathine penicillin G injections. Clinicians should have a low threshold for performing objective assessments, including blood tests for streptococcal serology and echocardiography.
Mitral regurgitation is the most common rheumatic valve lesion and is often accompanied by an eccentric regurgitation jet, which may best be heard posteriorly.19 The second most commonly affected valve in RHD is the aortic valve, with aortic regurgitation. Mitral stenosis may develop with recurrent episodes. It is not unusual for severe mitral stenosis to present similarly to an acute asthma attack, with ensuing misdiagnosis and bronchodilator treatment resulting in a poor clinical outcome. Unexplained dyspnoea in a young, pregnant Indigenous woman is also a red flag. The mitral stenosis murmur is often difficult to detect clinically. A high index of clinical suspicion and early echocardiography help to confirm or exclude the diagnosis.
Clinical examination may be difficult in young Indigenous patients. They are often shy and particularly sensitive to being examined by a clinician of the opposite sex. Use of a chaperone, typically an Aboriginal health worker or registered nurse, may be helpful.
The clinical features of these valve lesions are well documented.19 Echocardiography is an essential clinical tool in the diagnosis and management of RHD, but its availability outside major centres may be limited, leading to delays in diagnosis. Developing outreach echocardiography programs in areas of need is important.
It is not unusual for echocardiography to underestimate valve lesions due to images of suboptimal quality and eccentric regurgitation jets that compromise Doppler assessment. It is important to assess clinical signs of heart failure and pulmonary hypertension if valvular heart disease is suspected. When there is a discrepancy between clinical assessment and echocardiographic findings, further evaluation with transoesophageal echocardiography should be considered.
Management
Patients with established RHD or previously documented ARF should be given secondary prophylaxis with 4-weekly benzathine penicillin G injections to prevent recurrences.20 Adherence to these injections is highly variable in Indigenous communities and may be as low as 50% in remote areas of Australia. Community mobility and fear of needles are common reasons for avoiding injections. A well organised community monitoring and recall system needs to be in place to ensure that patients receive their regular injections. Recurrences of rheumatic fever are not uncommon in patients with poor medication adherence, leading to further valve damage.
Clinical management of valve disease in Indigenous patients does not differ from that in the non-Indigenous population. Heart failure is treated with diuretics, and advanced valve disease may require valve surgery, including replacement or repair. These complications require referral to major metropolitan centres with cardiac surgery facilities. A high proportion of female patients are of childbearing age, and the impact of RHD in pregnancy is significant, especially for women with mitral stenosis or mechanical valves. If surgery is indicated, mechanical valve replacement should be avoided in young women who are or may become pregnant because of the risk to the mother and fetus of warfarin therapy during pregnancy. These women should undergo either valve repair or bioprosthetic valve replacement. The latter option may require reoperative valve surgery in 5–10 years because of prosthetic valve degeneration. A well informed and collaborative decision-making process for choice of valve operation, including consultation with local health care providers regarding medication adherence, is essential for improving longer term outcomes.21,22
New oral anticoagulants should not be used in RHD patients with prosthetic valves, as they have been shown to be inferior to warfarin.23 As patients require ongoing warfarin therapy after mechanical valve replacement, those who have problems with medication adherence are at risk of the life-threatening complication of valve thrombosis, which can result in heart failure, stroke and death. Early warning signs include a history of non-adherence, documented subtherapeutic international normalised ratio (INR), worsening exertional dyspnoea and reduced intensity or absence of mechanical valve click during cardiac auscultation. Any of these findings should be considered a medical emergency and requires prompt administration of therapeutic anticoagulation with heparin, specialist consultation and urgent transfer to a tertiary cardiac facility for management. Prevention of valve thrombosis requires meticulous attention to monitoring and optimising therapeutic anticoagulation. This is best achieved with the use of point-of-care INR testing devices in a community health setting.24
Interstate travel for cardiac surgery often results in social dislocation and disruption for Indigenous patients. Some patients may refuse to travel and will instead choose alternative, suboptimal medical treatment options and to die closer to home. It is rare for Indigenous patients to undergo heart transplantation because of the prolonged social dislocation and problems with adherence.
Chronic cardiovascular disease
Although Indigenous people access cardiac care items on the Medicare Benefits Schedule at similar rates to non-Indigenous people, the burden of heart disease is much greater in the Indigenous population, meaning that Indigenous people are still underserviced compared with the non-Indigenous population (Box 1). Practical approaches to optimising cardiovascular care for Indigenous Australians are summarised in Box 2 and include focusing on appropriate supportive care, general comorbidities and specific cardiac comorbidities.
Supportive care
Long term follow-up after ACS has shown that outcomes for Indigenous patients are significantly less favourable than for non-Indigenous patients.10 The availability of a local nurse or health worker as a cardiac care coordinator has been shown to greatly improve the efficacy of long term follow-up care.25 Typical roles include arranging clinics, liaising with all health care providers and families involved in each patient’s case and following up patients who miss outpatient appointments.
Care close to home can be achieved through improving specialist outreach and telehealth consultations. Well established specialist outreach models of care exist in various jurisdictions.6 Despite the focus on remote communities, most Indigenous people live in metropolitan areas (Box 3),26 and specialists should also consider outreach clinics in metropolitan Aboriginal community-controlled health services, as patients are better supported and engaged in these settings than in hospital outpatient settings.27 Complementary use of telehealth in tandem with outreach models of care can add value to care and be cost-effective.28
Access barriers remain for Indigenous people who need regular, especially specialist, care for their chronic cardiovascular disease.2 These include distance to specialist medical centres, affordability and reluctance to attend mainstream outpatient health services because of perceived discrimination. Ambulatory cardiac care is best provided in an Aboriginal community-controlled environment with a visiting cardiology specialist and portable echocardiography capability. Once a specialist assessment has been made, follow-up care may be possible using telehealth methods, in conjunction with the primary health care practitioner. Again, continuity of care is important to Aboriginal patients, and using the same health care provider can enable culturally appropriate rapport and mutual understanding to develop.
General comorbidities
The burden of comorbidities is much greater and their age of onset earlier in the Indigenous population than in the non-Indigenous population. Many patients will have multiple comorbidities, such as diabetes, hypertension and chronic kidney disease.1 Other factors that may influence care are substance misuse (especially alcohol), tobacco use, mental health problems and medication adherence. A more holistic approach is needed to provide care to Indigenous people with cardiovascular disease, with attention directed towards these important non-cardiac factors as well as cardiovascular risk factors. A multidisciplinary case conference may assist in complex cases. Health practitioners involved in the care of patients with chronic cardiac disease should consider not only the cardiovascular system but also renal function, diabetes control and medication adherence. They need to work with Aboriginal health workers, cardiac nurse coordinators and family members to provide support and health education to the patient. Reasons for medication non-adherence, such as cost, access barriers and poor health literacy, need to be understood and overcome.29
Cardiac comorbidities
Chronic heart failure and hypertension occur at a younger age and are significantly more common in Indigenous people than in non-Indigenous people.30,31 Heart failure is most commonly due to coronary artery disease, but hypertension, dilated cardiomyopathy and RHD are other important causes. In one study from central Australia, about two-thirds of patients with heart failure had impaired left ventricular function and one-third had heart failure with preserved systolic function on echocardiography.30 Many of these patients had not been previously diagnosed. This finding indicates the need for a high index of clinical suspicion for possible heart failure and the need for access to echocardiography to assess left ventricular function in such populations.32 Atrial fibrillation occurs in younger people more often in the Indigenous Australian population than in the non-Indigenous population, but less commonly in older Indigenous people compared with non-Indigenous people.33 It is frequently associated with comorbidities such as hypertension and RHD. Indigenous patients with non-rheumatic atrial fibrillation tend to have a higher risk of stroke, as assessed by CHA2DS2-VASc score, than non-Indigenous patients, and often meet the criteria for anticoagulation therapy (CHA2DS2-VASc score ≥ 2).34
Given the high burden of heart disease, even at young ages, risk assessment should be routine for all Indigenous patients at any health facility contact. Clinicians should provide primary preventive approaches, such as brief interventions for smoking cessation and monitoring and optimisation of blood pressure and diabetes control. Routine health checks for Indigenous adults are practised in remote health centres in the NT.35
Conclusion
Indigenous Australians experience a disproportionately high burden of cardiovascular disease, resulting in significantly higher morbidity and mortality compared with non-Indigenous Australians. Although improvements in morbidity and mortality from cardiovascular disease have occurred over time in the Indigenous population, improvements have also occurred in the non-Indigenous population, such that the differential between the groups, although narrower, persists. A better understanding of both the factors contributing to adverse outcomes and potential mitigation strategies can assist clinicians in providing care to the Indigenous population. This includes understanding of cardiovascular disease presentations, realistic management approaches that are appropriate to the individual patient and support mechanisms applicable to Indigenous communities. Indigenous Australians deserve the same level of evidence-based cardiovascular health care and access to care as non-Indigenous Australians.36
Box 1 – Summary of results of Better Cardiac Care measures for Indigenous and non-Indigenous Australians*
|
Measure |
Age-standardised rate |
||||||||||||||
|
Indigenous |
Non-Indigenous |
||||||||||||||
|
|
|||||||||||||||
|
Indigenous-specific annual health assessments (MBS item 715), 2014–15 |
25% |
na |
|||||||||||||
|
Cardiac-related diagnostic items, 2014–15 |
4% |
4% |
|||||||||||||
|
Hospitalised events for ST-segment elevation myocardial infarction in adult patients treated with percutaneous coronary intervention, 2011–14 |
52% |
75% |
|||||||||||||
|
Hospitalised events for acute coronary syndrome in adult patients who received diagnostic angiography or definitive revascularisation, 2011–14 |
48% |
61% |
|||||||||||||
|
Hospitalised events for acute myocardial infarction in patients aged over 35 years that ended in death of the patient, 2009–14 |
4.4% |
4.0% |
|||||||||||||
|
People with cardiac disease with a Team Care Arrangement, 2014–15 |
24% |
13% |
|||||||||||||
|
People with cardiac disease with a General Practitioner Management Plan, 2014–15 |
27% |
16% |
|||||||||||||
|
People with cardiac disease with MBS allied health services, 2014–15 |
22% |
19% |
|||||||||||||
|
Incidence of acute rheumatic fever, 2011–2014 (per 100 000)† |
59 |
0.2 |
|||||||||||||
|
Benzathine penicillin G doses, 2014 (% receiving > 80% of doses)† |
37% |
29% |
|||||||||||||
|
Hospitalisations for cardiac conditions, 2011–14 (per 1000) |
25 |
13 |
|||||||||||||
|
Deaths due to cardiac conditions, 2009–2013 (per 100 000) |
208 |
128 |
|||||||||||||
|
In-hospital deaths of patients with cardiac conditions, 2009–14 (per 100 000) |
69 |
36 |
|||||||||||||
|
|
|||||||||||||||
|
MBS = Medicare Benefits Schedule. na = not applicable. * Based on Australian Institute of Health and Welfare material.4 † Data are not age-standardised. |
|||||||||||||||
Box 2 – Optimising cardiovascular care for Indigenous Australians
Routine comprehensive cardiovascular health assessment- Risk factors: smoking, dyslipidaemia, hypertension, diabetes, obesity, physical inactivity
- Cardiac conditions: ischaemic heart disease, heart failure, atrial fibrillation, rheumatic heart disease
- Comorbidities: chronic kidney disease, chronic airway disease, chronic mental illness, hazardous alcohol use, cancer
- Beware of atypical presentations at relatively young age
- Beware of low clinical yield of cardiac auscultations to determine valve lesions; use echocardiography
- Rationalise cardiac investigations based on local capacity and travel distance; use highly specific testing (eg, stress echocardiography instead of stress electrocardiography)
- Ensure patient- and family-centred care
- Understand the specific barriers to care:
- Socio-economic — use social worker or community support
- Language difficulty — use interpreter service and visual aids
- Shyness — use Aboriginal health worker or relative
- Remoteness — use telehealth or specialist outreach services to minimise travel and social dislocation
- Adherence problems — use Aboriginal health worker or relative
- Substance misuse or mental health problem — refer to appropriate support agencies
- Remember that primary prevention is key whenever possible
- Aim to achieve early detection and secondary prevention
- Use multidisciplinary care planning and care coordination for patients with complex or high risk cardiovascular disease
- Provide evidence-based therapies
- Encourage self-management
- Ensure close ongoing monitoring and support
- Communicate, collaborate and co-manage with other relevant specialist services
Box 3 – Geographic location of Indigenous and non-Indigenous populations, by remoteness, 30 June 2011
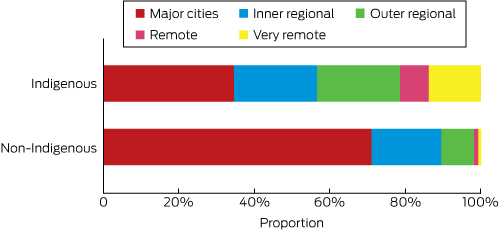
Source: Australian Institute of Health and Welfare.26
Provenance: Commissioned; externally peer reviewed.
- Warren F Walsh1
- Nadarajah Kangaharan2,3
- 1 Prince of Wales Hospital, Sydney, NSW
- 2 Royal Darwin Hospital, Darwin, NT
- 3 Alice Springs Hospital, Alice Springs, NT
No relevant disclosures.
- 1. Australian Institute of Health and Welfare. Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011 (AIHW Cat. No. BOD 7; Australian Burden of Disease Study Series No. 6). Canberra: AIHW, 2016. http://www.aihw.gov.au/publication-detail/?id=60129557110 (accessed May 2017).
- 2. Davidson PM, MacIsaac A, Cameron J, et al. Problems, solutions and actions: addressing barriers in acute hospital care for Indigenous Australians and New Zealanders. Heart Lung Circ 2012; 21: 639-643.
- 3. Brown A, Kritharides L. Overcoming cardiovascular disease in Indigenous Australians. Med J Aust 2017; 206: 10-12. <MJA full text>
- 4. Australian Institute of Health and Welfare. Better cardiac care measures for Aboriginal and Torres Strait Islander people: second national report 2016 (AIHW Cat. No. IHW 169). Canberra: AIHW, 2016. http://www.aihw.gov.au/publication-detail/?id=60129557610 (accessed May 2017).
- 5. Australian Institute of Health and Welfare. Coronary heart disease and chronic obstructive pulmonary disease in Indigenous Australians (AIHW Cat. No. IHW 126). Canberra: AIHW, 2014. http://www.aihw.gov.au/publication-detail/?id=60129547716 (accessed May 2017).
- 6. Gruen RL, Bailie RS, Wang Z, et al. Specialist outreach to isolated and disadvantaged communities: a population-based study. Lancet 2006; 368: 130-138.
- 7. Tideman PA, Tirimacco R, Senior DP, et al. Impact of a regionalised clinical cardiac support network on mortality among rural patients with myocardial infarction. Med J Aust 2014; 200: 157-160. <MJA full text>
- 8. Hurune PN, O’Shea JM, Maguire GP, Hewagama SS. Utility of exercise electrocardiography testing for the diagnosis of coronary artery disease in a remote Australian setting. Med J Aust 2013; 199: 201-204. <MJA full text>
- 9. National Heart Foundation of Australia and Australian Healthcare and Hospitals Association. Better hospital care for Aboriginal and Torres Strait Islander people experiencing heart attack. NFHA and AHHA, 2010. https://www.heartfoundation.org.au/images/uploads/publications/A-ATSI-Better-Hospital-Care-20110812.pdf (accessed Apr 2017).
- 10. Brown A. Acute coronary syndromes in Indigenous Australians: opportunities for improving outcomes across the continuum of care. Heart Lung Circ 2010; 19: 325-336.
- 11. Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Med J Aust 2016; 205: 128-133. <MJA full text>
- 12. Tavella RT, McBride K, Keech W, et al. Disparities in acute in-hospital cardiovascular care for Aboriginal and non-Aboriginal South Australians. Med J Aust 2016; 205: 222-227. <MJA full text>
- 13. Ilton MK, Walsh WF, Brown AD, et al. A framework for overcoming disparities in management of acute coronary syndromes in the Australian Aboriginal and Torres Strait Islander population: a consensus statement from the National Heart Foundation of Australia. Med J Aust 2014; 200: 639-643. <MJA full text>
- 14. Randall DA, Jorm LR, Lujic S, et al. Disparities in revascularization rates after acute myocardial infarction between Aboriginal and non-Aboriginal people in Australia. Circulation 2013; 127: 811-819.
- 15. National Health and Medical Research Council. Strengthening cardiac rehabilitation and secondary prevention for Aboriginal and Torres Strait Islander peoples: a guide for health professionals. Canberra: NHMRC, 2005. https://www.nhmrc.gov.au/guidelines-publications/ind1-ind2 (accessed Apr 2017).
- 16. Chow CK, Islam SM, Farmer A, et al. Text2PreventCVD: protocol for a systematic review and individual participant data meta-analysis of text message-based interventions for the prevention of cardiovascular diseases. BMJ Open 2016; 6: e012723.
- 17. Remond MG, Wheaton GR, Walsh WF, et al. Acute rheumatic fever and rheumatic heart disease — priorities in prevention, diagnosis and management. A report of the CSANZ Indigenous Cardiovascular Health Conference, Alice Springs 2011. Heart Lung Circ 2012; 21: 632-638.
- 18. Lawrence JG, Carapetis JR, Griffiths K, et al. Acute rheumatic fever and rheumatic heart disease: incidence and progression in the Northern Territory of Australia, 1997 to 2010. Circulation 2013; 128: 492-501.
- 19. RHDAustralia (ARF/RHD writing group), National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand. The Australian guideline for prevention, diagnosis and management of acute rheumatic fever and rheumatic heart disease (2nd edition). Darwin: Menzies School of Health Research 2012. https://www.rhdaustralia.org.au/node/950/attachment (accessed Apr 2017).
- 20. Australian Institute of Health and Welfare. Rheumatic heart disease and acute rheumatic fever in Australia: 1996–2012 (AIHW Cat. No. CVD 60; Cardiovascular Disease Series No. 36). Canberra: AIHW, 2013. http://www.aihw.gov.au/publication-detail/?id=60129542750 (accessed May 2017).
- 21. Finucane K, Wilson N. Priorities in cardiac surgery for rheumatic heart disease. Glob Heart 2013; 8: 213-220.
- 22. Alizzi AM, Knight JL, Tully PJ. Surgical challenges in rheumatic heart disease in the Australian Indigenous population. Heart Lung Circ 2010; 19: 295-298.
- 23. Eikelboom JW, Connolly SJ, Brueckmann M, et al; RE-ALIGN Investigators. Dabigatran versus warfarin in patients with mechanical heart valves. N Engl J Med 2013; 369: 1206-1214.
- 24. Dennis J, Majoni W, Tinsley J, Kangaharan N. Safety and efficacy of warfarin therapy in remote communities of the Top End of Northern Australia. Heart Lung Circ 2017. doi:10.1016/j.hlc.2017.01.004 [Epub ahead of print].
- 25. Jeremy R, Tonkin A, White H, et al. Improving cardiovascular care for Indigenous populations. Heart Lung Circ 2010; 19: 344-350.
- 26. Australian Institute of Health and Welfare. Indigenous observatory. The Indigenous population. http://www.aihw.gov.au/indigenous-observatory/reports/health-and-welfare-2015/indigenous-population (accessed May 2017).
- 27. Australian Institute of Health and Welfare. Healthy futures — Aboriginal community controlled health services report card 2016 (AIHW Cat. No. IHW 171). Canberra: AIHW, 2016. http://www.aihw.gov.au/publication-detail/?id=60129557721 (accessed May 2017).
- 28. Wade V, Stocks N. The use of telehealth to reduce inequalities in cardiovascular outcomes in Australia and New Zealand: a critical review. Heart Lung Circ 2017; 26: 331-337.
- 29. Davidson PM, Abbott P, Davison J, DiGiacomo M. Improving medication uptake in Aboriginal and Torres Strait Islander peoples. Heart Lung Circ 2010; 19: 372-377.
- 30. McGrady M, Krum H, Carrington MJ, et al. Heart failure, ventricular dysfunction and risk factor prevalence in Australian Aboriginal peoples: the Heart of the Heart Study. Heart 2012; 98: 1562-1567.
- 31. Wang Z, Knight S, Wilson A, et al. Blood pressure and hypertension for Australian Aboriginal and Torres Strait Islander people. Eur J Cardiovasc Prev Rehabil 2006; 13: 438-443.
- 32. National Heart Foundation of Australia. Multidisciplinary care for people with chronic heart failure: principles and recommendations for best practice. NHFA, 2010. https://www.heartfoundation.org.au/images/uploads/publications/Multidisciplinary-care-for-people-with-CHF.pdf (accessed Apr 2017).
- 33. Wong CX, Brooks AG, Cheng YH, et al. Atrial fibrillation in Indigenous and non-Indigenous Australians: a cross-sectional study. BMJ Open 2014; 4: e006242.
- 34. Katzenellenbogen JM, Teng THK, Lopez D. Initial hospitalisation for atrial fibrillation in Aboriginal and non-Aboriginal populations in Western Australia. Heart 2015; 101: 712-719.
- 35. Australian Institute of Health and Welfare. Indigenous health check (MBS 715) data tool. Canberra: AIHW, 2016. http://www.aihw.gov.au/indigenous-australians/indigenous-health-check-data-tool (accessed Apr 2017).
- 36. Brown A, O’Shea RL, Mott K, et al. Essential service standards for equitable national cardiovascular care for Aboriginal and Torres Strait Islander people. Heart Lung Circ 2015; 24: 126-141.





Summary