Aboriginal and Torres Strait Islander Australians (Indigenous Australians) bear a disproportionate burden of disease in Australia and have a life expectancy 13 years shorter than that of other Australians.1,2 Heart disease is the leading cause of death among both Indigenous and non-Indigenous Australians, and it is also the single largest contributor to the gap in life expectancy between the two populations.3,4 The mortality rate associated with cardiovascular disease is 60% higher in Indigenous than in non-Indigenous populations; the prevalence of cardiovascular disease is 30% higher and that of its risk equivalent, diabetes, is three times greater among Indigenous Australians.3-6
Promoting access to prescription drugs and improving the management of chronic disease are key components of the national strategy for reducing health disparities in Australia. In 1999, the Australian Government eliminated out-of-pocket drug costs for Indigenous patients attending remote Aboriginal community-controlled health clinics.7 Two subsequent initiatives, in 2008 and 2010, reduced medication co-payments for Indigenous patients who attended non-remote Aboriginal community-controlled clinics or mainstream general practices.8,9 Further, the Pharmaceutical Benefits Scheme modified its criteria for subsidised lipid-lowering medications to include all Indigenous Australians with diabetes or a blood total cholesterol level above 6.5 mmol/L.10 The Indigenous Practice Incentives Program of the federal Department of Health provides bonus payments to general practitioners who enrol chronically ill Indigenous patients and prepare chronic disease management plans for them.11
Whether these efforts have translated into increased prescribing of cardiovascular medications to Indigenous Australians or better control of cardiovascular risk factors is unknown. We therefore evaluated trends in the prescribing of lipid-lowering medications for Indigenous and non-Indigenous Australians seen in general practice. We focused on therapies that reduce blood lipid levels because treating this modifiable risk factor can reduce coronary events and mortality in selected patients.12,13
Methods
Study design, source of data and population
We conducted an observational time trend study, from April 2001 to March 2013, that determined the proportion of patient encounters in which GPs prescribed lipid-lowering medications. We analysed data from the Bettering the Evaluation and Care of Health (BEACH) survey, which randomly samples 1000 GPs each year.14 The source population included all registered GPs and GP registrars who had claimed at least 375 Medicare service items in the past 3 months.
Each participating GP provided information about 100 consecutive patient encounters. The BEACH survey collects reasons for the encounter, problems addressed during the encounter, and clinical actions undertaken to manage each problem. GPs record up to four medications for each problem managed, and link each medication with a single managed problem. The final study sample encompassed 759 673 GP encounters with patients aged 30 years or over: 9594 with Indigenous and 750 079 with non-Indigenous patients.
Outcome measures
The primary outcome was the report that at least one lipid-lowering medication had been prescribed during an encounter. Lipid-lowering medications included five classes: statins, bile acid sequestrants, fibrates, niacin, and cholesterol absorption inhibitors. The primary independent variable was Indigenous status (dichotomous: yes v no), based on the GP’s record of the patient’s self-report during the encounter.
Statistical analyses
We calculated the unadjusted rate of prescribing lipid-lowering medications (ie, the proportion of encounters at which at least one such medication was prescribed) for Indigenous and for non-Indigenous patients. These data were further stratified by time period (1 April 2001 – 31 March 2005, 1 April 2005 – 31 March 2009, 1 April 2009 – 31 March 2013) and by the clinical condition that was addressed during an encounter (non-gestational diabetes mellitus, hypertension, ischaemic heart disease, lipid disorder). We also calculated the age–sex standardised rate of prescription of lipid-lowering medications for Indigenous patients, using 14 discrete age–sex subgroups (men and women in seven age groups spanning 10 years each). Age–sex standardisation yields an estimate of the lipid-lowering prescribing rate for encounters with Indigenous patients, assuming an age–sex structure identical to that of the non-Indigenous population.
A further subgroup analysis calculated the proportions of all lipid-lowering medications prescribed for each specified clinical condition. To assess whether there were statistically significant increases over time in the age–sex standardised rate of prescribing of lipid-lowering medications, we constructed logistic regression models, with the time period (the three 4-year time periods) as the independent variable.
All analyses were adjusted for clustering by GP using SAS 9.3 survey procedures (SAS Institute). Differences were considered statistically significant at P < 0.05. For routine analyses of BEACH data, we report a significant difference only if there was no overlap of the 95% confidence intervals of the two comparison groups. This is a stricter threshold than the usual P < 0.05 criterion, equivalent to P < 0.006, and reduces the risk of Type 1 errors when making multiple comparisons.
The University of Sydney Human Research Ethics Committee approved the study (reference 2012/130).
Results
Rate of prescription of lipid-lowering medications for Indigenous and non-Indigenous patient encounters
During the study period, lipid-lowering medications were prescribed during 4.9% (95% CI, 4.2%–5.6%) of encounters with Indigenous patients, and at 4.6% (95% CI, 4.5%–4.7%) of encounters with non-Indigenous patients. After age–sex standardisation (which adjusts the Indigenous but not the non-Indigenous rate), the rate of prescription during Indigenous patient encounters was 5.5% (95% CI, 4.7%–6.3%), significantly greater than that for non-Indigenous patient encounters.
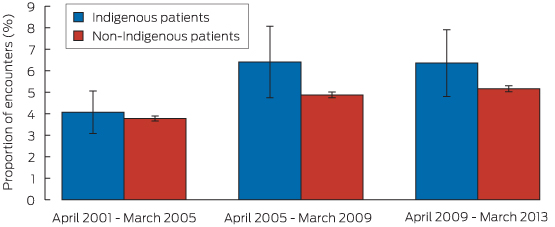
For Indigenous patient encounters, the age–sex standardised rate of prescription of lipid-lowering medications increased from 4.1% during 2001–2005 to 6.4% during 2009–2013 (P = 0.013 for trend). For non-Indigenous encounters, the rate of prescription increased from 3.8% to 5.2% over the same period (P < 0.01) (Box 1). The point estimates for these proportions were higher for Indigenous patient encounters for each of the three time periods, but these individual differences were not statistically significant.
Specified clinical conditions addressed during Indigenous and non-Indigenous patient encounters
Diabetes and ischaemic heart disease were significantly more commonly managed at encounters with Indigenous patients than at those with non-Indigenous patients: in age-standardised analyses, diabetes was managed at 13.8% (95% CI, 12.6%–15.1%) of encounters with Indigenous patients and at 4.7% (95% CI, 4.6%–4.7%) of encounters with non-Indigenous patients. Ischaemic heart disease was managed at 3.2% (95% CI, 2.6%–3.8%) of encounters with Indigenous patients and at 1.7% (95% CI, 1.7%–1.8%) of those with non-Indigenous patients. Lipid disorders were managed significantly less frequently during Indigenous encounters (3.8%; 95% CI, 3.1%–4.5%) than during non-Indigenous encounters (4.6%; 95% CI, 4.5%–4.7%). There was no significant difference between the proportions of encounters at which hypertension was managed (12.6% for each group).
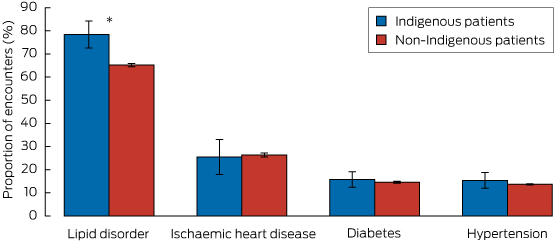
Rate of prescription of lipid-lowering medications, according to clinical condition
The proportion of Indigenous patient encounters involving diabetes, hypertension or ischaemic heart disease at which lipid-lowering medication was prescribed was similar to that for non-Indigenous patient encounters. However, for encounters at which GPs managed a lipid disorder, the age–sex standardised proportion at which lipid-lowering medication was prescribed was 78.4% (95% CI, 72.6%–84.2%) for Indigenous patient encounters, significantly greater than that for non-Indigenous patient encounters (65.2%; 95% CI, 64.5%–65.8%) (Box 2).
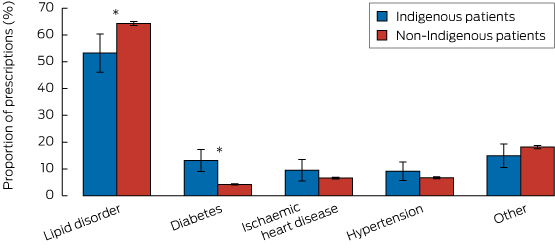
Proportion of lipid-lowering prescriptions linked with specific clinical conditions
Box 3 depicts the proportions of all 35 798 prescriptions for lipid-lowering medication according to the specified clinical conditions managed, and stratified by Indigenous status. Only the proportions linked with diabetes (Indigenous: 13.1% [95% CI, 9.1%–17.3%] v non-Indigenous: 4.2% [CI, 4.0–4.5]) and lipid disorders (Indigenous: 53.3% [95% CI, 46.1%–60.4%], v non-Indigenous 64.3% [95% CI, 63.5%–65.1%]) were significantly different between the two groups.
Discussion
There were three major findings from this nationally representative study of the prescribing of lipid-lowering medications for Indigenous and non-Indigenous adults managed in Australian general practice. First, the rates of prescription of lipid-lowering medication by GPs for both Indigenous and non-Indigenous Australians increased substantially from 2001–2005 to 2009–2013, with relative increases of 37% for non-Indigenous and 56% for Indigenous patients. Second, lipid-lowering medication was more likely to be prescribed at encounters with Indigenous patients than at those with non-Indigenous patients, including encounters at which lipid disorders were managed. Third, diabetes was about three times as likely to be managed at encounters with Indigenous patients.
We found that the rates of prescription of lipid-lowering medication were higher for all Indigenous patient encounters, and for encounters at which a lipid disorder was managed; the prescription rates at encounters during which diabetes, heart disease or hypertension were managed were similar for Indigenous and non-Indigenous patients. These findings may reflect extensive efforts by the Australian Government, clinicians and other stakeholders to identify and reduce cardiovascular risk among Indigenous people, to increase their access to medications, and to revise clinical and benefit guidelines for lipid-lowering prescriptions so that they include all Indigenous patients with diabetes or blood total lipid levels greater than 6.5 mmol/L.7-11 Our study cannot establish a causal link between these policies and increased prescribing of lipid-lowering agents. However, it is reassuring that, as lipid-lowering therapies have continued to diffuse into clinical practice over the past 15 years, we found no evidence that GPs were less likely to prescribe these agents to Indigenous patients.
As noted by other authors, screening for and managing cardiovascular risk in Australian general practice is suboptimal.15,16 It is therefore also possible that the equivalent prescribing rates may reflect underuse of these medications in both Indigenous and non-Indigenous patients who might benefit from these therapies. Future studies should characterise disparities in the proportion of clinically appropriate treatment candidates who are prescribed effective cardiovascular medications.
Our study has some limitations. First, the BEACH data do not include information on whether patients filled or adhered to lipid-lowering prescriptions. Second, data concerning managed conditions, medications prescribed, and the patient’s self-identified ethnicity may include errors, although we have no reason to believe that rates of misclassification changed over time. Third, the sample in our study included only patients seen in primary care. Fourth, the sample sizes for some subgroup analyses were small. Fifth, the data were collected at the encounter level, precluding calculation of the overall prevalence of lipid-lowering therapy in Indigenous and non-Indigenous populations. Finally, we lacked laboratory values and comprehensive data on comorbid conditions to determine the clinical appropriateness of prescribing decisions or to adjust for casemix.
In conclusion, we detected substantial increases in the rate of prescribing of lipid-lowering medication at encounters with both Indigenous and non-Indigenous patients in Australian general practice between 2001 and 2013, and found no evidence that Indigenous patients were less likely to be prescribed these agents. Indigenous patients were more likely than non-Indigenous patients to be prescribed lipid-lowering therapy during encounters at which a lipid disorder was managed. Our findings suggest some measure of success in expanding access to medications and reducing cardiovascular risk in Indigenous populations. Further efforts are needed to promote long-term adherence to effective medications and to improve cardiovascular health for Indigenous people in Australia.
Box 1 – Age–sex standardised proportions of patient encounters (with 95% CI) at which lipid-lowering medication was prescribed, by time period and Indigenous status
Received 18 June 2015, accepted 3 September 2015
- Amal N Trivedi1
- Allan J Pollack2
- Helena C Britt2
- Graeme C Miller2
- Christopher Harrison2
- Margaret A Kelaher3
- 1 Brown University, Providence, RI
- 2 Family Medicine Research Centre, University of Sydney, Sydney, NSW
- 3 Centre for Health Policy, University of Melbourne, Melbourne, VIC
This research was funded by the Commonwealth Fund and the Australian Department of Health.
Amal Trivedi has received consulting fees to edit the Merck Manual of Diagnosis and Therapy.
- 1. Hill K, Barker B, Vos T. Excess Indigenous mortality: are Indigenous Australians more severely disadvantaged than other Indigenous populations. Int J Epidemiol 2007; 36: 580-589.
- 2. Bramley D, Hebert P, Jackson R, Chassin M. Indigenous disparities in disease-specific mortality, a cross-country comparison: New Zealand, Australia, Canada, and the United States. N Z Med J 2004; 117: U1215.
- 3. Vos T, Barker B, Begg S, et al. Burden of disease and injury in Aboriginal and Torres Strait Islander Peoples: the Indigenous health gap. Int J Epidemiol 2009, 38: 470-477.
- 4. Zhao Y, Dempsey K. Causes of inequality in life expectancy between Indigenous and non-Indigenous people in the Northern Territory, 1981-2000: a decomposition analysis. Med J Aust 2006; 184: 490-494. <MJA full text>
- 5. Australian Institute of Health and Welfare 2015. Better Cardiac Care measures for Aboriginal and Torres Strait Islander people: first national report 2015. Canberra: AIHW, 2015. (AIHW Cat. No. 156.) http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129551949 (accessed Aug 2015).
- 6. Australian Institute of Health and Welfare. Prevalence of diabetes [website]. http://www.aihw.gov.au/diabetes-indicators/prevalence/ (accessed Aug 2015).
- 7. Kelaher M, Dunt D, Taylor-Thompson D, et al. Improving access to medicines among clients of remote area Aboriginal and Torres Strait Islander Health Services. Aust N Z J Public Health 2006; 30: 177-183.
- 8. Couzos S, Sheedy V, Delaney Thiele D. Improving Aboriginal and Torres Strait Islander people’s access to medicines — the QUMAX program. Med J Aust 2011; 195: 62-63. <MJA full text>
- 9. Australian Government. Department of Health Services. Closing the Gap — PBS Co-payment Measure. http://www.medicareaustralia.gov.au/provider/pbs/prescriber/closing-the-gap.jsp (accessed Aug 2015).
- 10. Luke JN, Brown A, O’Neal DN, et al. Lipid treatment guidelines and cardiovascular risk for Aboriginal people in Central Australia. Med J Aust 2009; 190: 552-556. <MJA full text>
- 11. Australian Government. Department of Health and Ageing. Practice Incentives Program. Indigenous Health Incentive guidelines — February 2014. http://www.humanservices.gov.au/spw/health-professionals/services/practice-incentives-programme/resources/indigenous-health-pip-guidelines.docx (accessed Aug 2015).
- 12. Grundy SM, Cleeman JI, Merz CN, et al. for the Coordinating Committee of the National Cholesterol Education Program. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation 2004; 110: 227-239.
- 13. American Diabetes Association. Dyslipidemia management in adults with diabetes. Diabetes Care 2004; 27: s68-s71.
- 14. Britt H, Miller GC, Henderson J, et al. General practice activity in Australia 2013–14. General practice series 36. Sydney: Sydney University Press, 2014. http://ses.library.usyd.edu.au/bitstream/2123/11882/4/9781743324226_ONLINE.pdf (accessed Aug 2015).
- 15. Webster RJ, Heeley EL, Peiris DP, et al. Gaps in cardiovascular disease risk management in Australian general practice. Med J Aust 2009; 191: 324-329. <MJA full text>
- 16. Peiris DP, Patel AA, Cass A, et al. Cardiovascular disease risk management for Aboriginal and Torres Strait Islander peoples in primary health care settings: findings from the Kanyini Audit. Med J Aust 2009; 191: 304-309. <MJA full text>





Abstract
Objective: To examine the prescribing of lipid-lowering medications during general practitioner encounters with Indigenous and non-Indigenous Australians from 2001 to 2013.
Design, setting and participants: Observational time trend study, using data from the Bettering the Evaluation and Care of Health (BEACH) survey, of 9594 primary care encounters with Indigenous patients and 750 079 encounters with non-Indigenous patients aged 30 years or over.
Main outcome measure: Prescription of at least one lipid-lowering medication.
Results: The age–sex standardised proportion of encounters that resulted in at least one lipid-lowering medication being prescribed was 5.5% (95% CI, 4.7%–6.3%) for Indigenous patients and 4.6% (95% CI, 4.5%–4.7%) for non-Indigenous patients. The proportion of encounters with Indigenous patients at which a lipid-lowering medication was prescribed increased significantly from 4.1% during 2001–2005 to 6.4% during 2009–2013 (P = 0.013 for trend). For encounters with non-Indigenous patients, the proportion increased significantly from 3.8% during 2001–2005 to 5.2% during 2009–2013 (P < 0.01). For encounters during which GPs managed diabetes, hypertension or ischaemic heart disease, the proportion of Indigenous encounters during which lipid-lowering medication was prescribed was similar to that for non-Indigenous patients. For encounters in which GPs managed a lipid disorder, however, the age–sex standardised proportion was significantly greater for Indigenous (78.4%; 95% CI, 72.6%–84.2%) than for non-Indigenous patients (65.2%; 95% CI, 64.5%–65.8%).
Conclusion: We detected substantial increases in the prescribing of lipid-lowering medications from 2001 to 2013 for both Indigenous and non-Indigenous patients seen in Australian general practice. Providers were more likely to prescribe lipid-lowering medications for Indigenous than for non-Indigenous patients, suggesting some measure of success in expanding access to medications and reducing cardiovascular risk among Indigenous people.