Have you ever wondered what makes a good research paper? Since 1995, the best original research paper published each year in the Medical Journal of Australia (MJA), as judged by the Journal’s Content Review Committee, has been awarded the MJA/Wyeth Research Award. To date, 12 papers have won the award ($10 000 and a commemorative trophy), representing a diverse range of research methodologies, practice settings, professional disciplines, and subsequent citation rates (Box 1).
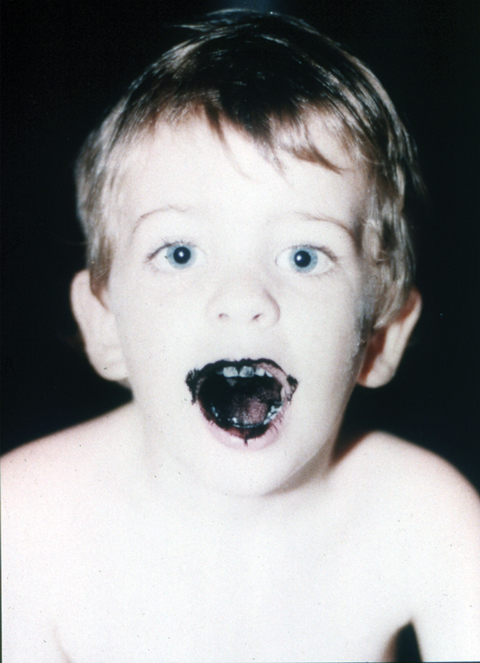
At that time, the treatment of overdose was quite empirical, and Pond set about collecting evidence for the ways in which charcoal could be used to remove poisons. Adapting the well known tradition of self-experimentation, Pond co-opted a couple of her six children to test out “easy” formulations of activated charcoal (Box 2).
Pond returned to Australia in the 1980s, where the opportunity arose, at Princess Alexandra Hospital in Brisbane, to challenge the long-established routine care for poisoning through a prospective, randomised controlled trial, comparing activated charcoal with a combination regimen of gastric emptying plus charcoal. In designing the study, Pond spent a long time talking with an American toxicologist, Ken Kulig, who had reported that acutely poisoned patients could be effectively treated without gastric emptying. Pond wanted to build on Kulig’s earlier research but without running into the same pitfalls: insufficient patient numbers and allocation bias.1
Published in the MJA in October 1995, it did not take long for the study results to filter through to clinical practice — in 1997, the American Academy of Clinical Toxicology issued a position statement on ipecac syrup, which concluded that gastric emptying by ipecac should not be administered routinely in the management of poisoned patients.2
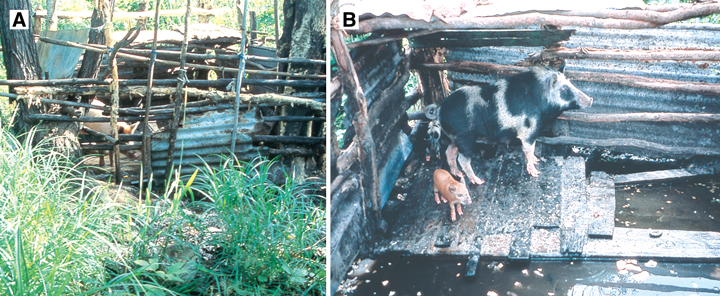
The researchers speculated that migratory birds and/or windblown mosquitoes had imported the virus into the Torres Strait, possibly from Papua New Guinea, and that a combination of environmental factors — including large numbers of domestic pigs kept in “wet” pigpens close to human dwellings and mosquito-breeding sites (Box 3) — had facilitated the outbreak.
Hanna and colleagues have continued to publish papers on disease outbreaks, including the 1998 JE outbreak and the Noah Beach malaria outbreak in Far North Queensland;3,4 the cross-agency collaboration continues to this day.
Several years earlier, while working in a melanoma clinic in San Francisco, Kelly had been involved in a case–control study that found that MDN were a strong and independent risk factor for the development of melanoma.5 “It seemed logical that if these people were most at risk for melanoma, then they were the people to put into a follow-up program to find the melanoma in the future”, Kelly said.
With others, Kelly has conducted further research along similar lines with a new cohort of patients, confirming the previous findings and showing that a new or changed pigmented lesion is more likely to be a melanoma in patients older, rather than younger, than 50 years of age.6
Internationally, photographic surveillance is now the standard practice in managing people with MDN.
Hensley, with co-researchers, has gone on to publish related papers about indoor air quality, including the effects of environmental tobacco smoke and bronchial reactivity among children,7,8 and is now Dean of Medicine at the University of Newcastle.
Today, aggressive public health approaches to STIs are considered the “norm” in Aboriginal communities. On the AP Lands, this program and others, like women’s health and child immunisation programs, continue to operate. New STI program initiatives continue to emerge, like Ushma Scales’ song about condom use, Take your shield to town, with lyrics in Pitjantjatjara.9
“Endorsement, intellectually, of chronic preventable disease strategies is no longer the issue; now, it’s resources and staffing to execute them in remote areas where the people have disastrous disease profiles”, said Hoy. After handover of the treatment program to the local health board in the Tiwi Islands, the intensity of the program declined and compliance with medicines use fell for a time, due to inadequate resources.10
A before–after time-series study suggested that quality of care at the hospital did improve as a result of the project.11 This evidence was soon bolstered when hard outcomes data on inhospital deaths, from the Queensland Hospitals Admitted Patient Data Collection, came to Scott’s attention. Using this state-based data, Scott and colleagues were able to demonstrate a significant reduction in the mortality rate for AMI at Ipswich Hospital, from 12.5% in 1994–1995 (pre-intervention) to 8.8% in 1996–1999 (post-intervention). The rates at a group of control hospitals in Queensland showed no significant change (remaining at about 12.8%) over the same period of time.
The quality improvement interventions have now been rolled out, with beneficial effects, across more Queensland hospitals.12 “I think it’s been a real success story. We’ve gone from a small community hospital to a collaborative of about 21 hospitals across the state, accounting for close to 80% of all AMI admissions.”
Now based at Brisbane’s Princess Alexandra Hospital, Scott has continued to pursue further quality improvements in relation to the management of AMI and heart failure. Recently, together with colleagues, he reported on “risk–treatment mismatching”, where much more treatment goes to lower- or moderate-risk patients than high-risk patients.13
The study has been presented and cited not only nationally but internationally, leading to ongoing relationships with doctors and educational videomakers in the US. A “Sharing the true stories” website has been developed, with links to further education resources (Box 4). There is also now greater systematic use of interpreters in Indigenous health settings.
The paper has had an impact in several key areas. Firstly, thanks to NACCHO’s advocacy role, said Couzos, remote area Aboriginal health services can now provide non-ototoxic ear drops to their clients for free, under Section 100 of the National Health Act 1953 (Cwlth). Secondly, the trial was pivotal to the listing of ototopical fluoroquinolone drops on the Pharmaceutical Benefits Schedule, which means that health care providers in non-remote areas can also provide subsidised medicine. Australian prescribing recommendations have also endorsed the use of fluoroquinolone ear drops in the presence of tympanic membrane perforation.14,15 Finally, in terms of research policy, the NACCHO Ear Trial has provided a real-world example of successful, community-based participatory research.16
“Here was an Australian industry initiative; here was a large public health problem and an opportunity to collaborate. It was a very attractive proposition”, said Campbell. After gaining some initial data from a small trial conducted in a high-risk group setting in Western Australia,17 the research partnership was granted National Health and Medical Research Council (NHMRC) funding for an open-label randomised controlled trial, conducted at the RMH in 2000.
But there is good news too. Recognising that pressure ulcers are a clinical indicator of quality of care, the Victorian Quality Council identified their reduction as a key objective for health care services in Victoria. Since state-wide surveys of the prevalence of pressure ulcers within Victoria’s acute and subacute health services began in 2003, progress has been made in implementing elements of a comprehensive program of pressure ulcer prevention and management. There has been a 33% reduction in the proportion of patients with pressure ulcers, from 26.5% in 2003 to 17.6% in 2006.18
Around the same time, while in Geneva at a World Health Organization meeting, Johnson arranged to meet Didier Pittet, who had recently published a landmark Swiss study in the Lancet showing that when staff regularly used a hand hygiene solution before and after every patient, contact rates of hospital infections, including MRSA, could be substantially cut.19 The “secret” of encouraging staff to use the solution was to include, along with the antibacterial alcohol and chlorhexidine, an emollient to protect the skin.
Pittet encouraged the Austin Health group to develop a similar program, and so they did — the multifaceted Operation Clean Start (OCS) program — developing their own hand hygiene solution (DeBugTM) and even adapting the concept of the “talking walls” (Box 5). The hospital staff and, in particular, nurses in infection control were incredibly supportive of OCS. “After we’d introduced it [the program] in one area, there was a real demand to introduce it into the next area, and so on. It just took off like wildfire”, said Johnson.
It is still early days since publication. Although local practice has changed on the beaches where the study was conducted, national changes in clinical practice as a result of this study are yet to be fully implemented. However, Isbister hopes that the Australian Resuscitation Council’s recent adoption of the new evidence in their treatment recommendations will mean hot water immersion becomes more widely available, and that cost and safety issues related to installing hot-water plumbing at surf lifesaving clubs around Australia can be resolved. And, after all, people can control the way they choose to treat their own jellyfish stings.20
While healing the tympanic membrane will improve hearing, if you have recurrent infections because your living circumstances aren’t right, then using ear drops will not totally solve the problem. It will create an environment where healing can occur, but the solution to Aboriginal health problems is not just medicines. Although improved access to medicines is vital, the solutions are holistic.
1 The Medical Journal of Australia/Wyeth Research Award-winning articles, 1995–2006, with ISI citations to date*
Received 17 October 2007, accepted 31 October 2007
- 1. Kulig K, Bar-Or D, Cantrill SV, et al. Management of acutely poisoned patients without gastric emptying. Ann Emerg Med 1985; 14: 562-567.
- 2. Krenzelok EP, McGuigan M, Lheur P. Position statement: ipecac syrup. American Academy of Clinical Toxicology; European Association of Poisons Centres and Clinical Toxicologists. J Toxicol Clin Toxicol 1997; 35: 699-709.
- 3. Hanna JN, Ritchie SA, Phillips DA, et al. Japanese encephalitis in north Queensland, Australia, 1998. Med J Aust 1999; 170: 533-536.
- 4. Hanna JN, Ritchie SA, Eisen DP, et al. An outbreak of Plasmodium vivax malaria in Far North Queensland, 2002. Med J Aust 2004; 180: 24-28. <MJA full text>
- 5. Holly EA, Kelly JW, Shpall SN, Chiu SH. Number of melanocytic nevi as a major risk factor for malignant melanoma. J Am Acad Dermatol 1987; 17: 459-468.
- 6. Banky JP, Kelly JW, English DR, et al. Incidence of new and changed nevi and melanomas detected using baseline images and dermoscopy in patients at high risk for melanoma. Arch Dermatol 2005; 141: 998-1006.
- 7. Hensley MJ, Chalmers A, Clover K, et al. Symptoms of asthma: comparison of a parent-completed retrospective questionnaire with a prospective daily symptom diary. Pediatr Pulmonol 2003; 36: 509-513.
- 8. Gibson PG, Simpson JL, Chalmers AC, et al. Airway eosinophilia is associated with wheeze but is uncommon in children with persistent cough and frequent chest colds. Am J Respir Crit Care Med 2001; 164: 977-981.
- 9. Nganampa Health Council. Programs — STD. http://www.nganampahealth.com.au/std.php (accessed Nov 2007).
- 10. Hoy WE, Kondalsamy-Chennakesavan SN, Nicol JL. Clinical outcomes associated with changes in a chronic disease treatment program in an Australian Aboriginal community. Med J Aust 2005; 183: 305-309. <MJA full text>
- 11. Scott IA, Eyeson-Annan ML, Huxley SL, West MJ. Optimising care of acute myocardial infarction: results of a regional quality improvement project. J Qual Clin Pract 2000; 20: 12-19.
- 12. Scott IA, Darwin IC, Harvey KH, et al. Multisite, quality-improvement collaboration to optimise cardiac care in Queensland public hospitals. Med J Aust 2004; 180: 392-397. <MJA full text>
- 13. Scott IA, Derhy PH, O’Kane D, et al. Discordance between level of risk and intensity of evidence-based treatment in patients with acute coronary syndromes. Med J Aust 2007; 187: 153-159. <MJA full text>
- 14. Black RJ, Cousins VC, Chapman P, et al. Ototoxic ear drops with grommet and tympanic membrane perforations: a position statement [letter]. Med J Aust 2007; 186: 605-606. <MJA full text>
- 15. Antibiotic Expert Group. Therapeutic guidelines. Antibiotic. 13th ed. Melbourne: Therapeutic Guidelines Limited, 2006: 236-240.
- 16. Couzos S, Lea T, Murray R, Culbong M. ‘We are not just participants — we are in charge’: the NACCHO ear trial and the process for Aboriginal community-controlled health research. Ethn Health 2005; 10: 91-111.
- 17. McGowan S, Montgomery K, Jolley D, Wright R. The role of sheepskins in preventing pressure ulcers in elderly orthopaedic patients. Primary Intention 2000; 8: 127-134.
- 18. Strachan V, and Clinical Epidemiology and Health Services Evaluation Unit, Melbourne Health. PUPPS 3 — Pressure ulcer point prevalence survey. Statewide report 2006. Melbourne: Victorian Department of Human Services, 2006. http://www.health.vic.gov.au/pressureulcers/pupps.htm (accessed Nov 2007).
- 19. Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet 2000; 356: 1307-1312.
- 20. Avorn J. The sting of ignorance [op-ed]. The New York Times 2006; 16 Sep.






We would like to thank Wyeth Australia for their generous support of this award for the past 12 years, and the interviewees for their time and willing participation.
None identified.