The ear health and hearing check (EHHC) recommendations presented in this article are for primary health care practitioners, to guide effective assessment of ear health and hearing status of Aboriginal and Torres Strait Islander children aged under 6 years attending primary care who are not known to have, or are not being actively managed for, ear health and hearing problems. A national expert panel provided cultural, clinical and research expertise during the development process. The recommendations complement the clinical management guidance provided in the Otitis media guidelines for Aboriginal and Torres Strait Islander children.1
The prevalence of recurrent or persistent otitis media (OM) in Aboriginal and Torres Strait Islander children remains among the highest globally.2 This prevalence is attributed to social and environmental factors that are a legacy of colonisation, racism, and disempowering government policies, including economic disadvantage, difficulty in accessing affordable and culturally appropriate health care, and lack of access to adequate housing that supports good health.3,4 Until these determinants are addressed, the ear health and hearing status of Aboriginal and Torres Strait Islander children will remain a matter of concern for years to come.
In addition, recurrent or persistent OM can limit children's developmental potential. For Aboriginal and Torres Strait Islander children, OM often starts in early infancy 5,6 without acute or obvious symptoms,1 and persists throughout childhood.7 This is the sensitive period for development — a time window in which early sensory experiences lay the foundation for cognitive, social and behavioural development.8 Persistent OM‐related hearing loss significantly reduces this experience, negatively impacting developmental outcomes, quality of life, family harmony, school readiness, and transmission of cultural and linguistic knowledge.9,10,11,12,13
To avoid these negative impacts, early detection is essential. The current OM guidelines recommend ear checks at every visit to primary health care,1 but in practice, checks are more often prompted by parent/carer concern than clinician initiated.8,13
These recommendations were motivated by the enormous variations in provision, components and timing of EHHCs for Aboriginal and Torres Strait Islander children in primary health care, and in identification of OM.14,15,16 Despite indications that a more systematic approach may be effective,17,18 no consensus has existed on the components or timing of EHHCs for Aboriginal and Torres Strait Islander children, or for similar populations experiencing high rates of early onset, persistent OM.15
Methods
The development of these recommendations was led by Aboriginal and non‐Indigenous researchers experienced in health research with Aboriginal and Torres Strait Islander people. Researcher expertise included Aboriginal health, primary health care and general practice, public health, hearing and communication science, and otolaryngology.
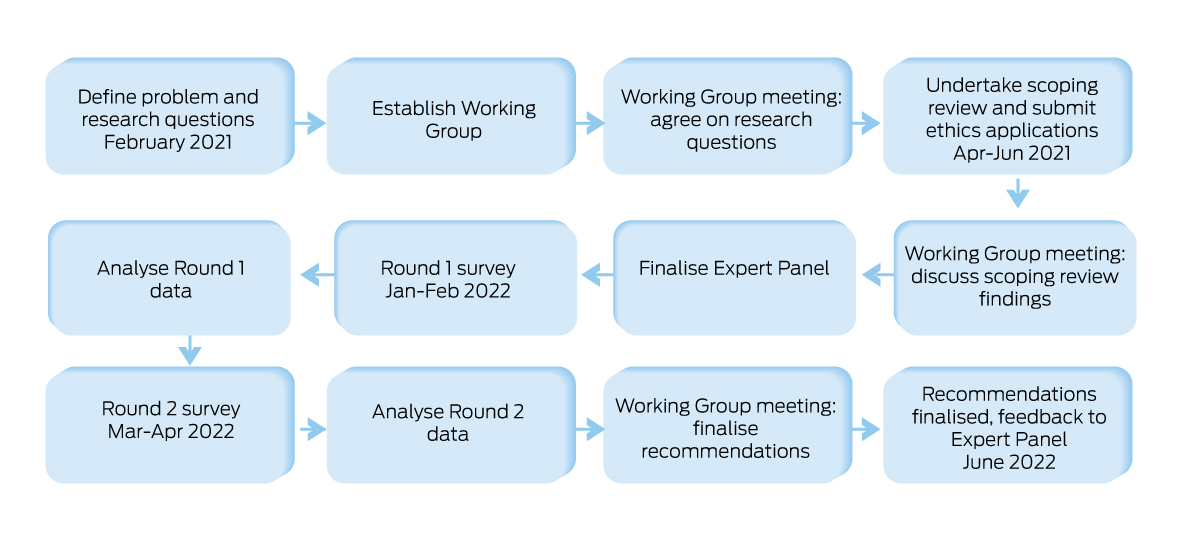
The project process is shown in Box 1. The process included a scoping review and a modified e‐Delphi consensus‐building process, described in a forthcoming methodology paper. A working group, comprising 22 experts from the Aboriginal and Torres Strait Islander community‐controlled and mainstream primary health, ear health, and hearing sectors, guided the project. Ten members were Aboriginal and/or Torres Strait Islander, and 13 worked in primary health.
The scope of the review was agreed with the working group. The review examined evidence on: (i) the effectiveness of tools for checking ear health and hearing in children aged under 6 years; (ii) existing recommendations on components and timing of such checks; and (iii) information on the feasibility of implementation in primary health care. Evidence sources included systematic reviews, meta‐analyses, randomised controlled trials, and single studies, as well as existing guidelines, health resources, and policy guidance. The quality of the evidence was assessed using the GRADE framework.19 Four EHHC domains were identified, which provided structure for the draft recommendations.
A national expert panel was assembled for the modified‐Delphi component of the process,20 comprising working group members and 57 invited experts from the Aboriginal and mainstream primary health care, hearing, specialist ear health, and relevant research sectors. Twenty‐three percent of panel members were Aboriginal and/or Torres Strait Islander; 61% worked in primary health care, 49% of whom were from the community‐controlled sector. All Australian states, territories and remoteness areas were represented.
Ethics approvals for the Delphi study were received from the Aboriginal Health and Medical Research Council (New South Wales) (1858/21), the Western Australian Aboriginal Health Ethics Committee (HREC1108), the Aboriginal Health Research Ethics Committee (South Australia) (04‐21‐944), the Menzies School of Health Research (Northern Territory) (HREC 2021‐4137), and the Hearing Australia Human Research Ethics Committee (HAHREC 2021‐07).
Eight draft EHHC recommendations and eight draft goals were presented to the expert panel via an online survey. Each recommendation was presented with a summary of evidence and a rationale. Panel members were invited to provide comment and to indicate on a five‐point Likert scale their level of agreement with each goal and recommendation (from “strongly disagree” to “strongly agree”), and rate feasibility for each recommendation (from “not feasible at all” to “very feasible”). An a priori consensus level of 80% was set — that is, consensus would be reached when 80% or more of the panel indicated “agree” or “strongly agree” (common practice in Delphi methodology21). Responses were anonymous; 82% of the expert panel took part in the first survey.
At first survey closure, panel members’ ratings and comments were analysed. Re‐drafted recommendations and analyses were presented in a second survey; 65% of the panel participated. Consensus was achieved for seven draft recommendations (Box 2) and for all goals (Box 3). Draft recommendations on the inclusion of audiometry in EHHCs did not reach consensus. A general recommendation on the role of audiometry in primary health care, aligning with the OM guidelines,1 was subsequently agreed upon by working group members. Expert panel members attended one of two online feedback sessions to discuss the recommendations and strategies for dissemination and implementation.
Recommendations
Eight proposed EHHC goals reached a high level of consensus agreement (Box 4). No additional goals were identified. Each recommendation is presented with indications of strength and certainty of evidence, levels of agreement, feasibility of implementation, evidence summaries, and rationales.
Domain: Parent and carer‐reported history, concerns, signs, and symptoms
As part of routine EHHCs, it is recommended that primary health care practitioners ask parents/carers about their child's ear health (recent and longer term), and any concerns about their child's ear health, hearing or communication.
Summary of evidence. Accuracy of caregiver‐reporting of signs and symptoms as a predictor of OM varies widely.22,23,24,25 Parent/carer concern correctly identifies children with OM 17–83% of the time, and correctly identifies children without OM 36–93% of the time.23 Ability of caregivers to correctly identify hearing loss is also low (sensitivity, 6.0–19.7%), with positive predictive values of 22.0–82.1%.22,23,26,27 However, most reviewed guidelines recommend investigating parent/carer concerns.28,29,30,31,32,33
Rationale for recommendation. Although parent/carer concern does not reliably predict ear health22,23,24,34 and hearing status,26,27 it should routinely be enquired about during checks because, when concern is expressed, a proportion of parents/carers will be correct.30,35 Following up on parent/carer concerns acknowledges the importance of their observations and advocacy for their child's health and wellbeing, and increases the likelihood that parents/carers feel respected and listened to. Although consensus was not reached on a specific timeframe (eg, 3 months, 6 months), there was consensus that “recent and longer term” would be meaningful to clinicians and parents/carers.
When persistent OM is diagnosed, specialist assessment and care is recommended.1 If documented ear health history is incomplete or unavailable, parent/carer report of ear health history may assist with differentiating OM subtypes.
No recommendations were developed relating to signs and symptoms: OM presents with a wide range, both ear‐specific and general,1,24,28,34,36 and one common subtype is largely asymptomatic.37
Domain: Listening and communication skills checklists
From the age of 6 months, review children's listening and communication skills development with parents/carers using appropriate questionnaires or checklists.
Summary of evidence. Listening skills checklists vary considerably in their ability to correctly identify current hearing loss (sensitivity, 100% and 39%) and to correctly identify no current hearing loss (specificity, 75% and 93%), with positive predictive values of 7% and 78%.38,39 A listening skills questionnaire developed for Aboriginal and Torres Strait Islander children reported normative data, but lacked information on sensitivity, specificity, and positive predictive values.40 Very low overall certainty of evidence may relate to the emergent nature of listening skills checklists in EHHCs. It is known that past or current auditory deprivation is associated with delays in listening skills development.41
Rationale for recommendation. Listening skills checklist results may reflect past and/or current access to auditory information. Results may be useful for differentiating transient and persistent OM and for flagging developmental risks that are not assessed by other components of the EHHC. Assessing parent/carer observations of their child's listening behaviours reinforces the importance of hearing in child development and builds parent/carer knowledge of the behaviours to watch for and nurture. Results should be interpreted as part of a broader clinical battery that includes objective ear health assessments and parent/carer observations.
Domain: Ear health
Examine appearance of the ear canal and ear drum, and assess movement of the ear drum and middle ear using either simple otoscopy plus tympanometry or pneumatic otoscopy. Use of video otoscopy is suggested for health promotion purposes with parents/carers, and/or for sharing images with other health care practitioners.
Summary of evidence. OM guidelines consistently recommend assessment of ear appearance (otoscopy) and mobility (pneumatic otoscopy or tympanometry)1,30,31,32 for accurate middle ear assessment. All reviewed guidelines recommended tympanometry.28,29,31,32,33,42,43,44 One study reported accuracy of tympanometry in correctly identifying OM (sensitivity, 56%), in correctly identifying no OM (specificity, 96%), and probability that tympanometry will correctly identify a middle ear condition (positive predictive value, 60%).45 One guideline recommended tympanometry over pneumatic otoscopy, for feasibility reasons.44 No studies considered sensitivity, specificity, or positive predictive values for pneumatic otoscopy as in most studies this was the comparator. There was no direct evidence for the advantages of pneumatic otoscopy over tympanometry. Two guidelines suggested video otoscopy was valuable for building parent/carer engagement in, and understanding of, ear health.29,42
Rationale for recommendation. Assessment of appearance and movement are consistently recognised as essential for accurate evaluation of ear health and diagnosis of OM, and are fundamental components of EHHCs for Aboriginal and Torres Strait Islander children.
Domain: Hearing sensitivity
Otoacoustic emissions (OAE) testing is suggested to confirm or exclude normal or near‐normal hearing when equipment is available, primary health practitioners have capability and are confident to use it, and there is a local preference for using OAE testing.
Summary of evidence. A systematic review of eight studies showed that OAEs correctly identify children aged 3–18 years with hearing loss 57–100% of the time, and without hearing loss 47–96% of the time.46 Wide variations relate to factors including choice of pass/refer thresholds and environmental noise. Screener training and experience potentially affects accuracy, the extent to which was not reported.46 Almost all studies were not done in primary health care.46 When present, emissions infer normal or near‐normal hearing, useful for children whose hearing cannot be behaviourally assessed, particularly those aged younger than 3 years.1,43
Rationale for recommendation. A conditional recommendation to use OAE testing to infer or exclude normal or near‐normal hearing did not reach consensus. Feedback from primary health practitioners who use OAEs was positive, but concerns remained about use, interpretation and feasibility in primary health care. A conditional recommendation for OAE testing as an optional component of EHHCs reached consensus.
Audiometry is recommended as per the OM guidelines1 when there are parent/carer and/or practitioner concerns about ear health, hearing, or communication; and/or the child's listening and communication development is not yet on track; and/or there is a persistent or recurrent middle ear condition.
Summary of evidence. A “refer” result on pure tone screening audiometry correctly identifies hearing loss 12–100% of the time; a “pass” correctly identifies no hearing loss 50–97% of the time, as identified in a systematic review of eight studies.46 Wide variations in accuracy relate to factors including choice of pass/refer thresholds and environmental noise during testing. Screener training and experience also potentially affects accuracy, the extent to which was not reported.46 Few studies were done in primary health services.46 Automated audiometry (eg, hearScreen, Sound Scouts) for children aged 4–14 years correctly identifies a child with hearing loss 41–89% of the time, and correctly identifies a child without hearing loss 86.5–98.5% of the time.47,48,49 Few published guidelines recommend audiometry be included in routine primary health EHHCs.1,31 Automated and manual audiometry are useful in broader primary health for children capable of play or push button audiometry (about 4 years and older).1,31,32,43,44 However, there are currently few non‐audiologists trained in audiometry techniques appropriate for use with children aged 0–3 years.
Rationale for recommendation. There was insufficient evidence to make a strong, positive (or negative) recommendation on the role of audiometry as part of routine primary health EHHCs. The role of audiometry in routine EHHCs did not reach consensus in the Delphi process. Consensus was reached, after consideration and discussion by the working group, to recommend audiometry as per the OM guidelines.1 In practice, this means that EHHCs do not include audiometry but do identify children who should be referred for audiometry. Whether audiometry should be routinely performed before school commencement was not addressed in the evidence review or the consultation process.
Timing of routine ear health and hearing checks
Following newborn hearing screening, EHHCs are recommended at least 6‐monthly until the age of 4 years, and then one check at 5 years of age. It is suggested that EHHCs be undertaken more frequently than 6 months: in high risk settings (as defined in the OM guidelines1), and/or for children aged under 2 years, and/or when it is acceptable to families, and/or in response to parent/carer concerns.
Summary of evidence. Of the 11 reviewed guidelines, five included recommendations on timing of checks with no agreement on intervals. In general, the timing of checks was linked to developmental milestones, with more frequent checks recommended for children at high risk of OM.
Rationale for recommendation. Australian and international guidelines vary in their recommendations on the timing of EHHCs, including at every health service visit, 3‐monthly, 3‐ to 6‐monthly, and at seven timepoints before school entry. Australian jurisdictional child health check schedules vary in the timing of EHHCs. In general, two to four checks are scheduled in a child's first year of life, one to two checks in their second year, and annual checks thereafter. In several jurisdictions, opportunistic checks or additional considerations are encouraged for Aboriginal and Torres Strait Islander children.
Research is lacking on the direct impact of early, frequent checks on outcomes. However, research indicates that hearing loss should be remediated no later than at 3–6 months of age, to ensure children achieve age‐appropriate communication and linguistic competence.41 Although 3‐monthly checks in the child's first 2 years may be optimal, many respondents expressed concerns about the feasibility and acceptability of this approach, and the challenges of frequent checks for families. Six‐monthly EHHCs were proposed as a feasible alternative. However, more frequent checks are encouraged when appropriate and acceptable. As part of implementation, the timing of checks would require evaluation, to ensure that benefit outweighs harm.
Considerations for implementation
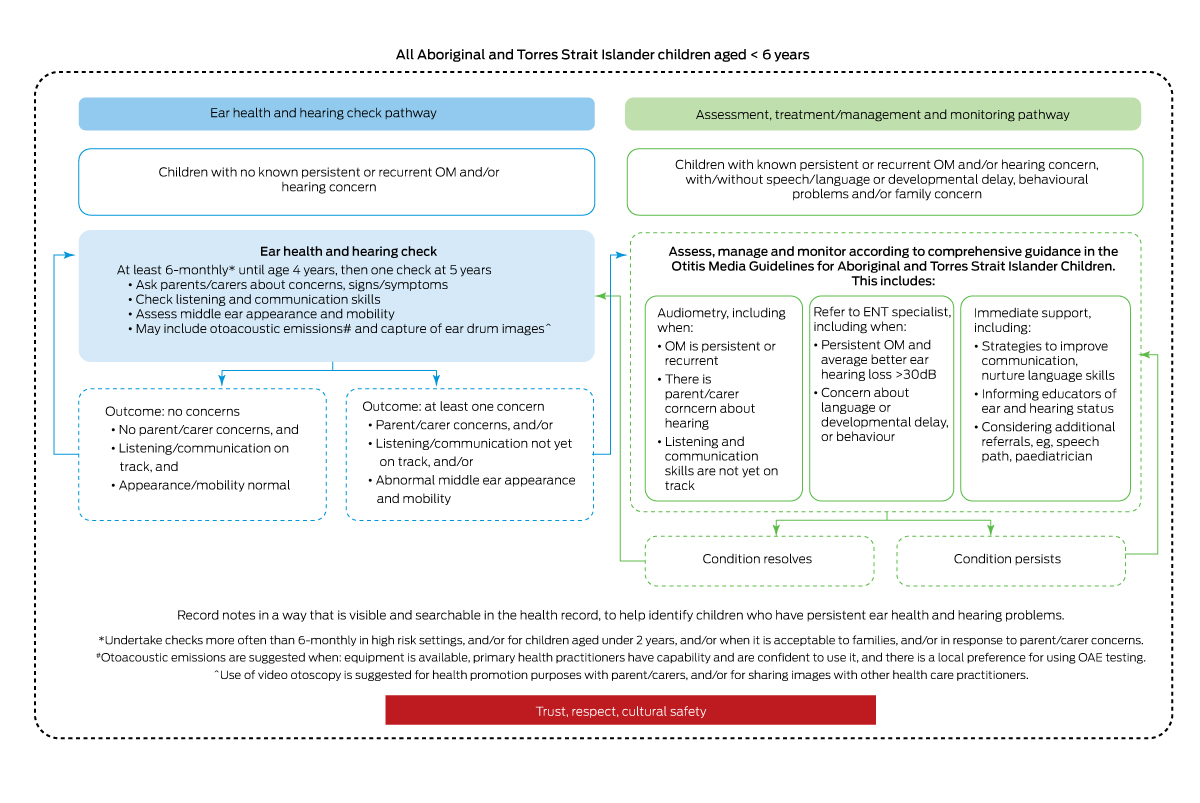
When problems are identified, an appropriate clinical response must be provided, as per the OM guidelines.1 This response must also include immediate support for hearing and communication, especially when access to audiology and ear, nose and throat services is delayed. When no problems are found, families can be reassured, and their expectations set for the scheduled checks to follow. A child whose ear and/or hearing condition has resolved should be returned to the EHHC pathway. Box 5 illustrates the EHHC and the assessment, management and monitoring pathways.
Key changes to practice include the routine use of tympanometry and listening and communication skills screening checklists. Scoping for implementation is recommended to identify how best to embed the recommendations. Actions that may facilitate implementation include:
- Change management that assists clinical staff to understand the impacts of persistent OM and that early action will make a difference.
- Positive communications to promote community understanding and acceptance.
- Involvement of practice staff in planning implementation, including, where possible, Aboriginal and Torres Strait Islander health workers and practitioners, practice nurses, and doctors.50
- Training, mentoring and support of Aboriginal and Torres Strait Islander health practitioners, to champion and undertake checks.
- Provision of necessary equipment.
- Practical information on immediate actions that families and educators can take to nurture children's listening and communication skills.
- Clear, timely pathways to referral services.
- Clinical data recorded in discoverable fields to increase visibility of ear health history, and to facilitate secondary use of data for reporting, auditing, and quality improvement activities.51
- Use of recall systems to support adherence to recommendations.
There is an urgent need for a radical shift in the perception and tolerance of OM prevalence and its impact, to create the expectation that Aboriginal and Torres Strait Islander children can have healthy ears and hearing, and experience rates of persistent OM comparable to non‐Indigenous children. This transformation requires a shift in policy and practice at all levels of the systems and services that support ear health and hearing, including addressing the social and environmental determinants of OM, and the availability of adequate primary health care and associated referral services.
Box 2 – Level of agreement and feasibility for each recommendation, for each round
|
|
Agreement |
Feasibility |
|||||||||||||
|
Component |
Round 1 |
Round 2 |
Round 1 |
Round 2 |
|||||||||||
|
|
|||||||||||||||
|
Parent/carer‐reported concerns, signs, symptoms |
96% |
– |
84% |
92% |
|||||||||||
|
Listening and communication skills screening |
98% |
– |
77% |
88% |
|||||||||||
|
Appearance and movement of ear drum and middle ear |
93% |
– |
67% |
82% |
|||||||||||
|
Video otoscopy (in certain conditions) |
96% |
– |
67% |
71% |
|||||||||||
|
Otoacoustic emissions (in certain conditions) |
68% |
84% |
67% |
75% |
|||||||||||
|
Audiometry |
65% |
71% |
– |
– |
|||||||||||
|
Timing (for all children) |
> 80%* |
88% |
– |
67% |
|||||||||||
|
Timing (additional checks in certain conditions) |
– |
88% |
– |
64% |
|||||||||||
|
|
|||||||||||||||
|
* Multiple questions. |
|||||||||||||||
Box 3 – Level of expert agreement reached for each routine ear health and hearing check goal
|
Goal |
Level of agreement |
||||||||||||||
|
|
|||||||||||||||
|
Identify children who have good ear health, hearing, and listening and communication development |
86% |
||||||||||||||
|
Identify children who have an acute or persistent ear health condition |
100% |
||||||||||||||
|
Identify children who may be experiencing hearing loss |
100% |
||||||||||||||
|
Identify children whose listening and hearing‐related communication development may be delayed |
100% |
||||||||||||||
|
Identify children who need further ear health and hearing assessment |
100% |
||||||||||||||
|
Provide an opportunity for parents/carers to talk about children's ear health and hearing |
98% |
||||||||||||||
|
Build rapport between health practitioners and parents/carers |
98% |
||||||||||||||
|
Build knowledge of ear health, hearing, listening and communication development among parents/carers |
100% |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 4 – Ear health and hearing check (EHHC) recommendations presented with strength of recommendation, GRADE certainty of evidence,19 level of expert agreement, and feasibility rating
|
Domain |
Recommendation |
Strength of recommendation |
Certainty of evidence |
Level of expert agreement |
Expert feasibility rating |
||||||||||
|
|
|||||||||||||||
|
Parent and carer‐reported history, concerns, signs and symptoms |
Ask parents/carers about:
|
Strong |
Low |
96% |
92% |
||||||||||
|
Listening and communication skills |
From the age of 6 months, review children's listening and communication skills development with parents/carers using appropriate questionnaires or checklists |
Strong |
Very low |
98% |
88% |
||||||||||
|
Ear health |
Examine appearance of the ear canal and ear drum, and assess movement of the ear drum and middle ear using either simple otoscopy plus tympanometry or pneumatic otoscopy |
Strong |
Low |
93% |
82% |
||||||||||
|
|
Use of video otoscopy is suggested for health promotion purposes with parents/carers, and/or for sharing images with other health care practitioners |
Conditional |
Low |
96% |
71% |
||||||||||
|
Hearing sensitivity |
Otoacoustic emissions testing is suggested to confirm or exclude normal or near‐normal hearing when:
|
Conditional |
Low |
84% |
75% |
||||||||||
|
|
Audiometry is recommended as per Otitis Media Guidelines for Aboriginal and Torres Strait Islander children1 when:
|
Strong |
– |
– |
– |
||||||||||
|
Timing of routine EHHCs |
Following newborn hearing screening, EHHCs are recommended at least 6‐monthly until the age of 4 years, and then one check at 5 years of age |
Strong |
Low |
88% |
67% |
||||||||||
|
|
It is suggested that EHHCs be undertaken more frequently than 6 months:
|
Conditional |
Low |
88% |
64% |
||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Provenance: Not commissioned; not externally peer reviewed.
- 1. Menzies School of Health Research. Otitis media guidelines for Aboriginal and Torres Strait Islander children. Darwin: Menzies School of Health Research, 2020. https://www.menzies.edu.au/icms_docs/324012_Otitis_Media_Guidelines_2020.pdf (viewed June 2021).
- 2. World Health Organization. World report on hearing. Geneva: World Health Organization, 2021. https://www.who.int/publications/i/item/9789240020481 (viewed June 2021).
- 3. DeLacy J, Dune T, Macdonald JJ. The social determinants of otitis media in aboriginal children in Australia: are we addressing the primary causes? A systematic content review. BMC Public Health 2020; 20: 492.
- 4. Sherwood J. Colonisation ‐ it's bad for your health: the context of Aboriginal health. Contemp Nurse 2013; 46: 28‐40.
- 5. Swift VM, Doyle JE, Richmond HJ, et al. Djaalinj Waakinj (listening talking): rationale, cultural governance, methods, population characteristics – an urban Aboriginal birth cohort study of otitis media. Deaf Educ Int 2020; 22: 255‐274.
- 6. Morris PS, Leach AJ, Silberberg P, et al. Otitis media in young Aboriginal children from remote communities in Northern and Central Australia: a cross‐sectional survey. BMC Pediatr 2005; 5: 27.
- 7. McGilchrist CA, Hills LJ. Estimation of cumulative illness using cross‐sectional data. J Chronic Dis 1986; 39: 929–31.
- 8. Dick F, Krishnan S, Leech R, Curtin S. Language development. In: Hickok G, Small SL, editors. Neurobiology of language. Academic Press, 2016; pp. 373‐388.
- 9. Harkus S, Caso K, Hall S, et al. ‘Sometimes they're gammin, playing tricks, but sometimes it's ears.’ The perspectives of urban parents and carers of young Aboriginal and Torres Strait Islander children on their journey to diagnosis of persistent ear health and hearing problems. Public Health Res Pract 2021; 31; 3152129.
- 10. Campbell L, Reath J, Hu W, et al. The socioemotional challenges and consequences for caregivers of Aboriginal and Torres Strait Islander children with otitis media: a qualitative study. Health Expect 2022; 25: 1374‐1383.
- 11. Simpson A, Sarkic B, Enticott JC, et al. Developmental vulnerability of Australian school‐entry children with hearing loss. Aust J Primary Health 2020; 26: 70‐75.
- 12. Bell MF, Bayliss DM, Glauert R, et al. Chronic illness and developmental vulnerability at school entry. Pediatrics 2016; 137; e20152475.
- 13. Su J‐Y, Guthridge S, He VY, et al. Impact of hearing impairment on early childhood development in Australian Aboriginal children: a data linkage study. J Paediatr Child Health 2020; 56: 1597‐1606.
- 14. Commissioner for Children and Young People Western Australia. Developmental screening. Overview and areas of concern. https://www.ccyp.wa.gov.au/our‐work/indicators‐of‐wellbeing/age‐group‐0‐to‐5‐years/developmental‐screening/ (viewed June 2021).
- 15. Australian Government Department of Health. New National Key Performance Indicator (nKPI) for primary health care – ear health. Consultation paper. 2021. https://consultations.health.gov.au/indigenous‐health/potential‐new‐national‐key‐performance‐indicators/supporting_documents/Ear%20Health%20Consultation%20Papers.pdf (viewed June 2021).
- 16. NSW Ministry of Health. My personal health record. https://www.health.nsw.gov.au/kidsfamilies/MCFhealth/Publications/blue‐book.pdf (viewed June 2021).
- 17. Office of the Auditor General Western Australia. Improving Aboriginal Children's ear health. Report 23: June 2018‐19. https://audit.wa.gov.au/wp‐content/uploads/2019/06/Improving‐Aborignal‐Childrens‐Ear‐Health.pdf (viewed Aug 2021).
- 18. Simpson SA, Thomas CL, van der Linden MK, et al. Identification of children in the first four years of life for early treatment for otitis media with effusion. Cochrane Database Syst Rev 2007; (1): CD004163.
- 19. Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction‐GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011; 64: 383‐394.
- 20. Niederberger M, Koberich S; members of the DeWiss Network. Coming to consensus: the Delphi technique. Eur J Cardiovasc Nurs 2021; 20: 692‐695.
- 21. Varndell W, Fry M, Lutze M, Elliott D. Use of the Delphi method to generate guidance in emergency nursing practice: a systematic review. Int Emerg Nurs 2021; 56: 100867.
- 22. Dickinson LJ, Nimmo M, Morton RP, Purdy SC. ‘Asymptomatic’ South Auckland preschool children have significant hearing loss and middle ear disease. Int J Pediatr Otorhinolaryngol 2018; 114: 106‐110.
- 23. Engel J, Anteunis L, Volovics A, et al. Predictive value of parent‐reported symptoms in the assessment of otitis media with effusion during infancy. Scand J Prim Health Care 2000; 18: 25‐29.
- 24. Cakabay T, Ustun Bezgin S, Tarakcioglu MC, et al. Why do infants pull their ears? Auris Nasus Larynx 2019; 46: 803‐807.
- 25. Laine MK, Tahtinen PA, Ruuskanen O, et al. Can nurses exclude middle‐ear effusion without otoscopy in young asymptomatic children in primary care? Scand J Prim Health Care 2015; 33: 115‐120.
- 26. Watkin PM, Baldwin M, Laoide S. Parental suspicion and identification of hearing impairment. Arch Dis Childhood 1990; 65: 846‐850.
- 27. Swierniak W, Gos E, Skarzynski PH, et al. The accuracy of parental suspicion of hearing loss in children. Int J Pediatr Otorhinolaryngol 2021; 141: 110552.
- 28. Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical practice guideline: otitis media with effusion (update). Otolaryngol Head Neck Surg 2016; 154 (1 Suppl): S1‐S41.
- 29. Leach AJ, Morris PS, Coates HL, et al. Otitis media guidelines for Australian Aboriginal and Torres Strait Islander children: summary of recommendations. Med J Aust 2021; 214: 228‐233. https://www.mja.com.au/journal/2021/214/5/otitis‐media‐guidelines‐australian‐aboriginal‐and‐torres‐strait‐islander
- 30. National Aboriginal Community Controlled Health Organisation; Royal Australian College of General Practitioners. National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people. 3rd ed. Melbourne: RACGP, 2018. https://www.racgp.org.au/FSDEDEV/media/documents/Clinical%20Resources/Resources/National‐guide‐3rd‐ed‐Sept‐2018‐web.pdf (viewed June 2021).
- 31. Rosenfeld RM, Shin JJ, Schwartz SR, et al. Clinical Practice Guideline: Otitis media with effusion (update). Otolaryngol Head Neck Surg 2016;154 (1 Suppl): S1‐S41.]
- 32. Lee HJ, Park SK, Choi KY, et al. Korean clinical practice guidelines: otitis media in children. J Korean Med Sci 2012; 27: 835‐848.
- 33. American Academy of Pediatrics Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics 2007; 120: 898‐921.
- 34. Laine MK, Tahtinen PA, Ruuskanen O, et al. Symptoms or symptom‐based scores cannot predict acute otitis media at otitis‐prone age. Pediatrics 2010; 125: e1154‐e1161.
- 35. Glascoe FP, MacLean WE, Stone WL. The importance of parents’ concerns about their child's behavior. Clin Pediatr (Phila) 1991; 30: 8‐11.
- 36. Golz A, Netzer A, Angel‐Yeger B, et al. Effects of middle ear effusion on the vestibular system in children. Otolaryngol Head Neck Surg 1998; 119: 695‐699.
- 37. Kong K, Coates HL. Natural history, definitions, risk factors and burden of otitis media. Med J Aust 2009; 191 (9 Suppl): S39‐S43. https://www.mja.com.au/journal/2009/191/9/natural‐history‐definitions‐risk‐factors‐and‐burden‐otitis‐media
- 38. Orzan E, Battelino S, Ciciriello E, et al. Reliability of parental assessment of auditory skills in young children: a cross‐sectional study in Italian language. BMJ Open 2021; 11: e042297.
- 39. Newton V, Macharia I, Mugwe P, et al. Evaluation of the use of a questionnaire to detect hearing loss in Kenyan pre‐school children. Int J Pediatr Otorhinolaryngol 2001; 57: 229‐234.
- 40. Ching T, Hou S, Seeto M, et al. The Parents’ evaluation of Listening and Understanding Measure (PLUM): Development and normative data on Aboriginal and Torres Strait Islander children below 6 years of age. Deaf Educ Int 2020; 22: 288‐304.
- 41. Ching TYC, Dillon H, Leigh G, Cupples L. Learning from the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study: summary of 5‐year findings and implications. Int J Audiol 2018; 57 Suppl 2: S105‐S111.
- 42. NACCHO–RACGP Partnership Project. Aboriginal and Torres Strait Islander health check – Infants and preschool children (birth – 5 years). https://www.racgp.org.au/getmedia/fef63587‐4a8a‐4734‐9dcf‐4ea4a93d75ff/Health‐check‐Infants‐and‐preschool.pdf.aspx (viewed June 2021).
- 43. American Academy of Audiology. Childhood hearing screening guidelines: Sept 2011. https://www.cdc.gov/ncbddd/hearingloss/documents/aaa_childhood‐hearing‐guidelines_2011.pdf (viewed June 2021).
- 44. Heidemann CH, Lous J, Berg J, et al. Danish guidelines on management of otitis media in preschool children. Int J Pediatr Otorhinolaryngol 2016; 87: 154‐163.
- 45. Puhakka T, Pulkkinen J, Silvennoinen H, Heikkinen T. Comparison of spectral gradient acoustic reflectometry and tympanometry for detection of middle‐ear effusion in children. Pediatr Infect Dis J 2014; 33: e183‐e186.
- 46. Prieve BA, Schooling T, Venediktov R, Franceschini N. An evidence‐based systematic review on the diagnostic accuracy of hearing screening instruments for preschool‐ and school‐age children. Am J Audiol 2015; 24: 250‐267.
- 47. Mahomed‐Asmail F, Swanepoel de W, Eikelboom RH, et al. Clinical validity of hearScreen smartphone hearing screening for school children. Ear Hear 2016; 37: e11‐e17.
- 48. Mealings K, Harkus S, Flesher B, et al. Detection of hearing problems in Aboriginal and Torres strait islander children: a comparison between clinician‐administered and self‐administrated hearing tests. Int J Audiol 2020; 59: 455‐463.
- 49. Ukoumunne OC, Hyde C, Ozolins M, et al. A directly comparative two‐gate case–control diagnostic accuracy study of the pure tone screen and HearCheck screener tests for identifying hearing impairment in school children. BMJ Open 2017; 7: e017258.
- 50. Spurling GK, Tyson CS, Askew D, Reath J. Mixed‐methods evaluation of screening for hearing loss using the hearScreen™ mobile health application in Aboriginal and Torres Strait Islander children presenting to an urban primary healthcare service. Aust J Primary Health 2021; 27: 371‐376.
- 51. Sibthorpe B, Agostino J, Coates H, et al. Indicators for continuous quality improvement for otitis media in primary health care for Aboriginal and Torres Strait Islander children. Aust J Primary Health 2017; 23: 1‐9.






This project received funding support from the Australian Government Department of Health and Aged Care, First Nations Health Division. We would like to acknowledge and thank the National Aboriginal Community Controlled Health Organisation, and Kim Terrell and Michele Clapin from Hearing Australia, who played important roles in conceptualising, shaping and supporting the project. We also express our gratitude to the members of the Ear Health and Hearing Check Working Group, for their commitment to, guidance of, and participation in the recommendations development process: Maricar Alcedo, Amarjit Anand, Chris Brennan‐Jones, Karl Briscoe (Kuku Yalanji), Matthew Brown, Hasantha Gunasekera, Gerry Hannan, Sarah Hayton, Rob James, Kirsty Jennings (Biripi), Amanda Leach, Karen Myors, Peter O'Mara (Wiradjuri), Pamela Paltridge, Leanne Quirino, Trumaine Rankmore (Wiradjuri, Gomeroi and Ngemba), Sowmya Rao, Simone Raye (Bardi Jabbir Jabbir), Melanie Stone, Valerie Swift (Menang Gnudju), Nicole Turner (Kamilaroi), Claudette (Sissy) Tyson (Kuku Yalanji), and Marianne Wood. Additional thanks to Working Group members Amanda Leach and Hasantha Gunasekera for guidance on assessing certainty of evidence. Further, we sincerely thank all expert panel members who took part in the Delphi consensus process, which required a considerable time commitment, and the organisations that assisted us in identifying expert representatives. Finally, our thanks to Viji Easwar for providing editorial guidance during writing of the manuscript.
No relevant disclosures.