By learning from Australia’s response to the pandemic and breaking down siloes, we can build a more integrated and resilient health system
The Australian health care system is well regarded on the global stage in terms of the balance between investment in health care and outcomes delivered, particularly in terms of universal access, quality and safety.1 However, there is considerable fragmentation and poor coordination of care and communication between hospitals and primary care, which limits further improvement.2,3 Geographical barriers, workforce shortages and issues relating to acceptability of services limit health care access for residents of rural, regional and remote communities, Aboriginal peoples and Torres Strait Islanders, and together with an inadequate focus on prevention, limit progress towards health equity.4
Australian responses to the coronavirus disease 2019 (COVID‐19) pandemic through both public health responses and the acute health sector have been viewed as among the best in the world. Nevertheless, challenges in the structure, organisation and financing of the Australian health care system have been brought into stark relief by the evolution of responses to the pandemic.
Many calls for health system reform have been made, including calls for integrated systems of care that encompass health promotion, preventive health care, and primary, secondary and tertiary care as needed, and calls for strong loco‐regional place‐based planning that involves consumers at all stages.5 Yet the Byzantine‐like system of federated states and resultant complexity in funding arrangements has made such reform extremely challenging. Limitations of the existing system have been illuminated by the passage of the COVID‐19 pandemic in Australia — from early outbreaks with small caseloads and high proportions of people with severe disease (who required hospital treatment) through to dominance of the highly transmissible Omicron strain and less severe disease (largely managed in the community).
Responding to the pandemic has improved our skills in and understanding of surveillance and response to infectious disease outbreaks, at both individual and systemic levels. It has also led to rapid breakthroughs in the development and testing of new diagnostic techniques, therapies and vaccines. Rapid policy evolution has been evident: for example, policy changes relating to telemedicine and hospital in the home arrangements, and development of systems for rapidly appraising and making available the best global evidence.6,7 However, the pandemic has also illuminated health system inequities based on social determinants, and gaps in service provision.8
As Australia transitions to a post‐pandemic mode, we reflect on lessons learned from impacts of COVID‐19 on the community and primary care sector over the past 2 years. We also consider how these lessons can help strengthen health service integration and equity into the future.
Pre‐pandemic planning
A parliamentary enquiry has been critical of Australia’s planning for a pandemic such as COVID‐19,9 and has illuminated the need for national coordination, particularly to support smaller jurisdictions such as the Northern Territory. It was predictable that people experiencing socio‐economic disadvantage, including people from diverse backgrounds, were more likely than others to be affected by COVID‐19, and this has highlighted long term underinvestment in public health and information systems.
Early central planning and discussion rarely involved primary care providers — from private, public or Aboriginal community controlled health sectors — and highlighted a lack of regional health care planning structures. In fact, early messaging for general practitioners reflected how to avoid contracting SARS‐CoV‐2, rather than how best to care for patients who contracted the virus. As the pandemic evolved, this fragmentation and lack of planning involving the primary care sector, together with policies that ignored the economic realities of running general practices, limited the provision of integrated patient‐centred care for people with COVID‐19 in the community.10
Strong advocacy from the National Aboriginal Community Controlled Health Organisation and GPs in outbreak areas (including the Primary and Chronic Care Panel of the National COVID‐19 Clinical Evidence Taskforce) did consider the issues inherent in managing COVID‐19 in remote communities with overcrowded housing,6 but resource constraints limited execution of solutions.
Shifting care to the community
With the logarithmic growth in cases following the spread of the Omicron variant, systems for triage, monitoring and escalation of care became overwhelmed.11 The burden of caring for people with mild to moderate COVID‐19 in the community defaulted to GPs and primary care, but there had been little planning for managing and escalating care when needed, educating the GP workforce, or protecting and supporting the primary care workforce. Primary Health Networks (PHNs) were tasked with coordinating supply chains and care networks, but in many cases they lacked the required clinical and organisational networks, and they were not provided with coordination from federal and state governments that would enable them to progress with this effectively.9
In Australia, general practices were very much second line in terms of receiving vaccines.12 Likewise, issues with supply and distribution of rapid antigen tests and personal protective equipment were resolved relatively quickly for hospitals, but many GPs had prolonged delays in distribution of their personal protective equipment (including P2 [N95] masks) through federal government and PHN‐based distribution systems.9
Impact of COVID‐19 on the health system
As the pandemic evolved, attendance at primary care services and hospitals dropped precipitously, fuelled by changes in service availability (owing to hospital crisis response plans and staff furlough, illness and shortages) and population and health care provider fear and avoidance of health care facilities.13 In a study done in six high income countries (including Australia), none of the emergency plans had considered how to best sustain primary care services in the face of a pandemic.10 Although this was somewhat offset by a shift to virtual care through telemedicine, the likelihood of perverse outcomes in terms of delayed and missed routine primary and preventive care throughout the health system is yet to be fully experienced but is projected to be significant. To date, it has been impossible to fully quantify the personal, social and economic impact of the loss of education, employment, and routine preventive, primary and chronic disease care during this period, which is highly likely to convert into higher premature mortality over time,14 particularly for those most vulnerable. For example, in the NT, service resilience within remote primary health care services was monitored closely in the face of COVID‐19, with profound shocks for workforce stability. This resulted in two‐thirds of people in remote communities with one or more common chronic condition having not seen a GP for chronic care monitoring in the past 12 months (NT Health, unpublished data).
In parallel, and in response to pandemic‐accelerated policy change, we saw rapid uptake of telehealth primary care services through general practice, allied health and Aboriginal community‐controlled health organisations, and to facilitate hospital specialist follow‐up care.15 Interestingly, telephone rather than video call appeared to be the preferred modality for telehealth care among patients and providers. This was a win for accessibility (particularly in areas of lower internet connectivity), but possibly came at the expense of communication and visual cues for assessment.16 Ongoing use of Medicare Benefits Schedule telehealth items introduced during the pandemic has been endorsed, with additional temporary item numbers introduced in July 2022 for longer telephone consultations with people diagnosed with COVID‐19.17 Our task as planners and health system researchers is now to optimise the use of telehealth services as a complement to face‐to‐face services and explore the broader role of digital innovation, remote monitoring and alternative models of care in building an optimal integrated health system for a post‐pandemic world.11 In a timely alignment with the National Health Reform Agreement,18 this might involve clinician leaders, PHNs, Local Hospital Networks (LHNs) and peak bodies at a regional level working with funders to explore alternative financing, commissioning and registration models for primary care, integration with hospital services, and the broader agenda of workforce sustainability, especially in rural areas. There is a particular need for purposeful rebuilding of remote primary health care, emphasising the primacy of the Aboriginal clinical workforce, demonstrated as essential for overcoming vaccine hesitancy and enabling timely vaccine rollout (NT Health, unpublished data).
Case studies of excellence in co‐design of integrated models of care
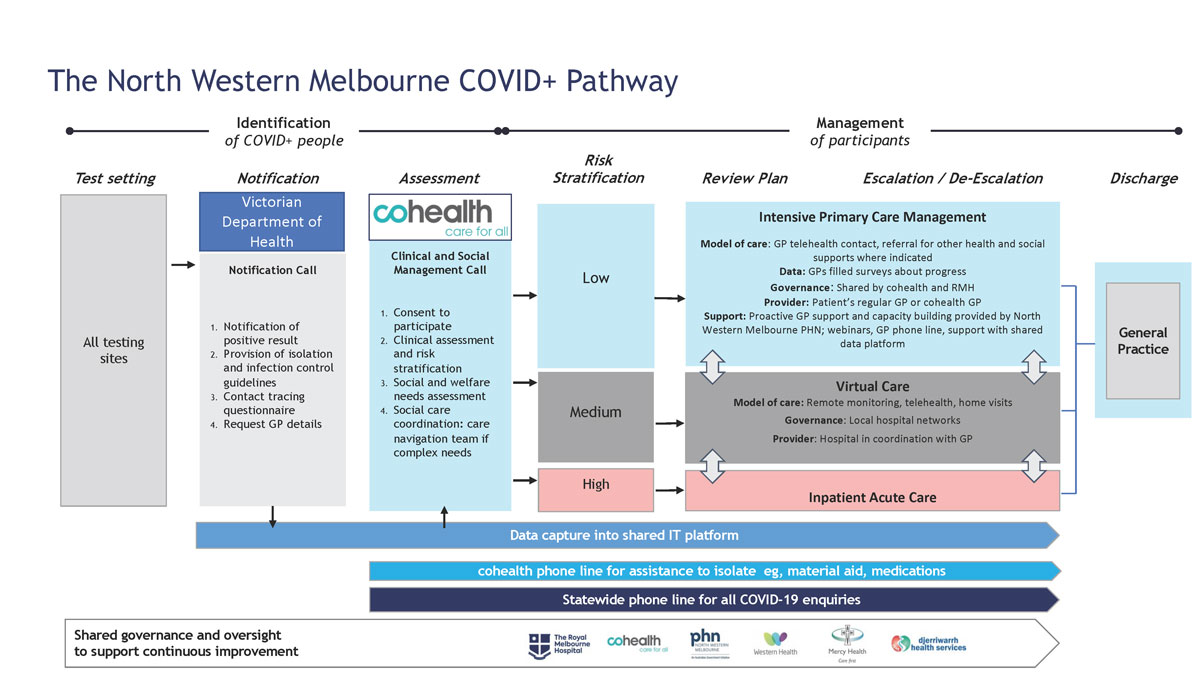
There are examples of excellence in planning coordinated response models that provide health care for people with mild to moderate COVID‐19 in the community. These offer lessons about how best to reduce fragmentation of care after the pandemic. One example developed in response to local need is the North Western Melbourne COVID Positive Pathway (Box 1 and Box 2).19 Other examples involve use of social media to promote vaccination and chronic disease care in Aboriginal communities, development of integrated public–private partnerships through hospital in the home models (eg, https://hiyh.com.au), and overseas models of coordinated home care for people with complex and chronic needs.20 These models:
- involve consumers and clinicians (from primary care and hospitals);
- consider equity and diversity and the broader determinants of health;
- include joined up pathways for escalation of care as appropriate; and
- collect data on processes and outcomes to inform subsequent evaluation and improvement.
What have we learned to strengthen our health system?
Despite acknowledgement that the health system is complex, primary care and community care are omitted from many analyses.21 As we look back at the Australian health system response to the COVID‐19 pandemic, we can use our experience to build resilience into the Australian health care system, particularly primary care,10 integrate different elements of the health system, and align our responses with existing calls for reform. Calls have been made to distribute resources during the pandemic using an approach that is informed by health equity and distributive justice22 — perhaps it is time for a similar approach in primary and community care? In our view, three key priorities gleaned from the pandemic experience in Australia and overseas might assist health care policymakers and planners to work with clinician leaders to build a stronger primary health care system.
The first of these priorities is co‐designed regional models of care involving primary care providers and referral hospitals working together with PHNs, LHNs, peak bodies and clinician leaders to implement referral, care and escalation pathways. These need to be inclusive, with clear shared governance mechanisms, and need to involve consumers and clinicians in their co‐design. Agility and responsiveness are required in designing, implementing and evaluating these responses.21
The second priority is exploring strategies to maintain critical access to essential primary and chronic care services, especially for those most vulnerable, during times of shock in the health system. Judicious use of digital solutions, including telehealth services, to complement, rather than replace, face‐to‐face services is likely to be part of the solution here. Education and training for the health workforce and consumers in the use of these models and ongoing policy and financing support for their use is important.
The third priority is ensuring education, care, engagement and support for a sustainable health workforce. This includes training a fit‐for‐purpose workforce in terms of competencies and geography, but also flexibility in deployment, scope of practice and workload to account for varied responsibilities and access to sufficient and appropriate mental health care and support. Training the clinician workforce to lead and advocate in terms of system improvement is paramount, as is producing a stable Indigenous clinical workforce to serve Aboriginal and Torres Strait Islander populations.
Let us hope that we can seize this opportunity to rethink planning, care and funding models for health care in Australia, to ensure a more integrated and equitable system into the future.
Box 1 – North Western Melbourne COVID Positive Pathway: summary18
- Partners of the North Western Melbourne COVID Positive Pathway are: cohealth, North Western Melbourne Primary Health Care Network, Melbourne Health, Western Health, Werribee Mercy Hospital and general practitioners across the region, with support from the Victorian Government Department of Health.
- The Pathway (Box 2) provides a coordinated approach to COVID‐19 care, which includes responding to all notified SARS‐CoV‐2‐positive patients and clear pathways for escalating primary care.
- ► cohealth, a community health organisation, performs triage and assessment, including detailed social assessment and complex care navigation if required.
- ► Hospital partners provide acute care and more intensive monitoring for higher risk patients, including oxygen saturation monitoring, while area GPs provide regular care every second day for the lower acuity group (80% of patients).
- ► The North Western Melbourne Primary Health Care Network provides logistic support to GPs, education sessions and coordination across the region for the shared information technology platform.
COVID‐19 = coronavirus disease 2019.
Provenance: Not commissioned; externally peer reviewed.
- 1. Schneider E, Shah A, Doty M, et al. Mirror, mirror 2021: reflecting poorly. Health care in the U.S. compared to other high‐income countries. New York: The Commonwealth Fund, 2021.
- 2. Duckett S. What should primary care look like after the COVID‐19 pandemic? Aust J Prim Health 2020; 26: 207‐211.
- 3. Jackson C, O’Halloran D. Reforming our health care system: time to rip off the bandaid? Med J Aust 2021; 215: 301‐303. https://www.mja.com.au/journal/2021/215/7/reforming‐our‐health‐care‐system‐time‐rip‐band‐aid
- 4. Smith JA, Wells L, Gelbart L, Lawson T. Beyond COVID‐19: consumers call for greater focus on health equity. Health Promot J Austr 2021; 32: 3‐5.
- 5. Consumers Health Forum of Australia. Snakes and ladders: the journey to primary care integration. The George Institute for Global Health, Consumers Health Forum of Australia, University of Queensland, 2018.
- 6. Turner T, Elliott J, Tendal B, et al. The Australian living guidelines for the clinical care of people with COVID‐19: what worked, what didn’t and why, a mixed methods process evaluation. PLoS One 2022; 17: e0261479.
- 7. Rojek A, Dutch M, Camilleri D, et al. Early clinical response to a high consequence infectious disease outbreak: insights from COVID‐19. Med J Aust 2020; 212: 447‐450.e1. https://www.mja.com.au/journal/2020/212/10/early‐clinical‐response‐high‐consequence‐infectious‐disease‐outbreak‐insights
- 8. Flavel J, Baum F. The influence of socio‐economic conditions on the epidemiology of COVID‐19 in Australia. Med J Aust 2022; 216: 344‐345. https://www.mja.com.au/journal/2022/216/7/influence‐socio‐economic‐conditions‐epidemiology‐covid‐19‐australia
- 9. Senate Select Committee on COVID‐19. First interim report. Canberra: Commonwealth of Australia, 2020.
- 10. Huston P, Campbell J, Russell G, et al. COVID‐19 and primary care in six countries. BJGP Open 2020; 4: bjgpopen20X101128.
- 11. Jackson CL. Living with COVID‐19 in 2022: the impact of the pandemic on Australian general practice. Med J Aust 2022; 216: 442‐444. https://www.mja.com.au/journal/2022/216/9/living‐covid‐19‐2022‐impact‐pandemic‐australian‐general‐practice
- 12. Stobart A, Duckett S. Australia’s response to COVID‐19. Health Econ Policy Law 2022; 17: 95‐106.
- 13. Sutherland K, Chessman J, Zhao J, et al. Impact of COVID‐19 on healthcare activity in NSW, Australia. Public Health Res Pract 2020; 30: e3042030.
- 14. Griffin S. Covid‐19: “staggering number” of extra deaths in community is not explained by covid‐19. BMJ 2020; 369: m1931.
- 15. Taylor A, Caffery LJ, Gesesew HA, et al. How Australian health care services adapted to telehealth during the COVID‐19 pandemic: a survey of telehealth professionals. Front Public Health 2021; 9: 648009.
- 16. Scott A, Bai T, Zhang Y. Association between telehealth use and general practitioner characteristics during COVID‐19: findings from a nationally representative survey of Australian doctors. BMJ Open 2021; 11: e046857.
- 17. Australian Government Department of Health and Aged Care. Providing health care remotely during the COVID‐19 pandemic. https://www.health.gov.au/health‐alerts/covid‐19/coronavirus‐covid‐19‐advice‐for‐the‐health‐and‐disability‐sector/providing‐health‐care‐remotely‐during‐the‐covid‐19‐pandemic (viewed Aug 2022).
- 18. Australian Health Ministers. National Health Reform Agreement (NHRA): long‐term health reforms roadmap. Canberra: Australian Health Ministers, 2021.
- 19. Lim SM, Allard NL, Devereux J, et al. The COVID Positive Pathway: a collaboration between public health agencies, primary care, and metropolitan hospitals in Melbourne. Med J Aust 2022; 216: 413‐419. https://www.mja.com.au/journal/2022/216/8/covid‐positive‐pathway‐collaboration‐between‐public‐health‐agencies‐primary‐care
- 20. Parkinson A, Matenge S, Desborough J, et al. The impact of COVID‐19 on chronic disease management in primary care: lessons for Australia from the international experience. Med J Aust 2022; 216: 445‐448. https://www.mja.com.au/journal/2022/216/9/impact‐covid‐19‐chronic‐disease‐management‐primary‐care‐lessons‐australia
- 21. Clay‐Williams R, Rapport F, Braithwaite J. The Australian health system response to COVID‐19 from a resilient health care perspective: what have we learned? Public Health Res Pract 2020; 30: e3042025.
- 22. Galiatsatos P, Kachalia A, Belcher HME, et al. Health equity and distributive justice considerations in critical care resource allocation. Lancet Respir Med 2020; 8: 758‐760.






Open access
Open access publishing facilitated by James Cook University, as part of the Wiley ‐ James Cook University agreement via the Council of Australian University Librarians.
We thank the anonymous peer reviewers, whose comments improved our article, and we acknowledge the work of the Primary and Chronic Care Panel of the National COVID‐19 Clinical Evidence Taskforce.
No relevant disclosures.