People with COVID‐19 can be cared for in a variety of settings, but home isolation would be most convenient if properly supported.
Isolating at home can be facilitated by a comprehensive multidisciplinary tiered care pathway that provides clinical and psychosocial support. The health care needs of about four in five people with COVID‐19 could be met by primary care, retaining hospital services for people with more severe disease.
Supporting people with epidemic infections or chronic disease requires a collaborative, tiered approach that takes public health, primary and community care, and the various roles of hospitals into account.
The coronavirus disease 2019 (COVID‐19) pandemic is an international public health emergency. A range of mitigation and containment strategies have been adopted around the world, ranging from lockdowns and strict isolation of people with COVID‐19 to more relaxed measures in areas with different pandemic dynamics.1,2 These strategies have ignited discussions about balancing personal freedoms and social responsibilities when managing people with COVID‐19.3
A sharp rise in the number of COVID‐19 cases during June and July 2020 led the Victorian government to declare a state of disaster on 2 August 2020.4 As Victorian legislation prohibits the disclosure of patient‐identifying information5,6 and testing for the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) relied on self‐referral, the Victorian public health unit is the sole repository for information on people with COVID‐19. As the capacity of contact tracing systems was stretched, concerns arose about the health, welfare, and compliance of people required to isolate, particularly as COVID‐19 has been associated with asymptomatic hypoxia and out‐of‐hospital cardiac arrest.7
The COVID Positive Pathway was designed as a collaborative model of care involving the Victorian public health unit, local hospital services, primary care practices, and the North Western Melbourne Primary Health Network. The aims of the coordinated care pathway, spanning primary to quaternary care, were to provide timely health, psychosocial, and welfare assessment and interventions for people with COVID‐19, to build general practitioner confidence and skills in supporting people with mild COVID‐19, and to develop agreed criteria for referrals to specialist care. In this article we report on the capacity of the Pathway to meet these objectives and to support people isolating at home.
Methods
The COVID Positive Pathway commenced operation on 3 August 2020. It initially included one health service (Royal Melbourne Hospital), a community health organisation (cohealth), the North Western Melbourne Primary Health Network (PHN), and the Victorian Department of Health and Human Services (DHHS). In September 2020 it expanded to include three further hospitals (Djerriwarrh Health Services, Western Health, Werribee Mercy Health), thereby encompassing seven municipalities and 1 032 853 residents across 877 km2 of northwest Melbourne.8 The Pathway was open to all adults with COVID‐19 (18 years or older) who could potentially isolate at home, including pregnant women. People living in residential aged care facilities, prisons, and similar shared accommodation, those residing outside the catchment area, and people in hotel quarantine were not eligible for the Pathway.
The design of the Pathway was funded by the DHHS, and was developed during three weeks of daily project meetings of representatives from the Royal Melbourne Hospital, cohealth, and North Western Melbourne PHN. The implementation of the Pathway, particularly its psychosocial aspects, was refined iteratively at once or twice weekly meetings of all collaborators. Consistent with the health privacy principles of the Health Records Act 2001 (Vic) (paragraph 2.2(h)(ii)), and with the consent provided to public health authorities when contacting people with COVID‐19 and information‐sharing agreements between Pathway collaborators, participating organisations were permitted to share information about people with COVID‐19.5 An electronic project database based on the Research Electronic Data Capture (REDCap) tool was accessible to all collaborators, facilitating transparency about participants’ status in the Pathway.9 Besides additional funding to cohealth for baseline triage and assessment, Pathway components were supported by federal and state funding through the Medicare Benefits Schedule (for telehealth care by general practitioners), PHN funding, and activity‐based funding of public hospital services.
The COVID Positive Pathway (Box 1)
The public health unit sought consent to refer people with positive reverse transcription–polymerase chain reaction (RT‐PCR) SARS‐CoV‐2 test results to the Pathway during initial contact tracing telephone calls. If consent was provided, cohealth community health workers conducted a standardised risk assessment for severe disease and psychosocial problems that might preclude home‐based isolation.10 People with drug and alcohol, financial, or social problems that affected their ability to isolate were referred to other support services or alternative isolation options (eg, quarantine hotels).
Following triage, enrolled participants were allocated to low, medium, or high tiers of care according to their symptoms and risk factors for severe disease. Low tier participants were monitored by telehealth services (provided by their regular GP when possible) every second day during the second week of their illness. People without access to their regular GP and those without access to Medicare benefits (eg, travellers, temporary visa holders) were referred to a pre‐identified primary care practice able to care for them.
Participants at risk of severe disease and those with moderate symptoms were referred to hospital outreach services. The medium A tier of care included nurse‐led telehealth assessments overseen by a respiratory physician; the medium B tier provided hospital‐in‐the‐home services,11 including remote patient monitoring, in‐person clinical reviews by nurses and doctors, laboratory investigations, and parenteral medications.
The high care tier included people who needed in‐hospital care. When person‐to‐person contact was necessary, care providers wore long‐sleeved gowns, gloves, N95 masks, and eye protection.
Transfer between care tiers was determined by clinical status, and participants could be transferred to hospital if they reported worrying symptoms, or hypoxia, tachypnoea, or tachycardia.10 People were discharged from the pathway after recovery from illness and the end of home isolation orders, in consultation with public health authorities.
Coordination and education of general practitioners
The North Western Melbourne PHN undertook the coordination and education of 550 primary care practices in the catchment region. This role included:
- ▪ hosting six educational webinars: attended by 353 GPs, followed by 585 views of the webinar recording;
- ▪ development of COVID‐19 information webpages for primary health care providers: 5355 views during 1 August – 8 November 2020;12
- ▪ support for 314 GPs in 205 practices; 195 practices were contacted within 24 hours of commencing Pathway involvement. North Western Melbourne PHN support included telephone calls and emails describing the telehealth process, providing information about the Pathway model of care, and troubleshooting problems for GP practices and Pathway collaborators.
Data collection
Information regarding the Pathway and participants during 3 August – 31 December 2020 was gathered from the project database, the North Western Melbourne PHN dashboard, and administrative records of hospital collaborators. Automated data linkage programs ensured the accuracy of information flow between the public health unit, the project database, and the North Western Melbourne PHN dashboard. Data from the database were matched with administrative records from collaborating organisations to ensure accuracy regarding the demographic characteristics of participants, their dates of entry and exit from each tier of care, and their status on discharge from the Pathway.
To assess whether the Pathway met its objectives of supporting people with COVID‐19 to isolate at home with appropriate transitions between tiers of care, and helping GPs manage people with mild COVID‐19, the information collected included:
- ▪ referral, assessment outcomes, and enrolment of people with COVID‐19 referred by the public health unit;
- ▪ demographic and clinical characteristics of people with COVID‐19, and their social and welfare needs;
- ▪ outcomes, lengths of stay, and transitions between care tiers;
- ▪ numbers of participating GPs and feedback about Pathway coordination and education.
After participating patients left the Pathway, GPs were emailed a survey of 15 close and open‐ended questions about their experience of the Pathway, and their assessment of its capacity to help people with COVID‐19 to isolate at home.
Statistical analyses
Data analyses were performed in SPSS 17.0 (IBM). Normally distributed data are summarised as means with and standard deviations (SDs), non‐normally distributed data as medians with interquartile ranges (IQRs), and dichotomous data as counts and proportions. Associations between participants’ age and selected Pathway outcomes were assessed in Spearman rank order correlation tests (two‐tailed).
Ethics approval
The Melbourne Health Human Research Ethics Committee approved the study (QA2020171). This article conforms with the Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) guidelines.13
Results
Of 1392 people in northwest Melbourne with COVID‐19 referred to the Pathway, 858 were eligible for enrolment, and 711 consented to participation (83% of eligible people, 51% of people with COVID‐19). The most frequent reasons for non‐enrolment of eligible patients were already having recovered from COVID‐19 (228 people, 16%), and not providing consent (147 people, 11%) (Box 2). During the first week of the Pathway, 28 of 61 people (46%) were assessed within 24 hours of referral, but all 29 people referred during its ninth week were assessed within 24 hours (Box 3). The mean time between symptom onset and enrolment reported by low tier participants was 2.9 days (SD, 1.8 days), by medium B participants 6.5 days (SD, 5.7 days), and by high tier participants 11.9 days (SD, 7.6 days) (Box 4).
The median age of the 711 participants was 35 years (IQR, 25–56 years); that of the 681 people who did not enrol was 37 years (IQR, 24–63 years). Of the people enrolled in the Pathway, 398 (56%) were from culturally and linguistically diverse backgrounds, but 512 participants (72%) nominated English as their primary language. Seven participants (1%) reported high risk social problems, and 145 (20%) medium risk problems. Material assistance (food, basic supplies) was required by 239 participants (34%), financial aid by 45 people (6%) (Box 4).
After triage, 542 of 711 people were initially assigned to low tier care (76%), 70 to medium A care (10%), 43 to medium B care (6%), and 56 to high tier care (8%). Two participants who reported symptoms that warranted a higher tier of care were allocated to low tier care (monitored by their usual GPs) at their request. A total of 647 people (91%) remained in the Pathway until they recovered and home isolation was completed; 52 (7%) withdrew from the Pathway before the end of their isolation. Twelve people died while enrolled in the Pathway (1.7%): eleven in high tier care, and one person in medium A care who died of COVID‐19 after presenting to an emergency department (Box 2).
Most participants (658 of 711, 93%) were cared for within a single care tier during their time in the Pathway. Of the 542 people initially allocated to low tier care, 448 were managed by their usual GPs (78%). Nine participants in low tier care, 16 in medium A care, and ten in medium B care were transferred to higher care tiers (Box 2). Across the study period, low tier care was provided for a total of 575 people (81%) by 314 GPs (median period of care, 10 days; IQR, 7–30 days). A total of 155 participants (22%) received medium A and B tier care (hospital outreach services), including 508 remote monitoring telephone calls (medium A) and 365 telehealth (audio and visual) assessments (medium B). Sixty‐four participants received high tier care (Box 5). Age was statistically associated with reported severity of symptoms (r = 0.12; P < 0.001) and with transfer to higher tiers of care (r = 0.22; P < 0.001).
Twenty‐four GPs declined participation in the Pathway, most frequently because they could not commit to reviewing participants every second day. Sixty‐four of the 292 participating GPs (22%) responded to the follow‐up survey (22 GPs had ended their participation prior to the survey). Fifty respondents thought the role of GPs in the Pathway was clear, 58 that people with COVID‐19 could be cared for in the community, 51 that care escalation criteria were clear, and 46 that information needed for decisions was provided in a timely manner and that the clinical handover process was appropriate.
Discussion
We assessed the feasibility of a comprehensive, coordinated care pathway from primary to quaternary care, for people with COVID‐19 in a metropolitan area. Most eligible people with COVID‐19 (83%) enrolled in the Pathway, of whom 91% remained in the Pathway until their isolation period ended. A large proportion of participants (81%) were supported for at least part of their time in the Pathway by primary care while isolating at home, and it is notable that 75% required only primary and community care support; hospital services were needed by a smaller proportion with more severe disease (medium tier care, 22%, high tier care, 9%). The timeliness of assessment of participants improved across the study period. In contrast to overseas reports,7 no Pathway participants experienced fatal events at home. Most were cared for by their usual GPs, some of whom subsequently provided positive feedback about the Pathway.
Our findings add to the evidence base regarding home‐based management of people with COVID‐19. It is important to take cultural, logistic, and financial factors into account if people are to successfully isolate at home, particularly in areas of low socio‐economic status.14,15,16 Seven of 53 postcode areas in the Pathway catchment are in the lowest quintile of the Australian Bureau of Statistics Index of Relative Socio‐economic Disadvantage;17 more than half the participants required assistance (particularly with food and basic supplies) beyond that provided by federal and state agencies.18
This is the first published report of outcomes in a collaborative pathway providing tiered clinical and psychosocial care for people with COVID‐19, involving public health authorities, primary and community organisations, and hospital services. Outcomes (need for hospital care, number of deaths) were similar to those reported in single centre studies focused on virtual health care technologies.19,20,21 Our collaboration between local health care providers and public health authorities enabled responsibilities for clinical care, contact tracing, and providing isolation to be shared, which is important when dealing with rapidly rising case numbers and limited resources during an epidemic. As we enter the third year of COVID‐19 in Australia, measures that facilitate successful home isolation and community‐based care for people with mild disease will help contain its impact and ensure the sustainability of health care resources.
The tiered design and coordinated nature of the Pathway is consistent with best practice principles of health care delivery, and could also be applied to the community‐based management of complex and chronic health conditions, reducing the burden on hospitals and emergency services.22 Pathway elements such as the shared database (providing transparency of care delivery), defined care escalation criteria, and shared governance helped ensure support from Pathway collaborators, while the North Western Melbourne PHN played a crucial role in engaging the predominantly privately owned primary care sector. Flexible funding for pathways focused on outcomes, digital health technologies providing better data integration, and the long term health reforms proposed by the 2020–25 National Health Reform Agreement23 could support similar collaborations between primary care, community and social care organisations, and assist hospital health services to optimise preventive health care, mental health care, and care for people with chronic diseases.
Limitations
Our study did not include a control group because rising COVID‐19 case numbers made the rapid and pragmatic implementation of the Pathway desirable. Separate clinical records kept by emergency services, GP practices, and hospitals limited our ability to obtain data about treatment, adverse effects, or ambulance use unless this information was incidentally recorded in the shared database. The usefulness of the Pathway for supporting isolation at home must be considered in the context of national and state pandemic measures, particularly the stage 4 restrictions in Victoria at the time of our study.4 Our experience in northwest Melbourne may not be generalisable to other metropolitan areas with different socio‐demographic characteristics or during outbreaks of SARS‐CoV‐2 variants of greater virulence or pathogenicity. Nevertheless, our findings could inform future initiatives for managing people with COVID‐19 or other illnesses.
Conclusion
Successfully dealing with a pandemic requires multifaceted strategies, including clinical and non‐clinical support for people affected by the disease, as well as other personal, cultural, and socio‐economic mitigation measures. The COVID Positive Pathway is a practical collaboration between public health authorities, primary care practices, primary health networks, and hospital services, and the lessons learned during its implementation have contributed to changes in care for Victorians with COVID‐19. While protecting the privacy of the individual is of fundamental importance, appropriate data‐sharing arrangements can enable health care collaborations that assist people with potentially life‐threatening illnesses and optimise the delivery of care. Strategies for overcoming regulatory, legislative, and funding barriers to timely sharing of information and care delivery by primary care, hospital services and public health authorities should be further investigated.
Box 1 – The COVID Positive Pathway (CPP): relationships between the Victorian public health unit, the North Western Melbourne Primary Health Network, hospitals, and primary care
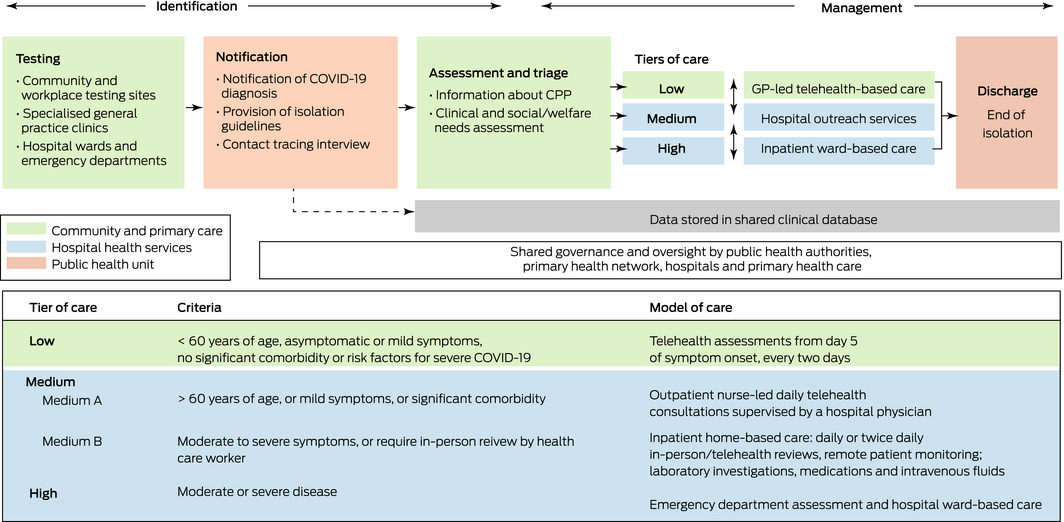
COVID‐19 = coronavirus disease 2019.
Box 2 – Enrolment and flow of participants through the COVID Positive Pathway (CPP)
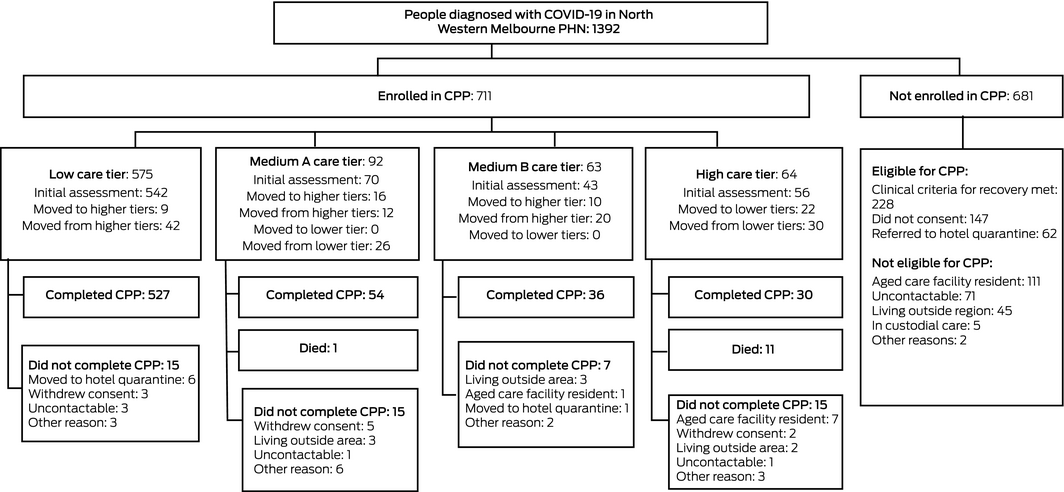
COVID‐19 = coronavirus disease 2019.
Box 3 – Initial assessment times for 1392 people with COVID‐19 referred by public health authorities to the COVID Positive Pathway, by week of pathway operation
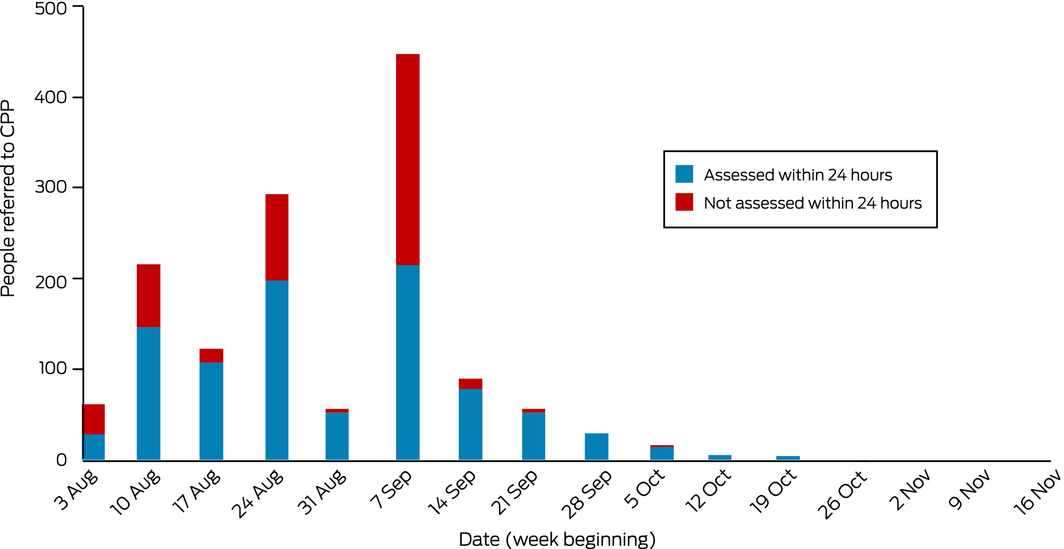
COVID‐19 = coronavirus disease 2019.
Box 4 – Demographic and clinical characteristics of the 711 people with COVID‐19 enrolled in the COVID Positive Pathway
|
|
|
Initial tier of care |
|||||||||||||
|
Characteristic |
All participants |
Low |
Medium A |
Medium B |
High |
||||||||||
|
|
|||||||||||||||
|
Initial care tier allocation |
711 |
542 |
70 |
43 |
56 |
||||||||||
|
Age (years), median (IQR) |
35 (25‒56) |
31 (24–42) |
55 (34–65) |
49 (31–59) |
73 (56–85) |
||||||||||
|
Nominated language for telehealth |
|
|
|
|
|
||||||||||
|
English |
512 (72%) |
476 |
26 |
10 |
0 |
||||||||||
|
Language other than English |
43 (6%) |
30 (6%) |
9 (13%) |
3 (7%) |
1 (2%) |
||||||||||
|
Missing data |
156 (22%) |
36 |
35 |
30 |
55 |
||||||||||
|
Usually ineligible for Medicare* |
153 (22%) |
153 (28%) |
0 |
0 |
0 |
||||||||||
|
Pregnant |
7 (1%) |
4 (1%) |
1 (1%) |
1 (2%) |
1 (2%) |
||||||||||
|
Relevant significant comorbidity† † |
112 (16%) |
56 (10%) |
36 (51%) |
16 (37%) |
4 (7%) |
||||||||||
|
Missing data |
75 (11%) |
12 (2%) |
4 (6%) |
10 (23%) |
49 (88%) |
||||||||||
|
Baseline clinical symptoms‡ ‡ |
|
|
|
|
|
||||||||||
|
Asymptomatic |
174 (24%) |
157 (29%) |
10 (14%) |
4 (9%) |
3 (5%) |
||||||||||
|
Mild symptoms |
411 (58%) |
357 (66%) |
37 (53%) |
14 (33%) |
3 (5%) |
||||||||||
|
Moderate symptoms |
51 (7%) |
15 (3%) |
18 (26%) |
17 (40%) |
1 (2%) |
||||||||||
|
Severe symptoms |
11 (2%) |
2 (< 1%) |
0 |
0 |
9 (16%) |
||||||||||
|
Missing data |
64 (10%) |
11 (2%) |
5 (7%) |
8 (19%) |
40 (71%) |
||||||||||
|
Time from symptom onset to enrolment (days), mean (SD) |
|
2.9 (1.8) |
4.0 (2.1) |
6.5 (5.7) |
11.9 (7.6) |
||||||||||
|
Time from COVID‐19 test to enrolment (days), mean (SD) |
|
4.0 (2.2) |
6.9 (1.9) |
6.9 (4.9) |
13.8 (8.2) |
||||||||||
|
Initial social and welfare risk assessment |
|
|
|
|
|
||||||||||
|
No risk factors |
261 (37%) |
220 (41%) |
22 (31%) |
16 (37%) |
3 (5%) |
||||||||||
|
Low risk§ § |
231 (32%) |
192 (35%) |
27 (39%) |
11 (26%) |
1 (2%) |
||||||||||
|
Medium risk¶ ¶ |
145 (20%) |
118 (22%) |
17 (24%) |
5 (12%) |
5 (9%) |
||||||||||
|
High risk** |
7 (1%) |
6 (1%) |
1 (1%) |
0 |
0 |
||||||||||
|
Missing data |
67 (9%) |
6 (1%) |
3 (4%) |
11 (26%) |
47 (84%) |
||||||||||
|
Social/welfare services required |
|
|
|
|
|
||||||||||
|
Material assistance (food, basic supplies) |
239 (34%) |
229 (42%) |
10 (14%) |
— |
— |
||||||||||
|
Intensive case management |
48 (7%) |
27 (5%) |
21 (30%) |
— |
— |
||||||||||
|
Financial counselling/government financial aid |
45 (6%) |
43 (8%) |
2 (3%) |
— |
— |
||||||||||
|
Housing services |
22 (3%) |
19 (4%) |
3 (4%) |
— |
— |
||||||||||
|
Social work/welfare support |
16 (2%) |
12 (2%) |
4 (6%) |
— |
— |
||||||||||
|
Mental health support |
13 (2%) |
11 (2%) |
2 (3%) |
— |
— |
||||||||||
|
Alcohol and drug services |
3 (< 1%) |
2 (< 1%) |
1 (1%) |
— |
— |
||||||||||
|
Other |
12 (2%) |
8 (2%) |
4 (6%) |
— |
— |
||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; IQR = interquartile range; SD = standard deviation. * People on temporary visas (tourist, student, work visas). † Poorly controlled hypertension, cardiovascular disease, chronic respiratory disease, poorly controlled diabetes mellitus, immunosuppression, active malignancy, morbid obesity. ‡ Cough, upper respiratory tract symptoms, myalgia, dyspnoea, fever, gastrointestinal symptoms (nausea, diarrhoea). § Need for material and logistic assistance (eg, food, basic supplies). ¶ Crowded or unstable housing conditions, poor health literacy, alcohol or drug dependence, mental health problems, financial stress or unstable employment, need for interpreter for communication. ** Homelessness, unsafe home environment (risk of violence or physical danger), risk of alcohol withdrawal or using opioid substitution therapy. |
|||||||||||||||
Box 5 – Outcomes for the 711 people with COVID‐19 enrolled in the COVID Positive Pathway
|
|
|
Tier of care |
|||||||||||||
|
Characteristic |
All participants |
Low |
Medium A |
Medium B |
High |
||||||||||
|
|
|||||||||||||||
|
Participants: Initial care tier allocation* |
711 |
542 |
70 |
43 |
56 |
||||||||||
|
Participants: in care tier at any time |
— |
575 |
92 |
63 |
64 |
||||||||||
|
Clinical course |
|
|
|
|
|
||||||||||
|
Length of stay (days), median (IQR) |
9 (6–10) |
10 (7–30) |
10 (6–13) |
8 (5–13) |
10 (7–30) |
||||||||||
|
Single care tier only |
658 (93%) |
533 (93%) |
45 (49%) |
29 (46%) |
51 (80%) |
||||||||||
|
Required higher tier care than on enrolment |
35 (5%) |
9 (2%) |
16 (17%) |
10 (16%) |
— |
||||||||||
|
Completed isolation in Pathway |
654 (92%) |
527 (92%) |
54 (59%) |
36 (57%) |
37 (58%) |
||||||||||
|
Withdrew from Pathway |
52 (7%) |
15 (3%) |
15 (16%) |
7 (11%) |
15 (23%) |
||||||||||
|
Died |
12 (2%) |
0 |
1 (1%) |
0 |
11 (17%) |
||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; IQR = interquartile range. * Some participants received care in more than one tier; proportions in this table are based on initial care tier allocation. |
|||||||||||||||
Received 5 August 2021, accepted 9 December 2021
- Seok Ming Lim1,2
- Nicole L Allard3,4
- Janelle Devereux5
- Benjamin C Cowie6,7
- Michelle Tydeman3
- Alistair Miller8
- Khanh Ho8
- Brigitte Cleveland8
- Liz Singleton8
- Karen Aarons9
- Paul Eleftheriou10
- Thomas Chan11
- George Braitberg1,2
- Andrea Maier1,11
- 1 The Royal Melbourne Hospital, Melbourne, VIC
- 2 The University of Melbourne, Melbourne, VIC
- 3 Cohealth, Melbourne, VIC
- 4 Peter Doherty Institute for Infection and Immunity, the University of Melbourne, Melbourne, VIC
- 5 North Western Melbourne Primary Health Network, Melbourne, VIC
- 6 WHO Collaborating Centre for Viral Hepatitis, Melbourne, VIC
- 7 Victorian Infectious Diseases Service, Royal Melbourne Hospital, Melbourne, VIC
- 8 Djerriwarrh Health Services, Bacchus Marsh, VIC
- 9 Western Health, Melbourne, VIC
- 10 Werribee Mercy Hospital, Melbourne, VIC
- 11 Vrije Universiteit Amsterdam, Amsterdam, The Netherlands
The Victorian Department of Health and Human Services funded the conception and design of the health services project described in this article.
No relevant disclosures.
- 1. MacIntyre CR. Navigating post‐vaccine COVID‐19 futures in the health and economic context. Lancet Infect Dis 2021; 21: 893–894.
- 2. Chen H, Shi L, Zhang Y, et al. A cross‐country core strategy comparison in China, Japan, Singapore and South Korea during the early COVID‐19 pandemic. Global Health 2021; 17: 22.
- 3. Nihlén Fahlquist J. The moral responsibility of governments and individuals in the context of the coronavirus pandemic. Scand J Public Health 2021; 49: 815–820.
- 4. Public Accounts and Estimates Committee (Parliament of Victoria). Inquiry into the Victorian government’s response to the COVID‐19 pandemic (PP No 103, session 2018–2020). Feb 2021. https://www.parliament.vic.gov.au/file_uploads/PAEC_59‐08_Vic_Gov_response_to_COVID‐19_pandemic_YKNbjt2Y.pdf (viewed Aug 2021).
- 5. Parliament of Victoria. Health Records Act 2001; authorised version incorporating amendments as at 27 August 2020. https://content.legislation.vic.gov.au/sites/default/files/2020‐08/01‐2aa046%20authorised.pdf (viewed June 2021).
- 6. Parliament of Victoria. Health Services Act 1988; authorised version incorporating amendments as at 1. November 2021. https://content.legislation.vic.gov.au/sites/default/files/2021‐11/88‐49aa174%20authorised.pdf (viewed Apr 2021).
- 7. Baldi E, Sechi GM, Mare C, et al. Lombardia CARe researchers. COVID‐19 kills at home: the close relationship between the epidemic and the increase of out‐of‐hospital cardiac arrests. Eur Heart J 2020; 41: 3045–3054.
- 8. Australian Bureau of Statistics. Regional population by age and sex, reference period. 2020. 27 Aug 2021. https://www.abs.gov.au/statistics/people/population/regional‐population‐age‐and‐sex/latest‐release (viewed Apr 2021).
- 9. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap): a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42: 377–381.
- 10. Thevarajan I, Buising KL, Cowie BC. Clinical presentation and management of COVID‐19. Med J Aust 2020; 213: 134–139. https://www.mja.com.au/journal/2020/213/3/clinical‐presentation‐and‐management‐covid‐19
- 11. Caplan GA, Sulaiman NS, Mangin DA, et al. A meta‐analysis of “hospital in the home”. Med J Aust 2012; 197: 512–519. https://www.mja.com.au/journal/2012/197/9/meta‐analysis‐hospital‐home
- 12. North Western Melbourne Public Health Network. Coronavirus disease (COVID‐19) information for primary health care providers. Updated 17 Feb 2022. https://nwmphn.org.au/for‐primary‐care/covid‐19 (viewed Feb 2022).
- 13. Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf 2016; 25: 986–992.
- 14. Kucharski AJ, Klepac P, Conlan AJK, et al; CMMID COVID‐19 working group. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS‐CoV‐2 in different settings: a mathematical modelling study. Lancet Infect Dis 2020; 20: 1151–1160.
- 15. Bodas M, Peleg K. Self‐isolation compliance in the COVID‐19 era influenced by compensation: findings from a recent survey in Israel. Health Aff 2020; 39: 936–941.
- 16. Paremoer L, Nandi S, Serag H, Baum F. Covid‐19 pandemic and the social determinants of health. BMJ 2021; 372: n129.
- 17. Australian Bureau of Statistics. 2033.0.55.001. Census of population and housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2016. 27 Mar 2018. https://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/2033.0.55.0012016 (viewed June 2021).
- 18. Higginson S, Milovanovic K, Gillespie J, et al. COVID‐19: the need for an Australian economic pandemic response plan. Health Policy Technol 2020; 9: 488–502.
- 19. Sitammagari K, Murphy S, Kowalkowski M, et al. Insights from rapid deployment of a “virtual hospital” as standard care during the COVID‐19 pandemic. Ann Intern Med 2021; 174: 192–199.
- 20. Ferry OR, Moloney EC, Spratt OT, et al. A virtual ward model of care for patients with COVID‐19: retrospective single‐center clinical study. J Med Internet Res 2021; 23: e25518.
- 21. Hutchings OR, Dearing C, Jagers D, et al. Virtual health care for community management of patients with COVID‐19 in Australia: observational cohort study. J Med Internet Res 2021; 23: e21064.
- 22. Capp R, Misky GJ, Lindrooth RC, et al. Coordination program reduced acute care use and increased primary care visits among frequent emergency care users. Health Aff (Millwood) 2017; 36: 1705–1711.
- 23. Australian Department of Health. 2020‒25 National health reform agreement (NHRA). Updated 19 Oct 2020. https://www.health.gov.au/initiatives‐and‐programs/2020‐25‐national‐health‐reform‐agreement‐nhra (viewed Oct 2021).





Abstract
Objectives: To assess the capacity of the COVID Positive Pathway, a collaborative model of care involving the Victorian public health unit, hospital services, primary care, community organisations, and the North Western Melbourne Primary Health Network, to support people with coronavirus disease 2019 (COVID‐19) isolating at home.
Design, setting, participants: Cohort study of adults in northwest Melbourne with COVID‐19, 3 August ‒ 31 December 2020.
Main outcome measures: Demographic and clinical characteristics, and social and welfare needs of people cared for in the Pathway, by care tier level.
Results: Of 1392 people referred to the Pathway by the public health unit, 858 were eligible for enrolment, and 711 consented to participation; 647 (91%) remained in the Pathway until they had recovered and isolation was no longer required. A total of 575 participants (81%) received care in primary care, mostly from their usual general practitioners; 155 people (22%) received care from hospital outreach services, and 64 (9%) needed high tier care (hospitalisation). Assistance with food and other basic supplies was required by 239 people in the Pathway (34%).
Conclusions: The COVID Positive Pathway is a feasible multidisciplinary, tiered model of care for people with COVID‐19. About 80% of participants could be adequately supported by primary care and community organisations, allowing hospital services to be reserved for people with more severe illness or with risk factors for disease progression. The principles of this model could be applied to other health conditions if regulatory and funding barriers to information‐sharing and care delivery by health care providers can be overcome.