The prevalence of rheumatic heart disease in Timor‐Leste, a lower middle income country of about 1.3 million people and one hour from Australia, is among the highest in the world.1 The East Timor Hearts Fund (ETHF; https://easttimorheartsfund.org.au) is the primary facilitator of access to cardiac procedures for people in Timor‐Leste.2 At the start of the coronavirus disease 2019 (COVID‐19) pandemic, both Australia and Timor‐Leste closed their international borders, and no Timorese patients have undergone cardiac surgery in Australia since March 2020. However, the ETHF has continued to provide remote care in the form of telehealth clinics.
In March 2020 and August 2021, we assessed the status of East Timorese people on the ETHF waiting list for cardiac procedures in Australia. If we could not contact a patient, we sought information about their status from the Hospital Nacional Guido Valadares and the two largest community medical centres in Dili (Bairo Pite Clinic Lanud and Maluk Timor). The St Vincent’s Hospital Melbourne Human Research Ethics Committee approved our study (QA 21037).
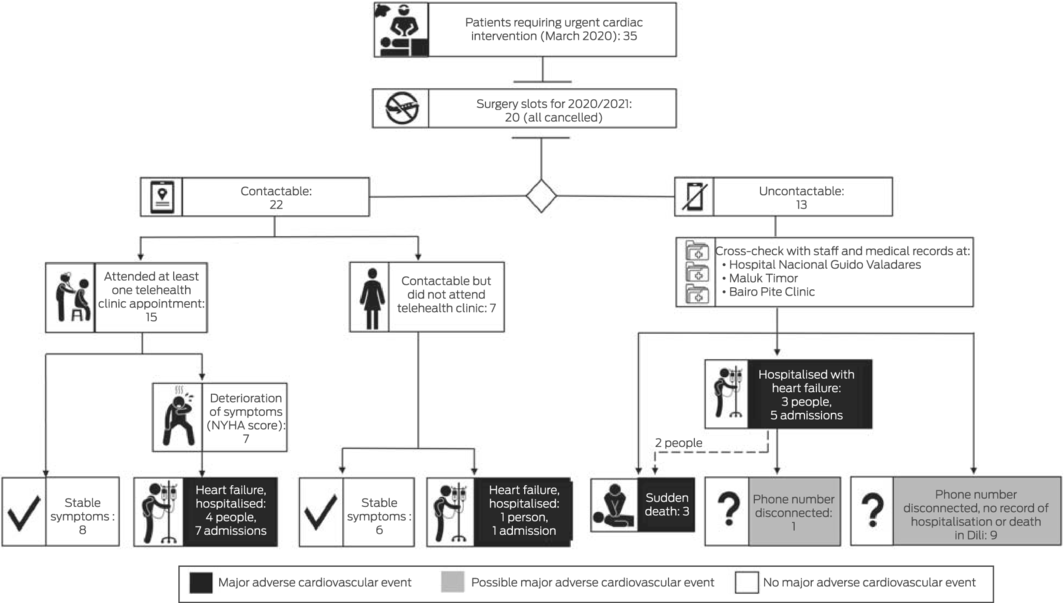
On 1 March 2020, 35 Timorese people were waiting for cardiac procedures in Australia, including 26 with rheumatic heart disease and nine with congenital cardiac disease (Box 1). By 31 August 2021, three people had died, and thirteen had been admitted to hospital with decompensated heart failure. The median New York Heart Association score declined from II (mild limitation of physical activity) in March 2020 to III (marked limitation) for the 15 people who attended ETHF online telehealth clinics during 2020 or 2021 (seven with lower, eight with stable scores). Of thirteen people who could not be contacted for follow‐up, three had died suddenly; the status of ten whose phone numbers were no longer current was unknown (Box 2).
The COVID‐19 border closures delayed cardiac interventions for our young patients by at least 18 months. Systemic delays in usual health care during the pandemic have increased morbidity and mortality in Australia, and not just for people with COVID‐19.3 In the case of Timor‐Leste, international border closures abruptly removed access to cardiac procedures for an entire nation.
The poor outcomes for many East Timorese people with cardiac disease during the pandemic also highlight the inherent uncertainty of fly‐in/fly‐out volunteer medical services. Over the past decade, ETHF has supported the development of local expertise, and the Timor‐Leste medical system has expanded markedly since independence in 2002. However, the COVID‐19 pandemic cut access to overseas cardiac procedures. About 60 non‐governmental organisations have cardiac surgery programs in low and middle income countries, with short term mission approaches similar to that of ETHF;4 it is likely that border closures also reduced access to cardiac surgery in other countries.
The COVID‐19 pandemic further restricted the access of low and middle income countries to surgical services, “with uncertain loss of function and risk of adverse prognosis as a collateral effect of the pandemic.”5 One‐quarter of our young patients waiting for cardiac surgery experienced major adverse cardiovascular events during the pandemic, including three who died. Sudden border closures that remove access to humanitarian surgery highlight the vulnerabilities of short term medical mission models, and raise concerns that levels of undiagnosed disease in Timor‐Leste may be higher after the COVID‐19 pandemic has ended.
Box 1 – Characteristics of 35 people in Timor‐Leste on the waiting list for cardiac procedures in Australia, 1 March 2020
|
Characteristic |
|
||||||||||||||
|
|
|||||||||||||||
|
Age (years), median (IQR) |
27 (19–34) |
||||||||||||||
|
Sex (men) |
11 (31%) |
||||||||||||||
|
Rheumatic heart disease |
26 (74%) |
||||||||||||||
|
Located in Dili |
23 (66%) |
||||||||||||||
|
NYHA class, median (IQR): most recent face‐to‐face review in March 2020 |
II (I–II) |
||||||||||||||
|
NYHA class, median (IQR): 15 people who attended online clinics in 2020 or 2021 |
III (II–III) |
||||||||||||||
|
Time on waiting list (to 1 March 2020; months), median (IQR) |
4 (4–13) |
||||||||||||||
|
Confirmed major adverse cardiovascular event |
9 (26%) |
||||||||||||||
|
|
|||||||||||||||
|
IQR = interquartile range; NYHA = New York Heart Association. |
|||||||||||||||
Received 25 September 2021, accepted 23 December 2021
- 1. Davis K, Remenyi B, Draper AD, et al. Rheumatic heart disease in Timor‐Leste school students: an echocardiography‐based prevalence study. Med J Aust 2018; 208: 303–307. https://www.mja.com.au/journal/2018/208/7/rheumatic‐heart‐disease‐timor‐leste‐school‐students‐echocardiography‐based
- 2. Paratz ED, Mock N, Gutman SJ, et al. Taking the pulse of Timor‐Leste’s cardiac needs: a 10‐year descriptive time‐trend analysis. Intern Med J 2020; 50: 838–845.
- 3. Degeling K, Baxter NN, Emery J, et al. An inverse stage‐shift model to estimate the excess mortality and health economic impact of delayed access to cancer services due to the COVID‐19 pandemic. Asia Pac J Clin Oncol 2021; 17: 359–367.
- 4. Ng‐Kamstra JS, Riesel JN, Arya S, et al. Surgical non‐governmental organizations: global surgery’s unknown nonprofit sector. World J Surg 2016; 40: 1823–1841.
- 5. Søreide K, Hallet J, Matthews JB, et al. Immediate and long‐term impact of the COVID‐19 pandemic on delivery of surgical services. Br J Surg 2020; 107: 1250–1261.





We acknowledge the contributions by the other East Timor Hearts Fund members (Will Wilson, Virag Kushwaha, Simon Eggleton, David Marlow, Nicki Mock, Diana Marques, Louise Creati, Sarah Gutman, Peter Barlis, Ari Horton) and by the Maluk Timor staff (Jess Harries, Anary dos Santos da Silva, Sergio da Silva, Juliana Saramento).
No relevant disclosures.