The known: Out‐of‐hospital cardiac arrest is a major cause of death in Australia. Symptom recognition, early activation of emergency medical services, and timely defibrillation improve survival.
The new: People who had cardiac arrests in general practices and were defibrillated by clinic staff with automated external defibrillators (AEDs) were twice as likely to survive as patients not defibrillated until after paramedics arrived.
The implications: Patients experiencing cardiac symptoms should immediately call emergency health services (000). Further, AEDs should be standard equipment in general practice clinics to enable prompt defibrillation when required.
More than 25 000 out‐of‐hospital cardiac arrests are recorded in Australia each year; the mean survival rate to hospital discharge or 30 days is 12%.1 Survival is higher for people who call emergency medical services immediately after experiencing the warning symptoms of a heart attack.2 However, some people instead seek the help of general practitioners;3,4 the delay in alerting emergency medical services is associated with increased risk of cardiac arrest before paramedics arrive, which in turn is associated with lower survival.5,6 The frequency and outcomes of cardiac arrests in general practice clinics have not been well described, and it is unclear whether general practice staff are adequately prepared for managing them.
To effectively manage a patient experiencing a cardiac arrest, clinic staff must immediately undertake the initial steps in the “chain of survival”: call 000, provide cardiopulmonary resuscitation, and perform defibrillation with an automated external defibrillator (AED).7 Although clinic administrative staff must undertake cardiopulmonary resuscitation training every three years, accreditation by the Royal Australian College of General Practitioners does not require general practices to have onsite AEDs.8
In this study, we compared the frequency and outcomes of cardiac arrests in general practice clinics with those of paramedic‐witnessed cases.
Methods
We undertook a retrospective analysis of Victorian Ambulance Cardiac Arrest Registry (VACAR) data on cardiac arrests in patients paramedics attempted to resuscitate. We included cardiac arrests in general practice clinics and those witnessed by paramedics during 1 January 2000 – 31 December 2019; arrests secondary to trauma, in terminally ill patients, or in people for whom resuscitation was not attempted were not included.
Setting
In Victoria (population, 6.5 million people; area, 227 444 square kilometres9), pre‐hospital emergency care is provided by Ambulance Victoria. Cardiopulmonary resuscitation instructions are provided to people who call 000 if the call‐taker suspects a cardiac arrest. A three‐tiered response is simultaneously dispatched: basic life support first responders (metropolitan Melbourne and some areas of rural Victoria), advanced life support paramedics, and intensive care paramedics.10 Ambulance Victoria cardiac arrest treatment guidelines follow the recommendations of the Australian Resuscitation Council.11
Data sources
The VACAR is a population registry of cardiac arrests in Victoria attended by emergency medical services staff.12 In brief, an advanced search algorithm searches electronic patient care records daily to identify possible cases of cardiac arrest; registry staff screen and audit the records, capturing data on more than 150 variables, including Utstein style variables.12,13 For patients transported by paramedics, VACAR collects hospital discharge outcomes by reviewing hospital medical records and cross‐validating the data with the Victorian Registry of Births, Deaths and Marriages. We reviewed the paramedic narratives in patient care records for people who had cardiac arrests in general practice clinics to identify their main symptom, the time of onset of symptoms, and their medical history, together with information about the location of and witnesses to the resuscitation attempt.
Definitions
We used data definitions recommended by the Utstein guidelines.13 Cardiac arrest aetiology was based on information in the patient care record, and was assumed to be cardiac in nature if no clear precipitator was recorded. Response times for cardiac arrests witnessed by paramedics refer to time since the initial call to emergency services. Treated patients are defined as those for whom any form of cardiopulmonary resuscitation or defibrillation by emergency medical services personnel was attempted, or who were shocked with public access defibrillators. Cardiac arrests in general practice clinics are defined as those in clinic buildings or carparks prior to the arrival of paramedics; paramedic‐witnessed cardiac arrests are those in which the initial arrest was witnessed by paramedics, irrespective of location. Bystander cardiopulmonary resuscitation was any attempt at chest compression by non‐dispatched responders, with or without ventilation. Return of spontaneous circulation is defined as return of a palpable pulse during the resuscitation attempt.
Outcomes
The primary outcome was survival to hospital discharge. Secondary outcomes were factors associated with survival, and changes over 20 years in the baseline characteristics and survival of people who had cardiac arrests in general practice clinics.
Statistical analyses
All statistical analyses were undertaken in SPSS Statistics 25 (IBM); P < 0.05 (two‐sided) was deemed statistically significant. Categorical data are summarised as frequencies and proportions, continuous variables as medians with interquartile ranges (IQRs). The statistical significance of between group differences were assessed in Mann–Whitney U or χ2 tests as appropriate. Cardiac arrests in general practice clinics were grouped by 4‐year epoch (2000–2003, 2004–2007, 2008–2011, 2012–2015, 2016–2019), and changes in baseline characteristics over time assessed in χ2 linear‐by‐linear association tests (categorical variables) or Kendall τ‐b tests (continuous variables).
We assessed the impact of cardiac arrest location on survival to hospital discharge in multivariable logistic regression analyses adjusted for location, year, shock provider, initial rhythm, paramedic response time, aetiology, geographic region, sex, and age. In a subgroup analysis of patients who presented with initial shockable rhythms, we compared survival after defibrillation by paramedics (for paramedic‐witnessed events) and by clinic staff (for general practice clinic cases) with survival when defibrillation was not performed for patients who had cardiac arrests in general practice clinics until paramedics arrived. Logistic regression model outcomes are presented as adjusted odds ratios (aORs) with 95% confidence intervals (CIs).
Ethics approval
The Monash University Human Research Ethics Committee approved the study (project 12758). The VACAR has independent ethics approval from the Committee (project 21046) and site‐specific governance approval from more than 100 participating hospitals for collecting hospital outcomes data.
Results
We identified 104 110 cardiac arrests in Victoria during 2000–2019; 18 659 were trauma‐related or were in terminally ill patients, 78 047 had not occurred in general practice clinics or been witnessed by paramedics, and in 1041 cases resuscitation was not attempted. Of the remaining 6363 included cases of cardiac arrest (6.1%), 216 occurred in general practice clinics (3.4%) and 6147 were witnessed by paramedics (96.6%).
Patient characteristics
The proportion of cases with a presumed cardiac aetiology was larger for general practice clinic cases (200 of 216, 92.6%) than for arrests witnessed by paramedics (4768 of 6147, 77.6%), as was the proportion of patients with initial shockable rhythms (126, 58.3% v 1929, 31.4%). Raw survival to discharge rates were similar for general practice clinic (63, 29%) and paramedic‐witnessed cases (1766, 28.7%) (online Supporting Information).
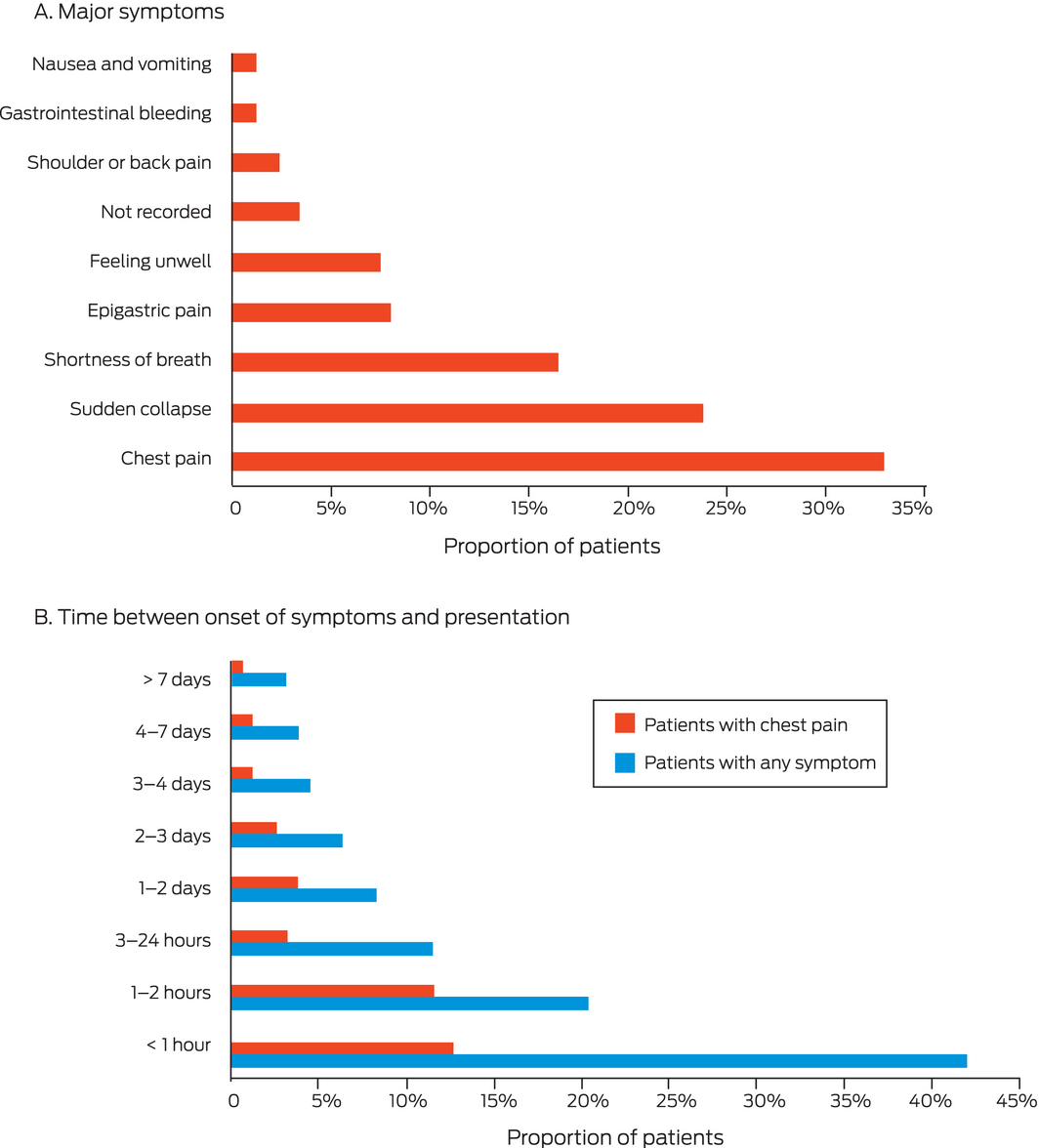
The most frequently recorded major symptoms in the paramedic narratives of the 176 available patient care records for people who had cardiac arrests in general practice clinics were chest pain (58, 33%), sudden collapse (42, 24%), and shortness of breath (29, 16%) (Box 1, A). Of the 157 patients with recorded times of symptom onset, chest pain had started for 38 patients (24%, or 66% of people with chest pain as their major symptom) more than one hour before attending the practice; the median time to visiting the practice for patients with chest pain as the major symptom was 12 hours (IQR, 2–24 hours) (Box 1, B).
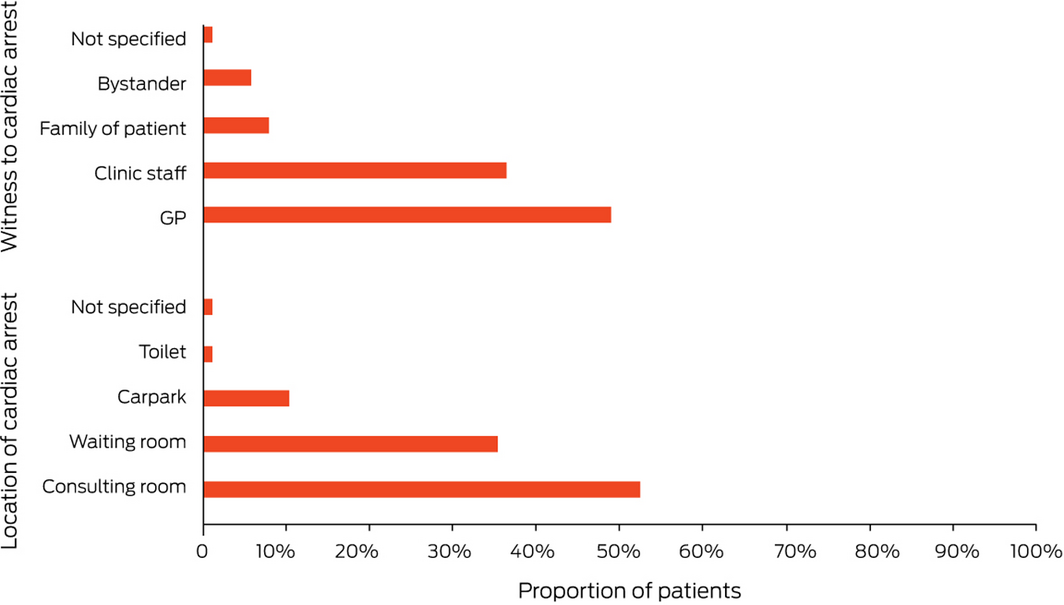
Of the 176 cases of cardiac arrest in general practice clinics with available patient care records, 92 occurred in consulting rooms (52%), 62 in waiting rooms (35%), and 18 in carparks (10%); 86 were initially witnessed by GPs (49%) and 64 by clinic staff (36%) (Box 2). A GP was present at resuscitation in 156 cases (89%).
A total of 2055 cardiac arrests were in patients with initial shockable rhythm (32.3%); of the 126 cases in general practice clinics, 47 patients were defibrillated by clinic staff (37%) and 79 received the first shock from arriving paramedics (63%). A larger proportion of general practice clinic cases were in metropolitan regions (111, 88.1%) than of paramedic‐witnessed events (1374 of 1929, 71.2%). Fifty‐seven patients who had arrests in general practice clinics (45%) survived to hospital discharge (including 27 of the 47 defibrillated by clinic staff [57%]), as did 1221 patients in paramedic‐witnessed cases (63.3%) (Box 3).
Changes in characteristics over time
The proportion of general practice cases in which defibrillation was provided in the clinic increased from 2 of 37 in 2000–2003 (5%) to 19 of 57 patients in 2016–2019 (33%); survival increased from 7 of 37 (19%) to 23 of 57 patients (40%) (Box 4). For patients presenting with shockable rhythms, the proportion undergoing general practice clinic defibrillation increased over the same period from 2 of 24 (8%) to 19 of 33 patients (58%), and survival increased from 7 of 24 (29%) to 20 of 33 patients (61%) (Box 5).
Survival to hospital discharge
Patient information was missing for 544 cardiac arrests (8.5%) and for 62 arrests in which patients presented with shockable rhythms (3%); we excluded these cases from our logistic regression analyses. After adjusting for confounding factors, survival to hospital discharge was more likely after paramedic‐witnessed cardiac arrests than after arrests in general practice clinics (aOR, 1.81; 95% CI, 1.33–2.47).
For patients with initial shockable rhythms, the odds of survival were greater following paramedic‐witnessed events than for general practice clinic arrests in which arriving paramedics provided defibrillation (ie, defibrillation was not undertaken by clinic staff; aOR, 3.39; 95% CI, 2.08–5.54). Survival of patients after arrests in general practices was greater when clinic staff provided defibrillation with a clinic AED rather than waiting for paramedics to arrive (aOR, 2.23; 95% CI, 1.03–4.83) (Box 6). Survival following paramedic‐witnessed cardiac arrests and arrests in general medical clinics with defibrillation by clinic staff was similar (aOR, 1.52; 95% CI, 0.82–2.81).
Discussion
Our findings reinforce the importance of rapid emergency medical service care for people with warning symptoms of cardiac arrest. For people with initial shockable rhythms, survival was more than three times as likely following paramedic‐witnessed cardiac arrests than events in general practice clinics that did not provide defibrillation. Many patients sought the help of GPs for typical cardiac warning symptoms, but 38 of 58 patients with chest pain as their chief symptom (66%) had experienced it for more than an hour before consulting their GP. It has been reported that patients having paramedic‐witnessed cardiac arrests presented with similar symptoms to those in general practice clinics, but one‐third were in profound shock at the time of assessment, and consciousness was altered in almost 40%;14 that is, they are generally more critically ill than people who experience arrests in general practice clinics.
The value of early defibrillation is reinforced by our study: the likelihood of survival was more than twice as high for general practice clinic patients for whom the first shock was administered by clinic staff with an onsite AED than in clinics in which it was provided by arriving paramedics. Similar differences in survival between people defibrillated promptly with public access AEDs or by arriving paramedics have been reported.15,16 When the first shock was delivered with a clinic AED, 27 of 47 patients survived to hospital discharge (57%), similar to the proportions in a study of AED‐equipped general practice clinics in the United Kingdom: 63% for people with GP‐witnessed arrests, and 54% when a GP was nearby.17
A number of factors may have contributed to higher survival following paramedic‐witnessed cardiac arrests in our study. Firstly, not all cardiac arrests in general practice clinics were witnessed by GPs, and other clinic staff initially cared for the patients. Secondly, in paramedic‐witnessed cases the attending paramedics probably initiated cardiac monitoring, facilitating prompt rapid defibrillation when appropriate. Thirdly, paramedics have more experience of resuscitation events and training than most GPs, and this familiarity is associated with higher survival rates.18 In Ireland, the Medical Emergency Responders Integration and Training project (MERIT) alerts GPs to cardiac arrests in their communities, increasing their experience of resuscitation.19 Importantly, their presence also enables them to consider end‐of‐life directives and, if required, to compassionately manage death and family support.
As cardiac arrests in general practice clinics are rare and GPs may not always be present, all clinic staff should receive regular refresher training in cardiopulmonary resuscitation and AED use, including skills in debriefing and supporting relatives.20 In Victoria, they should also be encouraged to download the GoodSAM app (https://www.ambulance.vic.gov.au/goodsam), which will alert them to nearby cases so that they can provide early cardiopulmonary resuscitation and defibrillation.
The limited availability of AEDs in Victorian general practice clinics may partly explain why the likelihood of survival after cardiac arrests was 45% lower than after paramedic‐witnessed cardiac arrests. Although the proportion of people with cardiac arrests in general practices who were defibrillated by clinic staff increased during the study period, 17 of 36 patients who received defibrillation in clinics during 2016–2019 (47%) were not shocked until after paramedics arrived. The importance of AEDs in general practice clinics has been recognised overseas: the British Heart Foundation donated more than 1200 AEDs to GPs over a nineteen‐year period,17 and the MERIT project has provided more than 500 AEDs to participating GPs in Ireland.19 A survey of 200 Australian general practices in 2005 found that only 18% had AEDs,21 while surveys in Denmark (2013)22 and Ireland (2015)23 respectively found that 32% or 67% of general practice clinics had AEDs. The United Kingdom Resuscitation Council requires that primary care facilities have immediate access to AEDs,24 in contrast to the Royal Australian College of General Practitioners.8 As public access AEDs are now often available in locations such as Woolworths and Coles supermarkets, patients expect general practice clinics to have AEDs.25
Limitations
We could not ascertain the availability or quality of cardiopulmonary resuscitation provided in general practice clinics, which could influence patient outcomes. Onset of symptoms and medical histories were not always fully recorded in patients’ care records, and patient care records were unavailable for 62 people who had cardiac arrests in general practice clinics (29%). The number of clinic cases was relatively small, which may affect the reliability of our between group comparisons. We did not adjust our analyses for hospital treatment and interventions that would have influenced survival.
Conclusion
We recommend that all patients with heart attack warning symptoms immediately call emergency medical services, not visit general practice clinics. All general practice clinic staff should be trained to manage people having cardiac arrests, including in providing rapid defibrillation with an onsite AED. These measures could substantially reduce mortality for patients who have cardiac arrests in general practice clinics.
Box 1 – Major symptoms for 176 people who had cardiac arrests in general practice clinics, and onset of symptoms for 157 people who had cardiac arrests in general practice clinics
Box 2 – Cardiac arrest location and witnesses for 176 people who had cardiac arrests in general practice clinics
Box 3 – Characteristics of cases of cardiac arrests in patients with initial shockable rhythm
|
|
Location of cardiac arrest |
|
|||||||||||||
|
Characteristic |
All arrests |
In general practice clinics |
Witnessed by paramedics |
P |
|||||||||||
|
|
|||||||||||||||
|
Number of cardiac arrests |
2055 |
126 |
1929 |
|
|||||||||||
|
Age (years), median (IQR) |
67 (55–78) |
71 (61–79) |
66 (55–78) |
0.06 |
|||||||||||
|
Sex (men) |
1499 (72.9%) |
99 (79%) |
1400 (72.6%) |
0.18 |
|||||||||||
|
Bystander cardiopulmonary resuscitation |
122 (5.9%) |
122 (97%) |
NA |
NA |
|||||||||||
|
Metropolitan region |
1485 (72.3%) |
111 (88%) |
1374 (71.2%) |
< 0.001 |
|||||||||||
|
EMS response time (min), median (IQR) |
10 (7–14) |
7 (5–9) |
10 (8–15) |
< 0.001 |
|||||||||||
|
Cardiac aetiology |
1942 (94.5%) |
124 (98%) |
1818 (94.2%) |
0.07 |
|||||||||||
|
General practice clinic defibrillation |
47 (2.3%) |
47 (37%) |
NA |
NA |
|||||||||||
|
Paramedic defibrillation |
2008 (97.7%) |
79 (63%) |
1929 (100%) |
< 0.001 |
|||||||||||
|
Return of spontaneous circulation |
1646 (80.1%) |
85 (68%) |
1561 (80.9%) |
< 0.001 |
|||||||||||
|
Pulse present on arrival at hospital |
1520 (74.0%) |
79 (63%) |
1441 (74.7%) |
0.004 |
|||||||||||
|
Survival to hospital discharge* |
1278 (62.2%) |
57 (45%) |
1221 (63.3%) |
< 0.001 |
|||||||||||
|
|
|||||||||||||||
|
EMS = emergency medical services; IQR = interquartile range; NA = not applicable. * Proportions exclude missing data: two general practice clinic cases, 47 paramedic‐witnessed cases. |
|||||||||||||||
Box 4 – Characteristics of cardiac arrests that occurred in general clinics, by epoch
|
Characteristic |
2000–2019 |
2000–2003 |
2004–2007 |
2008–2011 |
2012–2015 |
2016–2019 |
P |
||||||||
|
|
|||||||||||||||
|
Number of cardiac arrests |
216 |
37 |
29 |
33 |
60 |
57 |
|
||||||||
|
Age (years), median (IQR) |
70 (59–79) |
68 (55–73) |
70 (60–78) |
69 (56–78) |
71 (57–81) |
73 (61–81) |
0.19 |
||||||||
|
Sex (men) |
148 (68%) |
25 (68%) |
19 (66%) |
20 (61%) |
45 (75%) |
39 (68%) |
0.58 |
||||||||
|
Bystander cardiopulmonary resuscitation |
194 (90%) |
34 (92%) |
23 (79%) |
28 (85%) |
58 (97%) |
51 (90%) |
0.41 |
||||||||
|
Metropolitan region |
187 (87%) |
36 (97%) |
26 (90%) |
32 (97%) |
46 (77%) |
47 (83%) |
0.007 |
||||||||
|
EMS response time (min), median (IQR) |
7 (5–9) |
6 (5–8) |
7 (5–10) |
8 (6–9) |
7 (5–9) |
7 (5–9) |
0.23 |
||||||||
|
Cardiac aetiology |
200 (93%) |
36 (97%) |
27 (93%) |
30 (91%) |
57 (95%) |
50 (88%) |
0.16 |
||||||||
|
Initial shockable rhythm |
126 (58%) |
24 (65%) |
12 (41%) |
13 (39%) |
44 (73%) |
33 (58%) |
0.45 |
||||||||
|
General practice clinic defibrillation |
47 (22%) |
2 (5%) |
0 |
2 (6%) |
24 (40%) |
19 (33%) |
< 0.001 |
||||||||
|
Paramedic defibrillation |
99 (46%) |
26 (70%) |
19 (66%) |
15 (46%) |
23 (38%) |
17 (30%) |
< 0.001 |
||||||||
|
Return of spontaneous circulation |
126 (58%) |
16 (43%) |
14 (48%) |
18 (55%) |
42 (70%) |
36 (63%) |
0.010 |
||||||||
|
Pulse present on arrival at hospital |
112 (52%) |
14 (38%) |
14 (48%) |
14 (42%) |
37 (62%) |
33 (58%) |
0.022 |
||||||||
|
Survival to hospital discharge* |
62 (29%) |
7 (19%) |
7 (24%) |
8 (24%) |
18 (30%) |
23 (40%) |
0.025 |
||||||||
|
|
|||||||||||||||
|
EMS = emergency medical services; IQR = interquartile range. * Proportions exclude missing data: 2000‒2003, one case; 2008‒2011, two cases. |
|||||||||||||||
Box 5 – Characteristics of cardiac arrests that occurred in general clinics for patients with initial shockable rhythms, by epoch
|
Characteristic |
2000–2019 |
2000–2003 |
2004–2007 |
2008–2011 |
2012–2015 |
2016–2019 |
P |
||||||||
|
|
|||||||||||||||
|
Number of cardiac arrests |
126 |
24 |
12 |
13 |
44 |
33 |
|
||||||||
|
Age (years), median (IQR) |
71 (61–79) |
69 (63–73) |
75 (65–78) |
76 (55–84) |
71 (56–80) |
73 (58–80) |
0.65 |
||||||||
|
Sex (men) |
99 (79%) |
19 (79%) |
8 (67%) |
11 (85%) |
35 (80%) |
26 (79%) |
0.80 |
||||||||
|
Bystander cardiopulmonary resuscitation |
122 (97%) |
23 (96%) |
11 (92%) |
13 (100%) |
43 (98%) |
32 (97%) |
0.58 |
||||||||
|
Metropolitan region |
111 (88.1%) |
24 (100%) |
12 (100%) |
13 (100%) |
32 (73%) |
30 (91%) |
0.023 |
||||||||
|
EMS response time (min), median (IQR) |
7 (5–9) |
6 (5–8) |
6 (5–10) |
7 (4–9) |
8 (5–10) |
7 (6–9) |
0.15 |
||||||||
|
Cardiac aetiology |
124 (98%) |
24 (100%) |
12 (100%) |
13 (100%) |
42 (96%) |
33 (100%) |
0.55 |
||||||||
|
General practice clinic defibrillation |
47 (37%) |
2 (8%) |
0 |
2 (15%) |
24 (55%) |
19 (58%) |
< 0.001 |
||||||||
|
Paramedic defibrillation |
79 (63%) |
22 (92%) |
12 (100%) |
11 (85%) |
20 (46%) |
14 (42%) |
< 0.001 |
||||||||
|
Return of spontaneous circulation |
85 (68%) |
12 (50%) |
9 (75%) |
9 (69%) |
32 (73%) |
23 (70%) |
0.14 |
||||||||
|
Pulse present on arrival at hospital |
79 (63%) |
10 (42%) |
9 (75%) |
8 (62%) |
30 (68%) |
22 (67%) |
0.08 |
||||||||
|
Survival to hospital discharge* |
57 (45%) |
7 (29%) |
6 (50%) |
6 (46%) |
18 (41%) |
20 (61%) |
0.08 |
||||||||
|
|
|||||||||||||||
|
EMS = emergency medical services; IQR = interquartile range. * Proportions exclude missing data: 2000‒2003, one case; 2008‒2011, one case. |
|||||||||||||||
Box 6 – Survival to hospital discharge: multivariate logistic regression analyses
|
|
Adjusted odds ratio (95% confidence interval) |
||||||||||||||
|
Characteristic |
All patients |
Patients with initial shockable rhythm |
|||||||||||||
|
|
|||||||||||||||
|
Age, by year |
0.98 (0.97–0.98) |
0.97 (0.96–0.98) |
|||||||||||||
|
Sex (men v women) |
1.16 (1.00–1.34) |
1.26 (1.02–1.57) |
|||||||||||||
|
Location (paramedic‐witnessed v general practice clinic) |
1.81 (1.33–2.47) |
NA |
|||||||||||||
|
Geographic region (metropolitan v regional) |
1.48 (1.26–1.74) |
1.42 (1.13–1.77) |
|||||||||||||
|
Aetiology (cardiac v non‐cardiac) |
1.44 (1.19–1.75) |
4.47 (2.88–6.96) |
|||||||||||||
|
EMS response time, per minute |
1.00 (1.00–1.01) |
1.00 (0.99–1.01) |
|||||||||||||
|
Initial rhythm (shockable v non‐shockable) |
12.2 (10.5–14.1) |
NA |
|||||||||||||
|
Initial shock provider |
|
|
|||||||||||||
|
Arriving paramedics (general practice clinic arrests) |
NA |
1 |
|||||||||||||
|
Clinic staff (general practice clinic arrests) |
NA |
2.23 (1.03–4.83) |
|||||||||||||
|
Paramedics (paramedic‐witnessed arrests) |
NA |
3.39 (2.08–5.54) |
|||||||||||||
|
Year of arrest |
|
|
|||||||||||||
|
2000–2003 |
1 |
1 |
|||||||||||||
|
2004–2007 |
1.23 (0.93–1.62) |
0.92 (0.63–1.33) |
|||||||||||||
|
2008–2011 |
1.49 (1.15–1.94) |
1.27 (0.89–1.81) |
|||||||||||||
|
2012–2015 |
1.57 (1.22–2.01) |
1.34 (0.95–1.89) |
|||||||||||||
|
2016–2019 |
1.46 (1.14–1.87) |
1.29 (0.91–1.82) |
|||||||||||||
|
|
|||||||||||||||
|
EMS = emergency medical services; NA = not applicable. Patient information was missing for 544 included cardiac arrests (8.5%) and 62 cardiac arrests with initial shockable rhythms (3%); these cases were excluded from the logistic regression analyses. |
|||||||||||||||
Received 15 December 2020, accepted 22 April 2021
- Brian Haskins1,2
- Ziad Nehme2,3
- Peter A Cameron1,2,4
- Karen Smith1,2,3
- 1 NHMRC Centre of Research Excellence in Pre‐hospital Emergency Care Australia and New Zealand (PEC‐ANZ), Monash University, Melbourne, VIC
- 2 Monash University, Melbourne, VIC
- 3 Centre for Research and Evaluation, Ambulance Victoria, Melbourne, VIC
- 4 The Alfred Hospital, Melbourne, VIC
Brian Haskins holds a PhD scholarship from the National Health and Medical Research Council (NHMRC) Centre of Research Excellence in Pre‐hospital Emergency Care Australia and New Zealand (PEC‐ANZ), Ziad Nehme an NHMRC Early Career Fellowship (APP1146809), and Peter A Cameron a Medical Research Future Fund practitioner fellowship (MRF1139686).
Brian Haskins sits on the board of advisers for Defibsplus.
- 1. Beck B, Bray J, Cameron P, et al; Aus‐ROC Steering Committee. Regional variation in the characteristics, incidence and outcomes of out‐of‐hospital cardiac arrest in Australia and New Zealand: results from the Aus‐ROC Epistry. Resuscitation 2018; 126: 49–57.
- 2. Nishiyama C, Iwami T, Kawamura T, et al. Prodromal symptoms of out‐of‐hospital cardiac arrests: a report from a large‐scale population‐based cohort study. Resuscitation 2013; 84: 558–563.
- 3. Colquhoun MC. Resuscitation in general practice: time for action. Resuscitation 2014; 85: 5–6.
- 4. Barry T, Headon M, Glynn R, et al. Ten years of cardiac arrest resuscitation in Irish general practice. Resuscitation 2018; 126: 43–48.
- 5. Nehme Z, Andrew E, Bernard S, Smith K. Comparison of out‐of‐hospital cardiac arrest occurring before and after paramedic arrival: epidemiology, survival to hospital discharge and 12‐month functional recovery. Resuscitation 2015; 89: 50–57.
- 6. Nehme Z, Bernard S, Andrew E, et al. Warning symptoms preceding out‐of‐hospital cardiac arrest: do patient delays matter? Resuscitation 2018; 123: 65–70.
- 7. Olasveengen TM, Mancini ME, Perkins GD, et al; Adult Basic Life Support Collaborators. Adult basic life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2020; 142: S41–S91.
- 8. Royal Australian College of General Practitioners. Standards for general practices. 5th ed. Updated Apr 2021. https://www.racgp.org.au/running‐a‐practice/practice‐standards/standards‐5th‐edition/standards‐for‐general‐practices‐5th‐ed (viewed Apr 2021).
- 9. Australian Bureau of Statistics. National, state and territory population, Dec 2018. https://www.abs.gov.au/statistics/people/population/national‐state‐and‐territory‐population/latest‐release#data‐download (viewed Aug 2019).
- 10. Smith KL, McNeil JJ; the Emergency Medical Response Steering Committee. Cardiac arrests treated by ambulance paramedics and fire fighters. Med J Aust 2002; 177: 305–309. https://www.mja.com.au/journal/2002/177/6/cardiac‐arrests‐treated‐ambulance‐paramedics‐and‐fire‐fighters
- 11. Australian Resuscitation Council. ANZCOR guideline 11.2. Protocols for adult advanced life support. Updated Aug 2018. https://secureservercdn.net/198.71.190.10/777.066.myftpupload.com/download/section_11/anzcor‐guideline‐11‐2‐protocols‐august‐2018.pdf (viewed July 2020).
- 12. Nehme Z, Bernard S, Cameron P, et al. Using a cardiac arrest registry to measure the quality of emergency medical service care: decade of findings from the Victorian Ambulance Cardiac Arrest Registry. Circ Cardiovasc Qual Outcomes. 2015; 8: 56–66.
- 13. Perkins GD, Jacobs IG, Nadkarni VM, et al; Utstein Collaborators. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out‐of‐hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Circulation 2015; 132: 1286–1300.
- 14. Nehme Z, Andrew E, Bray JE, et al. The significance of pre‐arrest factors in out‐of‐hospital cardiac arrests witnessed by emergency medical services: a report from the Victorian Ambulance Cardiac Arrest Registry. Resuscitation 2015; 88: 35–42.
- 15. Nehme Z, Andrew E, Haskins B, et al. Trends in survival from out‐of‐hospital cardiac arrests defibrillated by paramedics, first responders and bystanders. Resuscitation 2019; 143: 85–91.
- 16. Pollack RA, Brown SP, Rea T, et al; ROC Investigators. Impact of bystander automated external defibrillator use on survival and functional outcomes in shockable observed public cardiac arrests. Circulation 2018; 137: 2104–2113.
- 17. Colquhoun M. Resuscitation by primary care doctors. Resuscitation 2006; 70: 229–237.
- 18. Dyson K, Bray JE, Smith K, et al. Paramedic exposure to out‐of‐hospital cardiac arrest resuscitation is associated with patient survival. Circ Cardiovasc Qual Outcomes 2016; 9: 154–160.
- 19. Barry T, Conroy N, Headon M, et al. The MERIT 3 project: alerting general practitioners to cardiac arrest in the community. Resuscitation 2017; 121: 141–146.
- 20. Anderson R, Sebaldt A, Lin Y, Cheng A. Optimal training frequency for acquisition and retention of high‐quality CPR skills: a randomized trial. Resuscitation 2019; 135: 153–161.
- 21. Hudson L, Jacobs I. Defibrillators: their use in general practice. Aust Fam Physician 2008; 37: 63–64.
- 22. Niegsch ML, Krarup NT, Clausen NE. The presence of resuscitation equipment and influencing factors at General Practitioners’ offices in Denmark: a cross‐sectional study. Resuscitation 2014; 85: 65–69.
- 23. Barry T, Bury G. Advisory external defibrillator availability in general practice. Ir Med J 2015; 108: 212–213.
- 24. Resuscitation Council UK. Quality standards: primary care equipment and drug lists. Updated May 2020. https://www.resus.org.uk/library/quality‐standards‐cpr/primary‐care‐equipment‐and‐drug‐lists (viewed Apr 2020).
- 25. Haskins B, Nehme Z, Cameron P, et al. Coles and Woolworths have installed public access defibrillators in all their stores: it is time other Australian businesses followed their lead. Emerg Med Australas 2020; 32: 166–168.





Abstract
Objective: To compare the frequency and outcomes of cardiac arrests in general practice clinics with those of paramedic‐witnessed cardiac arrests.
Design, setting: Retrospective study; analysis of Victorian Ambulance Cardiac Arrest Registry data, 1 January 2000 – 30 December 2019.
Participants: Patients with non‐traumatic cardiac arrests whom emergency medical services staff attempted to resuscitate.
Main outcome measures: Survival to hospital discharge.
Results: 6363 cases of cardiac arrest were identified: 216 in general practice clinics (3.4%) and 6147 witnessed by paramedics (96.6%). The proportion of patients presenting with initial shockable rhythms was larger in clinic (126 patients, 58.3%) than paramedic‐witnessed cases (1929, 31.4%). The proportion of general practice clinic cases in which defibrillation was provided in the clinic increased from 2 of 37 in 2000–2003 (5%) to 19 of 57 patients in 2016–2019 (33%); survival increased from 7 of 37 (19%) to 23 of 57 patients (40%). For patients with initial shockable rhythms, 57 of 126 in clinic cases (45%) and 1221 of 1929 people in paramedic‐witnessed cases (63.3%) survived to hospital discharge; of 47 general practice patients defibrillated by clinic staff, 27 survived (57%). For patients with initial shockable rhythms, the odds of survival were greater following paramedic‐witnessed events (adjusted odds ratio [aOR], 3.39; 95% CI, 2.08–5.54) or general clinic arrests with defibrillation by clinic staff (aOR, 2.23; 95% CI, 1.03–4.83) than for general practice clinic arrests in which arriving paramedics provided defibrillation.
Conclusion: Emergency medical services should be alerted as soon as possible after people experience heart attack warning symptoms. Automated external defibrillators should be standard equipment in general practice clinics, enabling prompt defibrillation, which may substantially reduce the risk of death for people in cardiac arrest.