We must consider how we can support communities hosting vaccine efficacy trials
Since the beginning of the coronavirus disease 2019 (COVID‐19) pandemic, Australia has pursued a strategy of “aggressive suppression”,1 or the attempt to maintain the number of incident infections as low as possible through diagnostic testing, contact tracing, quarantine, and societal shutdowns. This choice places Australia among a small group of wealthy island communities (notably, New Zealand, Hong Kong, Singapore and Taiwan) attempting to avoid the consequences of the large waves of infection seen in other parts of the world. As a strategy, epidemic suppression is not itself a complete solution to COVID‐19, but instead an epidemiological gambit, employed while waiting for the development of a safe and effective vaccine.2
At the time of writing (August 2020), none of the more than 100 severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) vaccines under development3 have demonstrated efficacy against SARS‐CoV‐2 infection in humans. Seven registered phase 3 field trials of four candidate vaccines are currently recruiting participants in the United States, the United Kingdom, Brazil, Indonesia, Bahrain, the United Arab Emirates and South Africa.4 The only mechanism by which these trials can demonstrate the efficacy of a vaccine in the prevention or modification of COVID‐19 is through the infection of trial participants and members of their surrounding communities. Wealthy countries successfully suppressing COVID‐19 are therefore reliant on infections and morbidity occurring elsewhere to deliver an effective vaccine. The risks and obligations of this strategy must be carefully considered.
Where and when can vaccine trials be conducted for epidemic diseases?
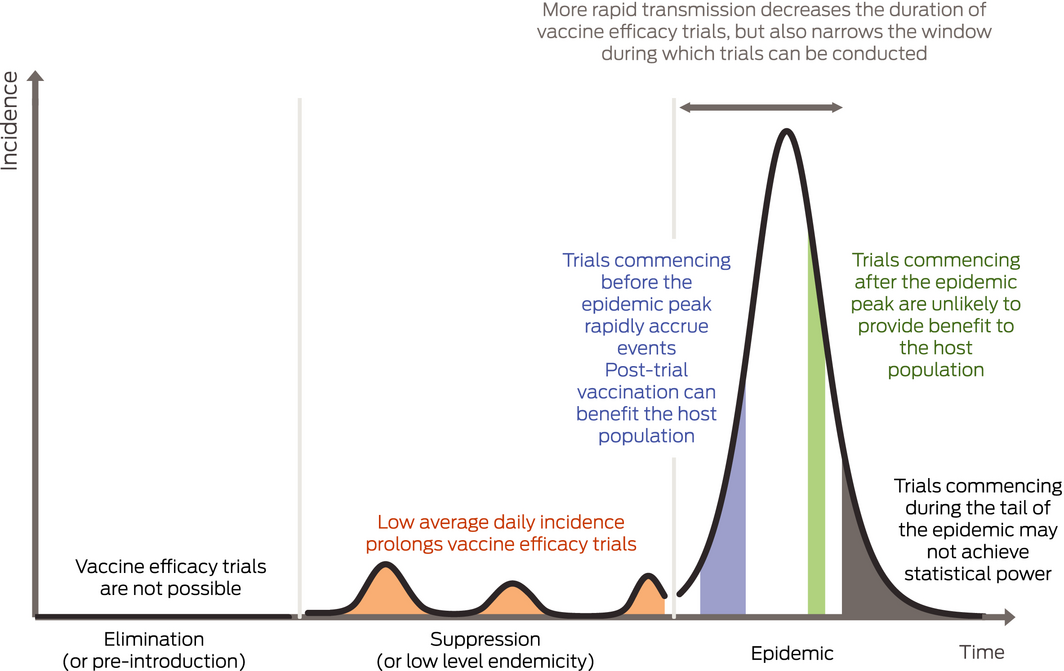
Unlike trials of therapies for non‐communicable diseases or vaccines against endemic diseases, the event rate (here the incidence of SARS‐CoV‐2 infection) in trials conducted during epidemics is unstable, subject to public health policy, and difficult to predict. Box 1 provides an illustration of the consequences of various public health strategies and the timing of trial commencement relative to the time of peak epidemic transmission. In brief, vaccine trials only accrue events during periods of active transmission, which can be slowed or stopped by either transmission control measures or the depletion of susceptible members of the population. Aggressive epidemic suppression may render local vaccine efficacy trials infeasible due to low average daily incidence. In contrast, rapid epidemics offer the opportunity for rapid demonstration of vaccine efficacy but delays to trial commencement can result in trial failure due to declining incidence of infection. Delays also erode the benefit of an effective vaccine for the population hosting a vaccine trial due to the accumulated prevalence of (initial) infection.
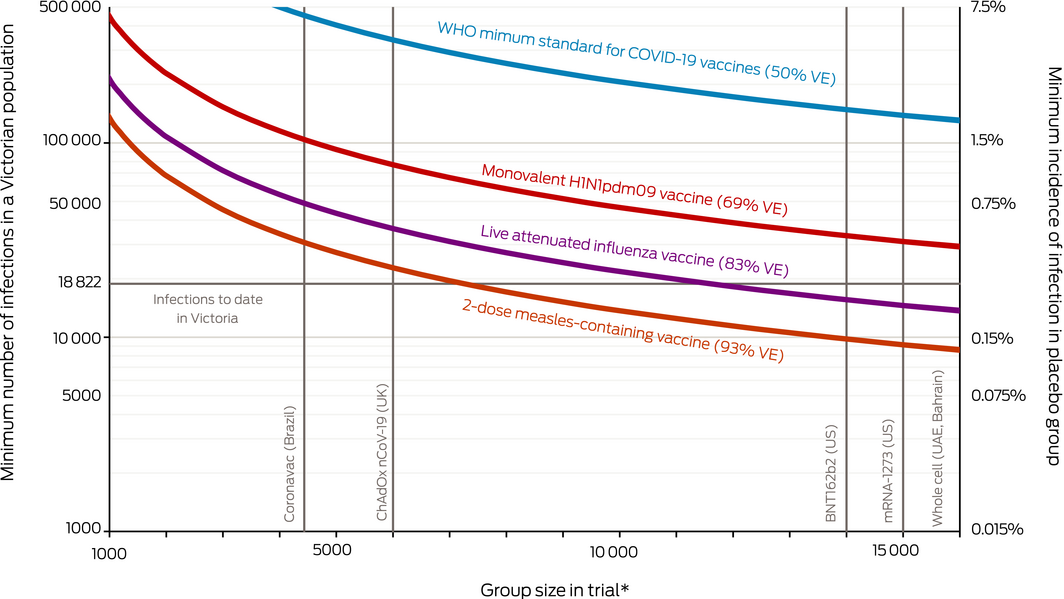
How many people must be infected for a vaccine trial?
Due to the large effect sizes seen in vaccine trials, the required number of infections occurring among trial participants for the demonstration of efficacy is relatively small. Larger trials require lower incidence of infection. However, where a vaccine trial enrols a random sample of an epidemiologically contiguous population, the incidence of infection in the general population will match the required incidence among the trial participants (Supporting Information). Box 2 presents the minimum number of infections required in a population the size of the Australian state of Victoria5 to achieve 90% statistical power with an α error of 5% and a minimum desirable vaccine efficacy of 30%.6 Curves in the figure present estimates relating to the vaccine efficacy of three established vaccines7,8 and also the World Health Organization minimum standard for a SARS‐CoV‐2 vaccine.9
Demonstration of the efficacy of an inactivated or component SARS‐CoV‐2 vaccine in a Victorian‐sized population is likely to require at least as many infections during the trial period as have occurred to date in Victoria (18 822 at the time of writing),10 unless the trial were substantially larger than any currently recruiting. Moreover, trials conducted in larger communities would be accompanied by a correspondingly larger number of infections because the number of population infections is a function of the proportional incidence in the trial.
These estimates represent the minimum number of infections, as incomplete event ascertainment (ie, insensitive or missed diagnostic testing of trial participants), losses to follow‐up, and delays to data availability or analysis (during which infections continue to accumulate) will all serve to increase the number of infections occurring in the population before the completion of the trial. These inefficiencies result in a much larger number of these infections occurring before trial reporting in settings with rapid disease transmission or large numbers of infectious individuals due to the momentum of the epidemic. The restriction of trial enrolment to health care workers or other groups whose incidence of infection exceeds that of the population may serve to reduce the required contemporaneous population infections but would require recruiting thousands of participants within these groups. Moreover, as health care settings become better equipped and organised to minimise transmission, vaccine efficacy trials with health care workers become less feasible. Trials conducted in quarantined subpopulations with more rapid epidemic growth (eg, workers dormitories in Singapore) might be considered ethically problematic, although such strategies are analogous to the general reliance of low incidence populations on vaccines developed in high incidence populations.
Relying on other populations for vaccine development
A public health strategy that aims to prevent local infections while waiting for an efficacious vaccine is inescapably reliant on infectious morbidity and mortality occurring in other populations. From a narrow perspective, this strategy could be seen as ideal in that it minimises the local consequence of disease before a vaccine becomes available. However, this isolationist strategy also involves risks: trial failures may lead to long vaccine development delays (and extension of suppressive measures and border closures), vaccine manufacturers may prioritise distribution to countries involved in trials, and the global public may object to the perceived exploitation of already burdened populations by isolationist holdouts.
For obvious reasons, all registered phase 3 vaccine trials actively recruiting at the time of writing are being conducted in countries with substantial ongoing disease transmission. If experimental vaccines prove efficacious, participation in these trials may be beneficial to at least some trial participants. Even so, the conduct of trials in these locations can be seen as exploitative on a global level, as the burdens of research are confined to populations hosting the trials yet the benefits of an effective vaccine will largely flow elsewhere, particularly to countries successfully maintaining suppression, such as Australia. Moreover, if higher levels of herd immunity are reached in countries after large epidemics during which trials are conducted, little to no post‐trial benefit from host community vaccination will remain.11
Finally, should the first round of overseas vaccine trials fail (due to lack of efficacy, safety concerns, or insufficient infections in trial participants) while the COVID‐19 pandemic continues to evolve, Australia risks being left marooned with a highly susceptible population behind closed borders. In the worst‐case scenario, a rapid decline in infection rates elsewhere may leave few locations able to successfully conduct vaccine efficacy trials (as was seen with trials for the Zika virus vaccine late in the 2015–2016 epidemic)12 and be associated with declining global motivation to make the attempt. In such a situation, Australia would have little choice but to swallow the sunk economic and social costs of a suppression strategy and accept the necessary infectious morbidity associated with local vaccine efficacy testing.
An important alternative strategy is the use of human challenge studies, in which volunteers would be infected with SARS‐CoV‐2 after being given experimental vaccines.13 These studies remain controversial and Australia has not yet developed facilities with relevant experience in respiratory viral challenge. Controlled infection of quarantined participants means that challenge studies can be conducted during tight suppression without causing infections in the surrounding community and can be conducted with a small number of participants (eg, 74 total participants for a vaccine with 69% vaccine efficacy assuming 90% successful inoculation). As demonstrating vaccine efficacy requires someone to be infected somewhere, it is arguable that challenge studies should not be viewed as an option of last resort, but instead as an option available to nations with candidate vaccines but few active infections.
Conclusions
Demonstrating efficacy of a COVID‐19 vaccine requires trial participants and members of their surrounding community to acquire infection in numbers currently deemed unacceptable in countries opting for epidemic suppression. Unless a change in strategy occurs, these countries will remain dependent on trials being performed in other populations whose potential benefit from vaccination is progressively diminishing. The unpredictability of trial outcomes and the progress of the pandemic elsewhere mean that this strategy is not only potentially exploitative but also uncertain.
Island nations relying on other communities to resolve this emergent occasion should acknowledge that every COVID‐19 death diminishes us, and reflect on the obligations owed to, and not just by,14 populations in which vaccine trials are being conducted. Recent additional contributions to the Coalition for Epidemic Preparedness Innovation15 are a welcome start, but we must also consider how we can support communities hosting vaccine efficacy trials, and what we are prepared to contribute to the search for an effective vaccine.
Box 1 – The consequence of the incidence of infection during an epidemic on the duration of vaccine efficacy trials. Equal shaded areas represent the number of population infections required for the demonstration of vaccine efficacy for trials commencing during suppression, before peak transmission, and after peak transmission
Provenance: Not commissioned; externally peer reviewed.
- 1. Coatsworth N. Eliminating COVID‐19 is a false hope [media release]. 16 July 2020. Canberra: Australian Government, Department of Health; 2020. https://www.health.gov.au/news/eliminating-covid-19-a-false-hope (viewed Aug 2020).
- 2. Australian Health Protection Principal Committee. Australian Health Protection Principal Committee (AHPPC) statement on strategic direction [media release]. 24 July 2020. Canberra: Australian Government, Department of Health; 2020. https://www.health.gov.au/news/australian-health-protection-principal-committee-ahppc-statement-on-strategic-direction (viewed Aug 2020).
- 3. Le Than T, Andreadakis Z, Kumar A, et al. The COVID‐19 vaccine development landscape. Nat Rev Drug Discov 2020; 19: 305–306.
- 4. ClinicalTrials.gov. CODIV‐19: phase 2 and 3 vaccine trials. US National Library of Medicine; 2020. https://clinicaltrials.gov/ct2/results?term=vaccine&cond=covid&recrs=a&age_v=&gndr=&type=Intr&rslt=&phase=1&phase=2&Search=Apply (viewed Aug 2020).
- 5. Australian Bureau of Statistics. Australian demographic statistics [ABS Cat. No. 3101.0]; Sept 2019 (updated 19 Mar 2020). Canberra: ABS; 2020. https://www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 (viewed Aug 2020).
- 6. World Health Organization. An international randomised trial of candidate vaccines against COVID‐19. WHO, 2020. https://www.who.int/publications/i/item/an-international-randomised-trial-of-candidate-vaccines-against-covid-19 (viewed Aug 2020).
- 7. Hughes SL, Bolotin S, Khan S, et al. The effect of time since measles vaccination and age at first dose on measles vaccine effectiveness. A systematic review. Vaccine 2020; 38: 460–469.
- 8. Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta‐analysis. Lancet Inf Dis 2012; 12: 36–44.
- 9. Krause P, Fleming TR, Longini I, et al. COVID‐19 vaccine trials should seek worthwhile efficacy. Lancet 2020; 396: 741–743.
- 10. Department of Health and Human Services. Coronavirus (COVID‐19) daily update 2020. Melbourne: DHHS, State Government of Victoria; 2020. https://www.dhhs.vic.gov.au/coronavirus-covid-19-daily-update (viewed Aug 2020).
- 11. Larson RC, Teytelman A. Modeling the effects of H1N1 influenza vaccine distribution in the United States. Value Health 2012; 15: 158–166.
- 12. Vannice KS, Cassetti MC, Eisinger RW, et al. Demonstrating vaccine effectiveness during a waning epidemic: A WHO/NIH meeting report on approaches to development and licensure of Zika vaccine candidates. Vaccine 2019; 37: 863–868.
- 13. Jamrozik E, Selgelid MJ. COVID‐19 human challenge studies: ethical issues. Lancet Infect Dis 2020; 20: e198–e203.
- 14. Morrison S. Press conference, Australian Parliament House [media release]. 24 July 2020. Department of the Prime Minister and Cabinet, 2020. https://www.pm.gov.au/media/press-conference-australian-parliament-house-act-24jul20 (viewed Aug 2020).
- 15. Indo‐Pacific Centre for Health Security. CEPI and FindDx to receive additional Australian funding. IPCHS, 2020. https://indopacifichealthsecurity.dfat.gov.au/cepi-and-finddx-receive-additional-australian-funding (viewed Aug 2020).





No relevant disclosures.