The known: Incivility, bullying, and harassment in hospitals has a negative impact on teamwork, staff wellbeing, and patient safety.
The new: Of 5178 survey respondents, 2009 (38.8%) had frequently (weekly or more) experienced incivility or bullying from co‐workers during the past year, and 753 (14.5%) had experienced extreme unprofessional behaviour (including assault). Nurses and younger staff experienced unprofessional behaviour more frequently, and employees with self‐identified speaking‐up skills less often. Staff perceptions of organisational culture and management influenced the likelihood of reporting unprofessional behaviour.
The implications: The frequency of unprofessional behaviour places patient safety and staff wellbeing at risk. Effective organisation‐wide interventions are required.
Unprofessional behaviour among hospital workers, ranging from incivility and bullying to violence, is frequent,1,2 and it affects care delivery and patient safety. In a United States study (including 13 653 patients and 202 surgeons), rates of medical and surgical complications for individual surgeons were significantly associated with the number of reports by co‐workers of their unprofessional behaviour.3
Unprofessional behaviour often draws attention, but the insidious effects of incivility on safety are becoming clearer.4 Simulation studies have found that even mild incivility causes significant declines in clinical team functioning and care outcomes.5,6 A multicentre study found that incivility during a simulated operating theatre crisis was associated with significantly poorer clinical performance by resident anaesthetists.7
Major health care inquiries have found that hospital cultures in which unprofessional behaviour is tolerated contribute to breaches in safety practices and poor patient outcomes.8 “Speaking up” programs are designed to counter such cultures by supporting open communication by staff about both immediate problems for patient safety (eg, poor hand hygiene among staff) and unprofessional behaviour (eg, incivility, bullying) that compromise teamwork and safe care delivery. The importance of providing employees with skills in speaking up (ie, effectively and assertively communicating views and ideas) is critical to ensuring patient safety and staff wellbeing.9
Health systems around the world have invested in programs that encourage staff to speak up. For example, the National Guardian Freedom to Speak‐up Office, established following the Francis inquiry into the Stafford Hospital scandal in the United Kingdom,8 has developed speaking‐up training and appointed more than 800 guardians across the National Health Service. Guardians received more than 1000 reports per month during 2019 — more than one‐third included elements of bullying and harassment10 — illustrating that patient safety concerns are often linked with unprofessional behaviour. Despite investments in speaking‐up programs, including by Australian hospitals, their effectiveness in reducing rates of unprofessional behaviour or improving safety has not been investigated.
Evidence for the effectiveness of organisational interventions for reducing unprofessional behaviour is limited.11 Effective interventions depend upon detailed understanding of the nature and impact of such behaviour and of factors that place particular groups at risk. While rates of unprofessional behaviour in hospitals have been assessed in surveys,12,13,14 its nature and extent has not been examined at a level that permits better targeting of interventions. surveys have seldom investigated the full spectrum of unprofessional behaviour, included all clinical and non‐clinical hospital staff, or asked staff about their speaking‐up skills. No study has examined the association between self‐assessed speaking‐up skills and experiencing unprofessional behaviour.
We therefore undertook a survey in seven Australian hospitals with the aim of identifying individual and organisational factors associated with the prevalence, types, and impact of unprofessional behaviour among hospital staff.
Methods
Participants
All clinical and non‐clinical staff in seven metropolitan tertiary hospitals operated by the same health care provider — three in Sydney, two in Melbourne, two in Brisbane — were invited to complete an anonymous survey; the survey was open for each hospital for two‐week windows during 4 December 2017 – 30 November 2018. An initial recruitment email and two follow‐up emails were sent over two weeks. The investigators attended wards, departments, and common areas each day (including on weekends and during night shifts) to distribute promotional material about the survey, answer questions from staff, and provide tablet devices for staff to complete the survey. Participants received chocolates and entry in a $50 daily gift card draw for their participation.
Procedures
The online version of the survey was created on the Qualtrics platform; a paper version was supplied when requested. It included questions about 26 unprofessional behaviours, ranging from incivility (eg, being spoken to rudely) to physical and sexual assault. We incorporated questions from the Negative Acts Questionnaire Revised (NAQ‐R)15 and the Royal Australasian College of Surgeons Discrimination, Bullying and Sexual Harassment Prevalence Survey.14 The survey asked participants to rate the frequency of experiencing the 26 unprofessional staff behaviours during the preceding 12 months (7‐point scale, from “never” to “multiple times daily”) and any negative impact on their personal wellbeing, teamwork, and quality of care (5‐point scale: no, minor, moderate, or major impact, and not sure). We also included questions about speaking‐up skills, managing unprofessional behaviour, job classification, and age and sex. The survey separately asked about observing (ie, not directly experiencing) unprofessional behaviour; the responses to this question are not reported in this article (online Supporting Information, part 1). The survey was piloted in a convenience sample of health professionals and tested for face validity prior to the study.
We classified five of the 26 behaviours as extreme behaviours (physical assault, threats of violence, inappropriate or unwanted touching, demands for sexual favours, sexual assault); for the purposes of our analysis, we classified their frequency as “ever” or “never” during the preceding 12 months. The remaining 21 items were categorised as incivility/bullying; for the purposes of our analysis, we classified their frequency as “never”, “occasionally” (at least one behaviour one or two times a year to monthly), or “frequent” (at least one behaviour a week).
Statistical analysis
Survey responses are summarised as descriptive statistics; 95% confidence intervals (CIs) for proportions were estimated as exact (Clopper–Pearson) intervals, assuming a binomial distribution. Associations of seven dichotomous outcomes with demographic characteristics, hospital, and responses to questionnaire items were assessed by multivariable logistic regression:
- experience of incivility/bullying behaviour (frequent v never/occasional);
- experience of extreme behaviour in the past year (ever v never);
- negative impact of unprofessional behaviour on wellbeing, on teamwork, and on patient care, frequency of errors/mistakes, or quality of service (moderate/major v minor/no impact);
- being comfortable with speaking up about or reporting unprofessional behaviour, and having the skills to speak up if experiencing unprofessional behaviour (strongly agree or agree v neither disagree or agree, disagree or strongly disagree).
Potential confounders, including age, sex, employment group, and hospital, were selected a priori for inclusion as factors suspected to be associated with both the primary exposure and outcome in models. Hospital G was selected as the hospital reference group because its staff members reported the lowest rates of experiencing unprofessional behaviour. All analyses were conducted in SAS 9.4.
Ethics approval
The Human Research Ethics Committee of St Vincent's Hospital Melbourne approved the multisite study (reference, HREC/17/SVHM/237).
Results
Prevalence and types of unprofessional behaviour reported by respondents
Of an estimated 15 213 staff members at the seven hospitals, 5178 submitted valid surveys (more than 60% of questions answered) (response rate, 34.0%; 95% CI, 33.3–34.8%) (Supporting Information, part 2), of whom 4846 respondents (93.6%; 95% CI, 92.9–94.2%) reported experiencing at least one unprofessional behaviour during the preceding 12 months. The behaviours most frequently experienced (at least weekly) were having opinions ignored (967 respondents, 18.9%; 95% CI, 17.9–20.0%) and being spoken to rudely (963, 18.8%; 95% CI, 17.7–19.9%) (Supporting Information, part 3).
Incivility or bullying were reported by 4631 respondents (89.4%; 95% CI, 88.6–90.3%) during the past year; 2009 respondents (38.8%; 95% CI, 37.5–40.1%) reported experiencing them at least weekly. Extreme unprofessional behaviour was reported by 753 respondents (14.5%; 95% CI, 13.6–15.5%) (Box 1).
Hospital staff who most frequently reported experiencing unprofessional behaviour
Staff members aged 25–34 years reported frequent incivility or bullying more often than people in other age groups and nurses and non‐clinical workers more often than people in other work classifications; the odds for men and women were similar (Box 2). Frequent incivility or bullying was reported less often by respondents who reported speaking‐up skills (odds ratio [OR], 0.53; 95% CI, 0.46–0.61).
Staff members aged 25–34 years reported extreme unprofessional behaviour more often than people in other age groups, and nurses reported it more often than doctors (OR, 2.06; 95% CI, 1.52–2.81); men reported it more often than women (OR, 1.26; 95% CI, 1.03–1.56) (Box 3). Extreme behaviour was reported less often by respondents who reported speaking‐up skills (OR, 0.80; 95% CI, 0.67–0.97).
Impact of unprofessional behaviour on personal wellbeing
A total of 1989 respondents (38.4%; 95% CI, 37.1–39.8%) reported that unprofessional behaviour had a moderate or major impact on their wellbeing. Staff members aged 18–24 years reported this impact less often than people in other age groups, men less often than women (OR, 0.68; 95% CI, 0.58–0.81), and medical staff less often than other staff groups (Box 4). A moderate or major negative impact was less often reported by respondents who reported speaking‐up skills (OR, 0.44; 95% CI, 0.38–0.51).
Staff members reporting frequent (OR, 8.39; 95% CI, 5.73–12.3) or occasional incivility or bullying from co‐workers (OR, 2.20; 95% CI, 1.51–3.22) more frequently reported a moderate or major impact on their wellbeing than those who never experienced them (Box 4).
Impact of unprofessional behaviours on teamwork and quality of care
A total of 2832 respondents (54.7%; 95% CI, 53.5–56.1%) reported that unprofessional behaviour in their hospital had a moderate or major negative impact on teamwork. Nurses and management and administrative staff reported this impact more often than medical staff. Staff members who reported frequent incivility or bullying reported a moderate or major impact on teamwork more frequently than those who had not (OR, 10.0; 95% CI, 7.25–13.8) (Box 5, A). A moderate or major impact on teamwork was less often reported by respondents who reported speaking‐up skills (OR, 0.56; 95% CI, 0.48–0.66).
A total of 2580 respondents (49.8%; 95% CI, 48.5–51.2%) reported that unprofessional behaviour had a moderate or major negative impact on patient care, frequency of errors, or quality of service. Nurses, non‐clinical staff, and management and administrative staff reported this impact more often than medical staff. Staff members who reported experiencing unprofessional behaviour (incivility or extreme behaviour) reported an impact on these quality indicators more often than those who had not (Box 5, B). A moderate or major impact on care quality was less often reported by respondents who reported speaking‐up skills (OR, 0.58; 95% CI, 0.50–0.68).
Comfort with speaking up or reporting unprofessional behaviour
Six factors each influenced the comfort of respondents about speaking up or reporting unprofessional behaviour, including self‐reported skills in speaking up (OR, 4.25; 95% CI, 3.50–5.16), confidence that they would be believed and taken seriously (OR, 3.05; 95% CI, 2.60–3.59), and perception that their hospital effectively managed complaints about unprofessional behaviour (OR, 1.98; 95% CI, 1.66–2.35) (Box 6).
Staff members aged 25–34 years reported less often than other age groups that they were comfortable with speaking up, while non‐clinical and management and administrative staff more often reported that they were comfortable doing so, as did men (v women: OR, 1.23; 95% CI, 1.02–1.48) (Box 6).
Perceived skills in speaking up about unprofessional behaviour
Most respondents (4560, 88.1%; 95% CI, 87.2–88.9%) agreed or strongly agreed that speaking up about unprofessional behaviour was important for patient safety; 3723 respondents (71.9%; 95% CI, 70.7–73.1%) agreed or strongly agreed that “I have the skills to effectively speak up if I experience unprofessional behaviour”.
Older respondents more often reported skills in speaking up than younger staff members; men reported these skills more often than women (OR, 1.26; 95% CI, 1.07–1.50). There were no significant differences between staff groupings (Box 7).
Discussion
A substantial proportion of the surveyed hospital staff regularly experienced unprofessional behaviour, 2009 (39%) reporting daily or more frequent incivility or bullying by co‐workers. A survey of New Zealand medical staff found a similar rate of frequent incivility and bullying (38%).13 Nurses, employees under 35 (more likely to be in relatively junior positions), and staff in non‐clinical positions more frequently reported exposure to such behaviour.
A total of 753 respondents (14.5%) reported experiencing at least one of the five extreme unprofessional behaviours during the preceding 12 months; nurses, people aged 25–34 years, and men reported such behaviour more frequently than other employee groups. An earlier Australian study16 found that the prevalence of physical aggression in a large sample of Australian medical workers was 4.3–13.0%, and that a larger proportion of male hospital non‐specialist doctors experienced physical aggression from co‐workers than their female colleagues (15.1% v 8.9%). It has also been reported that male nurses experience more aggression (from all sources) than female nurses.17
The impact of unprofessional behaviour was considerable: almost 40% of staff members reported moderate or major effects on their wellbeing, particularly if they reported frequent incivility or bullying. Further, 55% of staff reported that such behaviour seriously affected teamwork, consistent with findings from clinical simulation studies5,6,7 that rudeness is associated with significant declines in clinical performance and outcomes.
An important new finding was the strong association between self‐assessed speaking‐up skills and experiencing unprofessional behaviour. Respondents who reported having such skills were 47% less likely to report frequent experience of incivility or bullying and 20% less likely to report extreme unprofessional behaviour from co‐workers than colleagues without these skills. Reporting speaking‐up skills was also strongly associated with lower rates of reporting negative impacts on personal wellbeing, teamwork, and quality indicators.
Exposure to unprofessional behaviour may change a person's perception of their speaking‐up skills. However, health systems in several countries have invested in speaking‐up programs,10 reflecting the expectation that they will reduce the frequency of unprofessional behaviour. That having speaking‐up skills reduces the frequency and impact of unprofessional behaviour, as suggested by our results, is therefore plausible. Younger staff and women were significantly less likely to report speaking‐up skills, suggesting the need for training, support, and skills development.
Our study is the first to suggest that programs for strengthening the ability of hospital workers to identify and speak up about unprofessional behaviour could ameliorate some of its negative impact. The effective elements in these programs need to be identified, as well as factors that support their sustainability and scalability, including the organisational context in which staff are asked to speak up; exhortations to do so often “… belie the complexity and ambiguity that it creates for staff.”18 Individuals must decide when it is safe to speak up, or to stay silent.19
We also found that being comfortable about reporting unprofessional behaviour was significantly associated with staff perceptions of the organisational culture, the effectiveness of their hospital in managing complaints about unprofessional behaviour, and the likely consequences of reporting; staff who believed they would be taken seriously were three times more likely to report bad behaviour. Further, clinical culture is often not conducive to identifying and reporting poor behaviour,9,20,21 and clinicians were the employee group least likely to feel comfortable about reporting unprofessional behaviour in our study.
Just providing staff with the skills and knowledge to speak up is consequently insufficient for reducing the incidence and impact of unprofessional behaviour in organisations perceived to have poor management processes and with limited supervisory support for managing behaviour. Speaking up requires a psychologically safe environment; this requires that giving and receiving feedback is regarded as normal, and that teams are cohesive and authority gradients minimal.18
Training hospital leaders in how to engage with colleagues to counter disruptive and unprofessional behaviour is critical,9 including being receptive when staff speak up, and having both the skills and processes for an effective response.18 While the central role of senior hospital management and professional leaders in ensuring low tolerance for unprofessional behaviour is recognised,22 there are few effective interventions for achieving such environments.
Organisational culture can normalise incivility. As reported for other workplaces,23 we found that hospitals with higher rates of incivility and bullying also had higher rates of extreme behaviour. Tolerance for low level poor behaviour can be an enabler for more serious misbehaviour. Besides interventions that target individuals, organisation‐wide programs that demonstrate strong commitment to identifying and responding to unprofessional behaviour are required, including respectful behaviour by senior staff members and prompt intervention when required.24 Ensuring that such programs are rigorously evaluated for their effectiveness is equally important.2,9
Limitations
One strength of our study was that, beyond descriptive analyses, we controlled for a range of potential confounding factors. However, responder bias was possible in our survey. People who had experienced unprofessional behaviour may have been more likely to complete the survey or, conversely, have preferred to not draw attention to their experiences by completing the survey. A review of factors that influence participation rates in health‐related surveys and their likely effects on outcomes concluded that evidence for substantial bias caused by non‐participation was limited.25 In our model analyses, data for 8–12% of respondents were missing, and this may have affected our estimates. As the hospitals were run by a single operator, our findings may not be generalisable to hospitals outside this group. Finally, the cross‐sectional design means that findings should be interpreted as associations, not as causal links.
Conclusion
Our findings indicate that unprofessional behaviour is highly prevalent among hospital workers. They clearly indicate that providing staff, regardless of their age, sex, and professional group, with skills in speaking up about unprofessional behaviour and an organisational environment that effectively deals with it, may reduce the frequency of unprofessional behaviour and reduce its negative impacts on staff and patients.
Box 1 – Experience of unprofessional behaviour by 5178 survey respondents during the preceding 12 months, by respondent characteristic
|
Variable |
Number |
Incivility or bullying |
Extreme unprofessional behaviour |
||||||||||||
|
Frequent* |
Occasional† |
Never |
Missing data‡ |
Ever |
Never |
Missing data‡ |
|||||||||
|
|
|||||||||||||||
|
Number of respondents |
|
2009 |
2622 |
317 |
230 |
753 |
4376 |
49 |
|||||||
|
Age (years) |
|
|
|
|
|
|
|
|
|||||||
|
18–24 |
300 |
110 (36.7%) |
165 (55.0%) |
20 (6.7%) |
5 (2%) |
45 (15%) |
255 (85.0%) |
0 |
|||||||
|
25–34 |
1567 |
692 (44.2%) |
754 (48.1%) |
73 (4.7%) |
48 (3.1%) |
282 (18.0%) |
1274 (81.3%) |
11 (0.7%) |
|||||||
|
35–44 |
1127 |
421 (37.4%) |
586 (52.0%) |
65 (5.8%) |
55 (4.9%) |
152 (13.5%) |
965 (85.6%) |
10 (0.9%) |
|||||||
|
45–54 |
1097 |
414 (37.7%) |
574 (52.3%) |
63 (5.7%) |
46 (4.2%) |
151 (13.8%) |
931 (84.9%) |
15 (1.4%) |
|||||||
|
≥ 55 |
983 |
321 (32.7%) |
504 (51.3%) |
91 (9.3%) |
67 (6.8%) |
102 (10.4%) |
869 (88.4%) |
12 (1.2%) |
|||||||
|
Missing data‡ |
104 |
51 (49%) |
39 (38%) |
5 (5%) |
9 (9%) |
21 (20%) |
82 (79%) |
1 (1%) |
|||||||
|
Sex |
|
|
|
|
|
|
|
|
|||||||
|
Women |
3909 |
1521 (38.9%) |
2119 (54.2%) |
100 (2.6%) |
169 (4.3%) |
568 (14.5%) |
3307 (84.6%) |
34 (0.9%) |
|||||||
|
Men |
1176 |
434 (36.9%) |
471 (40.1%) |
216 (18.4%) |
55 (4.7%) |
168 (14.3%) |
993 (84.4%) |
15 (1.3%) |
|||||||
|
Missing data‡ |
93 |
54 (58%) |
32 (34%) |
1 (1%) |
6 (6%) |
17 (18%) |
76 (82%) |
0 |
|||||||
|
Role |
|
|
|
|
|
|
|
|
|||||||
|
Nursing |
2248 |
930 (41.4%) |
1156 (51.4%) |
76 (3.4%) |
86 (3.8%) |
443 (19.7%) |
1790 (79.6%) |
15 (0.7%) |
|||||||
|
Medical |
546 |
197 (36.1%) |
276 (50.5%) |
53 (9.7%) |
20 (3.7%) |
62 (11%) |
480 (87.9%) |
4 (0.7%) |
|||||||
|
Allied health/clinical services |
795 |
264 (33.2%) |
456 (57.4%) |
56 (7.0%) |
19 (2.4%) |
73 (9.2%) |
718 (90.3%) |
4 (0.5%) |
|||||||
|
Non‐clinical services |
590 |
233 (39.5%) |
245 (41.5%) |
65 (11%) |
47 (8.0%) |
67 (11%) |
509 (86.3%) |
14 (2.4%) |
|||||||
|
Management/administration |
822 |
301 (36.6%) |
427 (51.9%) |
58 (7.1%) |
36 (4.4%) |
67 (8.2%) |
751 (91.4%) |
4 (0.5%) |
|||||||
|
Missing data‡ |
177 |
84 (48%) |
62 (35%) |
9 (5%) |
22 (12%) |
41 (23%) |
128 (72%) |
8 (4.5%) |
|||||||
|
Hospital |
|
|
|
|
|
|
|
|
|||||||
|
A |
1874 |
680 (36.3%) |
993 (53%) |
109 (5.8%) |
92 (4.9%) |
268 (14.3%) |
1583 (84.5%) |
23 (1.2%) |
|||||||
|
B |
752 |
305 (40.6%) |
357 (47.5%) |
51 (6.8%) |
39 (5.2%) |
114 (15.2%) |
631 (83.9%) |
7 (0.9%) |
|||||||
|
C |
1309 |
586 (44.8%) |
623 (47.6%) |
48 (3.7%) |
52 (4.0%) |
210 (16.0%) |
1089 (83.2%) |
10 (0.8%) |
|||||||
|
D |
300 |
118 (39.3%) |
152 (50.7%) |
18 (6.0%) |
12 (4.0%) |
43 (14%) |
256 (85.3%) |
1 (0.3%) |
|||||||
|
E |
430 |
160 (37.2%) |
205 (47.7%) |
42 (9.8%) |
23 (5.4%) |
71 (16%) |
353 (82.1%) |
6 (1.4%) |
|||||||
|
F |
142 |
48 (34.0%) |
62 (43.7%) |
28 (20%) |
4 (3%) |
19 (13%) |
123 (87%) |
0 |
|||||||
|
G |
371 |
112 (30.2%) |
230 (62.0%) |
21 (5.7%) |
8 (2%) |
28 (7.6%) |
341 (91.9%) |
2 (0.5%) |
|||||||
|
Skills to speak up§ |
|
|
|
|
|
|
|
|
|||||||
|
Agree/strongly agree |
3723 |
1279 (34.4%) |
2040 (54.8%) |
263 (7.1%) |
141 (3.8%) |
500 (13.4%) |
3201 (86.0%) |
22 (0.6%) |
|||||||
|
Neither disagree nor agree/disagree/strongly disagree |
1259 |
631 (50.1%) |
524 (41.6%) |
43 (3.4%) |
61 (4.9%) |
212 (16.8%) |
1028 (81.7%) |
19 (1.5%) |
|||||||
|
Missing data‡ |
196 |
99 (50%) |
58 (30%) |
11 (6%) |
28 (14%) |
41 (21%) |
147 (75%) |
8 (4%) |
|||||||
|
|
|||||||||||||||
|
* Weekly, daily, or several times a day. † Once or twice a year, every few months, or about monthly. ‡ No response or preferred not to answer. § “I have the skills to effectively speak up if I experience unprofessional behaviour”. |
|||||||||||||||
Box 2 – Frequent experience of incivility or bullying during the preceding 12 months, by respondent characteristics and hospital*
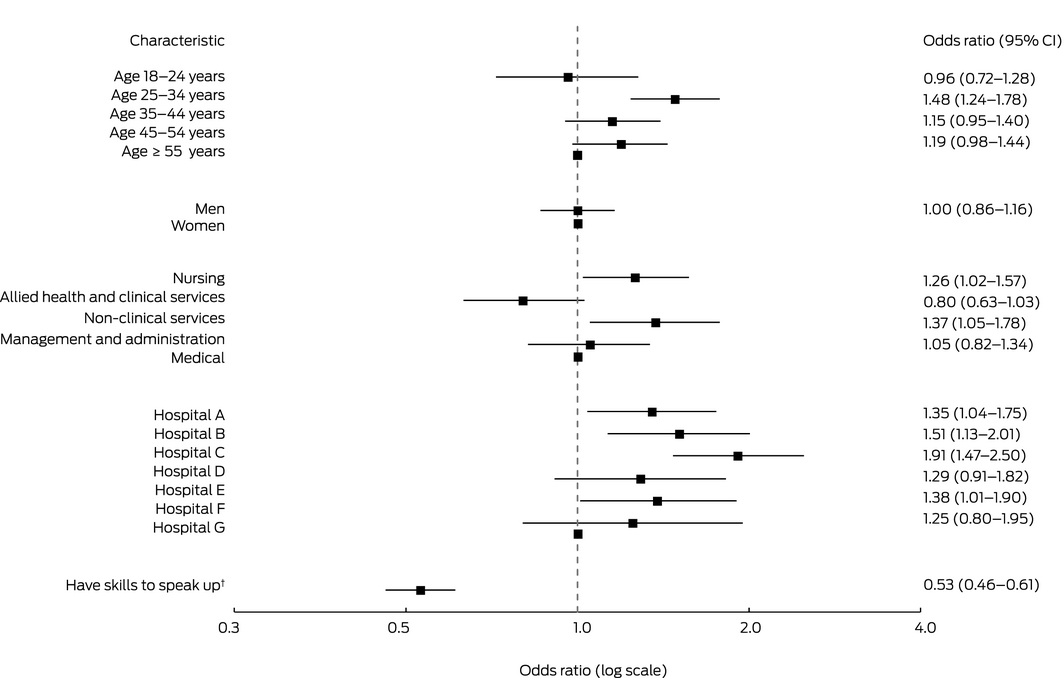
CI = confidence interval. * Data for 4585 respondents who answered all required questions (88.5%). † “I have the skills to effectively speak up if I experience unprofessional behaviour”: (strongly) agree v (strongly) disagree or neither agree nor disagree.
Box 3 – Experience of extreme unprofessional behaviour during the preceding 12 months, by respondent characteristics and hospital*
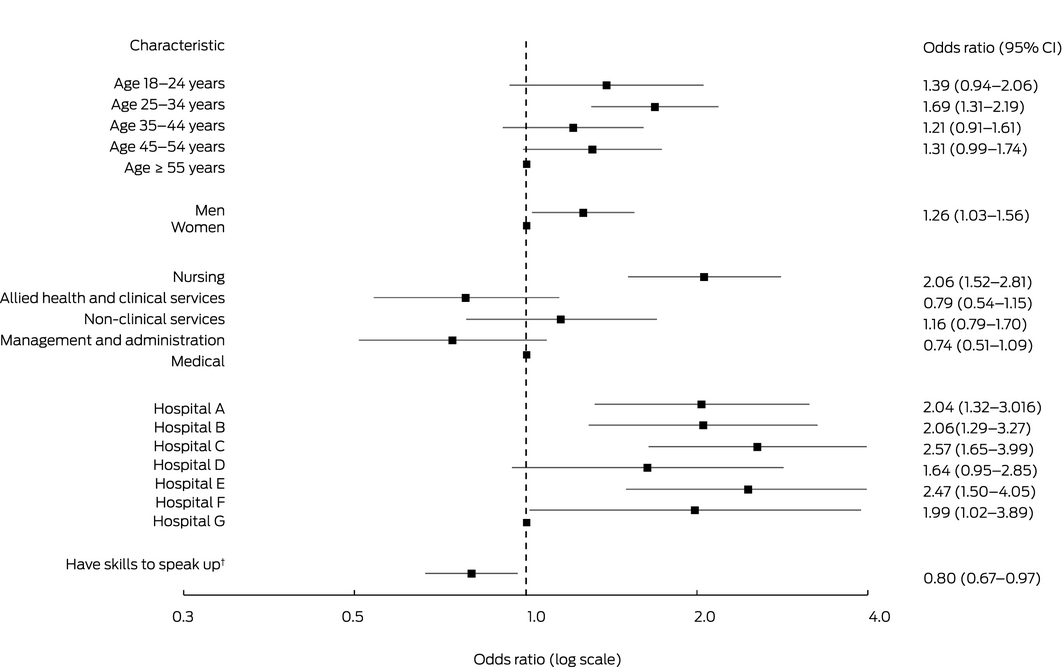
CI = confidence interval. * Data for 4727 respondents who answered all required questions (91.3%). † “I have the skills to effectively speak up if I experience unprofessional behaviour”: (strongly) agree v (strongly) disagree or neither agree nor disagree.
Box 4 – Moderate or major impact of unprofessional behaviour on the respondent or their wellbeing, by respondent characteristics*
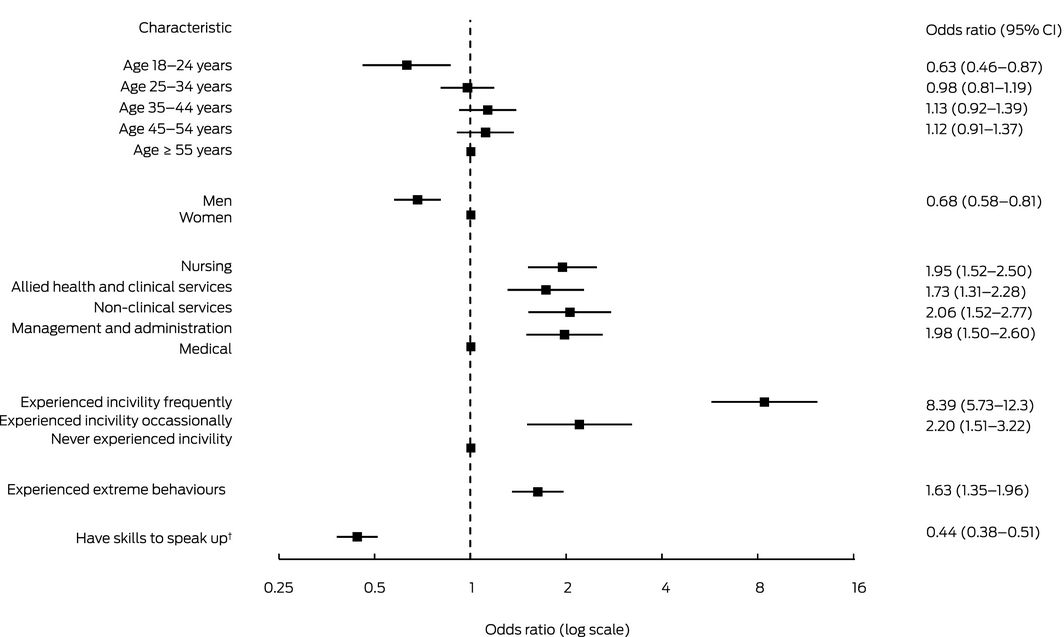
CI = confidence interval. * Data for 4588 respondents who answered all required questions (88.6%). † “I have the skills to effectively speak up if I experience unprofessional behaviour”: (strongly) agree v (strongly) disagree or neither agree nor disagree. Hospital was included as a variable in the model, but is not displayed here for brevity.
Box 5 – Moderate or major impact of unprofessional behaviour on teamwork * or patient care, frequency of errors, or quality of service,† by respondent characteristics
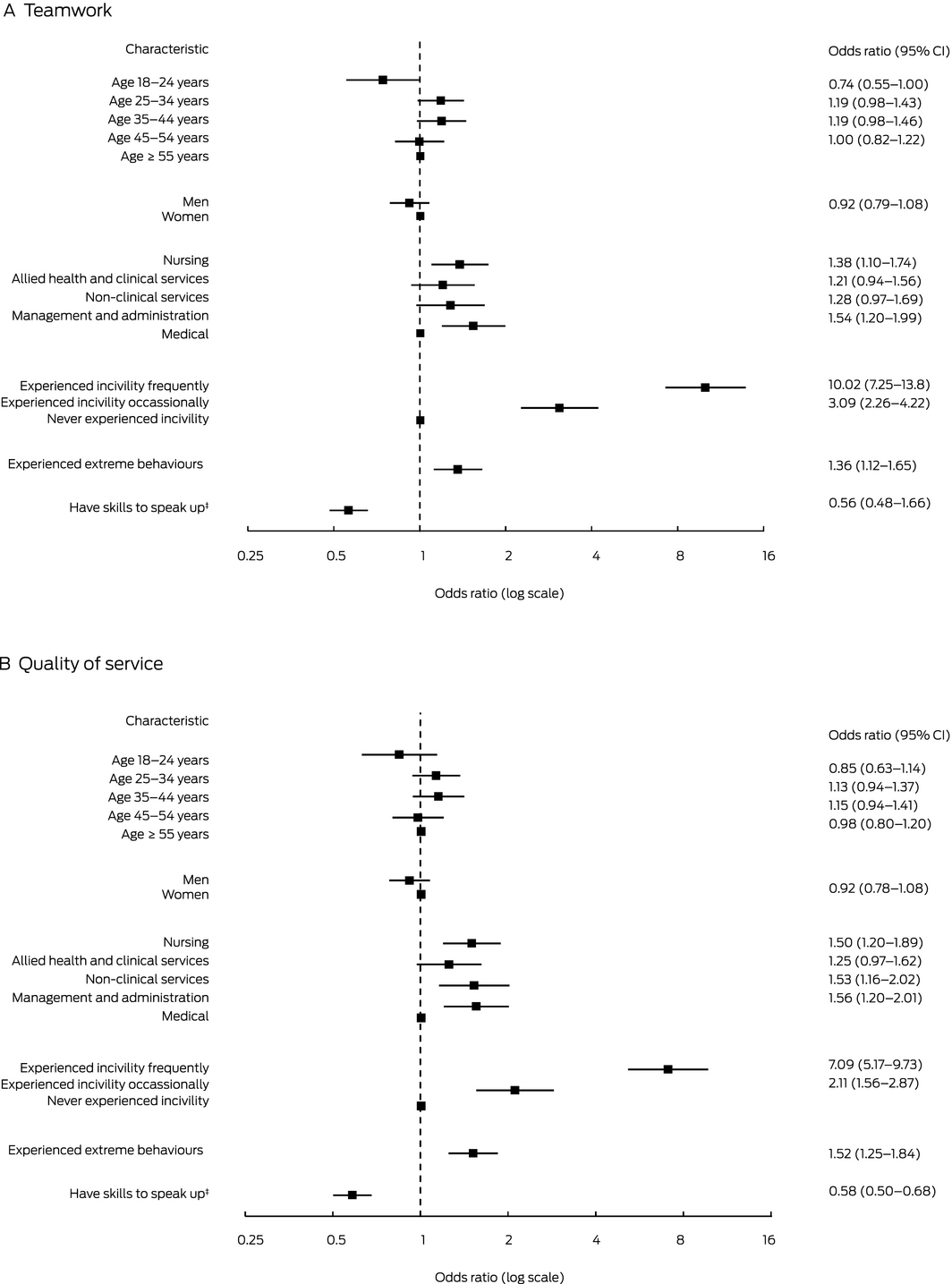
CI = confidence interval. * Data for 4534 respondents who answered all required questions (87.6%). † Data for 4389 respondents who answered all required questions (84.8%). ‡ “I have the skills to effectively speak up if I experience unprofessional behaviour”: (strongly) agree v (strongly) disagree or neither agree nor disagree. Hospital was included as a variable in the model, but is not displayed here for brevity.
Box 6 – Comfort with speaking up or reporting unprofessional behaviour,* by respondent characteristics and hospital†
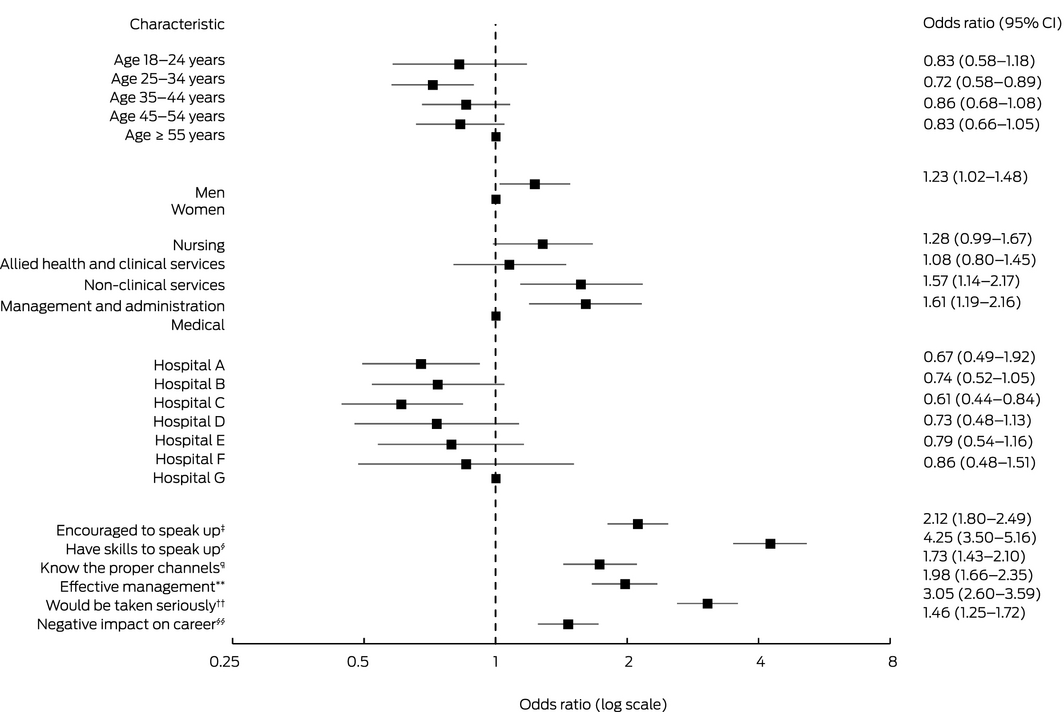
* Agree or strongly agree that “I feel comfortable speaking up or reporting unprofessional behaviour”.
† Data for 4553 respondents who answered all required questions (87.9%).
‡ “I am encouraged by my colleagues to speak up about unprofessional behaviour” (agree or strongly agree).
§ “I have the skills to effectively speak up if I experience unprofessional behaviour” (agree or strongly agree).
¶ “I know the proper channels to raise concerns about unprofessional behaviour” (agree or strongly agree).
** “Unprofessional behaviour is effectively managed in this hospital” (agree or strongly agree).
†† “I am confident I would be believed and taken seriously if I reported unprofessional behaviour” (agree or strongly agree).
§§ “Speaking up or reporting unprofessional behaviour is likely to have a negative impact on my career” (disagree or strongly disagree).
Box 7 – Reporting having the skills to speak up if experiencing unprofessional behaviour,* by respondent characteristic†
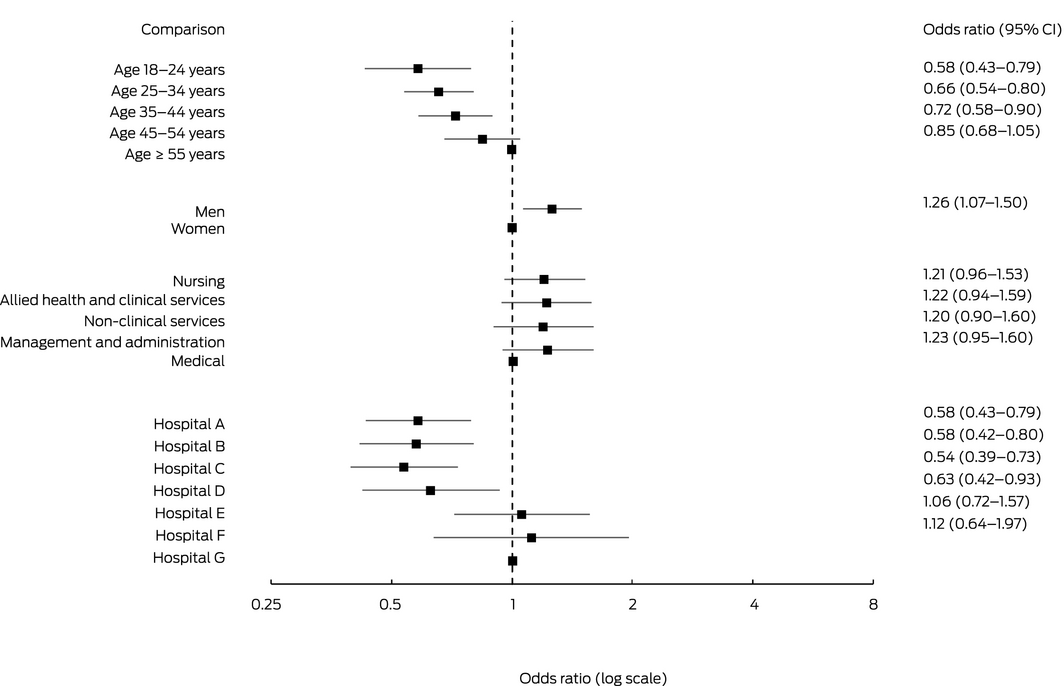
* Agree or strongly agree that “I have the skills to effectively speak up if I experience unprofessional behaviour”.
† Data for 4765 respondents who answered all required questions (92.0%).
Received 16 April 2020, accepted 11 August 2020
- Johanna Westbrook1
- Neroli Sunderland1
- Ling Li1
- Alain Koyama1
- Ryan McMullan1
- Rachel Urwin1
- Kate Churruca1
- Melissa T Baysari2
- Catherine Jones3
- Erwin Loh1,4
- Elizabeth C McInnes
- Sandy Middleton5,6
- Jeffrey Braithwaite1
- 1 Australian Institute of Health Innovation, Sydney, NSW
- 2 The University of Sydney, Sydney, NSW
- 3 St Vincent's Health Australia, Melbourne, VIC
- 4 Monash Centre for Health Research and Implementation, Monash University, Melbourne, VIC
- 5 Nursing Research Institute, Sydney, NSW
- 6 Australian Catholic University, Sydney, NSW
We thank all hospital staff who completed the survey, and particularly the managers who contributed to facilitating the study.
This investigation was supported by a National Health and Medical Research Council Partnership Project Grant (1134459) in partnership with St Vincent's Health Australia.
- 1. Leape LL, Shore MF, Dienstag JL, et al. A culture of respect, part 1. The nature and causes of disrespectful behavior by physicians. Acad Med 2012; 87: 845–852.
- 2. Westbrook J, Sunderland N, Atkinson V, et al. Endemic unprofessional behaviour in health care: the mandate for a change in approach. Med J Aust 2018; 209: 380–381. https://www.mja.com.au/journal/2018/209/9/endemic-unprofessional-behaviour-health-care-mandate-change-approach.
- 3. Cooper WO, Spain DA, Guillamondegui O, et al. Association of coworker reports about unprofessional behavior by surgeons with surgical complications in their patients. JAMA Surg. 2019; 160: 810–817.
- 4. Flin R. Rudeness at work. BMJ 2010; 340: c2480.
- 5. Riskin A, Erez A, Foulk TA, et al. The impact of rudeness on medical team performance: a randomized trial. Pediatrics 2015; 136: 487–495.
- 6. Riskin A, Erez A, Foulk TA, et al. Rudeness and medical team performance. Pediatrics 2017; 139: e20162305.
- 7. Katz D, Blasius K, Isaak R, et al. Exposure to incivility hinders clinical performance in a simulated operative crisis. BMJ Qual Saf 2019; 28: 750–757.
- 8. Francis R. Report of the Mid Staffordshire NHS Foundation Trust public inquiry (House of Commons papers, session 2012/13; HC 947). Feb 2013. https://www.bl.uk/collection-items/report-of-the-mid-staffordshire-nhs-foundation-trust-public-inquiry-executive-summary (viewed July 2020).
- 9. Dixon‐Woods M, Campbell A, Martin G, et al. Improving employee voice about transgressive or disruptive behavior: a case study. Acad Med 2019; 94: 579–585.
- 10. National Guardian Freedom to Speak Up Office. Speaking up in the NHS in England 2018/2019: a summary of speaking up to Freedom to Speak Up Guardians in NHS trusts and foundation trusts. Jan 2020. www.nationalguardian.org.uk/wp-content/uploads/2020/01/speaking_up_data_report_2018-19.pdf (viewed July 2020).
- 11. Gillen PA, Sinclair M, Kernohan WG, et al. Interventions for prevention of bullying in the workplace. Cochrane Database Syst Rev 2017; CD009778.
- 12. Carter M, Thompson N, Crampton P, et al. Workplace bullying in the UK NHS: a questionnaire and interview study on prevalence, impact and barriers to reporting. BMJ Open 2013; 3: e002628.
- 13. Chambers CNL, Frampton CMA, McKee M, et al. “It feels like being trapped in an abusive relationship”: bullying prevalence and consequences in the New Zealand senior medical workforce: a cross‐sectional study. BMJ Open 2018; 8: e020158.
- 14. Crebbin W, Campbell G, Hillis DA, et al. Prevalence of bullying, discrimination and sexual harassment in surgery in Australasia. ANZ J Surg 2015; 85: 905–909.
- 15. Einarsen S, Hoel H, Notelaers G. Measuring exposure to bullying and harassment at work: validity, factor structure and psychometric properties of the Negative Acts Questionnaire‐Revised. Work Stress 2009; 23: 24–44.
- 16. Hills D, Joyce C, JS H. A national study of workplace aggression in Australian clinical medical practice. Med J Aust 2012; 197: 336–340. https://www.mja.com.au/journal/2012/197/6/national-study-workplace-aggression-australian-clinical-medical-practice
- 17. Edward K‐l, Stephenson J, Ousey K, et al. A systematic review and meta‐analysis of factors that relate to aggression perpetrated against nurses by patients/relatives or staff. J Clin Nurs 2016; 25: 289–299.
- 18. Mannion R, Davies H. Raising and responding to frontline concerns in healthcare. BMJ 2019; 366: l4944.
- 19. Schwappach D, Richard A. Speak up‐related climate and its association with healthcare workers’ speaking up and withholding voice behaviours: a cross‐sectional survey in Switzerland. BMJ Qual Saf 2018; 27: 827.
- 20. Aasland OG, Førde R. Impact of feeling responsible for adverse events on doctors’ personal and professional lives: the importance of being open to criticism from colleagues. Qual Saf Hlth Care 2005; 14: 13–17.
- 21. Mannion R, Blenkinsopp J, Powell M, et al. Understanding the knowledge gaps in whistleblowing and speaking up in health care: narrative reviews of the research literature and formal inquiries, a legal analysis and stakeholder interviews. Southampton: NIHR Journals Library, 2018. https://www.ncbi.nlm.nih.gov/books/NBK519615 (viewed July 2020).
- 22. Leape LL, Shore MF, Dienstag JL, et al. A culture of respect, part 2. Creating a culture of respect. Acad Med 2012; 87: 853–858.
- 23. Andersson LM, Pearson CM. Tit for tat? The spiraling effect of incivility in the workplace. Acad Manage Rev 1999; 24: 452–471.
- 24. Gilin Oore D, Leblanc D, Day A, et al. When respect deteriorates: incivility as a moderator of the stressor–strain relationship among hospital workers. J Nurse Manage 2010; 18: 878–888.
- 25. Galea S, Tracy M. Participation rates in epidemiologic studies. Ann Epidemiol 2007; 17: 643–653.





Abstract
Objective: To identify individual and organisational factors associated with the prevalence, type and impact of unprofessional behaviours among hospital employees.
Design, setting, participants: Staff in seven metropolitan tertiary hospitals operated by one health care provider in three states were surveyed (Dec 2017 – Nov 2018) about their experience of unprofessional behaviours — 21 classified as incivility or bullying and five as extreme unprofessional behaviour (eg, sexual or physical assault) — and their perceived impact on personal wellbeing, teamwork and care quality, as well as about their speaking‐up skills.
Main outcome measures: Frequency of experiencing 26 unprofessional behaviours during the preceding 12 months; factors associated with experiencing unprofessional behaviour and its impact, including self‐reported speaking‐up skills.
Results: Valid surveys (more than 60% of questions answered) were submitted by 5178 of an estimated 15 213 staff members (response rate, 34.0%). 4846 respondents (93.6%; 95% CI, 92.9–94.2%) reported experiencing at least one unprofessional behaviour during the preceding year, including 2009 (38.8%; 95% CI, 37.5–40.1%) who reported weekly or more frequent incivility or bullying; 753 (14.5%; 95% CI, 13.6–15.5%) reported extreme unprofessional behaviour. Nurses and non‐clinical staff members aged 25–34 years reported incivility/bullying and extreme behaviour more often than other staff and age groups respectively. Staff with self‐reported speaking‐up skills experienced less incivility/bullying (odds ratio [OR], 0.53; 95% CI, 0.46–0.61) and extreme behaviour (OR, 0.80; 95% CI, 0.67–0.97), and also less frequently an impact on their personal wellbeing (OR, 0.44; 95% CI, 0.38–0.51).
Conclusions: Unprofessional behaviour is common among hospital workers. Tolerance for low level poor behaviour may be an enabler for more serious misbehaviour that endangers staff wellbeing and patient safety. Training staff about speaking up is required, together with organisational processes for effectively eliminating unprofessional behaviour.