Workplace aggression is a worldwide concern that has been linked to impaired physical and mental health.1-4 There is limited international research describing the extent and impact of workplace aggression in medicine, however, and the few Australian studies have primarily focused on general practitioner experiences of patient aggression.5-8 There are no comprehensive data on workplace aggression in Australia, and workplace aggression is considered to be grossly underreported by health workers.9,10 In the absence of comprehensive data, legislators and policymakers have to rely on anecdote, opinion, ideology or poor-quality evidence, where it exists, to inform decision making.11 Currently, the research literature appears to be the most reliable source of data on workplace aggression in Australia.
This exploratory–descriptive study was conducted between March 2010 and June 2011, in the third wave of the Medicine in Australia: Balancing Employment and Life (MABEL) survey. Eight workplace aggression prevalence items were included in questionnaires tailored for GPs and GP registrars, specialists, hospital non-specialists and specialists in training. Questionnaire items were tested in the pilot phase of the survey.12 The sampling frame was the Medical Directory of Australia (MDA), a comprehensive database of 59 144 Australian medical practitioners,13 as accessed in February and May 2010. Of these, 16 327 (27.6%) were surveyed in accordance with the MABEL protocol.14 Invitees comprised contactable respondents from previous waves of the MABEL survey (12 068) and clinical medical practitioners new to or re-entering the MDA by May 2010 (4259). The study was approved by the University of Melbourne Faculty of Economics and Commerce Human Ethics Advisory Group and the Monash University Standing Committee on Ethics in Research Involving Humans.
A range of demographic and other profile data were collected, including doctor type, sex, age, IMG status, and location by state and Australian Standard Geographic Classification of remoteness.15 Years elapsed since medical graduation was also determined. Estimates of the frequency of aggression from patients, patients’ relatives or carers, coworkers and others external to the workplace were elicited with a five-point, ordinal response scale: “Frequently (once or more each week)”, “Often (a few times each month)”, “Occasionally (a few times each 6 months)”, “Infrequently (a few times in 12 months)” and “Not at all”. Workplace aggression was defined in survey questionnaires as:
A response rate of 60.9% (9951) was achieved, with 57.9% (9449) of invitees indicating that they worked in clinical practice in Australia. Comparisons of the study sample and national profiles are shown in Box 1 (doctor type, State and rurality) and Box 2 (sex and mean age, by doctor type). While statistically significant (P < 0.001), except for mean age for male hospital non-specialists, the differences between the sample and the national profiles suggest only a slight bias toward specialist, Victorian, non-metropolitan, female and younger clinicians.
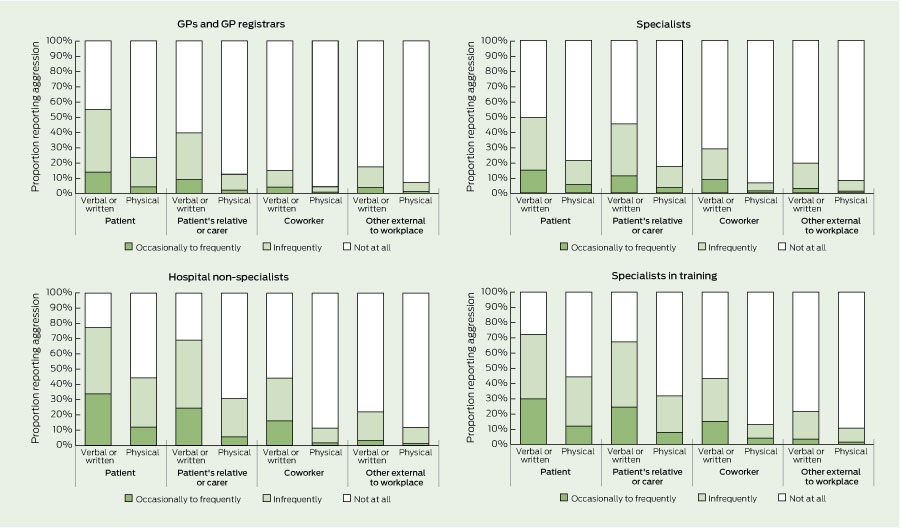
Overall, 70.6% (95% CI, 69.7%–71.5%) of clinicians reported experiencing verbal or written aggression, and 32.3% (95% CI, 31.3%–33.3%) reported experiencing physical aggression from one or more sources in the previous 12 months. As shown in Box 3, exposure levels varied by source, form and doctor type. There were statistically significant differences (P < 0.01) between aggression prevalence from each source reported by doctor type. Verbal aggression from each source was reported by up to one-and-a-half times the proportion of hospital non-specialists and specialists in training compared with GPs and specialists, and up to two times for physical aggression from each source.
Differences by clinicians’ sex were also identified (Box 4). Overall, 69.1% (95% CI, 67.9%–70.4%) of male clinicians reported experiencing verbal or written aggression in the previous 12 months from one or more sources compared with 72.6% (95% CI, 71.1%–73.9%) of female clinicians, while 31.2% (95% CI, 30.0%–32.5%) of male clinicians reported experiencing physical aggression in the previous 12 months from one or more sources compared with 33.8% (95% CI, 32.3%–35.3%) of female clinicians. The differences, however, were unevenly spread across aggression sources for each doctor type (Box 4).
Age and years since graduation were strongly correlated (ρ = 0.968; P < 0.001) across all doctor types. Both variables, almost identically, were negatively though weakly associated with the reported frequency of workplace aggression from each source in the previous 12 months (Box 5). This pattern was replicated for individual doctor types, but the statistical significance of associations disappeared for hospital non-specialists and specialists in training.
There are few comparable studies on workplace aggression in clinical medical practice, not only in relation to the scale and scope of the research, but also because of differences in definitions, terminologies and recall periods employed by researchers. Nevertheless, consistent with the broader health care literature,4,16-19 patients were the most common source of aggression, followed by aggression from patients’ relatives or carers, and prevalence rates for non-physical aggression were generally one-and-a-half to four times that for physical aggression. For GPs and GP registrars, the prevalence of verbal aggression from patients (54.9%) was consistent with outcomes from previous Australian research (42%–58%), but the prevalence of physical aggression was much higher (23.4% v 2%–6%).5-8 Coworkers were the third most common source of aggression overall. Prevalence rates for coworker verbal aggression (14.8%–44.3%) and physical aggression (4.3%–13.0%) were much higher than for United Kingdom clinicians, where less than 5% experienced verbal aggression and less than 1% experienced physical aggression from coworkers in the previous 12 months.20,21
Of particular importance is the finding that workplace aggression prevalence for the primarily hospital-based, younger and less experienced hospital non-specialists and specialists in training was up to twice that for GPs or specialists. Other studies suggest that hospital-based medical work is a greater risk for workplace aggression than community-based practice,7,22,23 no doubt related to higher levels of patient acuity, stress and distress. Other research evidence supports the contention that younger and less experienced medical practitioners are at higher risk of workplace aggression than older and more experienced clinicians.5,8,24
Hospital non-specialists and specialists in training are about 15 to 25 years younger and comprise relatively more female clinicians compared with specialists. They are more likely to be afforded lower status in “a pecking order of seniority”.25 They are also likely to be less skilled or experienced in aggression minimisation and de-escalation, particularly where the perpetrators are more senior personnel or clinical colleagues. Clearly, greater institutional efforts are required to enhance the aggression minimisation skills of doctors who are new to clinical practice, and to reduce both the prevalence and impact of workplace aggression.
With the exception of coworker aggression, female GPs experienced significantly less aggression from all other sources than male clinicians. This contrasts with other studies showing that female GPs experienced more bullying, gender-based or sexual aggression.5-8 In addition, all female clinicians experienced lower rates of aggression from others external to the workplace. This suggests that, where non-clinically or non-professionally related aggression arises in the workplace, male clinicians are more often the target of, or more often at the forefront of dealing with, such incidents. The finding that more female than male specialists in training report verbal or written and physical aggression from patients and verbal or written aggression from patients’ relatives or carers suggests a particular risk for junior female clinicians.
IMGs in general practice appear more vulnerable to workplace aggression. While previous Australian qualitative research suggests that some individual cultural and communication issues may serve as triggers for aggression,26 overall there has been a lack of research investigating IMG experiences of workplace aggression. More research is clearly warranted, since IMGs have an important role in efforts to ensure Australia has sufficient medical practitioners to maintain medical care in non-metropolitan communities and areas of workforce shortages.
The importance of workplace aggression in medicine cannot be underestimated. Beyond individual physical and mental health effects,1-4 there is evidence of the greater impact of the more prevalent non-physical forms of aggression on work participation decisions.18 Doctors exposed to workplace aggression have reported a loss of confidence or enthusiasm for treating patients20,21 and increased medical errors.27 A failure to reduce the prevalence and impact of workplace aggression, especially for younger clinicians and IMGs, may also contribute to ongoing challenges in the recruitment and retention of medical practitioners in this era of increasing workforce shortages internationally.28
1 Profile of survey respondents compared with national profile, by doctor type, state and rurality, March 2010 – June 2011
MABEL = Medicine in Australia: Balancing Employment and Life. MDA = Medical Directory of Australia, accessed May 2010.13 GP = general practitioner. ACT = Australian Capital Territory. NSW = New South Wales. NT = Northern Territory. Qld = Queensland. SA = South Australia. Tas = Tasmania. Vic = Victoria. WA = Western Australia. * P < 0.001 for categories (not subcategories).
2 Profile of survey respondents compared with national profile (age and sex), by doctor type, March 2010 – June 2011
MABEL = Medicine in Australia: Balancing Employment and Life. MDA = Medical Directory of Australia, accessed May 2010.13 GP = general practitioner. * P < 0.001 for all subcategories except male hospital non-specialist, which was not significant.
3 Proportions of medical practitioners reporting workplace aggression within the previous 12 months, by doctor type and source of aggression, March 2010 – June 2011 (n = 9449)
4 Proportions of medical practitioners reporting workplace aggression within the previous 12 months, by doctor type, form of aggression, doctor’s sex and source of aggression, March 2010 – June 2011 (n = 9449)
| Men | ||||||
| Men | ||||||
| Men | ||||||
Received 4 March 2012, accepted 5 July 2012
- Danny J Hills1
- Catherine M Joyce1
- John S Humphreys2
- 1 Department of Epidemiology and Preventive Medicine, Monash University, Melbourne, VIC.
- 2 School of Rural Health, Monash University, Bendigo, VIC.
No relevant disclosures.
- 1. Mayhew C, Chappell D. Workplace violence: an overview of patterns of risk and the emotional/stress consequences on targets. Int J Law Psychiatry 2007; 30: 327-339.
- 2. di Martino V. Workplace violence in the health sector. Country case studies: Brazil, Bulgaria, Lebanon, Portugal, South Africa, Thailand and an additional Australian study. Synthesis report. Geneva: Joint Programme on Workplace Violence in the Health Sector, 2002. http://www.who.int/violence_injury_prevention/injury/en/WVsynthesisreport.pdf (accessed Jul 2012).
- 3. di Martino V. Workplace violence in the health sector: relationship between work stress and workplace violence in the health sector. Geneva: Joint Programme on Workplace Violence in the Health Sector, 2003. http://www.who.int/violence_injury_prevention/violence/interpersonal/WVstresspaper.pdf (accessed Jul 2012).
- 4. Hahn S, Zeller A, Needham I, et al. Patient and visitor violence in general hospitals: a systematic review of the literature. Aggress Violent Beh 2008; 13: 431-441.
- 5. Koritsas S, Coles J, Boyle M, Stanley J. Prevalence and predictors of occupational violence and aggression towards GPs: a cross-sectional study. Br J Gen Pract 2007; 57: 967-970.
- 6. Magin PJ, Adams J, Sibbritt DW, et al. Experiences of occupational violence in Australian urban general practice: a cross-sectional study of GPs. Med J Aust 2005; 183: 352-356.
- 7. Tolhurst H, Baker L, Murray G, et al. Rural general practitioner experience of work-related violence in Australia. Aust J Rural Health 2003; 11: 231-236.
- 8. Forrest LE, Herath PM, McRae IS, Parker RM. A national survey of general practitioners’ experiences of patient-initiated aggression in Australia. Med J Aust 2011; 194: 605-608.
- 9. Mayhew C, Chappell D. Occupational violence: types, reporting patterns, and variations between health sectors. Working paper series 139. Sydney: School of Industrial Relations and Organizational Behaviour and Industrial Relations Research Centre, University of New South Wales, 2001.
- 10. Mayhew C, Chappell D. The occupational violence experiences of 400 Australian health workers: an exploratory study. J Occup Health Safety Aust N Z 2003; 19: 3-43.
- 11. Banks G. Challenges of evidence-based policy-making. Canberra: Australian Public Service Commission, 2009.
- 12. Hills DJ, Joyce CM, Humphreys JS. Prevalence and prevention of workplace aggression in Australian clinical medical practice. Aust Health Rev 2011; 35: 253-261.
- 13. Australasian Medical Publishing Company. Medical Directory of Australia. https://www.mda.com.au/secure2.jsp (subscription accessed Feb and May 2010).
- 14. Joyce CM, Scott A, Jeon SH, et al. The “Medicine in Australia: Balancing Employment and Life (MABEL)” longitudinal survey — protocol and baseline data for a prospective cohort study of Australian doctors’ workforce participation. BMC Health Serv Res 2010; 10: 50. http://www.biomedcentral.com/1472-6963/10/50 (accessed Feb 2012).
- 15. Australian Institute of Health and Welfare. Rural, regional and remote health: a guide to remoteness classifications. Canberra: AIHW, 2004. (AIHW Cat. No. PHE 53; Rural Health Series No. 4.) http://www.aihw.gov.au/publications/phe/rrrh-gtrc/rrrh-gtrc.pdf (accessed Feb 2012).
- 16. Arnetz JE, Arnetz BB. Violence towards health care staff and possible effects on the quality of patient care. Soc Sci Med 2001; 52: 417-427.
- 17. Alexander C, Fraser J. Occupational violence in an Australian healthcare setting: implications for managers. J Healthc Manag 2004; 49: 377-392.
- 18. Gerberich SG, Church TR, McGovern PM, et al. An epidemiological study of the magnitude and consequences of work related violence: the Minnesota Nurses’ Study. Occup Environ Med 2004; 61: 495-503.
- 19. O’Brien-Pallas L, Hayes L, Wang S, Laporte D. Creating work environments that are violence free. World Hosp Health Serv 2009; 45: 12-18.
- 20. Health Policy and Economic Research Unit. Violence at work: the experience of UK doctors. London: British Medical Association, 2003.
- 21. Health Policy and Economic Research Unit. Violence in the workplace: the experience of doctors in Great Britain. London: British Medical Association, 2008.
- 22. Catanesi R, Carabellese F, Candelli C, et al. Violent patients: what Italian psychiatrists feel and how this could change their patient care. Int J Offender Ther Comp Criminol 2010; 54: 441-447.
- 23. Aydin B, Kartal M, Midik O, Buyukakkus A. Violence against general practitioners in Turkey. J Interpers Violence 2009; 24: 1980-1995.
- 24. Arimatsu M, Wada K, Yoshikawa T, et al. An epidemiological study of work-related violence experienced by physicians who graduated from a medical school in Japan. J Occup Health 2008; 50: 357-361.
- 25. Paice E, Aitken M, Houghton A, Firth-Cozens J. Bullying among doctors in training: cross sectional questionnaire survey. BMJ 2004; 329: 658-659.
- 26. Parker RM, Ceramidas DM, Forrest LE, et al. Patient initiated aggression and violence in the Australian general practice setting. Canberra: The Australian Primary Health Care Institute, 2010. http://aphcri.anu.edu.au/sites/aphcri.anu.edu. au/files/panel/214/violence_in_general_practice_pdf_32978.pdf (accessed Jun 2012).
- 27. Paice E, Smith D. Bullying of trainee doctors is a patient safety issue. Clin Teach 2009; 6: 13-17.
- 28. National Health Workforce Taskforce. Health workforce in Australia and factors for current shortages. Canberra: Canberra: Australian Health Workforce Online, 2009. http://www.ahwo.gov. au/documents/NHWT/The health workforce in Australia and factors influencing current shortages.pdf (accessed Feb 2012).





Abstract
Objective: To describe the 12-month prevalence of verbal or written and physical aggression from patients, patients’ relatives or carers, coworkers and others in Australian clinical medical practice.
Design, setting and participants: An exploratory, descriptive study of cross-sectional survey design in the third wave (March 2010 to June 2011) of the Medicine in Australia: Balancing Employment and Life longitudinal survey.
Main outcome measures: Proportions of clinicians reporting verbal or written and physical aggression from each aggression source and the significance of differences reported by doctor type, sex, international medical graduate status, age and postgraduate experience.
Results: Of 16 327 medical practitioners sampled, a response rate of 60.9% (9951) was achieved and 9449 (57.9%) were in Australian clinical practice. Participants comprised 3515 general practitioners and GP registrars, 3875 specialists, 1171 hospital non-specialists and 888 specialists in training. Overall, 70.6% of medical practitioners experienced verbal or written aggression and 32.3% experienced physical aggression from one or more sources in the previous 12 months. While patterns of exposure were complex, more female clinicians, international medical graduates (IMGs) and hospital-based clinicians experienced workplace aggression. Age and postgraduate experience were significantly negatively associated with aggression exposure.
Conclusions: This is the first nationwide study of workplace aggression from all sources experienced by all subpopulations of Australian medical clinicians. The findings suggest particular risks for younger and more junior hospital-based clinicians, and for IMGs in general practice. A failure to address this important professional and public health concern may contribute to ongoing challenges in the recruitment and retention of medical practitioners in an era of increasing shortages internationally.