Heart failure is a growing public health problem around the world, currently affecting more than 37.7 million people.1 Although the management of heart failure has improved markedly over the past three decades, about 50% of patients die within five years of diagnosis,2 suggesting that important pathogenic mechanisms are not addressed by current treatment.
Trimethylamine N‐oxide (TMAO) is formed in the liver from trimethylamine, which is generated exclusively by the gut microbiota from dietary phosphatidylcholine, choline, and carnitine.3,4 Elevated plasma TMAO levels are associated with increased risks of cardiovascular disease and renal fibrosis,5,6,7,8,9,10 and TMAO levels are higher in patients with heart failure than in other people.11,12,13,14,15,16 However, whether elevated TMAO is a biomarker with prognostic value for patients with heart failure is unclear. It has been reported that high plasma TMAO is an independent risk factor for long term mortality in patients with chronic heart failure, even after adjusting for renal insufficiency and natriuretic peptide levels.16 But some studies have found that adjusting for indices of renal function reduced the strength of the association between TMAO level and mortality risk,14,17 suggesting that it is a marker of cardio‐renal function interaction, but not of the prognosis for patients with heart failure.
To assess the prognostic value of TMAO in patients with heart failure, and to determine whether this association is modified by renal dysfunction, we performed a systematic review and meta‐analysis of prospective clinical studies.
Methods
Search strategy and selection criteria
Applying the recommendations of the Meta‐analysis of Observational Studies in Epidemiology group,18 we searched electronic databases (PubMed and EMBASE) for prospective studies published to 31 October 2019. We used a combined MeSH heading and text search strategy with the following terms: “trimethylamine N‐oxide” or “TMAO” and “heart failure”, “cardiac failure”, “myocardial failure”, “cardiac dysfunction”, “heart dysfunction”, or “myocardial dysfunction” (Supporting Information, table 1). We did not restrict our search by language or publication type. Reference lists were checked to identify further relevant studies.
We included publications in our analysis that described prospective studies of heart failure in adults (18 or more years old), assessed plasma TMAO concentration and other cardiovascular risk factors at baseline, and reported adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) for adverse cardiac outcomes of heart failure by TMAO level.
Studies were excluded if they reported only unadjusted risks for associated events, if duplicate outcomes were derived from the same studies, or if the outcomes of interest were not clearly reported.
Our primary outcome was the composite outcome of major adverse cardiac events (MACEs), including all‐cause mortality, hospitalisation with heart failure, and heart transplantation; the secondary outcome was all‐cause mortality alone.
Data extraction and quality assessment
Two reviewers (WL, AH) independently conducted literature searches and screened publications according to our criteria. Study information — participant characteristics, study sample size, methods for assessing TMAO, duration of follow‐up, adjusted risk factors, and outcome assessment — were recorded. The principal authors of retrieved publications were contacted for additional data if necessary.
We assessed the quality of the included studies with the Newcastle–Ottawa Quality Assessment Scale for observational studies.19 The scale assesses selection (four items, one point each), comparability (one item, up to two points), and exposure/outcome (three items, one point each). We graded the quality of included studies as good (at least 7 points), fair (4–6 points), or poor (fewer than 4 points).
Data synthesis and analysis
In the included publications, the relationship between TMAO concentration and outcomes was reported as hazard ratios based on a standard deviation (SD) increment in TMAO concentration or by comparing outcomes for TMAO level tertiles, quartiles, or quintiles. To enable a consistent approach for the meta‐analysis and to facilitate interpretation, we performed two comparisons: we calculated HRs for people in the highest and lowest TMAO tertiles, and we calculated HRs based on an SD increment in baseline TMAO concentration. If a study did not report effect measures per tertile or per SD difference, we converted the results according to previously reported methods.8,20 Briefly, we assumed that the exposure variable (TMAO) is normally distributed and that the association with MACEs or all‐cause mortality was log‐linear. The expected difference in means of the highest and lowest tertiles of the standard normal distribution is 2.18 SDs. The HRs reported for the highest and lowest tertile comparison can thus be converted to HRs based on SD difference by dividing the log HRs by 2.18; similarly, HRs per SD difference can be multiplied by 2.18 to obtain the highest v lowest tertile comparison. The corresponding factor for comparing extreme quartiles is 2.54, and 2.80 for extreme quintiles. Conversely, HRs comparing extreme quartiles or quintiles can be converted to comparisons of extreme tertiles by multiplying the log HRs by 2.18/2.54 or 2.18/2.80 respectively.
Outcomes adjusted for multiple variables were extracted for meta‐analysis. If a publication reported several results adjusted for different numbers of covariates, the result adjusted for the greatest number of variables was extracted for our meta‐analysis. To explore whether the association of prognosis with TMAO level was mediated by renal dysfunction, studies with estimates of HRs both before and after adjustment for estimated glomerular filtration rate (eGFR) were also extracted for meta‐analysis. The inverse variance approach was used to combine the log HRs and corresponding standard errors (SEs) in random effects models.
Heterogeneity among studies was expressed with the I2 statistic; values exceeding 50% were deemed statistically significant. However, even when heterogeneity was not significant, results from random effects models (rather than fixed effects models) were reported because of clinical and methodologic heterogeneity, such as differences in study design, baseline characteristics of patients, adjustment for confounding variables, and follow‐up duration.21
Subgroup analyses of primary outcomes were conducted according to mean age (under 65 years, 65 years or more), follow‐up duration (less than 5 years, 5 years or more), heart failure type (acute, chronic), and study sample size (fewer than 1000, at least 1000 participants). Publication bias was evaluated by inspecting funnel plots for outcomes in which the natural log HR was plotted against SE, as well as with the Egger and Begg tests. In sensitivity analyses for assessing the impact of individual studies on the estimated risk, pooled HR was re‐calculated after omitting one study at a time. We also conducted sensitivity analyses in which fixed effects rather than random effects models were used for the meta‐analysis.
All analyses were performed in RevMan 5.3 (Cochrane Collaboration).
Results
Characteristics of the included studies
A total of 109 potentially relevant publications were identified in the PubMed and EMBASE database searches. After screening the titles and abstracts, 18 qualified for full review (Supporting Information, figure 1), of which seven studies,11,12,13,14,15,16,17 with a total of 6879 participants, were included in our meta‐analysis. Baseline plasma TMAO levels were reported in all included studies (Box 1).
Only one study included patients with acute heart failure;14 all others included patients with stable or chronic heart failure. Follow‐up duration ranged from one to 9.7 years, with median follow‐up of 5.0 years. The quality of five studies was graded as good11,12,13,14,16 and of two as fair15,17 (Box 1; Supporting Information, table 2).
Primary outcome: association between TMAO level and MACEs in patients with heart failure
The heterogeneity of the seven included studies with respect to the association of MACEs with TMAO level was not significant, whether assessed per tertile (I2 = 0%) or per SD increment (I2 = 0%). Random effects model analyses indicated that higher TMAO level was associated with greater risk of MACEs in patients with heart failure (tertile 3 v tertile 1: HR, 1.68; 95% CI, 1.44–1.96; per SD increment: HR, 1.26; 95% CI, 1.18–1.36) (Box 2). Neither visual inspection of the funnel plot (Supporting Information, figure 2) nor the Egger and Begg tests (data not shown) provided evidence of publication bias.
Secondary outcome: association between TMAO level and all‐cause mortality in patients with heart failure
Five studies reported the association of all‐cause mortality with TMAO level.11,14,15,16,17 Their heterogeneity was significant, whether results were evaluated per TMAO level tertile (I2 = 64%) or per SD increment (I2 = 65%). Random effects model analyses indicated that higher TMAO level was associated with greater risk of all‐cause mortality in patients with heart failure (tertile 3 v tertile 1: HR, 1.67; 95% CI, 1.17–2.38; per SD increment: HR, 1.26; 95% CI, 1.07–1.48) (Box 3). Neither visual inspection of the funnel plot (Supporting Information, figure 3) nor the Egger and Begg tests (data not shown) provided evidence of publication bias.
The importance of renal function for the association between TMAO level and MACEs in patients with heart failure
Six studies reported MACE risk before and after adjusting for eGFR.11,13,14,15,16,17 Without adjustment for eGFR, the highest TMAO level tertile was associated with greater risk of MACEs than the lowest tertile (HR, 2.10; 95% CI, 1.76–2.51); the difference was smaller after adjusting for eGFR but still significant (HR, 1.59; 95% CI, 1.30–1.94). The heterogeneity of the six studies with respect to MACE risk was significant (I2 = 76%). Similar results were obtained when the risk was evaluated per SD increment in TMAO level (without adjusting for eGFR: HR, 1.36; 95% CI, 1.25–1.47; after adjusting for eGFR: HR, 1.23; 95% CI, 1.12–1.35) (Box 4).
Sensitivity and subgroup analyses
Sensitivity analyses using fixed effects models instead of random effects models, or re‐calculating the HRs after omitting one study at a time, yielded results similar to our primary findings (data not shown). High TMAO level was associated with increased risks of MACEs in all subgroups, except for patients with acute heart failure (tertile 3 v tertile 1: HR, 1.21; 95% CI, 0.83–1.76; per SD increment: HR, 1.09; 95% CI, 0.92–1.29) (Box 5).
Discussion
In the first meta‐analysis of studies on this topic, we found that, after controlling for several cardiovascular disease risk factors, higher TMAO levels were associated with poorer prognoses with respect to all‐cause mortality, hospitalisation with heart failure, and heart transplantation for patients with heart failure. The association remained significant after further adjusting for eGFR, indicating that the predictive value of TMAO is not wholly attributable to diminished cardio‐renal function, but is also linked with other pathophysiological processes.
Patients with heart failure are consistently reported to have higher plasma TMAO concentrations than other people.11,12,14,15,16 Several mechanisms may underlie this phenomenon, including intestinal congestion and dysfunction caused by heart failure, leading to dysbiosis of the gut microbiome;22,23 reduced perfusion leading to increased intestinal permeability and consequently to higher circulating levels of the TMAO precursor trimethylamine;24 and reduced clearance of TMAO secondary to cardio‐renal dysfunction in people with congestive heart failure, leading to its systemic accumulation.25 It is therefore possible that higher TMAO concentrations in people with heart failure reflect the severity of heart failure and renal dysfunction. Our findings are consistent with those of a laboratory study which found that the severity of myocardial fibrosis and heart failure was exacerbated in mice fed TMAO.26
Previous meta‐analyses have found that elevated TMAO concentrations were associated with increased risks of cardiovascular disease and all‐cause mortality.7,8,9 However, they included studies of great heterogeneity with respect to patient characteristics, including people with diabetes, chronic kidney disease, acute coronary syndrome, and community‐acquired pneumonia. These studies did not report the association of TMAO level and prognosis in patients with heart failure, nor was the influence of renal dysfunction on the increase in risks associated with higher TMAO concentrations examined. In contrast, our meta‐analysis included only studies of patients with heart failure, and we assessed the association between TMAO level and the risks of adverse events before and after adjusting for eGFR, allowing us to explore the influence of renal dysfunction on relative risks in patients with higher TMAO concentrations.
Several mechanisms may contribute to the poor prognosis for patients with heart failure who have higher TMAO levels. TMAO has pro‐atherogenic properties27,28 that may contribute to the adverse prognosis for patients with heart failure and accompanying coronary artery disease. However, the adverse effect of elevated TMAO levels has been reported to be similar in ischaemic and non‐ischaemic heart failure,11 suggesting that other mechanisms are involved, such as inflammation and oxidative stress,29,30 direct suppressive effects on the myocardium by inhibition of the actomyosin motor,31 and impaired fatty acid oxidation in cardiac mitochondria.32
Our findings underscore the importance of microbiota‐dependent TMAO formation for the prognosis for people with heart failure, independent of traditional risk factors, including renal dysfunction. They have important implications for risk stratification and the treatment of patients with heart failure. The BIOSTAT‐CHF (BIOlogy Study to TAilored Treatment in Chronic Heart Failure) found that current guideline‐based heart failure treatment did not affect TMAO levels, and that patients with higher plasma TMAO both before and after treatment had poorer outcomes.16
Therapeutic interventions for reducing TMAO levels may be useful as adjunctive therapy for patients with heart failure. Laboratory studies and preliminary clinical trials have found that modulating gut microbiota composition and function through diet, the use of prebiotics and probiotics, and targeted non‐lethal antimicrobial enzyme inhibitors can reduce TMAO levels.33,34,35 Whether these strategies would improve outcomes for people with heart failure remains to be established.34 For example, the GutHeart phase II randomised clinical trial in Norway and Brazil is testing the hypothesis that the non‐absorbable antibiotic rifaximin, by manipulating the bacterial composition of the gut, can reduce inflammatory activation and the progression of heart failure.36
Limitations of our meta‐analysis
First, without access to data for individual patients, residual confounding by unidentified factors was possible. However, we included only prospective studies that reported adjusted HRs, and most were adjusted for several risk factors relevant to the prognosis of heart failure, including natriuretic peptide levels and eGFR. Our findings were also stable in several sensitivity and subgroup analyses.
Second, as plasma TMAO concentration is affected by diet, it is unclear whether the influence of TMAO level on cardiovascular risk is attributable to foods rich in l‐carnitine (such as red meat),37 as investigators have not controlled for the effect of diet. Further, as all included studies were conducted in Europe or the United States, it is unknown whether the association of TMAO level with prognosis for patients with heart failure is similar in populations with different dietary patterns (eg, east Asians). However, as plasma TMAO level is determined not only by l‐carnitine intake, but also by gut microbiota dysbiosis and renal dysfunction,38 diet is unlikely to wholly explain the estimated increase in risk.
Third, in subgroup analyses we found that the risk of MACEs for patients with acute heart failure was not increased for those with higher plasma TMAO levels. However, only one study focused on patients with acute heart failure, and they were followed up for only one year.14 Large studies examining the association of TMAO level with acute heart failure, with long term follow‐up, are needed.
Finally, the pathophysiological mechanisms underlying heart failure with reduced ejection fraction and heart failure with preserved ejection fraction are different.39 The influence of TMAO level in patients with the two types of heart failure could not be compared, as the requisite data were not available.
Conclusions
We found that elevated TMAO plasma level is associated with a poorer long term prognosis for patients with heart failure, even after adjusting for renal dysfunction. Studies that clarify whether treatment strategies that aim to reduce TMAO plasma levels are beneficial for people with heart failure are still needed.
Box 1 – Summary characteristics of the included studies of trimethylamine N‐oxide (TMAO) levels in patients with heart failure
|
Study |
Tang 201411 |
Tang 201512 |
Trøseid 201513 |
Suzuki 201614 |
Schuett 201715 |
Suzuki 201916 |
Salzano 201917 |
||||||||
|
|
|||||||||||||||
|
Location |
USA |
USA |
Norway |
UK |
Germany |
Europe |
UK |
||||||||
|
Heart failure type |
Chronic |
Chronic |
Chronic |
Acute |
Chronic |
Chronic |
Chronic |
||||||||
|
Number of patients (male proportion) |
720 (59%) |
112 (84%) |
155 (83%) |
972 (61%) |
2490 (NA) |
2234 (74%) |
196 (50%) |
||||||||
|
Age (years), mean (SD or range) |
66 (10) |
57 (14) |
57 (11) |
78 (69–84) |
63 (10) |
70 (61–78) |
73 (63–78) |
||||||||
|
TMAO in patients with heart failure (μmol/L), median (IQR) |
5.0 (3.0–8.5) |
5.8 (3.6–12.1) |
NA |
5.6 (3.4–10.5) |
4.7 (3.22–6.85) |
5.9 (3.6–10.8) |
7.0 (4.2–12.5) |
||||||||
|
Follow‐up (years), median |
5 |
5 |
5.2 |
1 |
9.7 |
3 |
5 |
||||||||
|
Events for analysis |
All‐cause mortality |
All‐cause mortality/heart transplantation |
All‐cause mortality/heart transplantation |
All‐cause mortality; |
All‐cause mortality |
All‐cause mortality; |
All‐cause mortality; |
||||||||
|
Adjusted risk factors |
|
|
|
|
|
|
|
||||||||
|
Age |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
Yes |
||||||||
|
Sex |
Yes |
— |
— |
— |
Yes |
— |
Yes |
||||||||
|
Blood pressure |
Systolic |
— |
— |
Systolic |
|
Systolic,diastolic |
|
||||||||
|
NYHA class |
— |
— |
Yes |
Yes |
— |
— |
— |
||||||||
|
eGFR |
Yes |
Yes |
Yes |
Yes |
— |
Yes |
Yes |
||||||||
|
Diabetes mellitus |
Yes |
— |
Yes |
Yes |
— |
Yes |
— |
||||||||
|
Smoking |
Yes |
— |
— |
— |
— |
— |
— |
||||||||
|
Body mass index |
|
— |
— |
— |
— |
— |
Yes |
||||||||
|
BNP |
Yes |
— |
— |
— |
— |
Yes |
— |
||||||||
|
NT‐proBNP |
— |
Yes |
Yes |
Yes |
— |
— |
— |
||||||||
|
Sodium |
— |
— |
— |
Yes |
— |
Yes |
— |
||||||||
|
Other |
LDL‐C, HDL‐C |
Ratio of early (E) and late (A) diastolic filling velocities by tissue Doppler imaging |
Hypertension |
Heart rate, respiratory rate |
— |
Blood urea, haemoglobin, β‐blockers, previous hospitalisation with HF, peripheral oedema, ischaemic aetiology, COPD |
— |
||||||||
|
Study quality |
Good |
Good |
Good |
Good |
Fair |
Good |
Fair |
||||||||
|
|
|||||||||||||||
|
BNP = B‐type natriuretic peptide; COPD = chronic obstructive pulmonary disease; CRP = C‐reactive protein; eGFR = estimated glomerular filtration rate; HDL‐C = high‐density lipoprotein cholesterol; HF = heart failure; hsCRP = high‐sensitivity C‐reactive protein; IQR = interquartile range; LDL‐C = low‐density lipoprotein cholesterol; NA = not available; NT‐proBNP = N‐terminal pro‐B‐type natriuretic peptide; NYHA = New York Heart Association; SD = standard deviation. |
|||||||||||||||
Box 2 – Risk of major adverse cardiac events (MACEs) in patients with heart failure, by trimethylamine N‐oxide (TMAO) level
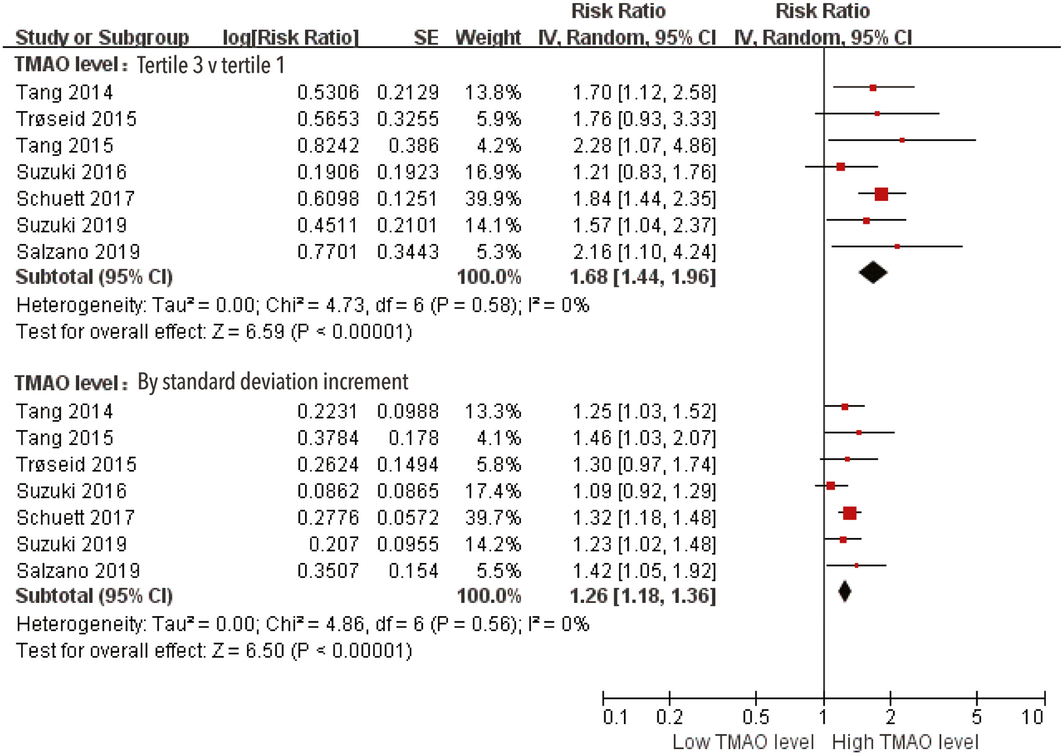
CI = confidence interval; IV = inverse variance approach; SE = standard error.
Box 3 – Risk of all‐cause mortality in patients with heart failure, by trimethylamine N‐oxide (TMAO) level
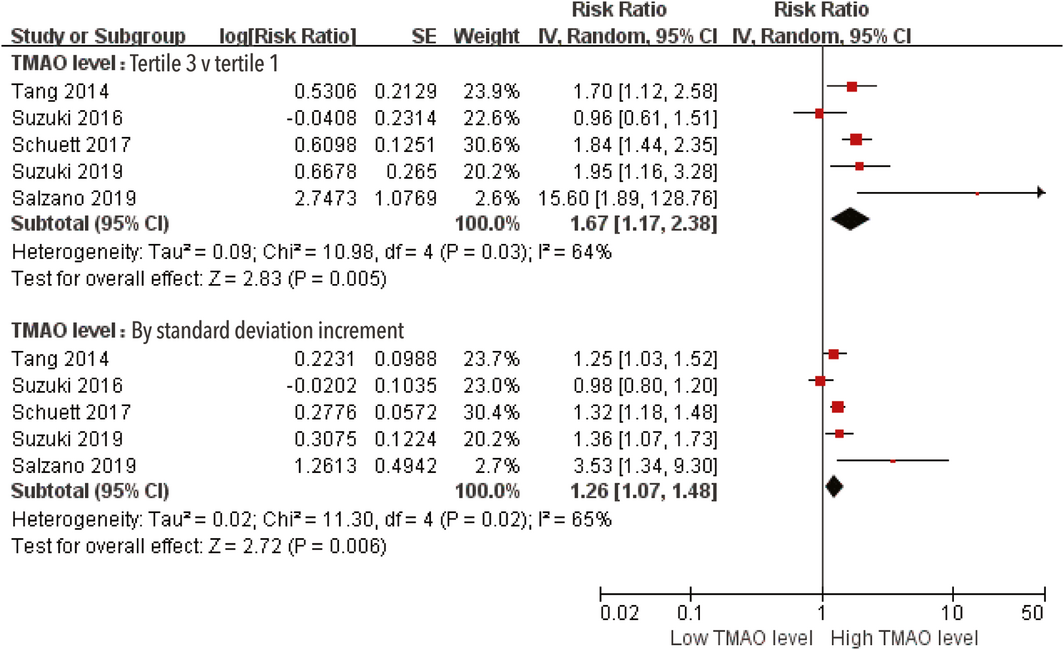
CI = confidence interval; IV = inverse variance approach; SE = standard error.
Box 4 – Risk of major adverse cardiac events (MACEs) in patients with heart failure, by trimethylamine N‐oxide (TMAO) level, before and after adjusting for estimated glomerular filtration rate (eGFR)
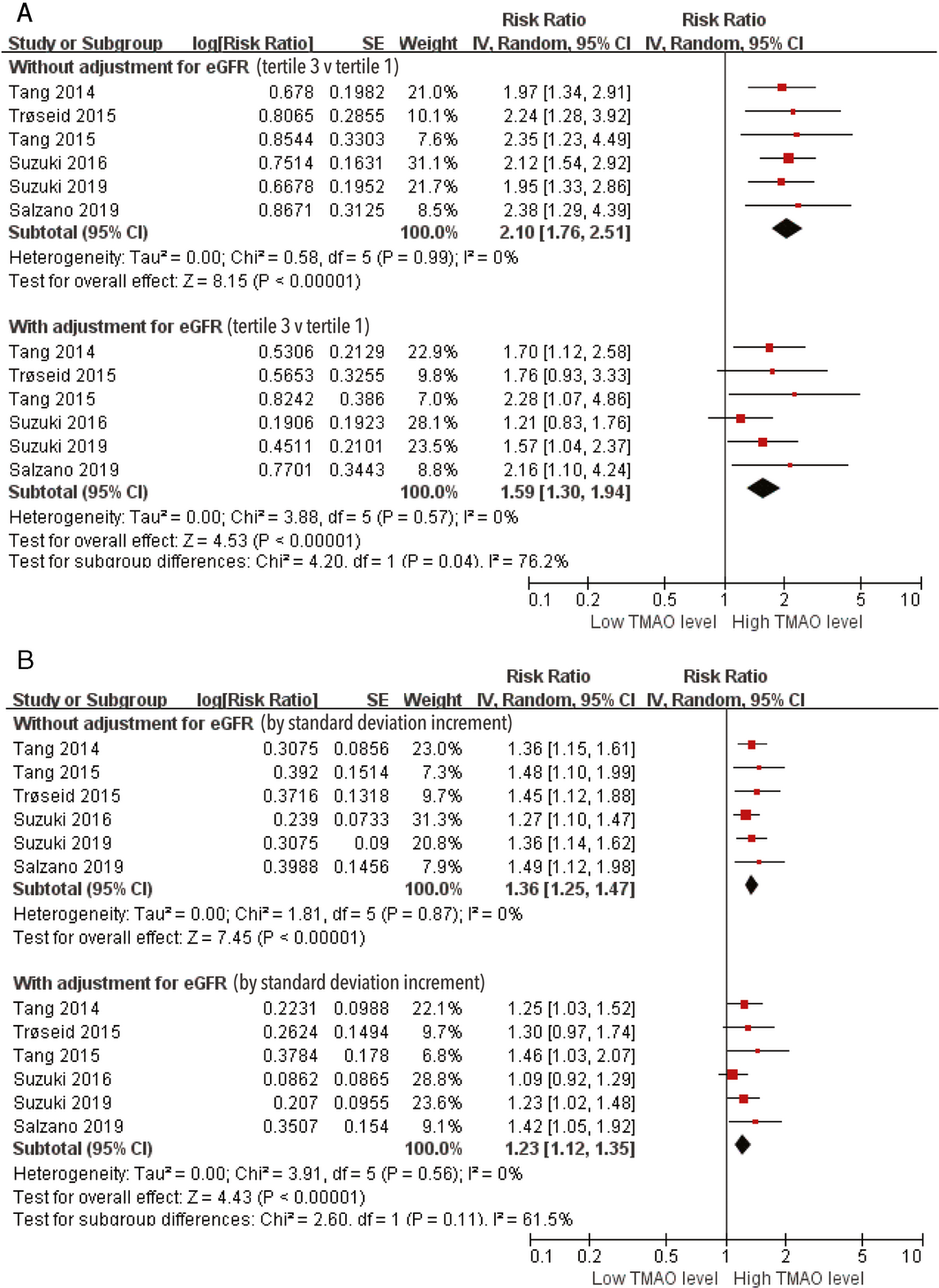
CI = confidence interval; IV = inverse variance approach; SE = standard error.
Box 5 – Risk of major adverse cardiac events (MACEs) in patients with heart failure, by trimethylamine N‐oxide (TMAO) level: subgroup analyses
|
|
Studies |
Tertile 3 v tertile 1 |
Per standard deviation increment |
||||||||||||
|
Hazard ratio (95%CI) |
P * |
I 2 |
Hazard ratio (95%CI) |
P * |
I 2 |
||||||||||
|
|
|||||||||||||||
|
Mean age |
|
|
0.20 |
40% |
|
0.17 |
47% |
||||||||
|
< 65 years |
3 |
1.86 (1.50–2.32) |
|
|
1.33 (1.20–1.47) |
|
|
||||||||
|
≥ 65 years |
4 |
1.52 (1.22–1.89) |
1.20 (1.09–1.33) |
||||||||||||
|
Follow‐up duration |
|
|
0.07 |
69% |
|
0.08 |
68% |
||||||||
|
< 5 years |
2 |
1.36 (1.03–1.80) |
|
|
1.15 (1.02–1.31) |
|
|
||||||||
|
≥ 5 years |
5 |
1.85 (1.54–2.23) |
1.32 (1.21–1.44) |
||||||||||||
|
Heart failure type |
|
|
0.06 |
72% |
|
0.06 |
72% |
||||||||
|
Acute |
1 |
1.21 (0.83–1.76) |
|
|
1.09 (0.92–1.29) |
|
|
||||||||
|
Chronic |
6 |
1.80 (1.52–2.13) |
1.30 (1.21–1.41) |
||||||||||||
|
Study sample size (participants) |
|
|
0.51 |
0% |
|
0.46 |
0% |
||||||||
|
< 1000 |
5 |
1.59 (1.27–2.00) |
|
|
1.23 (1.11–1.36) |
|
|
||||||||
|
≥ 1000 |
2 |
1.77 (1.43–2.18) |
|
|
1.30 (1.18–1.43) |
|
|
||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * For heterogeneity among subgroups. |
|||||||||||||||
Received 10 January 2020, accepted 23 April 2020
- Wensheng Li1
- Anqing Huang1
- Hailan Zhu1
- Xinyue Liu1
- Xiaohui Huang1
- Yan Huang1
- Xiaoyan Cai1
- Jianhua Lu1
- Yuli Huang1,2
- 1 Shunde Hospital of Southern Medical University, Foshan (Guangdong), China
- 2 George Institute for Global Health, Sydney, NSW
Our investigation was supported by the Science and Technology Innovation Project in Foshan, Guangdong (FS0AA‐KJ218‐1301‐0006), the Clinical Research Startup Program of Shunde Hospital, Southern Medical University (CRSP2019001, CRSP2019008), the self‐financing Science and Technology Plan Project of Foshan, Guangdong (Medical Science and Technology Research Key Project; 2018AB00208), and the Medical Science and Technology Research Foundation of Guangdong Province (A2018209).We thank Julia Jenkins (Liwen Bianji, Edanz Editing China; www.liwenbianji.cn/ac), for editing the English text of our manuscript.
No relevant disclosures.
- 1. Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol 2016; 13: 368–378.
- 2. Benjamin EJ, Muntner P, Alonso A, et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2019 update. A report from the American Heart Association. Circulation 2019; 139: e56–e528.
- 3. Tang W, Bäckhed F, Landmesser U, Hazen SL. Intestinal microbiota in cardiovascular health and disease. J Am Coll Cardiol 2019; 73: 2089–2105.
- 4. Brown JM, Hazen SL. Microbial modulation of cardiovascular disease. Nat Rev Microbiol 2018; 16: 171–181.
- 5. Antza C, Stabouli S, Kotsis V. Gut microbiota in kidney disease and hypertension. Pharmacol Res 2018; 130: 198–203.
- 6. Kanbay M, Onal EM, Afsar B, et al. The crosstalk of gut microbiota and chronic kidney disease: role of inflammation, proteinuria, hypertension, and diabetes mellitus. Int Urol Nephrol 2018; 50: 1453–1466.
- 7. Qi J, You T, Li J, et al. Circulating trimethylamine N‐oxide and the risk of cardiovascular diseases: a systematic review and meta‐analysis of 11 prospective cohort studies. J Cell Mol Med 2018; 22: 185–194.
- 8. Schiattarella GG, Sannino A, Toscano E, et al. Gut microbe‐generated metabolite trimethylamine‐N-oxide as cardiovascular risk biomarker: a systematic review and dose‐response meta‐analysis. Eur Heart J 2017; 38: 2948–2956.
- 9. Heianza Y, Ma W, Manson JE, et al. Gut microbiota metabolites and risk of major adverse cardiovascular disease events and death: a systematic review and meta‐analysis of prospective studies. J Am Heart Assoc 2017; 6: e004947.
- 10. Tang WH, Hazen SL. Microbiome, trimethylamine N‐oxide, and cardiometabolic disease. Transl Res 2017; 179: 108–115.
- 11. Tang WHW, Wang Z, Fan Y, et al. Prognostic value of elevated levels of intestinal microbe‐generated metabolite trimethylamine‐N‐oxide in patients with heart failure: refining the gut hypothesis. J Am Coll Cardiol 2014; 64: 1908–1914.
- 12. Tang WHW, Wang Z, Shrestha K, et al. Intestinal microbiota‐dependent phosphatidylcholine metabolites, diastolic dysfunction, and adverse clinical outcomes in chronic systolic heart failure. J Card Fail 2015; 21: 91–96.
- 13. Trøseid M, Ueland T, Hov JR, et al. Microbiota‐dependent metabolite trimethylamine‐N-oxide is associated with disease severity and survival of patients with chronic heart failure. J Intern Med 2015; 277: 717–726.
- 14. Suzuki T, Heaney LM, Bhandari SS, et al. Trimethylamine N‐oxide and prognosis in acute heart failure. Heart 2016; 102: 841–848.
- 15. Schuett K, Kleber ME, Scharnagl H, et al. Trimethylamine‐N-oxide and heart failure with reduced versus preserved ejection fraction. J Am Coll Cardiol 2017; 70: 3202–3204.
- 16. Suzuki T, Yazaki Y, Voors AA, et al. Association with outcomes and response to treatment of trimethylamine N‐oxide in heart failure: results from BIOSTAT‐CHF. Eur J Heart Fail 2019; 21: 877–886.
- 17. Salzano A, Israr MZ, Yazaki Y, et al. Combined use of trimethylamine N‐oxide with BNP for risk stratification in heart failure with preserved ejection fraction: findings from the DIAMONDHFpEF study. Eur J Prev Cardiol 2019; https://doi.org/10.1177/2047487319870355. [online ahead of print].
- 18. Stroup DF, Berlin JA, Morton SC, et al. Meta‐analysis of observational studies in epidemiology: a proposal for reporting. Meta‐analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000; 283: 2008–2012.
- 19. Wells GA, Shea B, O'Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta‐analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (viewed Oct 2019).
- 20. Chowdhury R, Stevens S, Gorman D, et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: systematic review and meta‐analysis. BMJ 2012; 345: e6698.
- 21. Huang Y, Cai X, Mai W, et al. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta‐analysis. BMJ 2016; 355: i5953.
- 22. Pasini E, Aquilani R, Testa C, et al. Pathogenic gut flora in patients with chronic heart failure. JACC Heart Fail 2016; 4: 220–227.
- 23. Cui X, Ye L, Li J, et al. Metagenomic and metabolomic analyses unveil dysbiosis of gut microbiota in chronic heart failure patients. Sci Rep 2018; 8: 635.
- 24. An D, Zhan Q, Bai Y, et al. The clinical significance of serum trimethylamine N‐oxide (TMAO) level in patients with chronic heart failure [abstract]. J Am Coll Cardiol 2017; 70: C145.
- 25. Tomlinson J, Wheeler DC. The role of trimethylamine N‐oxide as a mediator of cardiovascular complications in chronic kidney disease. Kidney Int 2017; 92: 809–815.
- 26. Organ CL, Otsuka H, Bhushan S, et al. Choline diet and its gut microbe‐derived metabolite, trimethylamine N‐oxide, exacerbate pressure overload‐induced heart failure. Circ Heart Fail 2016; 9: e002314.
- 27. Koeth RA, Levison BS, Culley MK, et al. γ‐Butyrobetaine is a proatherogenic intermediate in gut microbial metabolism of L‐carnitine to TMAO. Cell Metab 2014; 20: 799–812.
- 28. Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011; 472: 57–63.
- 29. Livshits G, Kalinkovich A. Inflammaging as a common ground for the development and maintenance of sarcopenia, obesity, cardiomyopathy and dysbiosis. Ageing Res Rev 2019; 56: 100980.
- 30. Kitai T, Kirsop J, Tang WH. Exploring the microbiome in heart failure. Curr Heart Fail Rep 2016; 13: 103–109.
- 31. Kumemoto R, Yusa K, Shibayama T, Hatori K. Trimethylamine N‐oxide suppresses the activity of the actomyosin motor. Biochim Biophys Acta 2012; 1820: 1597–1604.
- 32. Makrecka‐Kuka M, Volska K, Antone U, et al. Trimethylamine N‐oxide impairs pyruvate and fatty acid oxidation in cardiac mitochondria. Toxicol Lett 2017; 267: 32–38.
- 33. Tang WH, Kitai T, Hazen SL. Gut microbiota in cardiovascular health and disease. Circ Res 2017; 120: 1183–1196.
- 34. Chioncel O, Ambrosy AP. Trimethylamine N‐oxide and risk of heart failure progression: marker or mediator of disease. Eur J Heart Fail 2019; 21: 887–890.
- 35. Cho CE, Taesuwan S, Malysheva OV, et al. Trimethylamine‐N‐oxide (TMAO) response to animal source foods varies among healthy young men and is influenced by their gut microbiota composition: a randomized controlled trial. Mol Nutr Food Res 2017; 61: 1600324.
- 36. Mayerhofer C, Awoyemi AO, Moscavitch SD, et al. Design of the GutHeart — targeting gut microbiota to treat heart failure — trial: a Phase II, randomized clinical trial. ESC Heart Fail 2018; 5: 977–984.
- 37. Abbasi J. TMAO and heart disease: the new red meat risk? JAMA 2019; 321: 2149–2151.
- 38. Cui X, Ye L, Li J, et al. Metagenomic and metabolomic analyses unveil dysbiosis of gut microbiota in chronic heart failure patients. Sci Rep 2018; 8: 635.
- 39. Ponikowski P, Voors AA, Anker SD, et al. ESC Scientific Document Group. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 2129–2200.





Abstract
Objective: Gut microbiota‐produced trimethylamine N‐oxide (TMAO) is a risk factor for cardiovascular events. However, conflicting findings regarding the link between plasma TMAO level and prognosis for patients with heart failure have been reported. We examined the association of plasma TMAO concentration with risk of major adverse cardiac events (MACEs) and all‐cause mortality in patients with heart failure.
Study design: Meta‐analysis of prospective clinical studies.
Data sources: We searched electronic databases (PubMed, EMBASE) for published prospective studies examining associations between plasma TMAO level and MACEs and all‐cause mortality in adults with heart failure.
Data synthesis: Hazard ratios (HRs) with 95% confidence intervals for associations between TMAO level and outcomes were estimated in random effects models. In seven eligible studies including a total of 6879 patients (median follow‐up, 5.0 years) and adjusted for multiple risk factors, higher plasma TMAO level was associated with greater risks of MACEs (TMAO tertile 3 v tertile 1: HR, 1.68; 95% CI, 1.44–1.96; per SD increment: HR, 1.26; 95% CI, 1.18–1.36) and of all‐cause mortality (TMAO tertile 3 v tertile 1: HR, 1.67; 95% CI, 1.17–2.38; per SD increment: HR, 1.26; 95% CI, 1.07–1.48). Higher TMAO level was also associated with greater risk of MACEs after adjusting for estimated glomerular filtration rate (eGFR; six studies included); however, the heterogeneity of studies in which risk was adjusted for eGFR was significant (I2 = 76%).
Conclusions: Elevated plasma TMAO level in patients with heart failure is associated with poorer prognoses. This association is only partially mediated by renal dysfunction.