The global pandemic of coronavirus disease 2019 (COVID‐19) — caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) — has caused widespread disruption to health care systems and the wider society. Some high income countries have sustained large numbers of infections and high mortality rates. Australia and New Zealand have fared considerably better; this is thought to be due to early border control and quarantine measures, contact tracing, and strict social restrictions, which have begun to be relaxed.1
Experience from previous coronavirus outbreaks — notably severe acute respiratory syndrome (SARS) in 2003 — suggests that health care workers are at considerable risk of acquiring infection, particularly when involved in aerosol generating critical care procedures.2,3,4 This risk appears more pronounced with COVID‐19, with reports of personal protective equipment (PPE) shortages and fatalities of health care workers in other countries.5
In emergency departments (EDs), the traditional approach of rushing to a critically ill patient's side to provide life‐saving resuscitation must now be balanced with the risk of acquiring a potentially fatal illness.6,7 This highlights an ethical tension between the duty to treat and a health care worker's right to protection.8
Methods
In March 2020, clinical guidelines on many aspects of the ED response to COVID‐19 were produced by a team of emergency physicians and by staff of the Australasian College for Emergency Medicine (ACEM) working in collaboration with Safer Care Victoria.9 An expert group developed guidelines on the management of cardiac arrest, based on a review of the emerging literature related to COVID‐19 and guidance from national and international resuscitation bodies, including the Australian and New Zealand Committee on Resuscitation,10 the New Zealand Resuscitation Council,11 the United Kingdom Resuscitation Council,12,13 the International Liaison Committee on Resuscitation (ILCOR),14 and the American Heart Association.15
This consensus statement also aligns with other local critical care guidelines for the management of COVID‐19, including the Safe Airway Society16 and the Australian and New Zealand Intensive Care Society guidelines.17 These other guidelines provide specific detailed advice on airway management and tracheal intubation, which are not reproduced in this document.
In the setting of low community transmission, cardiac arrest is very unlikely to be due to COVID‐19. Although the risk posed to health care workers is very small, a number of considerations exist. These include acknowledging that early defibrillation and chest compressions save lives, balancing the appropriateness of resuscitation against the risk of health care worker infection, and appropriate use of personal protective equipment (PPE). In addition, if widespread COVID‐19 infections affect hospital resource availability, the ethics of resource allocation must be considered.
Most recommendations in this document are based on low certainty evidence. We have applied standard resuscitation principles and substantially rely on expert opinion. Similar to other COVID‐19 guidelines, as knowledge develops during the pandemic, recommendations may change and this consensus statement will need to be updated. However, at the time of writing (17th June 2020), it is believed that these recommendations are safe and appropriate for use in pre‐hospital and emergency care systems during the current COVID‐19 pandemic.
Appropriateness of resuscitation
Ethical consideration of the appropriateness of resuscitation should balance:
- individuals’ goals of care and requests for limitations on measures to prolong life — these should be clarified early for all patients admitted to hospital or at risk of requiring hospital admission; this is a shared responsibility of community‐ and hospital‐based clinicians;
- the likelihood that the patient will benefit from treatment;
- the potential for such treatment to limit capacity to offer treatment to other patients with an imperative for fair resource allocation; and
- the potential of such treatments to cause harm, including harm to other patients (by diverting staff from attending to other patients who then deteriorate) and staff (through transmission of infection).
A variety of resources are available to assist patients and clinicians in discussions regarding treatment limitations and end‐of‐life decisions. ACEM's broader clinical guidelines include specific recommendations for establishing treatment goals in the context of COVID‐19 (Box 1).9 To ensure appropriate and evidence‐based care for the dying, palliative care pathways should be used for patients when resuscitation is deemed inappropriate.
If the health system becomes overwhelmed, resource‐based decision making regarding the care of individual patients may be required. Discussions should occur at jurisdictional level, including with medical regulators, to ensure that decisions are made fairly, and according to ethical principles.
Systems to recognise clinical deterioration and prevent cardiorespiratory arrest due to progression of severe illness are also important within the community, in the ED and in hospital.
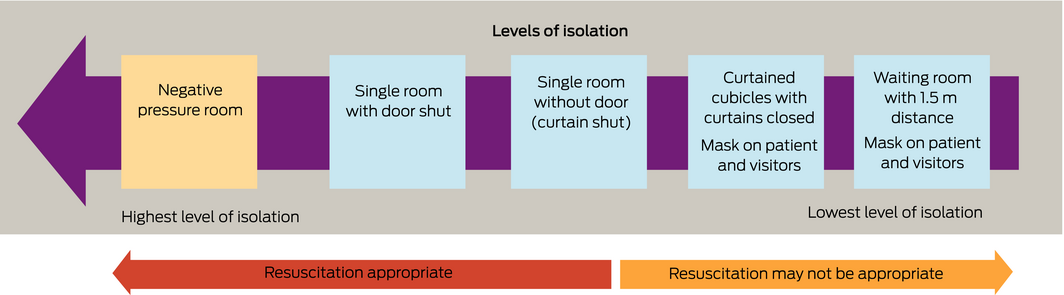
In the event that resuscitation is required, a number of factors should be considered, including goals of care or advance care directives, community prevalence of COVID‐19, adequacy of staff protection (PPE), the availability of an appropriate resuscitation setting (single or negative pressure room) that limits infection risk, and the likelihood of successful resuscitation with good neurological outcome.
Infection control and aerosol generating procedures in the context of resuscitation
During periods when there is sustained community transmission of SARS‐CoV‐2 and no significant population immunity (either naturally or vaccine‐acquired), there will be times when it is reasonable to assume that in the first instance, all undifferentiated critically ill patients are infected with SARS‐CoV‐2.
On the other hand, if rates of community transmission are extremely low, local health department advice may be that specific precautions against COVID‐19 are no longer necessary for critically ill patients.
SARS‐CoV‐2 is primarily transmitted through droplets. This type of transmission occurs when infectious droplets contact the conjunctiva or mucosal surfaces of the upper respiratory tract, either directly transmitted from a cough or sneeze or by contact with a surface where droplets have deposited. The use of droplet and contact PPE (ie, gown or apron, surgical mask, gloves and eye protection) reduces the risk of transmission, as it provides a physical barrier between the droplets and the portal of entry,18 and is recommended in most settings to prevent the transmission of SARS‐CoV‐2.19
Airborne transmission of SARS‐CoV‐2 may occur if there is generation of aerosols during specific procedures, such as intubation and non‐invasive ventilation.19 These aerosol generating procedures are hypothesised to result in an infectious aerosol beyond that which would normally be released by coughing, sneezing or breathing.20 This aerosol may remain suspended in the air for a period and can be inhaled, leading to health care worker infection. Airborne (gown, N95 [or P2] mask, gloves and eye protection) and contact PPE is recommended for health care workers conducting aerosol generating procedures in patients with confirmed or suspected COVID‐19.
Box 2 provides a summary of the minimum recommended PPE for various interventions and procedures associated with resuscitation. Some patients will have been assessed as low risk for COVID‐19 before deterioration and will not require droplet precautions for initial resuscitation steps. However, other patients will either be at high risk for COVID‐19 or their risk will be unable to be determined.
There is active debate and ongoing research regarding the extent to which resuscitative procedures are considered to be aerosol generating. At the time of writing, defibrillation is not considered an aerosol generating procedure, with a recent ILCOR systematic review finding no evidence that defibrillation generates aerosols.21
Compression‐only cardiopulmonary resuscitation (CPR) has recently been assessed by the UK New and Emerging Respiratory Virus Threats Advisory Group22 and the Australian Department of Health23 and is not considered an aerosol generating procedure by either body. ILCOR suggests — through a weak recommendation based on very low certainty evidence — that chest compressions have the potential to generate aerosols.21
Current Australian Government recommendations for paramedics and ambulance first responders suggest that it is reasonable to commence compression‐only CPR with eye protection, gloves and a surgical mask (or with a fit‐checked N95 [or P2] mask if available).24 All other resuscitative procedures are considered to be aerosol generating and should be performed by health care workers wearing airborne PPE. However, these recommendations are based on weak evidence, and further research may lead to changes in advice. We have taken a deliberately conservative approach, in line with various resuscitation organisations.10,11,12,15,16,19,25
The level of PPE dictates which interventions may be safely provided by health care workers. A staff member should be specifically assigned as a “spotter” to ensure safe PPE use by all staff participating in resuscitation. Attention should be paid to mask fit for staff members wearing airborne PPE and to supervising appropriate donning and doffing.
Senior oversight and expertise should be used to minimise the number of people involved in resuscitation. In situ simulation may be helpful for ED staff to become familiar with the roles and practical challenges of a smaller resuscitation team.
Optimal setting for resuscitation
Cardiac arrests do not always occur in a convenient location. In hospital, a collapse may occur in a waiting room, a bathroom, a corridor or in a patient cubicle. Traditionally, resuscitation occurs in a large, open ED resuscitation cubicle.
A single negative pressure room is the most appropriate location for aerosol generating procedures (Box 3), and the patient should be moved to one as soon as practicable. However, resuscitation should not be withheld if a single room is not immediately available.
Changes in the management of cardiac arrest
Modifications to existing advanced life support protocols are necessary. These are discussed below in the context of the DRSABC (Danger, Response, Send for help, Airway, Breathing, Circulation) approach. It should be emphasised that all standard resuscitation interventions are still appropriate but need to be performed by staff wearing adequate PPE.
Danger
Ideally, all resuscitation should be performed by health care workers in PPE suitable for aerosol generating procedures. However, it is recognised that this may not be possible for first responders.
Based on the available evidence, we recommend that first responders should be wearing at least a surgical mask, eye protection and gloves. If the patient is suspected or known to have COVID‐19, first responders should be wearing droplet PPE.
- The patient's mouth and nose should be covered by an oxygen mask (if available) with flow of up to 10 L/min. Additional protection against droplet or spray contamination is recommended, and can be achieved by covering the oxygen mask with a towel, cloth, surgical mask or clear plastic sheet.11 If a view of the mouth and nose is obscured, regularly check the patient's airway for vomit or secretions.
- A staff member wearing a minimum of gloves, eye protection and surgical face mask should immediately place defibrillation pads on the chest, check the cardiac rhythm, and defibrillate the patient if they are in a shockable rhythm.
- Compression‐only CPR (with the face covered) should be instituted rapidly by the first available staff member wearing a minimum of gloves, eye protection and a surgical mask (or N95 [or P2] mask if available). It is reasonable for compression‐only CPR to commence outside and en route to a single room (eg, in a corridor or waiting room).
- Further resuscitation (ongoing chest compressions, assisted ventilation and advanced airway manoeuvres) should be carried out in an appropriate space by staff in airborne PPE who should take over resuscitation as soon as possible. Any rescuers not wearing airborne PPE should leave the area, remove their PPE and perform careful hand hygiene.
Response and send for help
If the patient is unresponsive and not breathing normally, then resuscitation may be necessary. Call for help. Ensure that all clinicians are wearing appropriate PPE.
Airway and breathing
Listening or feeling for breathing should not occur. Instead, place a hand on the patient's chest to feel for chest rise and fall while assessing for normal breathing.
Place a standard oxygen mask (eg, Hudson mask) on the patient and open their airway with a head tilt/chin lift. Do not attempt to clear the airway using any other methods. Suctioning of the oropharynx should not occur through an open suction device (ie, Yankauer sucker) until the patient is in an appropriate location with staff using airborne PPE.
Provide passive oxygen at a flow rate of 10 L/min. Do not provide positive pressure ventilation until the patient is in an appropriate physical location and staff are wearing airborne PPE. An appropriate heat and moisture exchanger filter must be connected to any positive pressure oxygen delivery device as close to the patient as possible. Take care to ensure that all connections are secure.
Bag mask ventilation should be minimised. If required, use two hands to hold the mask. Compressions should be paused, and the bag should be squeezed by a second rescuer at a compression to ventilation ratio of 30:2.21 Compressions should also be paused before placing an advanced airway.
If ongoing ventilation is required, a well fitted supraglottic airway device is preferred to a face mask, as it is thought to reduce the risk of aerosols.16 This should be connected to an appropriate filter, and then to a Mapleson circuit (“anaesthetic bag”) or a standard self‐inflating bag.
A Mapleson circuit is preferred due to the ability to provide passive oxygen flow without the need to deliver positive pressure ventilation. If using a Mapleson circuit, connect the circuit to the oxygen but do not squeeze the bag.
If using a standard self‐inflating bag, monitor the movement of the reservoir bag. If oxygen is being delivered, then do not squeeze the bag. However, in the absence of respiratory effort, oxygen may not be delivered due to the valve mechanism of a standard self‐inflating bag and gentle squeezing of the bag may be required.
If possible, positive pressure ventilation should only be delivered once an endotracheal tube has been inserted in the trachea, the cuff has been inflated, a heat and moisture exchanger filter connected, and correct placement confirmed.
Suctioning through an endotracheal tube should occur through a closed inline system, in the highest level of isolation available and by a health care worker wearing airborne PPE.
Circulation
Rapid rhythm assessment and defibrillation should be prioritised.
Until endotracheal intubation has occurred, compression‐only CPR is recommended. However, if positive pressure ventilation is required, then compressions should be paused to allow ventilation while using a mask or supraglottic airway.12
Mechanical CPR devices should be used when available and staff are adequately trained in their use. These devices may be useful to reduce the number of health care workers present during resuscitation.
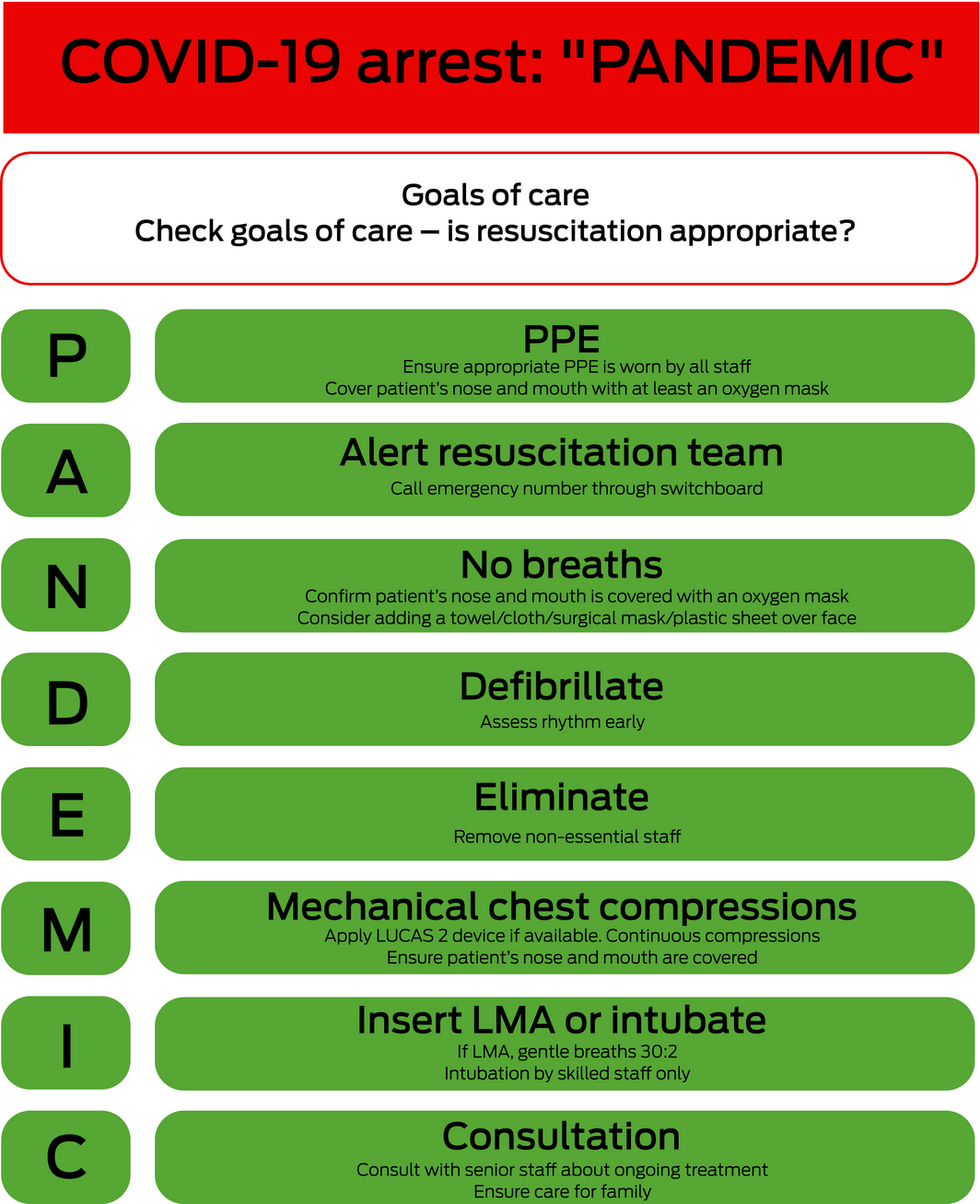
Modified resuscitation algorithm
The algorithm for adult advanced life support presented in Box 4 has been adapted from the New Zealand Resuscitation Council algorithm. An approach to the initial steps of resuscitation is presented in Box 5.
Monitoring of resuscitation
Apart from minimising the number of people in the room, resuscitation should occur according to established protocols. Waveform capnography should be used. Focused cardiac ultrasound may be useful to guide resuscitation efforts.
Advanced resuscitation techniques
Advanced resuscitation techniques such as extracorporeal life support should be carefully considered and only used in exceptional circumstances for currently accepted indications (eg, massive pulmonary embolism, or specific toxicological emergencies). Provision of such interventions should include assessment of the potential benefit to the patient, resources required, and the potential associated diversion of resources from others for delivery of such treatments.
In the setting of a cardiac arrest in the ED from presumed COVID‐19, escalation to extracorporeal life support is not currently recommended due to a high likelihood of futility. However, as the evidence matures, this recommendation may change.
Post‐resuscitation care
If return of spontaneous circulation is achieved before intubation, assess the need for and potential benefit of intubation in the context of the individual's goals of care.
If mechanical ventilation is required, clamp the endotracheal tube before disconnecting from the patient. Ensure a closed inline suction system is connected.
At the end of resuscitation attempts, everyone should remove the PPE carefully and perform hand hygiene. It is recommended that staff observe each other while removing PPE to monitor for possible breaches in infection control procedures.
Equipment should be cleaned, disinfected or disposed of according to hospital protocols.
A post‐resuscitation debrief should address clinical care and decision making, communication, PPE, and prevention of COVID‐19 transmission. Any breaches of PPE should be documented, reported and followed up according to local protocols. Maintain a log of staff attending the resuscitation to facilitate appropriate infection control follow‐up if required.
Termination of resuscitation
Decisions regarding resuscitation termination should be made according to currently accepted standards. A cardiac arrest in a patient with COVID‐19 infection and respiratory failure should prompt rapid assessment and treatment of potentially reversible causes. If no such cause is identified, clinicians should give early consideration to futility of ongoing resuscitation.26
Care for family members
During the COVID‐19 pandemic, family members are likely to be restricted from entering resuscitation rooms, apart from exceptional circumstances (eg, paediatric cardiac arrest).
Unsuccessful resuscitation
If resuscitation is unsuccessful, family members may be allowed to view the body — according to local hospital policies and infection control measures. However, restrictions in place due to COVID‐19 may significantly disrupt usual grieving processes; for example, not being allowed to touch or kiss the deceased.27 If required, social work support should be provided to family members in a safe location or via telehealth where COVID‐19 precludes visitation. Appropriate PPE should be used by staff when preparing the body for the mortuary.
Training and simulation
The changes outlined above require a significant adaptation for many doctors, nurses and paramedics. All health care workers should have regular PPE and advanced life support training, be able to access in situ simulation sessions, and receive extensive debriefing after actual resuscitations. This will ensure safe, timely and effective management of the patient with cardiac arrest in the COVID‐19 era.
Conclusion
Although infection risks posed by COVID‐19 influence all aspects of adult cardiac arrest management, the basic principles of resuscitation remain the same. Prioritisation of rapid defibrillation and attention to reversible causes of cardiac arrest remain critical interventions. Modifications to traditional approaches include a greater emphasis on the safety of health care workers and on the use of adequate PPE. Future updates to this document will be available at www.acem.org.au/covid-19.
Endorsement
This consensus statement is endorsed by ACEM and the Safe Airway Society.
Box 1 – An ethical framework for establishing treatment goals in the context of coronavirus disease 2019 (COVID‐19)*
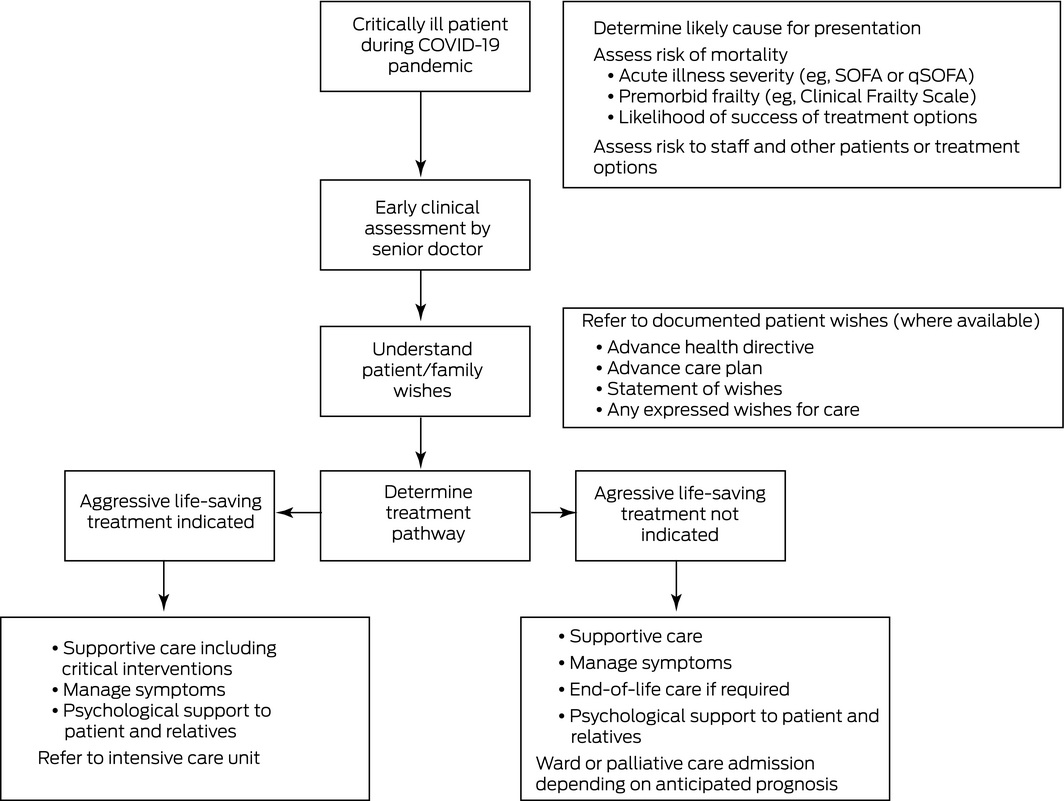
qSOFA = quick SOFA; SOFA = Sequential Organ Failure Assessment. * Source: Adapted from Australasian College for Emergency Medicine,9 with permission.
Box 2 – Summary of minimum personal protective equipment (PPE) for various resuscitation procedures
|
|
Surgical mask,* eye protection and gloves |
Droplet PPE† |
Airborne PPE‡ |
||||||||||||
|
|
|||||||||||||||
|
First responder (recognise cardiac arrest and send for help) |
✔ |
✔ |
|
||||||||||||
|
Low risk for COVID‐19 or unable to assess risk |
High risk for COVID‐19 |
|
|||||||||||||
|
Oxygen mask (up to 10 L/min) on patient, covered with towel, cloth, clear plastic sheet or surgical mask |
✔ |
✔ |
|
||||||||||||
|
Low risk for COVID‐19 or unable to assess risk |
High risk for COVID‐19 |
|
|||||||||||||
|
Defibrillation (with patient's face covered) |
✔ |
✔ |
|
||||||||||||
|
Low risk for COVID‐19 or unable to assess risk |
High risk for COVID‐19 |
|
|||||||||||||
|
Initial (first responder) compression‐only CPR while awaiting staff in airborne PPE |
✔ |
✔ |
|
||||||||||||
|
Low risk for COVID‐19 or unable to assess risk |
High risk for COVID‐19 |
|
|||||||||||||
|
Basic airway manoeuvres (chin lift/head tilt/jaw thrust) |
✔ |
✔ |
|
||||||||||||
|
Low risk for COVID‐19 or unable to assess risk |
High risk for COVID‐19 |
|
|||||||||||||
|
Ongoing chest compressions during CPR |
✔ |
|
✔ |
||||||||||||
|
Low risk for COVID‐19 |
|
High risk for COVID‐19 or unable to assess risk |
|||||||||||||
|
Oropharyngeal/nasopharyngeal airway |
✔ |
|
✔ |
||||||||||||
|
Low risk for COVID‐19 |
|
High risk for COVID‐19 or unable to assess risk |
|||||||||||||
|
Bag mask ventilation |
✔ |
|
✔ |
||||||||||||
|
Low risk for COVID‐19 |
|
High risk for COVID‐19 or unable to assess risk |
|||||||||||||
|
Supraglottic airway |
✔ |
|
✔ |
||||||||||||
|
Low risk for COVID‐19 |
|
High risk for COVID‐19 or unable to assess risk |
|||||||||||||
|
Intubation |
✔ |
|
✔ |
||||||||||||
|
Low risk for COVID‐19 |
|
High risk for COVID‐19 or unable to assess risk |
|||||||||||||
|
|
|||||||||||||||
|
COVID‐19 = coronavirus disease 2019; CPR = cardiopulmonary resuscitation. * Or N95 (or P2) mask if available. † Surgical mask, eye protection, gloves, gown/apron. ‡ N95 (or P2) mask, eye protection, gloves, gown/apron, visor, hat and neck protection as per local guidelines. |
|||||||||||||||
Box 4 – Suggested algorithm for adult advanced life support in the coronavirus disease 2019 (COVID‐19) era
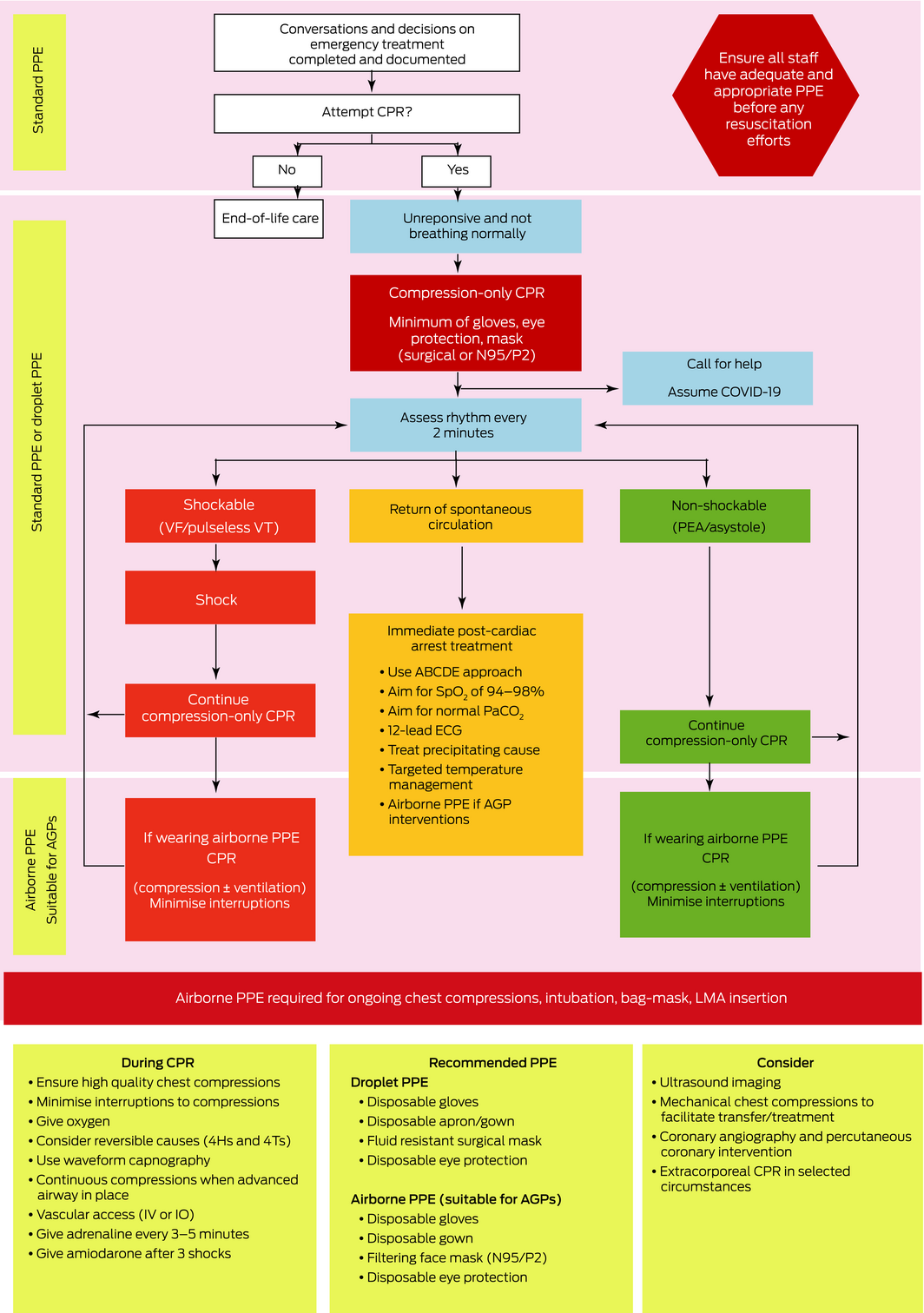
4 Hs = Hypoxia (low levels of oxygen), Hypovolaemia (shock), Hyperkalaemia/hypokalaemia/hypoglycaemia/hypocalcaemia (plus other metabolic disturbances), Hypothermia; 4 Ts = Tension pneumothorax, Tamponade, Thrombosis, Toxins; ABCDE = Airway, Breathing, Circulation, Disability, Exposure; AGP = aerosol generating procedure; CPR = cardiopulmonary resuscitation; ECG = electrocardiogram; IO = intraoral; IV = intravenous; LMA = laryngeal mask airway; PAco2 = arterial partial pressure of carbon dioxide; PEA = pulseless electrical activity; PPE = personal protective equipment; Spo2 = oxygen saturation measured by pulse oximetry; VF = ventricular fibrillation; VT = ventricular tachycardia. Source: Adapted, with permission, from the New Zealand Resuscitation Council.11
Provenance: Not commissioned; externally peer reviewed.
- Simon Craig1,2
- Mya Cubitt3,4
- Ashish Jaison5
- Steven Troupakis1,6
- Natalie Hood1,7
- Christina Fong1,6
- Adnan Bilgrami1
- Peter Leman8,9
- Juan Carlos Ascencio‐Lane10,11
- Guruprasad Nagaraj12,13
- John Bonning14,15
- Gabriel Blecher2,16
- Rob Mitchell2,5
- Ellen Burkett17,18
- Sally M McCarthy13,19
- Amanda M Rojek3,20
- Kim Hansen21,22
- Helen Psihogios1
- Peter Allely9,23
- Simon Judkins24
- Lai Heng Foong25,26
- Stephen Bernard27
- Peter A Cameron2,5
- 1 Monash Health, Melbourne, VIC
- 2 Monash University, Melbourne, VIC
- 3 Royal Melbourne Hospital, Melbourne, VIC
- 4 Centre for Integrated Critical Care, University of Melbourne, Melbourne, VIC
- 5 Emergency and Trauma Centre, Alfred Health, Melbourne, VIC
- 6 Epworth HealthCare, Melbourne, VIC
- 7 Surf Life Saving Australia, Sydney, NSW
- 8 Fiona Stanley Hospital, Perth, WA
- 9 University of Western Australia, Perth, WA
- 10 Royal Hobart Hospital, Hobart, TAS
- 11 University of Tasmania, Hobart, TAS
- 12 South Western Emergency Research Institute, Liverpool Hospital, Sydney, NSW
- 13 University of New South Wales, Sydney, NSW
- 14 Australasian College for Emergency Medicine, Melbourne, VIC
- 15 Council of Medical Colleges of Aotearoa New Zealand, Wellington, New Zealand
- 16 Monash Medical Centre, Melbourne, VIC
- 17 Princess Alexandra Hospital, Brisbane, QLD
- 18 Clinical Excellence Queensland, Brisbane, QLD
- 19 Prince of Wales Hospital and Community Health Services, Sydney, NSW
- 20 Centre for Integrated Critical Care, University of Melbourne, Melbourne, VIC
- 21 St Andrew's War Memorial Hospital, Brisbane, QLD
- 22 Prince Charles Hospital, Brisbane, QLD
- 23 Sir Charles Gairdner Hospital, Perth, WA
- 24 Austin Hospital, Melbourne, VIC
- 25 Bankstown–Lidcombe Hospital, Sydney, NSW
- 26 University of Western Sydney, Sydney, NSW
- 27 Centre for Research and Evaluation, Ambulance Victoria, Melbourne, VIC
The authors would like to acknowledge the assistance of the following ACEM staff in the production of this consensus statement: Robert Lee, Nicola Ballenden, Andrea Johnston and Belinda Rule.
No relevant disclosures.
- 1. Falconer R. Australia and New Zealand reopen after coronavirus cases plummet. Axios News 2020; 14 May. https://www.axios.com/coronavirus-australia-new-zealand-reopen-lockdown-3da28be5-1526-4790-a44a-a25c63dc0895.html (viewed May 2020).
- 2. Chan‐Yeung M. Severe acute respiratory syndrome (SARS) and healthcare workers. Int J Occup Environ Health 2004; 10: 421–427.
- 3. Christian MD, Loutfy M, McDonald LC, et al. Possible SARS coronavirus transmission during cardiopulmonary resuscitation. Emerg Infect Dis 2004; 10: 287–293.
- 4. Loeb M, McGeer A, Henry B, et al. SARS among critical care nurses, Toronto. Emerg Infect Dis 2004; 10: 251–255.
- 5. Wang J, Zhou M, Liu F. Reasons for healthcare workers infected with novel coronavirus disease 2019 (COVID‐19) in China. J Hosp Infect 2020; 105: 100–101.
- 6. Fritz Z, Perkins GD. Cardiopulmonary resuscitation after hospital admission with COVID‐19. BMJ 2020; 369: m1387.
- 7. Mahase E, Kmietowicz Z. covid‐19: doctors are told not to perform CPR on patients in cardiac arrest. BMJ 2020; 368: m1282.
- 8. Markwell A, Mitchell R, Wright A, Brown AF. Clinical and ethical challenges for emergency departments during communicable disease outbreaks: can lessons from Ebola virus disease be applied to the COVID‐19 pandemic? Emerg Med Australas 2020; 32: 520–524.
- 9. Australasian College for Emergency Medicine. Clinical guidelines for the management of COVID‐19 in Australasian emergency departments, version 4.0. Updated June 2020. https://acem.org.au/Content-Sources/Advancing-Emergency-Medicine/COVID-19/Resources/Clinical-Guidelines (viewed July 2020).
- 10. Australian and New Zealand Committee on Resuscitation. Resuscitation during the COVID‐19 pandemic (updated Apr 2020). Australian Resuscitation Council, 2020. https://resus.org.au/ (viewed Apr 2020).
- 11. New Zealand Resuscitation Council. COVID‐19 modifications to essential life support (updated Mar 2020). https://www.nzrc.org.nz/assets/Guidelines/COVID-19/2020-03-27-Temporary-Guideline-in-State-of-EmergencyFINAL.pdf (viewed Apr 2020).
- 12. Resuscitation Council UK. Resuscitation Council UK statement on COVID‐19 in relation to CPR and resuscitation in acute hospital settings (updated Apr 2020). https://www.resus.org.uk/media/statements/resuscitation-council-uk-statements-on-covid-19-coronavirus-cpr-and-resuscitation/covid-healthcare/ (viewed Apr 2020).
- 13. Resuscitation Council UK. Guidance for the resuscitation of adult COVID‐19 patients in acute hospital settings, version 4 (updated Apr 2020). https://www.resus.org.uk/media/statements/resuscitation-council-uk-statements-on-covid-19-coronavirus-cpr-and-resuscitation/covid-healthcare/ (viewed Apr 2020).
- 14. Couper K, Taylor‐Phillips S, Grove A, et al; International Liaison Committee on Resuscitation. Consensus on Science with Treatment Recommendations (CoSTR). COVID‐19 infection risk to rescuers from patients in cardiac arrest (updated Apr 2020.). Brussels: International Liaison Committee on Resuscitation, 2020. https://costr.ilcor.org/document/covid-19-infection-risk-to-rescuers-from-patients-in-cardiac-arrest (viewed Apr 2020).
- 15. Edelson DP, Sasson C, Chan PS, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID‐19: from the Emergency Cardiovascular Care Committee and Get with the Guidelines‐Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation. 2020; 141: e933–e943.
- 16. Brewster DJ, Chrimes N, Do TB, et al. Consensus statement: Safe Airway Society principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group. Med J Aust 2020; 212: 472–481. https://www.mja.com.au/journal/2020/212/10/consensus-statement-safe-airway-society-principles-airway-management-and-0
- 17. Australian and New Zealand Intensive Care Society. ANZICS COVID‐19 guidelines. Melbourne: ANZICS, 2020. https://www.anzics.com.au/coronavirus-guidelines/ (viewed Apr 2020).
- 18. Siegel JD, Rhinehart E, Jackson M, Chiarello L; Healthcare Infection Control Practices Advisory Committee. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings (updated July 2019). https://www.cdc.gov/infectioncontrol/pdf/guidelines/isolation-guidelines-H.pdf (viewed June 2020).
- 19. World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID‐19): interim guidance; 27 Feb 2020. https://apps.who.int/iris/handle/10665/331215 (viewed Apr 2020).
- 20. Davies A, Thomson G, Walker J, et al. A review of the risks and disease transmission associated with aerosol generating medical procedures. J Infect Prev 2009; 10: 122–126.
- 21. International Liaison Committee on Resuscitation. COVID‐19: practical guidance for implementation (updated Apr 2020). https://www.ilcor.org/covid-19 (viewed Apr 2020).
- 22. Public Health England. PHE statement regarding NERVTAG review and consensus on cardiopulmonary resuscitation as an aerosol generating procedure (AGP); 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/phe-statement-regarding-nervtag-review-and-consensus-on-cardiopulmonary-resuscitation-as-an-aerosol-generating-procedure-agp (viewed May 2020).
- 23. Australian Government, Department of Health. Guidance on the use of personal protective equipment (PPE) in hospitals during the COVID‐19 outbreak. https://www.health.gov.au/resources/publications/guidance-on-the-use-of-personal-protective-equipment-ppe-in-hospitals-during-the-covid-19-outbreak (viewed May 2020).
- 24. Australian Government, Department of Health. Coronavirus Disease (COVID‐19): information for paramedics and ambulance first responders. https://www.health.gov.au/resources/publications/coronavirus-covid-19-information-for-paramedics-and-ambulance-first-responders (viewed May2020).
- 25. World Federation of Societies of Anaesthesiologists. Coronavirus — guidance for anaesthesia and perioperative care providers. WFSA, 2020. https://www.wfsahq.org/resources/coronavirus (viewed Apr 2020).
- 26. Shao F, Xu S, Ma X, et al. In‐hospital cardiac arrest outcomes among patients with COVID‐19 pneumonia in Wuhan, China. Resuscitation 2020; 151: 18–23.
- 27. Department of Health and Human Services. Handling the body of a deceased person with suspected or confirmed COVID‐19. https://www.dhhs.vic.gov.au/guidance-handling-body-deceased-person-suspected-or-confirmed-covid-19 (viewed Apr 2020).





Abstract
Introduction: The global pandemic of coronavirus disease 2019 (COVID‐19) has caused significant worldwide disruption. Although Australia and New Zealand have not been affected as much as some other countries, resuscitation may still pose a risk to health care workers and necessitates a change to our traditional approach. This consensus statement for adult cardiac arrest in the setting of COVID‐19 has been produced by the Australasian College for Emergency Medicine (ACEM) and aligns with national and international recommendations.
Main recommendations:
Changes in management: The changes outlined in this document require a significant adaptation for many doctors, nurses and paramedics. It is critically important that all health care workers have regular PPE and advanced life support training, are able to access in situ simulation sessions, and receive extensive debriefing after actual resuscitations. This will ensure safe, timely and effective management of the patients with cardiac arrest in the COVID‐19 era.