An outbreak in Wuhan, China, in 2019 of the novel coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) (formerly called HCoV‐19) has led to a pandemic of coronavirus disease 2019 (COVID‐19). More than 80% of confirmed cases report a mild febrile illness; however, 14–17% of confirmed cases develop severe COVID‐19 with acute respiratory distress syndrome and 5% also develop septic shock and/or multiple organ dysfunction.1,2,3 Like other patient groups with acute respiratory distress syndrome, patients with severe COVID‐19 are likely to be considered for emergency tracheal intubation and mechanical ventilation to support potential recovery from their illness.
From recent reported data in Wuhan and northern Italy, at least 10% of reported positive COVID‐19 cases require intensive care unit (ICU) admission, with many requiring urgent tracheal intubation for profound and sudden hypoxia.2 As the incidence of SARS‐CoV‐2 infection rises in the community, an increasing number of patients who have mild or asymptomatic disease as an incidental comorbidity, but are nonetheless infective, may still present for urgent surgery.
Risks to health care workers
Transmission of COVID‐19 is primarily through droplet and fomite spread. Droplets are larger particles of body fluid that are affected by gravity within a few seconds and can therefore travel only short distances through the air before landing on surrounding surfaces. Virus‐containing droplets may cause direct transmission from close contact or contribute to contamination of fomites.4 Fomites are surfaces or objects (eg, clothing, equipment, furniture) that can become contaminated by the virus, where it may remain active for hours to days. In contrast, aerosols are composed of much smaller fluid particles that can remain suspended in the air for prolonged periods. If a virus is able to remain stable within aerosolised airway secretions, this increases the risk of transmission. Current evidence suggests that while it is plausible that coronaviruses can survive in aerosol form within fluid particles under certain conditions, this is not the primary mechanism for transmission in the community.5,6,7,8
Some events (Box 1) may lead to aerosolisation of virally contaminated body fluid.9 The process of caring for patients with severe COVID‐19 and performing procedures associated with aerosol‐generating events in this group thus present an increased risk of infection for health care workers.5 During the SARS‐CoV‐1 outbreak in Canada in 2003, half of all the SARS‐CoV‐1 cases were due to nosocomial transmission to health care workers. In addition to the personal health risks to infected health care workers, illness and quarantine procedures may diminish the available resources to manage patients at a time of high demand. COVID‐19 has now been classified as a high consequence infectious disease, emphasising the significant risk to health care workers and the health care system.10
Aerosol‐generating events are those that inevitably involve gas flow, especially high velocity flow (Box 1); they potentially generate aerosols and increase droplet formation. Positive pressure ventilation during non‐invasive ventilation or when using a face mask or supraglottic airway may generate droplets or aerosols, as the seal obtained is usually inferior to that achieved with a correctly placed tracheal tube with its cuff inflated.
In contrast, procedures that are merely vulnerable to aerosol generation (Box 1) do not inevitably involve gas flow. Generation of aerosols from these latter procedures requires occurrence of an aerosol‐generating event. Laryngoscopy, tracheal intubation and bronchoscopy will only cause aerosolisation if coughing is precipitated or another aerosol‐generating procedure is performed. Front‐of‐neck airway may generate aerosols if the patient receives concurrent positive pressure ventilation from above. Many of these precipitating events can therefore be prevented by adequate neuromuscular blockade and avoiding concurrent aerosol‐generating procedures, such that, if performed properly and without complications, they may not generate aerosols.
The process of airway management is a period of increased risk for aerosol‐based transmission for the following reasons:
- the patient may become agitated or combative due to hypoxia;
- the patient's mask must be removed;
- clinicians are near the patient's airway;
- laryngoscopy and intubation are vulnerable to aerosol generation; and
- aerosol‐generating events are more likely.
It is crucial to minimise the risk of aerosol‐generating events during airway management. Box 2 outlines the risk factors for aerosol generation during airway management and associated protective strategies that can be adopted to mitigate them.
Coronaviruses are smaller than the minimum sized particles that most so‐called viral filters and masks are able to remove. However, the particles of respiratory secretions with which coronaviruses are associated when in aerosol form are larger and able to be filtered by these devices. Therefore, in this statement, reference to viral filters or masks refers to their ability to filter aerosolised respiratory secretions that potentially contain the virus, rather than the ability to filter the virus itself.
Non‐invasive ventilation and high flow nasal oxygen therapy
It is beyond the scope of this article to discuss the efficacy of non‐invasive ventilation and high flow nasal oxygen therapy for the treatment of respiratory failure in patients with COVID‐19. We recommend seeking guidance from the current version of the Australian and New Zealand Intensive Care Society (ANZICS) COVID‐19 guidelines.11
However, in order to make the recommendations below, we have considered the risks and benefits of these therapies as an adjunct to tracheal intubation. During the 2003 SARS outbreak, there were reports of significant transmission secondary to non‐invasive ventilation.12 Manikin studies suggest that dispersal of liquid from high flow nasal oxygen at 60 L/min is minimal and significantly less than that caused by coughing and sneezing, providing that nasal cannulae are well fitted.13,14 Nevertheless, the risk to health care workers of aerosolisation remains unclear and will depend on many variables, including flow rates, ventilator pressures, patient coughing and cooperation, and the quality and fit of staff personal protective equipment (PPE).
Until further data become available, it should be assumed that non‐invasive ventilation and high flow nasal oxygen are aerosol‐generating procedures. Patients receiving these therapies should be cared for in airborne isolation rooms and staff should wear close contact aerosol protective PPE (including N95/P2 masks) while in the patient's room.
Methods
This statement was planned on 11 March 2020, when an urgent need for guidance in Australia and New Zealand for both clinical practice and staff preparation for the COVID‐19 pandemic was identified.
The Safe Airway Society board assembled 14 experts from Australia and New Zealand to prepare the statement. They first reviewed the current literature on COVID‐19 relevant to airway practice, as well as relevant publications from the 2003 SARS epidemic. All recommendations were debated extensively. Some of the endorsing societies — ANZICS and the Australian Society of Anaesthetists — were consulted during the development of the document to allow external opinion. The recommendations in this document were primarily guided by expert opinion. It must be acknowledged that only weak evidence was available from the current COVID‐19 pandemic at the time of the statement. Most articles reviewed were either observational data or opinion.
In recent weeks, a small number of articles, guidelines and flow diagrams have appeared to aid the airway management of patients with COVID‐19, based mainly on recent experiences in China, Hong Kong and Italy.15,16 We aim to rapidly distribute clear local recommendations to clinicians in emergency medicine, intensive care, anaesthesia and pre‐hospital care in Australia and New Zealand to guide airway management of the adult COVID‐19 patient group (patients with known or suspected COVID‐19).
Specifically, we aim to:
- recommend routine airway management practices that should also be adopted in patients with COVID‐19;
- recommend principles specific to the airway management practices for patients with COVID‐19;
- recommend standard airway rescue practices that should also be adopted for patients with COVID‐19;
- recommend a consistent but flexible approach to planned airway management practices in the COVID‐19 patient group regardless of their location (pre‐hospital, emergency department [ED], ICU, or operating theatre);
- recommend safe practices for unplanned episodes of airway management (eg, cardiac or respiratory arrest, other resuscitation scenarios) that may arise in any area; and
- seek endorsement and distribution of these guidelines by all relevant Australian and New Zealand societies and specialty colleges with an interest in airway management. A common approach will allow early education and simulation training for all staff. Early education is paramount to improving compliance with the techniques, particularly the use of PPE. A consistent approach will also improve safe and effective clinical practice during episodes of airway management involving collaboration between clinicians from multiple clinical disciplines, as well as for clinicians working between different sites.
Implementation of the guidance provided in this statement and its adjunctive materials may need to be adapted to local policies and resources.
It should be acknowledged that staff involved in the airway management of patients during the COVID‐19 pandemic may have to deal with challenges such as variations to normal workflow, unfamiliar working environments, unfamiliar interprofessional teams, potential resource depletion, critically ill patients with limited physiological reserves, and clinician stress and fatigue.
General comments
Generic guidelines already exist for the intubation of critically ill patients and other patient groups.17 The appropriate guidelines should be followed where they do not contradict specific recommendations for the COVID‐19 patient group (outlined below).
In addition, there are generic resources already available to facilitate airway rescue and transition to the “can't intubate, can't oxygenate” (CICO) scenario.18,19 Many of these algorithms are similar in content20 and should be followed where they do not contradict the specific recommendations for patients with COVID‐19.
Furthermore, generic checklists available for the intubation of the critically ill patient should still be used as a minimum, but consideration should be given to using a checklist that has been specifically modified for patients with COVID‐19.
Early intubation should be considered to prevent the additional risk to staff of emergency intubation during severe hypoxia or cardiac or respiratory arrest, and to avoid prolonged use of high flow nasal oxygen or non‐invasive ventilation.
Significant institutional preparation is required to optimise staff and patient safety in preparing for the airway management of patients with COVID‐19. In addition to clinical and support staff in the ICU, operating theatre and ED, extensive liaison will be required with multiple other stakeholders including, but not limited to, administration, infection control, engineering, sterilisation and equipment disposal services, and procurement and education units.
The principles for airway management outlined below should be the same for both the COVID‐19 patient group with mild or asymptomatic disease requiring urgent surgery and for critically ill patients with acute respiratory distress syndrome.
Guiding principles
The recommendations have been developed according to the following general principles, with the goal of maintaining staff safety while providing timely, efficient and effective airway management (Box 3).
Standardised practice should be developed in accordance with the following criteria:
- safety — choose options that will not expose patients or staff to unnecessary risk;
- simplicity — straightforward solutions that can be executed efficiently;
- familiarity — where possible, rely on existing techniques that are familiar to the relevant clinicians;
- reliability — choose options that are known to be successful in the hands of the relevant clinicians; and
- robustness — choose options that will continue to fulfil the above criteria in the face of foreseeable variations in patient characteristics, environment, and personnel and resources availability.
Recommendations for airway management in patients with COVID‐19
Environment for airway management
Negative pressure ventilation rooms with an anteroom are ideal to minimise exposure to aerosol and droplet particles. Where this is not feasible, normal pressure rooms with closed doors are recommended. Furthermore, positive pressure ventilation areas, which are common in operating theatres, should ideally be avoided (see below).
Some hospitals have created dedicated spaces for the planned airway management of patients with COVID‐19 (eg, airborne infection isolation rooms). The resource and ergonomic advantages of this approach need to be balanced against the implications of transporting potentially infective patients around the hospital and of room cleaning between patients.
The decision to move a clinically stable patient between two clinical areas before airway management should primarily be based on whether the destination environment will provide a more controlled situation, better equipment and/or more experienced staff to make the process of airway management safer.
Equipment, monitoring and medications
General principles
When an equivalent disposable item of equipment is available, this is always preferred over reusable equipment. If disposable items are not considered equivalent, the time, resource and infection risk implications of employing reusable equipment should be considered on a case‐by‐case basis.
Allocation of dedicated items of reusable equipment for use in the COVID‐19 patient group is preferred where feasible.
Oxygen delivery and ventilation equipment during pre‐oxygenation
Pre‐oxygenation should be performed using a well fitting occlusive face mask attached to a manual ventilation device with an oxygen source.
A viral filter must be inserted between the face mask and the manual ventilation device to prevent circuit contamination and minimise aerosolisation in expired gas from non‐rebreathing circuits. The viral filter should be applied directly to the face mask, as an increased number of connections between the face mask and the filter increase the opportunity for disconnection on the patient side.
An anaesthetic machine with a circle system, a hand‐held circuit (eg, a Mapleson circuit) or a self‐inflating bag valve mask attached to an occlusive face mask can be used as the manual ventilation device. While bag collapse when using Mapleson and circle systems provides a sensitive indication of face mask leaks (alerting to potential aerosolisation), this should only be a consideration for clinicians already familiar with these devices. For anaesthetists, manometry and end‐tidal oxygen (ETO2) monitoring are further advantages of using an anaesthetic machine for this purpose.
The rebreathing or non‐rebreathing nature of the ventilation device should not be a consideration for any clinician group in choosing between these alternatives because once the viral filter is applied, no virus should enter the ventilation device. Hence, the most important factor in choosing between these devices is prior familiarity.
Non‐rebreather masks (with a reservoir bag) provide suboptimal pre‐oxygenation and promote aerosolisation and are not recommended for this purpose. Furthermore, nasal oxygen therapy (via standard or high flow nasal cannulae) should not be used during pre‐oxygenation or for apnoeic oxygenation due to the risk to the intubation team.
Oxygen delivery and ventilation equipment after intubation
Oxygenation and mechanical ventilation can be delivered using operating theatre anaesthetic machines or mechanical ventilators (in ICU or ED). While both machines have advantages and disadvantages, the choice will likely depend more on their availability and the location of patient care rather than on their individual characteristics.
Airway equipment
To keep the main airway trolley outside the patient room, we recommend a pre‐prepared COVID‐19 intubation tray (Box 4) or a dedicated COVID‐19 airway trolley.
Supraglottic airways
If a supraglottic airway is indicated, the use of a second generation device is recommended, as its higher seal pressure during positive pressure ventilation decreases the risk of aerosolisation of virus‐containing fluid particles.
Videolaryngoscopy
It is recognised that videolaryngoscopes are a limited resource in many settings. Where they can be accessed, they should be immediately available in the room during tracheal intubation. A videolaryngoscope should be dedicated for use in patients with COVID‐19, where this is feasible, and disposable videolaryngoscope blades are preferred. Both Macintosh and hyperangulated blades should ideally be available — hyperangulated blades should only be used by airway operators who are proficient in their use.
Suction
Once the patient is intubated, closed suction systems should be used to minimise aerosolisation.
Additional information
A cuff manometer should be available to measure tracheal tube cuff pressure in order to minimise leaks and the risk of aerosolisation.
Furthermore, the equipment ready outside the room should include a cardiac arrest trolley, an airway trolley and a bronchoscope.
Intubation team
When assembling a team for intubation, numbers should be limited — only those directly involved in the process of airway management should be in the room — and the most experienced staff should be included.
Consideration should be given to excluding staff who are vulnerable to infection from the airway team, such as staff who are older (aged > 60 years), immunosuppressed, pregnant, or who have serious comorbidities.
Clearly defined roles should be allocated (Box 5) including:
- an airway operator: the most experienced or skilled airway clinician should perform upper airway interventions. This may require calling for the assistance of another clinician (eg, a senior anaesthetist) within the hospital. If an anaesthetist is called, they should perform tracheal intubation, and all airway management decisions should be deferred to them;
- an airway assistant: this should be an experienced clinician who will pass airway equipment to the airway operator and help with bougie use and bag valve mask ventilation;
- a team leader: a second senior airway clinician should be included to coordinate the team, manage drugs, observe monitoring and provide airway help if emergency front‐of‐neck airway (eFONA) is required;
- an in‐room runner: this team member is optional, depending on need — the number of team members in the room should always be minimised;
- a door runner: this team member, who should be placed in the anteroom or just outside the patient's room, should pass in any further equipment that may be needed in an emergency. This team member may also act as the “PPE spotter” (see below); and
- an outside room runner: this team member will pass equipment into the anteroom (dirty side) (Box 5) or directly to the door runner if there is no anteroom.
Intubation teams may be employed by certain hospitals, but this would be at the discretion of individual institutions and dependent on the number of cases and staff resources. The use of intubation teams may improve familiarity, compliance and efficiency of processes around airway management in patients with COVID‐19, including proper application and removal of PPE among the staff. Evidence for the benefit of this strategy is not yet available.
Planning
Meticulous airway assessment should be performed early by a senior airway clinician and should be clearly documented. In addition, an individualised airway management strategy should be formed, based on patient assessment and the skill mix of the team. This strategy should include plans for intubation and airway rescue via face mask, supraglottic airway and eFONA, with defined triggers for moving between each plan.
The ventilation plan should be discussed before intubation and may involve protective lung ventilation, use of high positive end expiratory pressure (PEEP), prone ventilation, and other strategies for refractory hypoxaemia, including consideration of extracorporeal membrane oxygenation.
Communication
When managing patients with COVID‐19, clear communication is vital due to the risk of staff contamination, but it may be impeded by the use of a PPE. Therefore, it is important to do a prior briefing to share a mental model with the whole team before intubation. This briefing should include, but is not limited to, verbalising role allocation, checking equipment, discussing any anticipated challenges and determining the airway management strategy, post‐intubation plans, and PPE donning and doffing processes.
Team members should use clear, simple, concise language and they should raise their voice to be heard through the PPE. Moreover, it may be hard for the outside room runner to hear requests from inside the room; thus, if there is no audio communication system in place, a whiteboard and marker pen should be provided for each patient room.
Standardised language should be consistently employed; that is, it should be precisely defined, mutually understood and used to communicate key moments of situation awareness (critical language).21 In addition, closed‐loop communication and speaking up should be encouraged.
Cognitive aids
The incidence of errors during airway management is known to increase under stress, even when experienced clinicians are involved. Task fixation, loss of situation awareness and impaired judgement may arise.22 The use of resources to support the implementation of the airway strategy is particularly important in the COVID‐19 patient group, where the challenges involved may consume significant cognitive bandwidth, even before airway management becomes difficult.
Using a “kit dump mat” may facilitate the preparation of equipment. Ideally, this mat should be specifically modified for patients with COVID‐19. In addition, it is recommended to routinely use an intubation checklist, preferably specifically modified for patients with COVID‐19 (Supporting Information). Furthermore, it is recommended to be familiar with and use a simple cognitive aid for airway rescue designed to be referred to in real‐time during an evolving airway crisis.
Personal protective equipment
For the management of patients with COVID‐19, a “buddy system” should be implemented. Therefore, all staff should ideally have donning and doffing of PPE individually guided by a specially trained and designated staff member acting as a “spotter” before entering the patient's room. This may help protect task‐focused staff from PPE breaches and may help mitigate the stress experienced by the intubation team.
The type of PPE used by the airway operator, the airway assistant and the team leader, who may need to perform eFONA, should be guided by local health regulatory authorities.23 At a minimum, it should include an impervious gown, a theatre hat, an N95 mask, a face shield and eye protection, and double gloves should also be considered. Clinicians requiring corrective eyewear should be cognisant of institutional policies for removing and cleaning it without self‐contamination. Outer gloves (if used) should be removed carefully after airway management is completed. This level of PPE should also be worn for endotracheal tube repositioning or replacement, bronchoscopy, and percutaneous dilatational tracheostomy.
The PPE for the in‐room runner and the door runner should include a gown, gloves, an N95 face mask and eye protection. No PPE should be worn by the outside room runner.
Infection control and staff safety should remain a top priority. Furthermore, hand hygiene processes and hospital and/or World Health Organization guidelines for both donning and doffing of PPE need to be vigilantly followed.24
It is important to recognise that doffing is a high risk step for virus transmission to health care workers. Any exposed areas of skin (eg, neck) should be cleaned with hospital‐grade antiviral wipes after doffing.
Process for airway management
Familiar, reliable techniques should be used to maximise first pass success, secure the airway rapidly and minimise risks to staff.
Pre‐oxygenation
Limited experience with patients with COVID‐19 has shown that rapid and profound desaturation may occur on induction of anaesthesia. Pre‐oxygenation is therefore of particular importance.
In the period before the team enters the room to perform intubation, the patient's oxygen delivery should be maximised by placing the patient in a 45° head up position and they should remain in this position for pre‐oxygenation.
Before the team enters the room, a critically ill patient with COVID‐19 may be receiving high flow oxygen via nasal cannulae, a simple oxygen mask, or a non‐rebreather mask with a reservoir bag. Due to the risks of aerosolisation, these devices should not be used for pre‐oxygenation when the team is in position.
Furthermore, if the patient is receiving high flow oxygen, it should be turned off before removal of the face mask or nasal cannulae to minimise aerosolisation.
Pre‐oxygenation should then be commenced immediately, using the best available face mask device, with a viral filter firmly applied directly to the mask and end‐tidal carbon dioxide (ETCO2) in the system. Added connections on the patient side of the viral filter increase the opportunity for disconnection.
PEEP should be applied via a PEEP valve attached to a Mapleson C circuit, via a self‐inflating bag valve mask, via an adjustable pressure‐limiting valve on an anaesthetic machine, or via non‐invasive ventilation.
A vice (V‐E) grip is recommended to maximise the face mask seal and minimise gas leak after induction (Box 6). Moreover, it is suggested that patients with COVID‐19 should be encouraged to remove all facial hair on admission, where feasible, so as to optimise face mask seal if airway management is required.
Continuous waveform capnography should be used if available. A triangular rather than a square ETCO2 trace or a low numerical ETCO2 value during pre‐oxygenation may indicate a leak around the face mask and should prompt interventions to improve the seal.
To fully pre‐oxygenate the patient, a minimum of 5 minutes of pre‐oxygenation is recommended if ETO2 is not available.
After neuromuscular blockade, patients with severe disease are likely to require manual ventilation to prevent profound oxygen desaturation. To minimise the risk of aerosolisation of airway secretions, this should be performed as a two‐person technique, with the airway assistant gently squeezing the bag and adjusting the level of PEEP as required.
If non‐invasive ventilation is used for pre‐oxygenation, any perceived advantage over the technique outlined above should be balanced against increased complexity and risk of aerosolisation. A viral filter should be inserted between the face mask and the circuit, and the ventilator should be placed on standby before removing the mask.
The use of high flow nasal oxygen for apnoeic oxygenation during intubation is not recommended because of the risk to staff.
Induction
Rapid sequence intubation should be used as the default technique, unless concerns with airway difficulty make this inappropriate.
Initial neuromuscular blockade can be achieved with rocuronium (> 1.5 mg/kg ideal body weight) or suxamethonium (1.5 mg/kg total body weight). Generous dosing promotes rapid onset of deep neuromuscular blockade and minimises the risk of the patient coughing during airway instrumentation.
Palpating for the cricoid cartilage may inadvertently encourage clinicians to lean in closer to the patient's airway and, given its highly stimulating nature, it may precipitate coughing. In view of the limited evidence for its effectiveness, the risk–benefit of application of cricoid pressure should be carefully considered.
The time between administration of a neuromuscular blocking agent and laryngoscopy should be closely monitored to minimise the apnoea time, while ensuring adequate time is given for the neuromuscular blocking agent to take effect to avoid precipitating coughing. The extended duration of action of rocuronium potentially provides an advantage over suxamethonium in patients with COVID‐19 by preventing coughing should attempts at airway management be prolonged.
It is discouraged to disconnect the viral filter from the ventilation device once the face mask has been removed from the patient to perform laryngoscopy. This has been proposed as a mechanism to avoid aerosolisation of virus‐containing secretions on the patient side of the filter. However, teams under stress may fail to reconnect the viral filter after intubation, potentially allowing virally contaminated expired gas to be expelled into the room with ventilation.
Intubation
For clinicians proficient with its use, the routine use of a videolaryngoscope is recommended for the first attempt at intubation. In addition to a videolaryngoscope potentially contributing to first‐pass success, visualising the larynx using the indirect (video screen) view, with the operator standing upright and elbow straight, maximises the distance between the airway operator's face and the patient. This should reduce the risk of viral transmission.
The choice between a Macintosh geometry and a hyperangulated videolaryngoscope blade should be made according to the skill set and clinical judgement of the airway operator. Care should be taken to place the tube to the correct depth the first time to minimise the need for subsequent cuff deflations. Once the tube is placed, the cuff should be inflated before positive pressure ventilation is attempted. The viral filter should be applied directly to the end of the tracheal tube, as increasing the number of connections between the filter and the tracheal tube increases opportunities for disconnection. The cuff pressure should be monitored with a cuff manometer to ensure an adequate seal.
Airway rescue
If airway management is challenging, standard airway rescue interventions should be applied where they do not conflict with the specific recommendations for managing patients with COVID‐19. The use of a bronchoscope for asleep video‐assisted fibre‐optic intubation or for exchange of a supraglottic airway for a tracheal tube is not an aerosol‐generating event when performed in a profoundly paralysed apnoeic patient without use of positive pressure ventilation or insufflation or suction via the bronchoscope port. Such techniques should only be implemented by clinicians familiar with their use, in accordance with their usual practice for airway rescue.
If rescue face mask ventilation is required, a vice (V‐E) grip is recommended (the airway assistant is therefore required to squeeze the bag), and ventilation pressure should be minimised through ramping and/or early use of an oropharyngeal airway with low gas flows.
In a CICO situation, it is recommended to use a scalpel‐bougie eFONA technique to minimise the risk of high pressure oxygen insufflation via a small‐bore cannula. Contrary to usual practice, further attempts to deliver oxygen from above should not occur during the performance of eFONA to avoid aerosolisation of virus‐containing fluids when the trachea is punctured.
After intubation
A nasogastric tube should be placed at the time of intubation to avoid further close contact with the airway. Unless single use, the laryngoscope blade should be bagged and sealed for sterilisation immediately after intubation, according to national standards.25
The PPE should be removed as per local and WHO guidelines, using a PPE spotter and noting that there is more risk of contamination during doffing than donning. The PPE should be disposed of as per local policy.
Chest x‐ray should usually be performed to confirm tube position, but it should be delayed until after central line insertion to minimise staff entries into the room.
A debrief should occur after every episode or airway management in this patient group to discuss lessons learned.
Extubation practices
There are generic guidelines available for extubation26 and they should be followed when they do not conflict with the special considerations for the extubation of patients with COVID‐19 outlined below. Patients should ideally be non‐infective before extubation, but this is likely to be unfeasible as resources are drained. However, when this is achievable, standard extubation procedures apply. In situations where a patient is still at risk of viral transmission, the following recommendations should be observed:
- patients should ideally be ready for extubation onto face mask;
- two staff members should perform the extubation;
- the same level of PPE should be worn for extubation as is worn by the airway operator, airway assistant and team leader during intubation;
- the patient should not be encouraged to cough;
- strategies to minimise coughing during extubation include the use of intravenous opioids, lidocaine or dexmedetomidine. Placement of plastic sheets over the patient's face during extubation, in case coughing occurs, has been proposed, but caution is advised with this approach as the risk of clinician self‐contamination may be increased due to collection of viral‐containing secretions on the plastic;
- a simple oxygen mask should be placed on the patient immediately after extubation to minimise aerosolisation from coughing; and
- oral suctioning may be performed, with care taken not to precipitate coughing.
Education
Early, department‐based interprofessional education is vital for all staff involved in the airway management of patients with COVID‐19. Regular and repeated education, simulation‐based education, and staff education on donning and doffing of PPE, accompanied by multimedia visual aids and supervised practice are strongly recommended.
Special contexts
Immediate intensive care after intubation
For ongoing mechanical ventilation, humidification of inspired gases can be achieved using a heat and moisture exchanger filter or a humidified circuit. If the latter is chosen, the viral filter used for tracheal intubation needs to be removed (due to the risk of waterlogging) during a planned disconnection. At the same time, an in‐line suction catheter system can be inserted. In a planned disconnection, the ventilator should be placed on standby and the tube clamped before disconnection. Care should be taken when applying and removing a tube clamp, as this can lead to tube damage or dislodgement. Furthermore, care should also be taken to ensure ventilation is recommenced after reconnection.
In a dry circuit, a combined heat and moisture exchanger and viral filter can be left in place, but this means that nebulisers cannot be administered without breaking the circuit to place a nebuliser between the patient and the filter.
If the viral filter has been removed, the ventilator should be placed on standby for all circuit disconnections to minimise the risks of aerosolisation. Great care should be taken that ventilation is recommenced after the circuit is reconnected.
Urgent surgery in patients with COVID‐19
Patients with COVID‐19 who need urgent surgery will have COVID‐19 as an incidental comorbidity, unrelated to their need for airway management, and may have only mild or asymptomatic COVID‐19.
If surgery is non‐urgent and can be delayed until the patient is non‐infective, it should be deferred. If patients have suspected rather than confirmed COVID‐19 and surgery is not time‐critical, then testing to confirm or exclude COVID‐19 will avoid wasting PPE. The ability of available testing to reliably exclude COVID‐19 is crucial if implementing this step. The time frame beyond which urgency of surgery precludes such testing depends on the speed with which results can be provided at a given institution.
For surgery that cannot be deferred in the COVID‐19 patient group, an operating theatre dedicated to patients with COVID‐19 should be used. Regional anaesthesia avoids airway management, thus decreasing the potential for aerosolisation and risk of transmission. It is important to avoid sedation to decrease the need for supplementary oxygen and to minimise the risk of precipitating unplanned airway management. Furthermore, clinicians should maintain a safe minimum distance from the patient's airway and implement standard droplet or contact precautions for both the anaesthetist and the patient. If a patient is unlikely to tolerate regional anaesthesia without significant sedation, the risk of precipitating unplanned airway management must be balanced against the risk of proceeding immediately to general anaesthesia. It is encouraged to create expert regional anaesthesia teams to assess the potential for surgery to be conducted using regional techniques and to maximise their success.
If general anaesthesia is required, airway management in patients with COVID‐19 presenting for urgent surgery should follow the same principles outlined above, with particular attention to the following issues:
- positive pressure room ventilation should be disabled and converted to negative (ideally) or neutral pressure;
- when positive pressure room ventilation cannot be disabled, any neutral pressure anterooms should be regarded as dirty afterwards;
- the number of air exchanges per hour should be maximised; and
- early consultation with the engineering department about the best way to optimise theatre ventilation is advised.
All staff should enter the operating theatre via an anteroom using this as an airlock, without opening the inner and outer doors at the same time. Once the patient is inside, the doors to the operating theatre should be obstructed or locked and appropriately signed to prevent them from inadvertently being opened.
As there is little evidence to inform best practice, the choice of anaesthetic technique and airway type (face mask, supraglottic airway, tracheal tube) should primarily be based on the same principles as those for patients without COVID‐19. It is important to note that, when general anaesthesia is required, the use of neuromuscular blocking agents (according to the principles outlined above) ensures apnoea and prevention of coughing during airway interventions, thereby minimising the risk of aerosol generation while the airway management team is in close proximity to the patient's airway. Furthermore, it should be considered that intubation maximises the seal around the airway, limiting aerosol generation with positive pressure ventilation. In a patient not at risk of aspiration, deep extubation may be considered — other strategies to minimise coughing are described in the “Extubation practices” section above. Moreover, positive pressure ventilation with a face mask or supraglottic airway should be avoided due to the risk of aerosol generation with a suboptimal seal.
As discussed above, staff not immediately involved with airway management, including surgical staff, should not enter the operating theatre until after the airway has been secured. Once the airway is secured, sufficient time should be allowed for any aerosols generated to disperse before other staff enter the operating theatre. The time required for this will depend on the air exchange rate in the operating theatre. This may not be possible when initiation of surgery is time‐critical.
All staff in the operating theatre during and after airway management (even after the elapsed time) should wear aerosol‐protective PPE.
The patient should recover in the operating theatre to avoid exposure to other patients and staff.
Unplanned and pre‐hospital airway management
Unplanned and pre‐hospital airway management presents great risk to staff, especially during cardiac arrest. Devising management protocols that minimise time to commencement of external cardiac compressions while ensuring that staff are appropriately protected from viral exposure is extremely challenging. Some guidelines have already been suggested in the United Kingdom.27 We recommend the following principles:
- cardiac compressions should not commence until the responsible staff are in aerosol‐protective PPE — processes must be put in place to ensure appropriate PPE is rapidly allocated to staff at inpatient cardiac arrest calls (and pre‐hospital sites);
- the number of people in the room should be kept to a minimum at all times and no one should be allowed in the room without aerosol‐protective PPE;
- steps must be taken to protect first responders from exposure to aerosols and droplets during external cardiac compressions;
- compression‐only cardiopulmonary resuscitation is advocated until the airway has been secured with a viral filter in place;
- early tracheal intubation should be performed by a skilled airway operator;
- before intubation, first responders should only use the airway techniques in which they have experience;
- supraglottic airway placement is likely a better option than face mask ventilation due to less aerosolisation, if immediate intubation is not possible;
- face mask application and positive pressure ventilation should be avoided wherever possible, especially during cardiac compressions; and
- clinicians should avoid close contact with the patient's mouth at any time (eg, do not listen for breathing).
Conclusion
The Safe Airway Society principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group were developed after expert consultation and review of the available literature. This consensus statement recommends safe, simple, familiar, reliable and robust practices that should be adopted for all episodes of airway management for patients with COVID‐19. Accompanying cognitive aids have been released to promote early education of all airway clinicians in Australia and New Zealand.
The unedited version of this article was published as a preprint on mja.com.au on 16 March 2020.
Box 1 – Sources of potential aerosol generation during airway management
|
|
Sources |
||||||||||||||
|
|
|||||||||||||||
|
Aerosol‐generating events |
|
||||||||||||||
|
Procedures vulnerable to aerosol generation (increased risk of association with aerosol‐generating events) |
|
||||||||||||||
|
|
|||||||||||||||
|
NIV = non‐invasive ventilation. * The reliability of the seal is greatest with tracheal tube > supraglottic airway > face mask. |
|||||||||||||||
Box 2 – Risk factors for aerosol generation
|
Risk factor |
Protective strategy |
||||||||||||||
|
|
|||||||||||||||
|
Coughing |
|
||||||||||||||
|
Inadequate face mask seal during pre‐oxygenation |
|
||||||||||||||
|
Positive pressure ventilation with inadequate seal |
|
||||||||||||||
|
High gas flows |
Avoid high flow nasal oxygen |
||||||||||||||
|
|
|||||||||||||||
|
EET = endotracheal tube; ETO2 = end‐tidal oxygen; PPE = personal protective equipment. * Only beneficial for clinicians with prior familiarity with these devices. † Where applicable. |
|||||||||||||||
Box 3 – Guiding principles for airway management of patients with coronavirus disease 2019 (COVID‐19)
- Intensive training
- Early intervention
- Meticulous planning
- Vigilant infection control
- Efficient airway management processes
- Clear communication
- Standardised practice
Box 4 – Suggested contents for the coronavirus disease 2019 (COVID‐19) intubation tray
- Macintosh videolaryngoscope (with blade sized to patient)
- Hyperangulated videolaryngoscope (if available, with blade sized to patient)
- Macintosh direct laryngoscope (with blade sized to patient)
- Bougie/stylet*
- 10 mL syringe
- Tube tie
- Sachet lubricant
- Endotracheal tubes (appropriate size range for patient)
- Second generation supraglottic airway (sized to patient)
- Oropharyngeal airway and nasopharyngeal airway (sized to patient)
- Scalpel and bougie CICO rescue kit
- Large‐bore nasogastric tube (appropriate size for patient)
- Continuous waveform ETCO2 cuvette or tubing
- Viral filter
- In‐line suction catheter
CICO = “can’t intubate, can’t oxygenate”; ETCO2 = end-¬tidal carbon dioxide. * At least one pre-curved introducer (bougie/stylet) must be available for use with a hyperangulated videolaryngoscope blade.
Box 5 – Coronavirus disease 2019 (COVID‐19) intubation team members
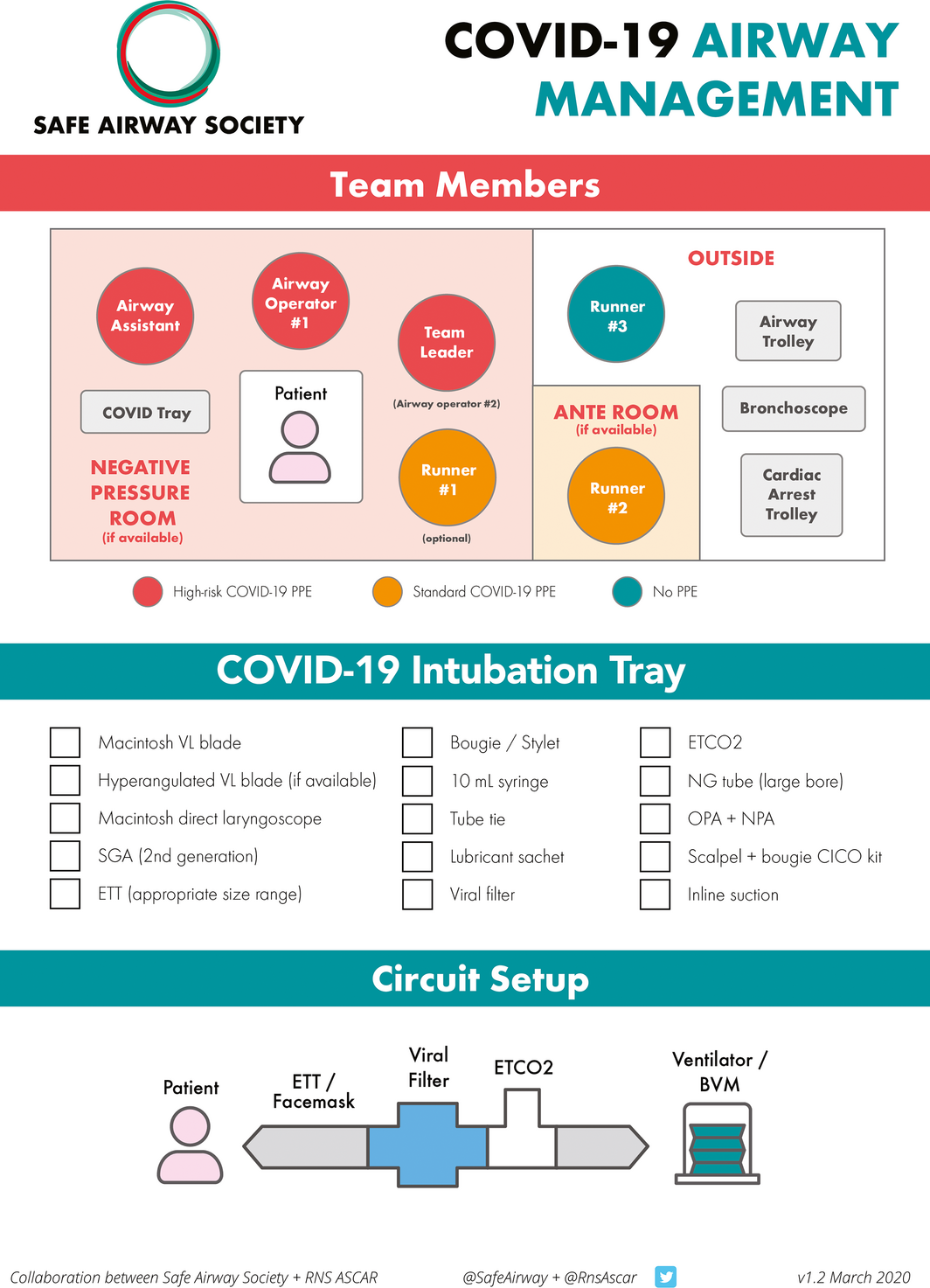
BVM = bag valve mask; CICO = ”can't intubate, can't oxygenate”; ETCO2 = end‐tidal carbon dioxide; ETT = endotracheal tube; NG = nasogastric; NPA = nasopharyngeal airway; PPE = personal protective equipment; OPA = oropharyngeal airway; SGA = supraglottic airway; VL = videolaryngoscope.
Provenance: Not commissioned; externally peer reviewed.
- David J Brewster1,2,3
- Nicholas Chrimes3
- Thy BT Do3
- Kirstin Fraser3
- Christopher J Groombridge3
- Andy Higgs3
- Matthew J Humar3
- Timothy J Leeuwenburg3
- Steven McGloughlin1,4
- Fiona G Newman3
- Chris P Nickson1,3,4
- Adam Rehak3,5
- David Vokes3
- Jonathan J Gatward3,5
- 1 Monash University, Melbourne, VIC
- 2 Cabrini Hospital, Melbourne, VIC
- 3 Safe Airway Society, Melbourne, VIC
- 4 Alfred Hospital, Melbourne, VIC
- 5 Royal North Shore Hospital, Sydney, NSW
We thank Tim Cook for allowing us to consult the Royal College of Anaesthetists COVID‐19 airway management principles in development during the preparation of this statement. We also thank Louise Ellard for allowing us to consult the Austin Health's COVID‐19 intubation guidelines during the preparation of this statement, and Dan Zeloof, Dan Moi, Jessie Maulder and Dush Iyer for their work on the graphics. Free, open access resources to accompany this article can be found at www.safeairwaysociety.org/covid19.
No relevant disclosures.
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506.
- 2. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507–513.
- 3. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020; https://doi.org/10.1001/jama.2020.2648. [Epub ahead of print]
- 4. Centers for Disease Control and Prevention. Environmental cleaning and disinfection recommendations: interim recommendations for US households with suspected/confirmed coronavirus disease 2019 (COVID‐19). Georgia, GA: CDC, 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/home/cleaning-disinfection.html (viewed Mar 2020).
- 5. Wolff MH, Sattar SA, Adegbunrin O, Tetro J. Environmental survival and microbicide inactivation of coronaviruses. In: Schmidt A, Weber O, Wolff MH editors. Coronaviruses with special emphasis on first insights concerning SARS. Germany: Birkhäuser Basel, 2005: 201–212.
- 6. Casanova LM, Jeon S, Rutala WA, et al. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl Environ Microbiol 2010; 76: 2712–2717.
- 7. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N Engl J Med 2020; https://doi.org/10.1056/nejmc2004973. [Epub ahead of print]
- 8. Yu IT, Qiu H, Tse LA, Wong TW. Severe acute respiratory syndrome beyond Amoy Gardens: completing the incomplete legacy. Clin Infect Dis 2014; 58: 683–686.
- 9. Parodi SM, Liu VX. From containment to mitigation of COVID‐19 in the US. JAMA 2020; https://doi.org/10.1001/jama.2020.3882. [Epub ahead of print]
- 10. Public Health England. High consequence infectious diseases (HCID). London: Crown, 2020. https://www.gov.uk/guidance/high-consequence-infectious-diseases-hcid (viewed Mar 2020).
- 11. Australian and New Zealand Intensive Care Society. COVID‐19 guidelines. Melbourne: ANZICS, 2020. https://www.anzics.com.au/wp-content/uploads/2020/03/ANZICS-COVID-19-Guidelines-Version-1.pdf (viewed Mar 2020).
- 12. Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019‐nCoV) patients. Can J Anaesth 2020; https://doi.org/10.1007/s12630-020-01591-x. [Epub ahead of print]
- 13. Hui DS, Chow BK, Lo T, et al. Exhaled air dispersion during high‐flow nasal cannula therapy versus CPAP via different masks. Eur Respir J 2019; 53: 1802339.
- 14. Kotoda M, Hishiyama S, Mitsui K, et al. Assessment of the potential for pathogen dispersal during high‐flow nasal therapy. J Hosp Infect 2019; https://doi.org/10.1016/j.jhin.2019.11.010. [Epub ahead of print]
- 15. Zuo MZ, Huang YG, Ma WH, et al. Expert recommendations for tracheal intubation in critically ill patients with novel coronavirus disease 2019. Chin Med Sci J 2020; https://doi.org/10.24920/003724. [Epub ahead of print]
- 16. Peng PWH, Ho PL, Hota SS. Outbreak of a new coronavirus: what anaesthetists should know. Br J Anaesth 2020; https://doi.org/10.1016/j.bja.2020.02.008. [Epub ahead of print]
- 17. Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 2018; 120: 323–352.
- 18. Chrimes N. The Vortex: a universal “high‐acuity implementation tool” for emergency airway management. Br J Anaesth 2016; 117 (Suppl): i20–i27.
- 19. Australian and New Zealand College of Anaesthetists. Guidelines for the management of evolving airway obstruction: transition to the can't intubate can't oxygenate airway emergency. Melbourne: ANZCA, 2017. http://www.anzca.edu.au/getattachment/resources/professional-documents/ps61_guideline_airway_cognitive_aid_2016.pdf (viewed Feb 2020).
- 20. Edelman DA, Perkins EJ, Brewster DJ. Difficult airway management algorithms: a directed review. Anaesthesia 2019; 74: 1175–1185.
- 21. Chrimes N, Cook TM. Critical airways, critical language. Br J Anaesth 2017; 118: 649–654.
- 22. Cook TM, Woodall N, Frerk C; Fourth National Audit Project.Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011; 106: 617–631.
- 23. Australian and New Zealand College of Anaesthetists. ANZCA statement on personal protection equipment during the COVID‐19 pandemic (30 March 2020). Melbourne: ANZCA, 2020. http://www.anzca.edu.au/documents/pcu_anzca-covid-ppe-statement_20200330.pdf (viewed Mar 2020).
- 24. World Health Organization. Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. Interim guidance. WHO, 2020. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 (viewed Apr 2020).
- 25. Australian Commission on Safety and Quality in Health Care. Advisory: reprocessing of reusable medical devices in health service organisations. Sydney: ACSQHC, 2020. https://www.safetyandquality.gov.au/sites/default/files/2020-03/as1807_reprocessing_of_reusable_medical_devices_in_health_service_organisations_march_2020.pdf (viewed Apr 2020).
- 26. Difficult Airway Society Extubation Guidelines Group; Popat M, Mitchell V, Dravid R, et al. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia 2012; 67: 318–340.
- 27. Resuscitation Council UK. Statement on COVID‐19 in relation to CPR and resuscitation in healthcare settings. https://www.resus.org.uk/media/statements/resuscitation-council-uk-statements-on-covid-19-coronavirus-cpr-and-resuscitation/covid-healthcare/ (viewed Mar 2020).






Abstract
Introduction: This statement was planned on 11 March 2020 to provide clinical guidance and aid staff preparation for the coronavirus disease 2019 (COVID‐19) pandemic in Australia and New Zealand. It has been widely endorsed by relevant specialty colleges and societies.
Main recommendations:
Changes in management as a result of this statement: Airway clinicians in Australia and New Zealand should now already be involved in regular intensive training for the airway management of the COVID‐19 patient group. This training should focus on the principles of early intervention, meticulous planning, vigilant infection control, efficient processes, clear communication and standardised practice.