Clinical services are central to improving preventive measures and reducing disease prevalence among Aboriginal and Torres Strait Islander (Indigenous) Australians, but non‐clinical support services can facilitate access to and the uptake of care. Examples of non‐clinical support include reducing anxiety about new diagnoses,1 interpreting biomedical information,2 and enabling cultural safety.3 Family and community members play key roles in providing non‐clinical support, including facilitating and motivating attendance at appointments,4 accompanying patients to health services to alleviate their anxiety,1 participating in shared care,5 and enhancing the effectiveness of preventive health promotion activities.6
The prevalence of vision impairment and blindness is three times as high among Indigenous Australians as among other Australians; 90% of these conditions are preventable or treatable.7 The three leading causes of vision impairment and blindness in Indigenous Australians are uncorrected refractive error, cataract, and diabetic retinopathy.7 Trachoma — in Australia found only in remote Indigenous communities — can lead to irreversible blindness if untreated.8 Eye care pathways can be long and access to services complex, particularly for patients in remote areas.9 A previous study10 identified the importance of non‐clinical support for Indigenous eye care at the community level, particularly given socio‐cultural determinants, such as limited understanding of English, poverty, historical trauma, and racism, that make access to services difficult for Indigenous patients. Eye care coordination involves many non‐clinical aspects and is critical for ensuring that patients attend care,11,12 but specific funding for such activities is limited.13
Given the need for better and more accessible eye care services for Indigenous Australians, it is important to understand what constitutes non‐clinical support and to know who provides it. Our aim was therefore to synthesise information about eye health care for Indigenous Australians in order to identify research into non‐clinical support, who is providing such support, and its impact on eye health outcomes.
Methods
Search strategy
The search strategy followed the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines.14 We searched MEDLINE/EMBASE, Web of Science, Informit, EBSCO (CINAHL and Anthropology Plus), and ProQuest Central for studies published between January 2000 and July 2018 with the search strategy summarised in Box 1. The search results were imported into a single EndNote X9 (Clarivate Analytics) library to identify duplicate articles. The combined library was imported into Abstrackr (Brown University, USA) for title and abstract screening.
Eligibility criteria
Articles were included in the review if they contained data on non‐clinical support for Indigenous eye health care in Australia, reported empirical research, and were published in peer‐reviewed journals. Articles were excluded if they were reviews, study protocols, commentaries, editorials or grey literature, did not refer to non‐clinical support for Indigenous eye health in Australia, or were in languages other than English.
Study selection and data extraction
To minimise selection bias, the titles and abstracts of each article identified by the literature search were independently assessed according to the inclusion and exclusion criteria by two reviewers. When it was unclear whether the selection criteria were met, studies were retained for full text review. Disagreements were resolved by discussion, and adjudicated by a third reviewer. Articles selected for inclusion were reviewed to identify evidence of non‐clinical support for Indigenous eye health. Each article was subjected to inductive thematic analysis,15 whereby references to non‐clinical support were coded with the NVivo qualitative data analysis software, version 12 (QSR International). Data extracted from publications were categorised as being either about types of non‐clinical support or about the people who provide non‐clinical support. Quantitative results directly related to the impact of non‐clinical support were also coded. Study characteristics, including year of publication, location, sample size, and methods, were recorded for each article.
Quality assessment
To limit the risk of bias, the quality of included articles was independently assessed by two reviewers with the QualSyst tool;16 disagreements were resolved by discussion. The QualSyst tool, developed for assessing qualitative and quantitative studies, applies a scoring system to specific aspects of study design and reporting (final calculated score: range, 0–1.00).16 For mixed methods studies, both qualitative and quantitative aspects were assessed and a combined average score was calculated.
Results
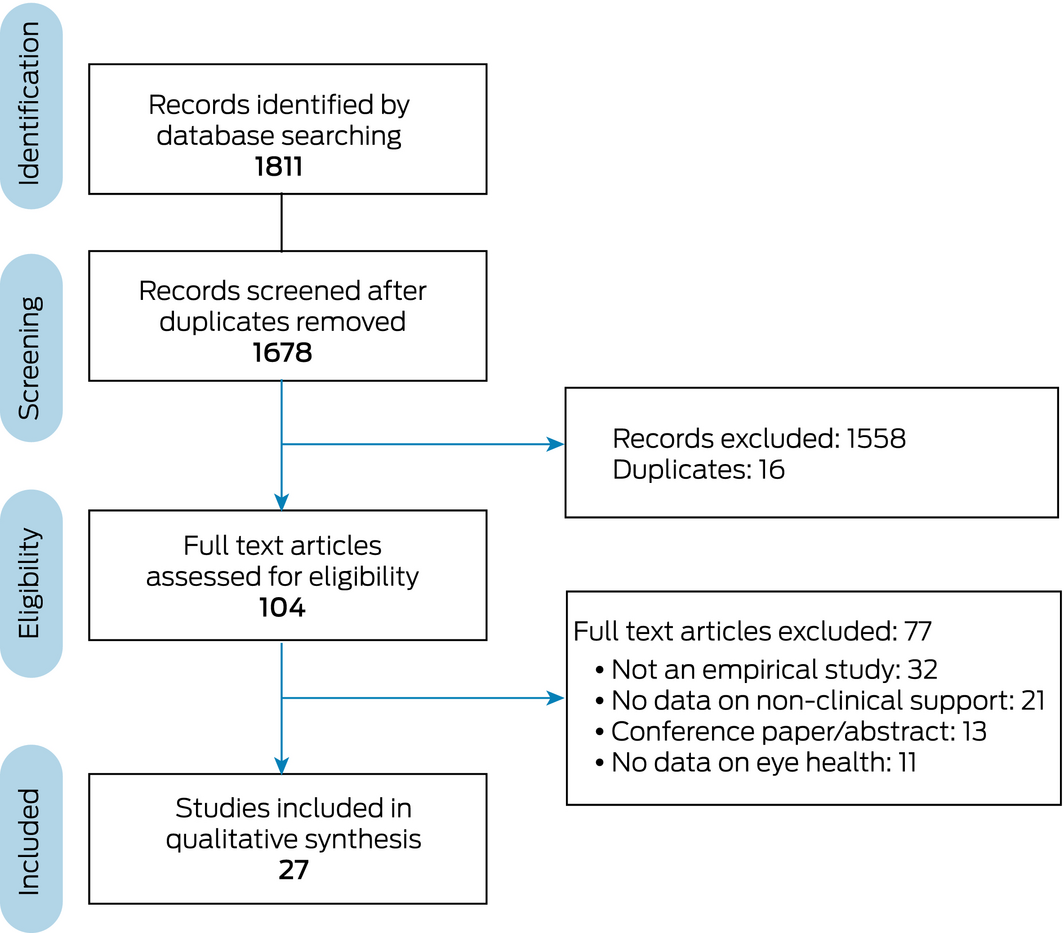
Our database search identified 1811 potentially relevant articles; after removing duplicates, the titles and abstracts of 1678 were screened. Of the 104 full text publications retrieved after screening, 77 articles were excluded after review (Box 2). The characteristics of the 27 included articles, including quality assessment scores, are summarised in Box 3. Quality assessment scores ranged from low (0.40) to very high (1.00); the mean score was 0.76 (standard deviation, 0.15). The studies were undertaken in various locations in urban and rural Australia. Most studies were specifically concerned with Indigenous eye care, but several reported eye care data in the context of diabetes care18,23,29 or specialist outreach care.17,20 Inductive thematic analysis identified five key areas of non‐clinical support for Indigenous eye health.
Coordination of care
As coordination of eye care was mentioned in 20 of the 27 included articles, it was defined as a key type of non‐clinical support. Examples of preventive eye care coordination included organising and facilitating screening of school students for refractive error,27 coordinating diabetic retinopathy screening by retinal camera,40 and coordinating community screening, including community trachoma control programs.24 In the Kimberley region of Western Australia,40 introducing a regional diabetic eye health coordinator increased retinal screening coverage — from 9.4% to 29.8% of the projected 1684 diabetic eye examinations required annually for Indigenous Australians in the region — and the number of screening sites from four to 17.
Primary eye care coordination included organising outreach optometry clinics as part of primary health care services, providing transport, and enabling patient attendance.27,30 Secondary and tertiary eye care coordination included organising and facilitating surgery attendance, booking travel and accommodation for ophthalmic care, and ensuring appropriate follow‐up care.38,41 Key providers of eye care coordination and associated support included eye health coordinators,11,12,24,25,26,30,34,35,40,41 Aboriginal Health Workers (AHWs),23,25,27,34 primary health care staff,34,38,41 and community liaison staff.12,23 One study reported that support provided by regional eye health coordinators was intended to cover multiple communities, but in practice was delivered only to the communities where the coordinators resided.27 The need for a central trachoma coordinator in the Northern Territory was suggested in one study, but the lack of sustainable funding for such a role was a barrier.24
Administrative functions, such as clerical support for visiting eye care practitioners,11,25 and case management, including organising eye care appointments for patients,34 were identified as cost‐effective enablers of improved outcomes for patients undergoing cataract surgery. Cultivating patient engagement with eye care was noted as a central component of coordination, with several studies identifying that contacting and counselling patients, reminding them about appointments, and community outreach were enablers of patient attendance at ophthalmic outreach clinics38 and cataract surgery.12,41 A mixed methods study in urban Queensland41 found that introducing regional cataract surgery coordinators at the primary care level increased the rate of surgery completion among Indigenous patients from one of 55 (2%) to 46 of 103 patients (45%); the increase was partially attributed to additional non‐clinical support, such as facilitating patient and community engagement.
Organising travel and providing transport were identified in four studies as facilitators of patient attendance.23,27,38,41 For instance, an intervention in which home visits were introduced as additional non‐clinical support for chronic disease patients and transport was provided by chronic care coordinators was associated with an 18% increase in visual acuity checks and a 20% increase in attendance at ophthalmology appointments over two years.23 In a qualitative study that analysed factors which influence attendance at ophthalmology appointments, transport drivers were identified as enabling patient engagement and attendance through their familiarity with the local population.38
Integrating and linking services
Fostering links between services and integrating eye care into primary, tertiary and chronic disease care18,23,25,29,30,41 were identified as key non‐clinical support types. Eye health coordinators were described in several articles as central to building and supporting links with and between services.25,26,30,35 A cross‐sectional case study25 found a significant correlation between ophthalmic surgery case rates and the integration of primary, secondary and tertiary service providers, and also that eye health coordinators were key enablers in increasing clinical activity (1.9 times as many cataract operations and 1.4 times as many clinical examinations each week) and reducing waiting times (42% reduction). Several studies reported chronic care coordinators as playing a central role in integrating primary eye care into chronic disease care.23,41 Integrating primary eye care into routine chronic disease care enabled a 29% increase in the number of annual eye examinations18 and an 8.8% increase in the number of visual acuity screenings.29 Several studies found that not having an eye care coordinator was a barrier to effective referral pathways.22,30,32,35 Factors related to ineffective referral pathways included primary care clinicians being reluctant to conduct vision screening35 or to support patients in post‐operative cataract care,32 as these tasks were perceived to be outside the scope of their work. One study highlighted that poor correspondence from tertiary services after ophthalmic surgery was associated with 47 of 221 patients (21%) not receiving follow‐up care after treatment for ocular trauma.22
Cultural support
Different types of cultural support were identified, including acting as a bridge between eye health services and the community, cultural mediation in consultation with eye care practitioners,25,26,33,35,38,41 explaining and interpreting health information,17,23,36,37 providing cultural knowledge support,23,24 and improving cultural competence among non‐Indigenous clinicians.30 Providers of cultural support included AHWs,17,23,24,26 community‐based liaison officers,23,24,25,41 eye health coordinators,30 family members,17,36,39 Elders,23 interpreters,23 and Indigenous reference group members.28 Several studies noted that different types of cultural mediation prompted and facilitated attendance at eye care clinics,25,26,30,33,35,38,41 as well as improving patients’ understanding of medical processes.17 Cultural assistance from Elder groups and interpreters in chronic disease care23 and from community liaison officers in trachoma control24 was reported, although this type of support was often unpaid.24 In one study in the NT, involving an Indigenous Elders committee was found to improve integrated chronic disease services;23 another NT study described the assistance of Indigenous interpreters in translating trachoma control surveys in schools.36 Interpreting assistance provided by AHWs during the development of a health promotion video improved knowledge about diabetic retinopathy in 27 of 84 Indigenous patients in Western Australia.37
Health promotion
Consulting AHWs,19 community members,37 and Indigenous consultative group members28 provided support for health promotion by designing materials or strategies regarding trachoma,28 visual impairment,19 and diabetic retinopathy37 that ensured cultural and linguistic appropriateness. Several studies noted that the support of AHWs, school staff,21,24,36,39 and family members36 were integral to trachoma control programs, including delivering and maintaining hygiene information. Conversely, lack of community involvement was a barrier to effective control programs. One study reported that inadequate clarity about the role of AHWs in school‐based trachoma initiatives was a barrier to eliminating the disease.24 A survey of community stakeholders about knowledge, attitudes and practices found that 33% of school staff believed that young children having eye and nose secretions every day was normal, posing a major barrier to trachoma elimination.39 Two studies suggested that fostering principals and teachers as trachoma educators could increase awareness, engagement, and knowledge in Indigenous communities.36,39
Social and emotional support
Social and emotional support included escorting and sitting with patients while attending eye care outside their communities12,17,41 and providing post‐operative home care support, including delivering meals to patients.41 Hospital‐based Aboriginal Liaison Officers, support workers, carers, and family members were identified as key providers of social and emotional support,12,17,41 and were reported to improve patient attendance at specialist care appointments.17,41 A Queensland study introduced community liaison officers to assist patients who had no carer to accompanying them to cataract surgery, and a home support team that delivered meals and social support to patients after surgery.41
Discussion
Our systematic review collated evidence about non‐clinical support for preventive, primary, and tertiary eye care for Indigenous Australians. Providers of non‐clinical support are both health system‐based (clinicians, coordinators, administrators), and community‐based (Elders, family, school staff). We found that patient liaison and case management is central to the coordination of eye care services,12 particularly given patient distrust and fear of cataract surgery.10,34 A key finding was the prominent role of eye health coordinators in providing these types of non‐clinical support. However, eye health coordinators are often employed part‐time,11,27 which may be attributable to the complex funding arrangements for eye health coordination through government initiatives such as the Visiting Optometry Scheme, the Medical Specialist Outreach Assistance Program, and the Indigenous Chronic Disease Package, as well as through non‐governmental initiatives.24 A 2013 study42 found that the total annual cost for coordinating eye care (treatment of refractive error, cataract, diabetic retinopathy) was $21.3 million. The 2019 update of the Roadmap to Close the Gap for Vision report13 stated that achieving targets for workforce resources for eye health, including eye care support and case management personnel, is still incomplete for most regions.
Because the numbers of eye care support personnel are limited, AHWs, primary care clinicians, administrators, transport drivers, Elders, and family and community members provide non‐clinical support to fill gaps in care. While the need for culturally responsive health services for Indigenous Australians is acknowledged,43 the levels of cultural mediation and interpreting in practice are poor.10 This may be because of the restricted availability of Indigenous interpreters44 and the shift in the role of AHWs from providing cultural support to activities requiring greater clinical skills and responsibilities.45,46 The limited availability of personnel to fulfil the linguistic and cultural needs of patients has reportedly resulted in burnout among the declining number of AHWs who act as both family or community members and clinicians.47 Cultural liaison officers and advisors can also facilitate cultural safety, but the lack of specific funding and supportive programs are barriers to establishing such positions. The author of one study10 found that the lack of funding for these roles reflects the general tendency in Australian public health systems to disregard or oversimplify Indigenous cultural heterogeneity and associated needs, and that this is directly linked with poorer eye health outcomes. Placing Elders and Indigenous health service staff in authoritative cultural knowledge positions in renal4 and sexual health48 services has been found to foster cultural awareness in non‐Indigenous staff. However, because of the challenges discussed above, service providers should consider additional strategies for increasing cultural safety and community engagement in eye care.
A study of the engagement of Canadian indigenous people (Cree) with tele‐ophthalmology clinics described initiatives for overcoming linguistic and cultural barriers, including employing nurses fluent in Cree, incorporating cultural artefacts into clinic screening protocols, and introducing a cultural space (tepee), whereby Cree Elders played a key role in health promotion initiatives. The program increased the tele‐ophthalmology clinic attendance rate from 20% to 50% in the first and to 85% in the second year of its operation.49 In the Indigenous Australian context, actively seeking collaboration with Elders has built trust and engaged the community in food security50 and mental health initiatives.51 Community health networks have improved community engagement in cancer care by demystifying screening processes, responding to the fears of patients and barriers to care, and assisting community members build relationships with others with similar health concerns.52
Having family members, carers, or escorts present during ophthalmic care appointments improves patient attendance and communication with health staff.17,20,41 Dedicated funding for escorts to accompany patients to ophthalmic surgery is available in all states, but only NSW and Victoria provide escorts with financial assistance for social, emotional or cultural support alone. The lack of this support in other jurisdictions is a key barrier to family‐centred and culturally appropriate specialist eye care.
Limitations
Our systematic review was limited to peer‐reviewed publications, and therefore did not include potentially relevant grey literature articles.
Conclusion
Non‐clinical support is critical to maximising patient attendance at appointments and the accessibility of preventive, primary, and tertiary eye care services for Indigenous Australians. The capacity of staff to provide these important services is currently limited. We recommend financial investment to support key providers of non‐clinical support, particularly eye health coordinators, community‐based liaison staff, and family members and carers. However, sustainable policies and additional resources are required to facilitate such support. Improving access to cultural mediation, interpreting, and social and emotional support is needed in all areas of Indigenous health, and current deficiencies reflect barriers in the health system in general. Further, our review highlights the disjuncture between acknowledging the important roles of family and community members in supporting the access of Indigenous Australians to health care and providing the specific resources and programs essential for supporting these roles. Improving the availability of and access to community‐based cultural mediators, liaison support and advisors, and Indigenous language interpreters, as well as integrating the roles of Elders and family and community members into clinical care, would improve access to non‐clinical support for eye care for Indigenous Australians.
Box 1 – Search terms for identifying publications included in our systematic review
#1 Health (health or well* or ill* or disease* or “health care” or patient* or hospital* or treatment* or medic* or pain* or chronic) AND#2 Australian context (Australi* or “New South Wales” or Queensland or “Northern Territory” or “WA” or “SA” or Tasmania or Victoria* or “ACT” or “NSW”) AND#3 Indigenous context (Indigen* or Aborigin* or Koori or Murri or “Torres Strait” or “Oceanic Ancestry Group”) AND#4 Eye care (eye care or blindness or ocular or optom* or ophthal* or refractive error or myop* or visual acuit* or vision screening* or visual impairment or vision impairment or eye‐care or vision care or visually impair* or amblyop* or cataract* or spectacle* or eyeglass* or glasses or vision or trachoma or trichiasis)Box 2 – Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) flow chart of our systematic review process
Box 3 – Characteristics of the 27 publications included in our systematic review
|
Study |
Year |
Location |
Participants |
Methods |
Overall study |
Quality assessment* |
|||||||||
|
|
|||||||||||||||
|
Gruen17 |
2001 |
NT |
22 clinicians, 3 patients |
Interviews and clinical audit |
— |
0.80 |
|||||||||
|
McDermott18 |
2001 |
Qld |
678 people with diabetes |
Randomised cluster trial |
— |
0.87 |
|||||||||
|
King19 |
2003 |
SA |
3 Aboriginal health workers |
Health promotion intervention |
— |
0.45 |
|||||||||
|
Gruen20 |
2006 |
NT |
2368 patients |
Population‐based observational study |
— |
0.95 |
|||||||||
|
Mak21 |
2006 |
NT, WA |
95 people involved in trachoma control |
Interviews, prevalence data |
— |
0.73 |
|||||||||
|
Smith22 |
2006 |
Qld |
226 patients |
Retrospective audit |
— |
0.90 |
|||||||||
|
Bailie23 |
2007 |
NT |
12 health centres |
Quality improvement intervention |
|
1.00 |
|||||||||
|
Wright24 |
2010 |
NT |
11 health clinic staff, one GP, one paediatrician, one ophthalmologist, one school principal |
Interviews |
— |
0.72 |
|||||||||
|
Turner25 |
2011 |
NSW, NT, Qld, SA, WA |
9 outreach ophthalmology services including nurses, clinic clerical staff, Aboriginal Health Workers, hospital staff, optometrists, ophthalmologists, eye service managers, and regional eye health coordinators |
Cross‐sectional case study |
IEHS |
0.65 |
|||||||||
|
Turner26 |
2011 |
NSW, NT, Qld, SA, WA, VIC, Tas |
1189 patients |
Randomised cluster trial, survey |
IEHS |
0.98 |
|||||||||
|
Anjou27 |
2012 |
NSW, NT, Qld, SA, WA, VIC |
530 clinicians, government/non‐government stakeholders, community members |
Interviews, focus groups |
IEHS |
0.75 |
|||||||||
|
Baunach28 |
2012 |
NT |
87 ACCHS, government stakeholders, 12 Indigenous reference group members |
Health promotion intervention |
TETS |
0.40 |
|||||||||
|
Harch29 |
2012 |
WA |
2351 baseline patients, 2471 follow up patients |
Clinical audit |
— |
0.82 |
|||||||||
|
Maher30 |
2012 |
NSW |
43 eye health service providers |
Interviews, cataract surgery rates |
— |
0.67 |
|||||||||
|
Anjou31 |
2013 |
NSW, NT, Qld, SA, WA, VIC |
81 community members, 98 ACCHS staff, 14 health clinic staff, 31 optometrists, 25 ophthalmologists, 35 hospital staff, 10 GP division staff, 16 non‐government staff, 50 government staff |
Interviews, focus groups |
IEHS |
0.75 |
|||||||||
|
Anjou11 |
2013 |
NSW, NT, Qld, SA, WA, VIC |
81 community members, 98 ACCHS staff, 14 health clinic staff, 31 optometrists, 25 ophthalmologists, 35 hospital staff, 10 GP division staff, 12 NACCHO staff, 29 government staff |
Interviews, focus groups |
IEHS |
0.88 |
|||||||||
|
Boudville32 |
2013 |
NSW, NT, Qld, SA, WA, VIC |
81 community members, 98 ACCHS staff, 14 health clinic staff, 31 optometrists, 25 ophthalmologists, 35 hospital staff, 10 GP division staff, 12 NACCHO staff, 29 government staff, 116 unclassified stakeholders |
Interviews, focus groups |
IEHS |
0.63 |
|||||||||
|
Boudville33 |
2013 |
NSW, NT, Qld, SA, WA, VIC |
98 ACCHS staff, 14 health clinic staff, 31 optometrists, 25 ophthalmologists, 35 hospital staff, 10 GP division staff, 12 NACCHO staff, 29 government staff, 116 unclassified stakeholders |
Interviews, focus groups |
IEHS |
0.75 |
|||||||||
|
Boudville34 |
2013 |
NSW, NT, Qld, SA, WA, VIC |
530 clinicians, government/non‐government stakeholders, community members |
Interviews, focus groups |
IEHS |
0.85 |
|||||||||
|
Hsueh12 |
2013 |
NSW, NT, Qld, SA, WA, VIC |
530 clinicians, government/non‐government stakeholders, community members |
Interviews, focus groups |
IEHS |
0.70 |
|||||||||
|
Tapp35 |
2013 |
NSW, NT, Qld, SA, WA, VIC |
370 clinicians, unclassified stakeholders |
Interviews |
IEHS |
0.55 |
|||||||||
|
Lange36 |
2014 |
NT |
72 ACCHS clinic staff members |
Knowledge Attitudes Practices survey |
TETS |
0.74 |
|||||||||
|
Meyer37 |
2016 |
WA |
84 patients |
Pre‐, post‐intervention questionnaires |
— |
0.69 |
|||||||||
|
Copeland38 |
2017 |
WA |
69 patients, 8 clinicians |
Interviews |
— |
0.78 |
|||||||||
|
Lange39 |
2017 |
NT |
272 baseline participants, 261 follow up participants (health clinic staff, school staff) |
Cross‐sectional pre‐post intervention survey |
TETS |
0.95 |
|||||||||
|
Moynihan40 |
2017 |
WA |
974 patients |
Intervention and retrospective audit |
— |
0.82 |
|||||||||
|
Penrose41 |
2018 |
Qld |
55 patients before, 103 patients after the intervention |
Intervention and retrospective audit |
— |
0.77 |
|||||||||
|
|
|||||||||||||||
|
ACCHS = Aboriginal Community Controlled Health Services; IEHS = Indigenous Eye Health Survey; NACCHO = National Aboriginal Community Controlled Health Organisation; TETS = Trachoma Elimination Toolkit Study. * Two independent reviewers used the QualSyst tool for mixed method studies.16 |
|||||||||||||||
Received 29 July 2019, accepted 13 November 2019
- Aryati Yashadhana1,2
- Ling Lee1,2
- Jessica Massie2
- Anthea Burnett1,2
- 1 University of New South Wales, Sydney, NSW
- 2 Brien Holden Vision Institute, Sydney, NSW
We acknowledge the Fred Hollows Foundation, who advised us during the initial design of the study.
The Fred Hollows Foundation financially supported the preparation of this review.
- 1. Aspin C, Brown N, Jowsey T, et al. Strategic approaches to enhanced health service delivery for Aboriginal and Torres Strait Islander people with chronic illness: a qualitative study. BMC Health Serv Res 2012; 12: 143.
- 2. Cass A, Lowell A, Christie M, et al. Sharing the true stories: improving communication between Aboriginal patients and healthcare workers. Med J Aust 2002; 176: 466–471. https://www.mja.com.au/journal/2002/176/10/sharing-true-stories-improving-communication-between-aboriginal-patients-and.
- 3. Kelly J, Dwyer J, Mackean T, et al. Managing two worlds together. Study 3: The experiences of patients and their carers. Melbourne: Lowitja Institute, 2011. http://www.flinders.edu.au/medicine/fms/sites/health_care_management/mtwt/documents/Study%203_WEB.pdf (viewed Nov 2019).
- 4. Rix EF, Barclay L, Stirling J, et al. The perspectives of Aboriginal patients and their health care providers on improving the quality of hemodialysis services: a qualitative study. Hemodial Int 2015; 19: 80–98.
- 5. Smith K, Flicker L, Shadforth G, et al. “Gotta be sit down and worked out together”: views of Aboriginal caregivers and service providers on ways to improve dementia care for Aboriginal Australians. Rural Remote Health 2011; 11: 1650.
- 6. Abbott P, Davison J, Moore L, Rubinstein R. Barriers and enhancers to dietary behaviour change for Aboriginal people attending a diabetes cooking course. Health Promot J Austr 2010; 21: 33–38.
- 7. Foreman J, Keel S, Xie J, et al. The National Eye Health Survey 2016. Melbourne: Centre For Eye Research Australia; Vision 2020, 2016. https://www.cera.org.au/wp-content/uploads/2016/10/National-Eye-Health-Survey_Full-Report_FINAL-V3.pdf (viewed Nov 2019).
- 8. Kirby Institute. Australian trachoma surveillance report 2015. Sydney: UNSW, 2015. https://kirby.unsw.edu.au/sites/default/files/kirby/report/Australian-Trachoma-Surveillance-Report-2015.pdf (viewed Nov 2019).
- 9. Taylor HR, Boudville AI, Anjou MD, McNeil RJ. The roadmap to Close the Gap for Vision (full report). Melbourne: Melbourne School of Population Health, University of Melbourne, 2012. https://mspgh.unimelb.edu.au/__data/assets/pdf_file/0008/1984166/roadmap_full_report.pdf (viewed Nov 2019).
- 10. Yashadhana A. The patient experience in eye care study: an exploration of the sociocultural and political determinants of diabetic eye care in rural Aboriginal communities [thesis]. University of New South Wales, 2019. http://handle.unsw.edu.au/1959.4/61532 (viewed Nov 2019).
- 11. Anjou MD, Boudville AI, Taylor HR. Local co‐ordination and case management can enhance Indigenous eye care: a qualitative study. BMC Health Serv Res 2013; 13: 255.
- 12. Hsueh YS, Dunt D, Anjou MD, et al. Close the gap for vision: the key is to invest on coordination. Aust J Rural Health 2013; 21: 299–305.
- 13. Indigenous Eye Health Unit. Annual update on the implementation of the roadmap to Close the Gap for Vision. Nov 2019. https://mspgh.unimelb.edu.au/__data/assets/pdf_file/0011/3222893/2019-AnnualUpdate.pdf (viewed Nov 2019).
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG; the PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: the PRISMA statement. BMJ 2009; 339: b2535.
- 15. Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. London: Routledge, 2009.
- 16. Kmet L, Lee RC, Cook LS. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Edmonton (AL): Alberta Heritage Foundation for Medical Research, 2004. https://www.ihe.ca/download/standard_quality_assessment_criteria_for_evaluating_primary_research_papers_from_a_variety_of_fields.pdf (viewed Nov 2019).
- 17. Gruen RL, Bailie RS, d'Abbs PH, et al. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust 2001; 174: 507–511.
- 18. McDermott RA, Schmidt BA, Sinha A, Mills P. Improving diabetes care in the primary healthcare setting: a randomised cluster trial in remote Indigenous communities. Med J Aust 2001; 174: 497–502.
- 19. King M, Baxter S. Co‐operative inquiry: the development of a visual impairment prevention program initiative for two Aboriginal communities in South Australia. Contemp Nurse 2003; 15: 241–248.
- 20. Gruen RL, Bailie RS, Wang Z, et al. Specialist outreach to isolated and disadvantaged communities: a population‐based study. Lancet 2006; 368: 130–138.
- 21. Mak DB, O'Neill LM, Herceg A, McFarlane H. Prevalence and control of trachoma in Australia, 1997–2004. Commun Dis Intell Q Rep 2006; 30: 236–247.
- 22. Smith AR, O'Hagan SB, Gole GA. Epidemiology of open‐ and closed‐globe trauma presenting to Cairns Base Hospital. Queensland. Clin Exp Ophthalmol 2006; 34: 252–259.
- 23. Bailie R, Si D, Dowden M, et al. Improving organisational systems for diabetes care in Australian Indigenous communities. BMC Health Serv Res 2007; 7: 67.
- 24. Wright HR, Keeffe JE, Taylor HR. Barriers to the implementation of the SAFE strategy to combat hyperendemic trachoma in Australia. Ophthalmic Epidemiol 2010; 17: 349–359.
- 25. Turner AW, Mulholland WJ, Taylor HR. Coordination of outreach eye services in remote Australia. Clin Exp Ophthalmol 2011; 39: 344–349.
- 26. Turner AW, Xie J, Arnold AL, et al. Eye health service access and utilization in the National Indigenous Eye Health Survey. Clin Exp Ophthalmol 2011; 39: 598–603.
- 27. Anjou MD, Boudvile AI, Taylor HR. We can see the gap: regional eye health coordination for Indigenous Australians. Aborig Isl Health Work J 2012; 36: 12–16.
- 28. Baunach E, Lines D, Pedwel B, et al. The development of culturally safe and relevant health promotion resources for effective trachoma elimination in remote Aboriginal communities. Aborig Isl Health Work J 2012; 36: 9–11.
- 29. Harch S, Reeve D, Reeve C. Management of type 2 diabetes: a community partnership approach. Aust Fam Physician 2012; 41: 73–76.
- 30. Maher L, Brown AM, Torvaldsen S, et al. Eye health services for Aboriginal people in the western region of NSW, 2010. NSW Public Health Bull 2012; 23: 81–86.
- 31. Anjou MD, Boudville AI, Taylor HR. Correcting Indigenous Australians’ refractive error and presbyopia. Clin Exp Ophthalmol 2013; 41: 320–328.
- 32. Boudville AI, Anjou MD, Taylor HR. Eye health promotion to improve awareness and prevent vision loss among Indigenous Australians. Health Promot J Aust 2013; 24: 76–77.
- 33. Boudville AI, Anjou MD, Taylor HR. Improving eye care for Indigenous Australians in primary health care settings. Aust J Rural Health 2013; 21: 121–127.
- 34. Boudville AI, Anjou MD, Taylor HR. Indigenous access to cataract surgery: an assessment of the barriers and solutions within the Australian health system. Clin Exp Ophthalmol 2013; 41: 148–154.
- 35. Tapp RJ, Anjou MD, Boudville AI, Taylor HR. The roadmap to close the gap for vision: diabetes‐related eye care in the Indigenous Australian population. Diabet Med 2013; 30: 1145–1146.
- 36. Lange FD, Baunach E, McKenzie R, Taylor HR. Trachoma elimination in remote Indigenous Northern Territory communities: baseline health‐promotion study. Aust J Prim Health 2014; 20: 34–40.
- 37. Meyer J, Johnson K, Bowyer J, et al. Evaluating a health video on diabetic retinopathy. Health Promot J Aust 2016; 27: 84–87.
- 38. Copeland S, Muir J, Turner A. Understanding Indigenous patient attendance: a qualitative study. Aust J Rural Health 2017; 25: 268–274.
- 39. Lange FD, Jones K, Ritte R, et al. The impact of health promotion on trachoma knowledge, attitudes and practice (KAP) of staff in three work settings in remote Indigenous communities in the Northern Territory. PLoS Negl Trop Dis 2017; 11: e0005503.
- 40. Moynihan V, Turner A. Coordination of diabetic retinopathy screening in the Kimberley region of Western Australia. Aust J Rural Health 2017; 25: 110–115.
- 41. Penrose L, Roe Y, Johnson NA, James EL. Process redesign of a surgical pathway improves access to cataract surgery for Aboriginal and Torres Strait Islander people in South East Queensland. Aust J Prim Health 2018; 24: 135–140.
- 42. Hsueh Y, Brando A, Dunt D, et al. Cost of close the gap for vision of Indigenous Australians: on estimating the extra resources required. Aust J Rural Health 2013; 21: 329–335.
- 43. Australian Health Ministers’ Advisory Council. Cultural respect framework 2016–2026. A national approach to building a culturally respectful health system. 2016. http://www.coaghealthcouncil.gov.au/Portals/0/National%20Cultural%20Respect%20Framework%20for%20Aboriginal%20and%20Torres%20Strait%20Islander%20Health%202016_2026_2.pdf (viewed Nov 2019).
- 44. Ralph AP, Lowell A, Murphy J, et al. Low uptake of Aboriginal interpreters in healthcare: exploration of current use in Australia's Northern Territory. BMC Health Serv Res 2017; 17: 733.
- 45. Willis E. From cultural brokers to shared care: the changing position of literacy for Aboriginal health workers in Central Australia. Stud Contin Educ 1999; 21: 163–175.
- 46. Abbott P, Gordon E, Davison J. Expanding roles of Aboriginal health workers in the primary care setting: seeking recognition. Contemp Nurse 2008; 27: 157–164.
- 47. Topp SM, Edelman A, Taylor S. “We are everything to everyone”: a systematic review of factors influencing the accountability relationships of Aboriginal and Torres Strait Islander health workers (AHWs) in the Australian health system. Int J Equity Health 2018; 17: 67.
- 48. Kelly J, Luxford Y. Yaitya tirka madlanna warratinna: exploring what sexual health nurses need to know and do in order to meet the sexual health needs of young Aboriginal women in Adelaide. Collegian 2007; 14: 15–20.
- 49. Arora S, Kurji AK, Tennant MTS. Dismantling sociocultural barriers to eye care with tele‐ophthalmology: lessons from an Alberta Cree community. Clin Invest Med 2013; 36: E57–E63.
- 50. Brimblecombe J, van den Boogaard C, Ritchie J, et al. From targets to ripples: tracing the process of developing a community capacity building appraisal tool with remote Australian indigenous communities to tackle food security. BMC Public Health 2014; 14: 914.
- 51. Isaacs AN, Maybery D, Gruis H. Mental health services for Aboriginal men: mismatches and solutions. Int J Ment Health Nurs 2012; 21: 400–408.
- 52. Cuesta‐Briand B, Bessarab D, Shahid S, Thompson SC. “Connecting tracks’”: exploring the roles of an Aboriginal women's cancer support network. Health Soc Care Community 2016; 24: 779–788.





Abstract
Objectives: To describe research into non‐clinical support eye health care for Aboriginal and Torres Strait Islander (Indigenous) Australians, the people who provide such care, and its impact on eye health outcomes.
Study design: Systematic review and qualitative analysis of peer‐reviewed research publications.
Data sources: Peer‐reviewed research articles published between January 2000 and July 2018 and included in MEDLINE/EMBASE, Web of Science, Informit, EBSCO (CINAHL and Anthropology Plus), or ProQuest Central.
Study selection: We included English language, peer‐reviewed articles reporting empirical data on non‐clinical support for eye health for Indigenous Australians. Two authors independently assessed the titles and abstracts of 1678 unique articles for inclusion in a full text review; the full texts of 104 publications were reviewed, of which 77 were excluded and 27 included in our qualitative analysis.
Data synthesis: Qualitative analysis identified five key areas of non‐clinical support for Indigenous eye health: coordination of eye care, integrating and linking services, cultural support, health promotion, and social and emotional support. People who provide non‐clinical support include eye health coordinators, Aboriginal Health Workers, primary care clinicians, family members, carers, and community‐based liaison workers. The availability of non‐clinical support is associated with increased patient attendance at eye care services, higher visual acuity examination and cataract surgery rates, broader eye health knowledge, and greater cultural responsivity.
Conclusion: Non‐clinical support is critical for facilitating attendance at appointments by patients and ensuring that preventive, primary, and tertiary eye care services are accessible to Indigenous Australians. Greater financial investment is needed to support key providers of non‐clinical support, especially eye health coordinators, community‐based liaison officers, and family members and carers.