Doctor–patient communication, by creating good interpersonal relationships, allowing the exchange of information and facilitating treatment-related decisions, is fundamental to optimal medical care.1 Effective communication correlates with improved outcomes, including physiological criteria such as levels of blood pressure and blood sugar.2 Conversely, professional, language and cultural barriers can impede communication.3,4
Few investigators have studied the extent and consequences of miscommunication in Australian Aboriginal healthcare,5 an area in which effective communication is extremely important.6 Previous studies involving interviews with service providers and Aboriginal patients have identified significant concerns about communication.7-9 Some researchers have identified an acceptance, as the norm, of a grossly deficient standard of cross-cultural communication.8 We believe that previous studies, based as they have been on indirect reporting or simulated interactions10 (rather than direct observation and analysis of the interaction itself), probably understate the degree of miscommunication. The communication gap may be so wide, and so ingrained in healthcare, that it is not even perceived by staff.11 Similar misunderstandings in Australian court cases often go unrecognised by the participants.12
In our study of staff–patient interactions in a dialysis unit in Darwin, NT, we attempted to develop a more informed understanding of intercultural communication between Aboriginal patients and non-Aboriginal staff and to devise strategies for improvement.
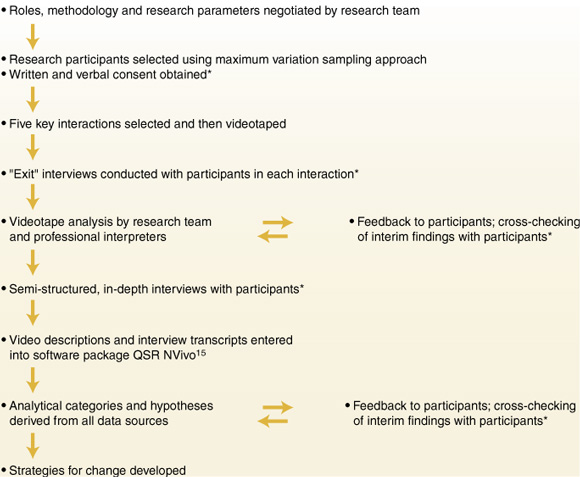
We used qualitative research methods to reflect the perspectives of all participants. The research design drew on "grounded theory", which describes the inductive process of identifying analytical categories to describe and explain key issues as they emerge from the data.13 Hypotheses were developed from the ground up, rather than being defined a priori, as is usually done in quantitative research.
Recognising that the effectiveness of communication is inextricably connected with structural issues of poverty, dispossession, marginalisation, low educational achievement and racial discrimination,7 we chose a "participatory action" approach. This is a style of research in which the demarcation between "researcher" and "subject" is blurred, research design is negotiated, and the participants perceive the need to change and are willing to participate actively in the change process.14 The research process is illustrated in Box 1.
We selected participants using a "maximum variation sampling approach", wherein a small sample is selected to reflect maximum diversity across specified attributes.16 The participants covered as wide a range as possible in terms of age, sex, duration of renal experience (receiving or providing treatment), degree of familiarity with the culture and language of the other group, and experience in cross-cultural communication.
The video descriptions and interview transcripts were entered into QSR NVivo,15 a computer software package that assists in managing qualitative data. Categories used in analysis were derived primarily from the data and through sequential analysis. To strengthen the validity of our analysis, we used "triangulation" (the comparison of results from two or more different methods of data collection) and "respondent validation" (cross-checking interim findings with the participants).17,18
A picture emerged of serious miscommunication, often unrecognised by participants, regarding fundamental issues in diagnosis, treatment and prevention. Although there were many differences of goals and structure observed in the interactions, common themes relating to miscommunication emerged. Factors impeding communication included lack of control by the patient, differing modes of discourse, dominance of the biomedical model, lack of shared knowledge and understanding, cultural and linguistic distance, lack of staff training in inter-cultural communication, and failure to call on trained interpreters (see Box 2 and Box 3).
Western modes of discourse dominated, with Yolngu modes being marginalised or excluded. Question-and-answer routines, central to Western discourse, do not feature commonly in Yolngu discourse, particularly in relation to personal topics. In Yolngu discourse, the question-and-answer approach is complicated by factors such as cultural restrictions on who may ask for, or give, specific information. It is generally considered impolite to directly contradict or to respond negatively, particularly in encounters of unequal power or when the participants lack a close relationship. The patients in our study repeatedly gave responses that they believed the staff wanted to hear, a practice known in linguistics as "gratuitous concurrence".19 Triangulation showed that these responses did not represent the patient's true feelings or experience, but were attempts to give "required" or "correct" responses, as in the following example:
Physician: How much are you drinking? How much water?
Patient: Little bit water tea, little bit ga bilin ["that's it"].
Physician: How much each day? Water, tea?
Patient: Three cup, two cup, little bit [said very confidently].
And yet he found that intercultural communication was
There were organisational barriers to formal training, as a renal nurse related:
Until recently, there was no alternative to attempting whatever communication was possible through the assistance of whoever was available. In the absence of professional interpreters, family members had to suffice — a seriously inadequate practice.20 Although an Aboriginal Interpreter Service providing Yolngu language speakers now exists, changes in practice are occurring only slowly. In the interactions observed in our study, the closest any of the staff or patients came to seeking the assistance of a professional interpreter was to call on the assistance of a family member who had some informal interpreting experience.
Videotaping the interactions did not appear to fundamentally alter the communication strategies used by staff. In any case, we would expect any bias, arising through participants' knowledge of being observed, to be towards more effective rather than less effective communication. Our results support similar findings of miscommunication in other Aboriginal health research8,11,21 and in international cross-cultural research.1,3 We believe that our research findings are both credible and relevant to the delivery of healthcare to Aboriginal people, and that similar miscommunication problems are likely to exist in other healthcare settings in which there are people whose first language is not English.
Fundamental change is required to achieve effective communication with Aboriginal patients who have renal disease. We will not be able to deliver optimal care without striking a balance between the staff's medical priorities and the patients' social needs. Some strategies for improving communication are set out in Box 4. Planning and implementing such strategies for the Yolngu will require collaboration between staff, patients and patients' families. We are currently developing such a project. Short of such radical change, attempts to improve communication can meet with only limited success.
Setting: The doctor's office in a remote community 500 kilometres from Darwin.
Communication goals: Dr B had clear goals:
The participants' assessment: Dr B was uncertain of the outcome of the interaction:
Setting: The open waiting area at the dialysis unit.
Neither participant mentioned what Ms C might have wanted to communicate.
- Alan Cass1
- Anne Lowell2
- Michael Christie3
- Paul L Snelling4
- Melinda Flack5
- Betty Marrnganyin6
- Isaac Brown7
- Cooperative Research Centre for Aboriginal and Tropical Health, NT.
Our study was supported by a grant from the Cooperative Research Centre for Aboriginal and Tropical Health. We would like to thank Dr Peter Arnold for his critical reading of the manuscript.
None declared.
- 1. Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor–patient communication: a review of the literature. Soc Sci Med 1995; 40: 903-918.
- 2. Stewart MA. Effective physician–patient communication and health outcomes: a review. CMAJ 1995; 152: 1423-1433.
- 3. Putsch RW. Cross-cultural communication. The special case of interpreters in health care. JAMA 1985; 254: 3344-3348.
- 4. Dollis N. Removing cultural and language barriers to health. Melbourne: National Health Strategy, 1993.
- 5. Lowell A. Communication and cultural knowledge in Aboriginal health care. Darwin: Cooperative Research Centre for Aboriginal and Tropical Health, 2001.
- 6. Australian Royal Commission into Aboriginal Deaths in Custody (Commissioner E Johnston). National report: overview and recommendations. Canberra: AGPS, 1991.
- 7. Humphery K, Weeramanthri T, Fitz J. Forgetting compliance: Aboriginal health and medical culture. Darwin: Northern Territory University Press in conjunction with the Cooperative Research Centre for Aboriginal and Tropical Health, 2001.
- 8. Devitt J, McMasters A. Living on medicine: a cultural study of end-stage renal disease among Aboriginal people. Alice Springs: IAD Press, 1998.
- 9. Mobbs R. But I do care! Communication difficulties affecting the quality of care delivered to Aborigines. Med J Aust 1986; 144(Suppl): S3-S5.
- 10. Edis F. "Just scratching the surface": miscommunication in Aboriginal health care. MEd thesis, Northern Territory University, 1998.
- 11. Trudgen R. Why warriors lie down and die. Darwin: Aboriginal Resource and Development Services Inc., 2000.
- 12. Cooke M. Anglo/Yolngu communication in the criminal justice system. PhD thesis, University of New England, 1998.
- 13. Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ 2000; 320: 114-116.
- 14. Meyer J. Qualitative research in health care. Using qualitative methods in health related action research. BMJ 2000; 320: 178-181.
- 15. QSR NVivo [computer program]. Version 1.2.42. Melbourne: QSR International Pty Ltd, 1999–2000.
- 16. Higginbotham N, Albrecht G, Connor L. Health social science: a transdisciplinary and complexity perspective. Melbourne: Oxford University Press, 2001.
- 17. Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ 2000; 320: 50-52.
- 18. Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ 2001; 322: 1115-1117.
- 19. Eades D. Communicative strategies in Aboriginal English. In: Romaine S, editor. Language in Australia. Cambridge: Cambridge University Press, 1991.
- 20. Campbell DA. Hope and harm: a delicate balance [commentary]. Med J Aust 2001; 175: 540-541.
- 21. Steffensen MS, Colker L. Intercultural misunderstandings about health care. Recall of descriptions of illness and treatment. Soc Sci Med 1982; 16: 1949-1954.





Abstract
Objectives: To identify factors limiting the effectiveness of communication between Aboriginal patients with end-stage renal disease and healthcare workers, and to identify strategies for improving communication.
Design: Qualitative study, gathering data through (a) videotaped interactions between patients and staff, and (b) in-depth interviews with all participants, in their first language, about their perceptions of the interaction, their interpretation of the video record and their broader experience with intercultural communication.
Setting: A satellite dialysis unit in suburban Darwin, Northern Territory. The interactions occurred between March and July 2001.
Participants: Aboriginal patients from the Yolngu language group of north-east Arnhem Land and their medical, nursing and allied professional carers.
Main outcome measures: Factors influencing the quality of communication.
Results: A shared understanding of key concepts was rarely achieved. Miscommunication often went unrecognised. Sources of miscommunication included lack of patient control over the language, timing, content and circumstances of interactions; differing modes of discourse; dominance of biomedical knowledge and marginalisation of Yolngu knowledge; absence of opportunities and resources to construct a body of shared understanding; cultural and linguistic distance; lack of staff training in intercultural communication; and lack of involvement of trained interpreters.
Conclusions: Miscommunication is pervasive. Trained interpreters provide only a partial solution. Fundamental change is required for Aboriginal patients to have significant input into the management of their illness. Educational resources are needed to facilitate a shared understanding, not only of renal physiology, disease and treatment, but also of the cultural, social and economic dimensions of the illness experience of Aboriginal people.