The known: Australians are searching the internet for health care advice with increasing frequency. Symptom checkers are common online tools for obtaining diagnostic and triage advice.
The new: Thirty‐six symptom checkers were evaluated with a range of clinical vignettes. The correct diagnosis was listed first in 36% of tests, and included among the first ten results in 58%; triage advice was appropriate in 49% of cases, including about 60% of emergency and urgent cases but only 30–40% of less serious case vignettes.
The implications: Symptom checkers may provide unsuitable or incomplete diagnostic or triage advice for users in Australia, resulting in inappropriate care advice.
Australians generally embrace online technology: in 2016–17, 86% of households had internet access1 and about 89% of surveyed adults owned smartphones.2 An abundance of material once accessible only to subject specialists is now more readily available on websites and via smartphone applications (apps), and widespread internet access has changed health information‐seeking behaviour.3 About 80% of Australians report searching the internet for health information, and nearly 40% seek self‐treatment advice online.4,5 An Australian study6 found that 34% of people attending emergency departments had searched the internet for information about their condition.
Symptom checkers (SCs) are algorithm‐based programs that provide potential diagnoses and triage advice. Medical students routinely use diagnostic apps to support their education,7 and similar products are publicly available. SCs may not function as intended; they can encourage users to seek professional care even when self‐care would be suitable, increasing the burden on health care systems.8,9 Not all SCs are affiliated with reputable organisations,3 and concerns have been raised about data security, privacy, the credentials of app authors and editors, and the accuracy of health information.9,10 The United States Food and Drug Administration recently launched a voluntary software pre‐certification program aimed at providing assurance of effectiveness and transparency of product performance and safety.11 In Australia, the Therapeutic Goods Administration oversees the regulation of medical software products and devices, but does not regulate SCs because they are not classified as medical devices.12,13
Semigran and colleagues recently tested 23 free online SCs with standardised patient vignettes; they found that correct diagnoses headed the result list in 34% of evaluations, and appropriate triage advice was provided in 57% of cases.8 In a study in a British primary care clinic, a self‐assessment tool recommended a more urgent level of care than the general practitioner in 56% of cases and less urgent advice for only 5% of consultations.14
The aim of our study was to investigate the diagnosis and triage performance of free SCs accessible in Australia.
Methods
Symptom checkers
To identify the most prominent free online SCs in Australia, we searched for “symptom checker”, “medical diagnosis”, “health symptom diagnosis”, “symptom”, and “cough fever headache” (ie, flu‐like symptoms) with five popular search engines (Google, Yahoo, Ask, Search Encrypt, Bing) between November 2018 and January 2019. The first three pages of results for each search engine were filtered to identify SCs that were publicly available, in English, for humans, and not restricted to specific medical conditions. The two major smartphone application distribution services (Google Play [Android] and App Store [Apple]) were also searched. As app store ranking algorithms place the most popular apps at the top of search results,9 we included the first fifteen listed apps for each store. SCs were characterised as to whether they requested demographic information, by the number of diagnoses provided in responses, and by whether they claimed to use artificial intelligence (AI) algorithms.
Patient vignettes
To assess the diagnostic and triage performance of the SCs, 30 patient vignettes from the study by Semigran and colleagues8 were adapted and supplemented by 18 new symptom‐based scenarios, including several reflecting Australia‐specific illnesses (Supporting Information, table 1). Clinical information for the vignettes was drawn from medical resource websites and training material for health care professionals.8,15,16,17 The disposition advice provided by the SCs was allocated to one of four triage categories (emergency, urgent, non‐urgent, self‐care; Box 1). The “correct” diagnoses and triage advice for each vignette were confirmed by two GPs (including author MS) and an emergency department specialist with a combined 87 years’ clinical experience; disagreements related to contextual factors (eg, timing, local access to resources) were resolved by discussion. For our study, the triage category for deep vein thrombosis was deemed “urgent”, not “emergency”,8 to reflect the recent benefits of oral anticoagulant therapy. Medical conditions described were characterised as being common (85% of vignettes) or uncommon (15%: similar to the 10% reported for general practice presentations in Australia18) on the basis of Bettering the Evaluation and Care of Health (BEACH) general practice research data (2006–07 to 2015–16),19 Australian Institute of Health and Welfare emergency department care statistics (2016–17),17 and information provided by the Victorian government Better Health Channel website;16 these assessments were confirmed by the two GPs. For vignettes describing conditions with similar symptoms, several results could be deemed correct (Supporting Information, table 1).
SCs require users to enter their symptoms and, in some cases, other information. Accordingly, vignettes were summarised, in lay language, as the chief complaint and the core symptoms, and only this information was entered into the SC. To maintain consistency, one investigator entered the information for each vignette. As some SCs were specific for adult or childhood conditions, not every vignette could be evaluated in all SCs.
Symptom checker performance: diagnosis
Only the first ten results for each vignette were examined. Accurate diagnosis was defined as including the correct diagnosis as the top result, or as being among the top three or top ten potential diagnoses; “incorrect diagnosis” was defined as the correct condition not being included in the top ten results. A vignette was deemed “unassessable” if the key symptoms could not be entered. Diagnostic performance was based on 1170 assessable vignettes across the 27 SCs providing diagnostic information (Box 2).
Symptom checker performance: triage
Appropriate triage advice can be more immediately useful to patients than a probable diagnosis,20 as timely care can improve outcomes, particularly for emergency and urgent conditions. We defined triage accuracy by whether the SC provided triage advice concordant with our assessment. If several triage options were provided, the most urgent level was accepted. All triage advice was analysed, regardless of whether a diagnosis was provided. If triage advice depended on the offered diagnosis, the vignette was deemed “unassessable”. For example, Buoy Health triage advice for the appendicitis vignette ranged from “self‐care” for the diagnosis of rotavirus infection to “emergency department” for appendicitis; that is, unambiguous triage advice could not be provided based on the entered symptoms alone. Triage performance was based on 688 assessable vignettes across the 19 SCs providing triage advice (Box 2).
Data analysis
Means with 95% confidence intervals (CIs) based on the binomial distribution were calculated in SPSS 25. Diagnostic and triage accuracy by diagnosis frequency (common, uncommon), vignette triage category, and SC characteristics (AI algorithms, demographic questions, maximum number of diagnosis results) were assessed in one‐way analyses of variance (ANOVAs) and independent samples t tests. Normality of data distribution was assessed with the Shapiro–Wilk test; when non‐normally distributed, the data were log transformed. Homogeneity of variance was assessed in Levene tests; when non‐homogeneous, Welch ANOVA was used for analysis. A post hoc sensitivity analysis of triage performance excluded SCs that never recommended self‐care. Individual SC performance was expressed as separate proportions of correct results for diagnosis and triage.
Ethics approval
Our study received ethics approval from the Edith Cowan University Human Research Ethics Committee on 27 March 2018 (reference, 20312).
Results
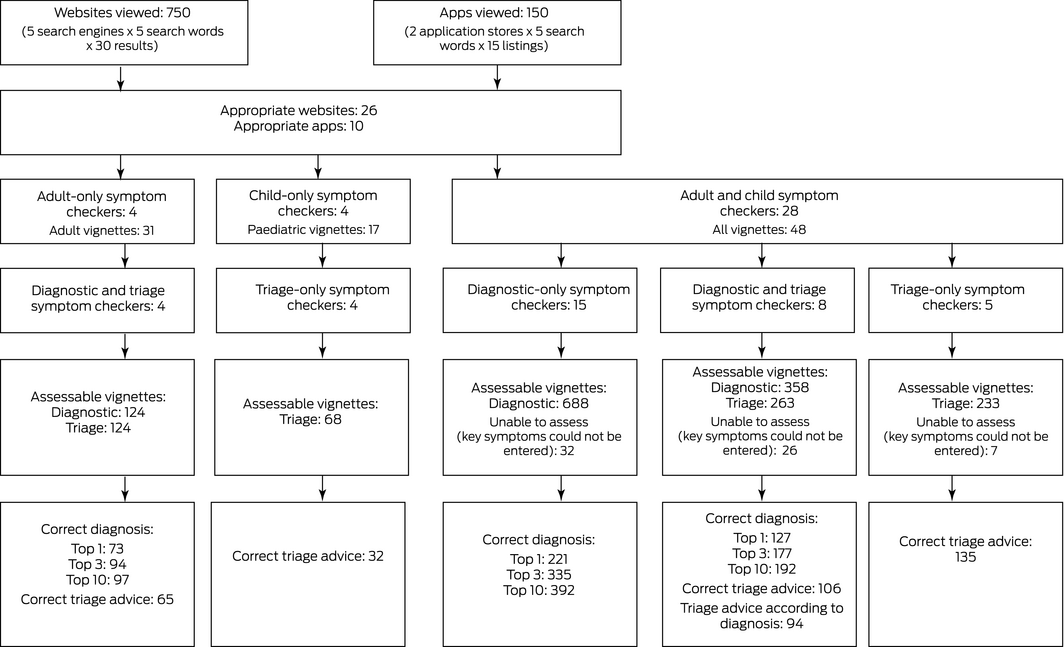
We identified 36 SCs for evaluation; ten provided both diagnostic and triage advice, 17 diagnostic information only, and nine triage advice only (Supporting Information, table 2).
Diagnostic performance
The 27 diagnostic SCs listed the correct diagnosis first in 421 of 1170 SC vignette tests (36%; 95% CI, 31–42%), among the top three results in 606 tests (52%; 95% CI, 47–59%), and among the top ten results in 681 tests (58%; 95% CI, 53–65%). The proportions of correct results listed first differed by patient condition in the vignette: emergency, 27% (95% CI, 21–34%); urgent, 45% (95% CI, 39–51%); non‐urgent, 39% (95% CI, 33–47%); and self‐care, 32% (95% CI, 25–42%). Correct diagnoses were more frequently listed first for vignettes describing common (42%; 95% CI, 37–50%) than for those describing uncommon conditions (4%; 95% CI, 1–7%) (Box 3; Supporting Information, table 3).
The eight SCs that used AI algorithms according to the suppliers also requested demographic information. These SCs listed the correct diagnosis first (46%; 95% CI, 40–57%) more frequently than the other 19 diagnostic SCs (32%; 95% CI, 26–38%). Diagnostic accuracy was not related to the maximum number of diagnoses provided by an SC (Box 4).
The performance of individual SCs in terms of correct first diagnosis ranged between 12% and 61%, and for correct diagnosis in the top ten results between 30% and 81%. Some SCs were available from different sources (website, App Store, Google Play), and the performance of the variants differed (Supporting Information, table 4).
Triage performance
The 19 triage SCs provided correct advice for 338 of 688 vignette tests (49%; 95% CI, 44–54%). Appropriate advice was more frequent for emergency care (63%; 95% CI, 52–71%) and urgent care vignette tests (56%; 95% CI, 52–75%) than for non‐urgent care (30%; 95% CI, 11–39%) and self‐care tests (40%; 95% CI, 26–49%) (Box 5; Supporting Information, table 5). The advice for 40% of non‐urgent and self‐care category vignettes was to seek urgent or emergency care, while for 10% of emergency category vignettes, non‐urgent care or self‐care was recommended (data not shown). For example, Family Doctor recommended self‐care for “acute liver failure” and non‐urgent care for “stroke”.
Four SCs (Isabel Healthcare, Everyday Health, Symcat, Doctor Diagnose) did not suggest self‐care for any vignette; excluding these tools from the analysis did not markedly increase the proportion of correct responses (275 of 528 tests, 52%; 95% CI, 48–55%). Correct triage advice was more frequent for vignettes describing common conditions (51%; 95% CI, 46–55%) than for those describing uncommon conditions (41%; 95% CI, 22–45%); the accuracy of the five SCs requiring demographic data (53%; 95% CI, 49–57%) was greater than for the 14 that did not (41%; 95% CI, 34–51%) (Box 6). Triage performance varied by SC (Supporting Information, table 6).
Discussion
In our assessment of SCs, the correct diagnosis was listed first in 36% of tests, similar to the figure of 34% reported by Semigram and colleagues;8 the correct diagnosis was included in the top ten results in 58% of our cases. Triage advice was appropriate in 49% of tests, compared with 57% reported by Semigram and colleagues.8 The proportion of correct diagnosis results was larger for programs that use AI algorithms and require demographic information. The questions and diagnosis results of SCs available on multiple platforms were not always consistent, possibly because of differences in AI algorithms or programming.
Triage advice, especially for less serious case vignettes, tended to be risk‐averse, although there were also notable instances of the opposite; the former can place unnecessary burdens on health care systems, but the latter can be dangerous. Neither we nor Semigran and colleagues8 found that omitting SCs which never suggest self‐care from analysis markedly increased the proportion of triage recommendations classified as appropriate.
The diagnostic accuracy of SCs is limited by their programming and how information is presented. For example, the core signs and symptoms in the “heart attack” vignette are chest pain, sweating, and breathlessness. The Health Tools (American Association of Retired Persons) SC found no “possible causes” for this symptom combination, but suggested 51 diagnoses for the lone symptom “chest pain”, with “heart attack” listed second. That is, diagnostic usefulness was reduced by increasing the number of symptoms entered, although the tool prompts users to enter multiple symptoms.
In a recent British National Health System study,21 20% of SC users were directed to the emergency phone number or an emergency department, suggesting that people consult online tools about urgent and emergency conditions. Health and computer literacy could affect how people use SCs,4 and this can pose challenges for patient–physician relationships if the SC advice contradicts that of the physician.10
Some SCs provide a directory of symptoms from which users can select, influencing the diagnostic capability of the program. For example, the Mayo Clinic SC includes 28 chief complaints for adult patients, but the list does not include “fever”. Overseas SCs do not include conditions specific to Australia, such as Ross River virus infection, reducing their local usefulness. The Healthdirect SC, the only Australian SC we assessed, provides triage but not diagnosis advice.
These limitations suggest that triage advice may be the more important function of online SC tools. Each included SC warned that their service was not a substitute for consulting a physician. Diagnosis is not a single assessment, but rather a process requiring knowledge, experience, clinical examination and testing, and the passage of time,16 impossible to replicate in a single online interaction. Overseas SCs also suggest health care services inappropriate for users in Australia, including self‐referral to specialist care. As reported by other investigators,10 some SCs did not report specific information about their authors or editors, or about the validity of their advice.
Despite their limitations and the lack of regulation of online health programs, SCs can be useful. Epidemiological data can be tracked on sites such as WebMD, providing timely data to health professionals.22 Users can educate themselves about their own health, potentially improving patient–physician relationships.3,5 SCs can also direct people to appropriate care, and some tools are even directly linked with health care services. As the public becomes more educated, active, and informed about health, online tools will be an increasingly popular resource.
Limitations and strengths
Our systematic approach to identifying SCs will have captured the most popular tools, but we may have missed some used by Australians. The vignettes were primarily simple scenarios describing patients without comorbid conditions, and did not reflect the complexity of real patients. The investigator who assessed all SCs was familiar with the clinical vignettes, and user bias was possible. Information about whether programs employed AI algorithms was drawn solely from that provided in the SC. Strengths of our investigation included our use of previously described vignettes and of lay language to test the programs, as well as our incorporating conditions specific to Australia.
Conclusion
The SCs we evaluated provided correct first diagnoses in 36% of cases and appropriate triage advice in 49%. Overseas SCs may not provide advice relevant to users in Australia. The medical terminology used in SCs and its effect on comprehensibility for users and their adherence to the advice provided should be investigated, as should the real life performance of SCs and their impact on health outcomes. To diminish the burden on health care systems, particularly emergency care, it is vital that online tools promptly direct people to appropriate care. Accordingly, online programs should be backed by quality sources, and provide diagnostic or triage advice that is as accurate as possible.
Box 1 – Triage categories and triage advice provided by symptom checkers
|
Triage category |
Advice provided in symptom checkers |
||||||||||||||
|
|
|||||||||||||||
|
Emergency |
|
||||||||||||||
|
Urgent |
|
||||||||||||||
|
Non‐urgent |
|
||||||||||||||
|
Self‐care |
|
||||||||||||||
|
|
|||||||||||||||
|
* In Australia, this requires referral by a general practitioner; this advice is therefore not used on Australian website symptom checkers. |
|||||||||||||||
Box 2 – Flowchart for selection and assessment of symptom checkers providing diagnostic or triage advice
Box 3 – Accuracy of diagnosis provided by 27 symptom checkers, by severity of patient condition in vignette and by frequency of diagnosis
|
|
|
Correct diagnosis |
|||||||||||||
|
|
Listed first |
Listed in top 3 |
Listed in top 10 |
||||||||||||
|
Total vignettes |
Number* |
Proportion |
Number* |
Proportion |
Number* |
Proportion |
|||||||||
|
|
|||||||||||||||
|
All vignettes |
48 |
421/1170 |
36% (31–42%) |
606/1170 |
52% (47–59%) |
681/1170 |
58% (53–65%) |
||||||||
|
Patient condition |
|
|
|
|
|
|
|
||||||||
|
Emergency |
13 (27%) |
92/343 |
27% (21–34%) |
139/343 |
41% (33–50%) |
161/343 |
47% (40–56%) |
||||||||
|
Urgent |
14 (29%) |
163/365 |
45% (39–51%) |
231/365 |
63% (58–70%) |
245/365 |
67% (62–73%) |
||||||||
|
Non‐urgent |
11 (23%) |
99/252 |
39% (33–47%) |
145/252 |
58% (51–67%) |
168/252 |
67% (61–75%) |
||||||||
|
Self‐care |
10 (21%) |
67/210 |
32% (25–42%) |
91/210 |
43% (36–53%) |
107/210 |
51% (42–60%) |
||||||||
|
Diagnosis frequency |
|
|
|
|
|
|
|
||||||||
|
Common |
41 (85%) |
414/986 |
42% (37–50%) |
593/986 |
60% (54–69%) |
666/986 |
68% (61–76%) |
||||||||
|
Uncommon |
7 (15%) |
7/184 |
4% (1–7%) |
13/184 |
7% (3–12%) |
15/184 |
8% (4–13%) |
||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Numbers of correct vignette evaluations and applicable evaluations. Some vignettes could not be applied to a given symptom checker (see Methods). |
|||||||||||||||
Box 4 – Accuracy of diagnosis provided by 27 symptom checkers, by tool characteristics
|
|
Correct diagnosis |
||||||||||||||
|
Listed first |
Listed in top 3 |
Listed in top 10 |
|||||||||||||
|
Characteristics |
Number |
Number* |
Proportion |
Number* |
Proportion |
Number* |
Proportion |
||||||||
|
|
|||||||||||||||
|
All symptom checkers |
27 |
421/1170 |
36% (31–42%) |
606/1170 |
52% (47–59%) |
681/1170 |
58% (53–65%) |
||||||||
|
Artificial intelligence algorithms |
|
|
|
|
|
|
|
||||||||
|
Yes |
8 (30%) |
144/312 |
46% (40–57%) |
201/312 |
64% (59–74%) |
220/312 |
71% (65–80%) |
||||||||
|
No |
19 (70%) |
277/858 |
32% (26–38%) |
405/858 |
47% (40–54%) |
461/858 |
54% (46–61%) |
||||||||
|
Demographic questions |
|
|
|
|
|
|
|
||||||||
|
At least age and sex |
18 (67%) |
293/770 |
38% (32–47%) |
421/770 |
55% (47–64%) |
481/770 |
62% (55–72%) |
||||||||
|
No |
9 (33%) |
128/400 |
32% (26–38%) |
185/400 |
46% (40–53%) |
200/400 |
50% (44–57%) |
||||||||
|
Maximum diagnoses listed |
|
|
|
|
|
|
|
||||||||
|
0 |
|
|
|
|
|
|
|
||||||||
|
1–5 |
5 (18%) |
83/218 |
38% (32–43%) |
111/218 |
51% (43–58%) |
111/218 |
52% (44–58%) |
||||||||
|
6–10 |
8 (30%) |
132/312 |
42% (32–58%) |
178/312 |
57% (44–76%) |
197/312 |
63% (49–82%) |
||||||||
|
11 or more |
14 (52%) |
206/640 |
32% (23–40%) |
317/640 |
50% (39–59%) |
373/640 |
58% (48–68%) |
||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Numbers of correct vignette evaluations and applicable evaluations. Some vignettes could not be applied to a given symptom checker (see Methods). |
|||||||||||||||
Box 5 – Accuracy of triage advice provided by 19 symptom checkers, by severity of patient condition in vignette and by frequency of diagnosis
|
|
|
Correct triage advice |
|||||||||||||
|
Total vignettes |
Number* |
Proportion (95% CI) |
|||||||||||||
|
|
|||||||||||||||
|
All vignettes |
48 |
338/688 |
49% (44–54%) |
||||||||||||
|
Patient condition |
|
|
|
||||||||||||
|
Emergency |
13 (27%) |
121/191 |
63% (52–71%) |
||||||||||||
|
Urgent |
14 (29%) |
115/206 |
56% (52–75%) |
||||||||||||
|
Non‐urgent |
11 (23%) |
46/151 |
30% (11–39%) |
||||||||||||
|
Self‐care |
10 (21%) |
56/140 |
40% (26–49%) |
||||||||||||
|
Diagnosis frequency |
|
|
|
||||||||||||
|
Common |
41 (85%) |
297/587 |
51% (46–55%) |
||||||||||||
|
Uncommon |
7 (15%) |
41/101 |
41% (22–45%) |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Numbers of correct vignette evaluations and applicable evaluations. Some vignettes could not be applied to a given symptom checker (see Methods). |
|||||||||||||||
Box 6 – Accuracy of triage advice provided by 19 symptom checkers, by tool characteristics
|
Characteristics |
|
Correct triage advice |
|||||||||||||
|
Number |
Number* |
Proportion (95% CI) |
|||||||||||||
|
|
|||||||||||||||
|
All symptom checkers |
19 |
338/688 |
49% (44–54%) |
||||||||||||
|
Artificial intelligence algorithms |
|
|
|||||||||||||
|
Yes |
5 (26%) |
88/172 |
52% (50–54%) |
||||||||||||
|
No |
14 (74%) |
250/516 |
48% (41–54%) |
||||||||||||
|
Demographic questions |
|
|
|||||||||||||
|
At least age and sex |
11 (58%) |
240/451 |
53% (49–57%) |
||||||||||||
|
No |
8 (42%) |
98/237 |
41% (34–51%) |
||||||||||||
|
Maximum diagnoses listed |
|
|
|||||||||||||
|
0 |
9 (47%) |
167/301 |
55% (48–58%) |
||||||||||||
|
1–5 |
4 (21%) |
66/169 |
39% (11–65%) |
||||||||||||
|
6–10 |
6 (32%) |
105/218 |
49% (42–56%) |
||||||||||||
|
11 or more |
0 |
— |
— |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Numbers of correct vignette evaluations and applicable evaluations. Some vignettes could not be applied to a given symptom checker (see Methods). |
|||||||||||||||
Received 29 August 2019, accepted 10 December 2019





Abstract
Objectives: To investigate the quality of diagnostic and triage advice provided by free website and mobile application symptom checkers (SCs) accessible in Australia.
Design: 36 SCs providing medical diagnosis or triage advice were tested with 48 medical condition vignettes (1170 diagnosis vignette tests, 688 triage vignette tests).
Main outcome measures: Correct diagnosis advice (provided in first, the top three or top ten diagnosis results); correct triage advice (appropriate triage category recommended).
Results: The 27 diagnostic SCs listed the correct diagnosis first in 421 of 1170 SC vignette tests (36%; 95% CI, 31–42%), among the top three results in 606 tests (52%; 95% CI, 47–59%), and among the top ten results in 681 tests (58%; 95% CI, 53–65%). SCs using artificial intelligence algorithms listed the correct diagnosis first in 46% of tests (95% CI, 40–57%), compared with 32% (95% CI, 26–38%) for other SCs. The mean rate of first correct results for individual SCs ranged between 12% and 61%. The 19 triage SCs provided correct advice for 338 of 688 vignette tests (49%; 95% CI, 44–54%). Appropriate triage advice was more frequent for emergency care (63%; 95% CI, 52–71%) and urgent care vignette tests (56%; 95% CI, 52–75%) than for non‐urgent care (30%; 95% CI, 11–39%) and self‐care tests (40%; 95% CI, 26–49%).
Conclusion: The quality of diagnostic advice varied between SCs, and triage advice was generally risk‐averse, often recommending more urgent care than appropriate.