Out‐of‐pocket expenses for cancer care are of growing concern for patients, clinicians, service providers, non‐governmental organisations, private insurers, and politicians. Contrary to popular belief, there is no direct link between the cost and quality of care. Out‐of‐pocket expenses are a particular problem for patients who live further from treatment centres, are younger, or have later stage disease.1
Adults (18 years or older) with pathologically confirmed colorectal, lung, prostate or breast cancer from four rural (Midwest, South West, Great Southern, Goldfields) and two outer metropolitan (Joondalup/Wanneroo and Rockingham/Peel) regions of Western Australia were identified in the WA Cancer Registry. Between 1 April 2014 and 31 April 2017, eligible patients were invited to complete questionnaires requesting demographic, financial, and treatment information, including all costs during treatment, as reported previously.2 We used log‐linked generalised linear models with gamma distribution, adjusted for age and sex, to estimate out‐of‐pocket expenses (with 95% confidence intervals [CIs]) for participant characteristics found to be significantly associated with out‐of‐pocket expenses in univariate analyses (online Supporting Information). The study was approved by the WA Country Health Service Ethics Committee (reference, 2014:10) and the Department of Health WA Human Research Ethics Committee (reference, 2014/26).
One hundred and seventeen of the 119 outer metropolitan participants (98%) and 294 of the 308 rural participants (95%) incurred out‐of‐pocket expenses for their cancer care, chiefly for surgery, medical tests, and medical appointments. These costs ranged between $51 and $106 140 for outer metropolitan participants, and between $13 and $20 842 for rural participants. Fifty‐three rural participants (17%) and 39 outer metropolitan participants (33%) spent more than 10% of their household income on cancer care (data not shown).
Among rural participants, mean out‐of‐pocket expenses were higher for men ($1988; 95% CI, $1605–$2461 v $1362; 95% CI, $1092–$1699), for people with private health insurance ($2455; 95% CI, $1973–$3053 v $1103; 95% CI, $877–$1386), and for people who were married ($2086; 95% CI, $1749–$2489 v $1297; 95% CI, $975–$1725), had undergone surgery ($1990; 95% CI, $1684–$2351 v $1360, 95% CI, $1005–$1839), or had worked prior to being diagnosed with cancer ($2084; 95% CI, $1643–$2644 v $1298; 95% CI, $1038–$1625) (Box).
Among outer metropolitan participants, mean out‐of‐pocket expenses were higher for men ($5217; 95% CI, $3928–$6928 v $2247; 95% CI, $1756–$2875), for people with private health insurance ($4670; 95% CI, $3588–$6078 v $2510; 95% CI, $1853–$3401), and for those who had undergone surgery ($5434; 95% CI, $4260–$6932 v $2157; 95% CI, $1541–$3020), worked prior to being diagnosed with cancer ($5471, 95% CI, $3952–$7573 v $2143; 95% CI, $1643–$2794), resided in areas of high socio‐economic status ($4299; 95% CI, $3235–$5712 v low, $1859; 95% CI, $1374–$2516), or were receiving chemotherapy ($4286; 95% CI, $3162–$5810 v $2735; 95% CI, $2116–$3534) (Box).
It is perhaps surprising that out‐of‐pocket expenses were higher for people in outer metropolitan areas, who presumably lived closer to treatment centres than rural residents. However, these findings are consistent with the recent report that out‐of‐pocket spending on non‐hospital Medicare‐subsidised services and specialist services was higher for metropolitan patients than for those in regional areas.4
The higher out‐of‐pocket expenses for people with private health insurance or undergoing surgery indicate the importance of health care funding arrangements and the magnitude of the costs borne by patients.
The marked variation in out‐of‐pocket expenses reported here and by others5 highlights the need for easily accessible information about services, medical costs, and gap payments for all health care services. The Informed Financial Consent website coordinated by the Australian Medical Association,6 consumer organisation fact sheets, and professional body initiatives are steps in the right direction, but their impact is yet to be determined. Problems that still need attention in the unregulated private fee‐setting environment in Australia include price discrimination in some specialist sectors.7 Bundles of care for cancer treatment that would allow patients and their families to better understand and plan for expenses should be explored.
Box – Estimated mean out‐of‐pocket expenses for cancer‐related health care (with 95% confidence intervals) for outer metropolitan and rural patients, by patient characteristics significantly associated with higher out‐of‐pocket expenses in univariate analyses*
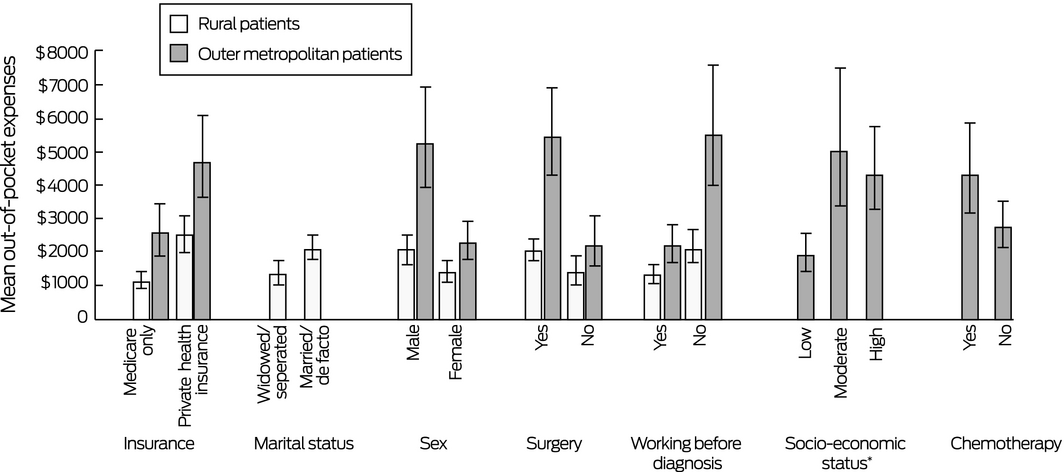
* For outer metropolitan patients, marital status, and for rural patients, socio‐economic status and chemotherapy were not significant predictors of out‐of‐pocket expenses, and were therefore not included in the final models. † Index of Relative Socio‐economic Disadvantage (IRSD):3 low (most disadvantaged), deciles 1–4; moderate, deciles 5–6; high (least disadvantaged), deciles 7–10.
Received 15 August 2019, accepted 4 December 2019
- 1. Lentz R, Benson AB, Kircher S. Financial toxicity in cancer care: prevalence, causes, consequences, and reduction strategies. J Surg Oncol 2019; 120: 85–92.
- 2. Newton JC, Johnson CE, Hohnen H, et al. Out‐of‐pocket expenses experienced by rural Western Australians diagnosed with cancer. Support Care Cancer 2018; 26: 3543–3452.
- 3. Australian Bureau of Statistics. 2033.0.55.001. Census of population and housing: Socio‐Economic Indexes for Areas (SEIFA), Australia, 2011: IRSD. Mar 2013. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2011~Main%20Features~IRSD~10005 (viewed Sept 2019).
- 4. Australian Institute of Health and Welfare. Patientsʼ out‐of‐pocket spending on Medicare services 2016–17 (Cat. no. HPF 35). Canberra: AIHW, 2018.
- 5. Gordon LG, Elliott TM, Olsen CM, et al. Out‐of‐pocket medical expenses for Queenslanders with a major cancer. Med J Aust 2018; 208: 497. https://www.mja.com.au/journal/2018/208/11/out-pocket-medical-expenses-queenslanders-major-cancer
- 6. Australian Medical Association. Informed financial consent [website], 23 July 2019. https://ama.com.au/article/ama-informed-financial-consent (viewed Sept 2019).
- 7. Johar M, Mu C, Van Gool K, Wong CY. Bleeding hearts, profiteers, or both: specialist physician fees in an unregulated market. Health Econ 2017; 26: 528–535.





Our investigation was funded by the Cancer Council of Western Australia and the WA Cancer and Palliative Care Network.
No relevant disclosures.