The known: Hyperglycaemia is common among hospital patients and may indicate undiagnosed diabetes.
The new: Routine blood glucose assessment of patients admitted to hospital from emergency departments led to 31% of patients (243 of 784) with newly detected hyperglycaemia (≥ 14 mmol/L) being diagnosed with diabetes. Adding automated requests for HbA1c assessment and notification of hyperglycaemic patients to diabetes services did not increase the proportion of patients diagnosed with diabetes and followed up.
The implications: Routine blood glucose assessment and notification of diabetes services are not sufficient for effectively identifying and caring for emergency department patients with previously unrecognised diabetes.
As many as one‐quarter of hospitalised adult patients are known to have diabetes.1,2,3,4 Hyperglycaemia in patients without previously diagnosed diabetes is also common; for instance, 12% of 2030 patients in one American hospital had newly identified hyperglycaemia.1 In an Australian study of 6187 patients admitted to a tertiary hospital from its emergency department (ED), 141 of 5192 patients without known diabetes (2.7%) had blood glucose levels in the diabetic range (≥ 11.1 mmol/L).3 Patients with newly identified hyperglycaemia may have unrecognised diabetes, or they may have stress hyperglycaemia, which usually resolves spontaneously after the acute illness has ended.
Hospital hyperglycaemia is strongly associated with adverse outcomes, but patient outcomes can be improved by effective glucose management.5 Detecting hyperglycaemia also provides an opportunity for diagnosing unrecognised diabetes, commencing its management, and averting its complications. In two studies including glucose screening of ED patients without diagnosed diabetes, 21 of 35 patients (68%) with random glucose levels of at least 6.9 mmol/L6 or 13 of 36 (36%) with levels of 7.0 mmol/L7 or more were diagnosed with diabetes following further testing.
However, blood glucose is not routinely measured on admission to hospital in Australia, even in patients admitted with conditions associated with diabetes. In Australian studies of myocardial infarction and stroke, admission blood glucose levels were measured in only one‐half8 or one‐quarter of patients.9
Electronic ordering of blood tests and the integration of different hospital databases, including pathology databases, facilitates automatic requests for blood glucose assessment of patients at the time of their admission to hospital. The effectiveness of such systems has not been systematically evaluated. In this pragmatic clinical trial, we aimed to determine whether routine blood glucose testing of patients admitted from EDs, together with automatic ordering of glycated haemoglobin (HbA1c) assessment and notification to the diabetes service of patients found to have hyperglycaemia, leads to more frequent recording of diabetes diagnoses and documentation of follow‐up plans. Further, we examined whether such testing is associated with improved hospital outcomes for patients.
Methods
Trial design and participants
The trial was overseen by a steering committee of the Endocrine Network of the New South Wales Agency for Clinical Innovation (https://www.aci.health.nsw.gov.au). NSW public district and tertiary referral hospitals were invited via the Agency to participate in our cluster randomised trial during the period 31 May 2011 – 31 December 2012; the duration of participation differed between hospitals because of local logistic and ethics‐related factors. Follow‐up data were collected until 2016. The trial was retrospectively registered with the Australian New Zealand Clinical Trials Registry on 20 September 2011 (ACTRN12611001007921).
Eighteen invited hospitals agreed to participate and were independently randomised by random number‐generating software to the intervention or control arms of the study, stratified by location (16 metropolitan, two regional hospitals) and type (12 tertiary, six district hospitals).
Intervention hospitals
In intervention hospitals, blood glucose was routinely measured by the pathology department, even if not specifically ordered, as part of initial blood assessment of all patients aged 18 years or more admitted to hospital from the ED, provided sufficient blood was available for analysis. When the patient's blood glucose level was 14 mmol/L or more, HbA1c assessment was automatically requested if sufficient blood in an ethylenediaminetetraacetic acid (EDTA)‐coated tube was available. In most cases, HbA1c results were available within two days; that is, while the patient was still in hospital. Measuring blood glucose and notifying diabetes centres about elevated results became routine care; individual consent for these measures was therefore not sought.
Lists of patients with blood glucose levels of 14 mmol/L or more were forwarded daily to the hospital diabetes service. The study project manager visited all intervention hospital diabetes services to discuss strategies for managing the increased workload, but no additional resources were provided.
Control hospitals
In control hospitals, blood glucose was routinely measured in all patients admitted from the ED, but HbA1c was not routinely assessed, nor were patients with newly detected hyperglycaemia notified to diabetes services.
At both intervention and control hospitals, the results of the additional blood tests were freely available in computerised pathology systems to teams managing the patients.
Study outcomes
The primary outcome was a new diagnosis of diabetes or suspected diagnosis for a person whose admission blood glucose level was at least 14 mmol/L, together with a documented follow‐up plan. The criteria for this outcome were:
- the diagnosis of diabetes or likely diagnosis recorded in the patient notes;
- a confirmatory test result — HbA1c level of at least 48 mmol/mol (6.5%), a second fasting blood glucose measurement of at least 7.0 mmol/L, or a random blood glucose measurement of at least 11.1 mmol/L — or prescribing of medication for diabetes on discharge;
- a plan for diabetes follow‐up by a member of the diabetes team (specialist, diabetes educator) or a statement that this was to be undertaken by a general practitioner.
Secondary outcomes included new diagnosis of diabetes (regardless of whether a plan for follow‐up was documented), length of hospital stay, re‐admission (to any NSW hospital) within 30 days, and death as an inpatient or after the index admission, censored at 31 March 2016.
Data collection and linkage
Serum glucose and HbA1c levels of adult patients measured in participating EDs during the study were available to the investigators. Research assistants, blinded to the intent of the trial, hospital group allocation and study design, reviewed the medical records of patients with admission blood glucose levels of 14 mmol/L or more to collect data on the primary outcome. For patients with more than one hospital admission during the study period, we included only the first admission for which the admission blood glucose level was 14 mmol/L or more.
Data (to 31 March 2016) for secondary outcomes (re‐admission within 30 days to any hospital, death) and coding data (major diagnostic category, Charlson index score) were collected by linking patient data in the Pathology Dataset with the NSW Admitted Patients Data Collection, the NSW Registry of Births, Deaths and Marriages, and the NSW Cause of Death Unit Record (held by the NSW Ministry of Health Secure Analytics for Population Health Research and Intelligence [SAPHaRI]). Probabilistic data linkage was performed by the NSW Centre for Health Record Linkage (CHeReL) based on name, date of birth, address, hospital medical record number, and date of hospital admission. For linkage purposes, we accepted differences between dates of blood glucose measurements and admission of up to two days. The final linked dataset was de‐identified before being made available to the investigators.
Statistical analysis
Data were analysed in SAS 9.4 (SAS Institute). Baseline characteristics (continuous variables) are presented as means and standard deviations (SDs); differences between intervention and control groups were assessed by linear regression. Differences in categorical variables were assessed by logistic regression. Regression models were fitted in a generalised estimating equations (GEE) framework with an exchangeable correlation matrix to adjust for clustering of individuals within hospitals, age, and sex. Empirical standard errors were used to calculate P values and confidence intervals (CIs).
Ethics approval
The trial was approved by the Western Sydney Human Research Ethics Committee (reference, HREC2010/2/4.4[3100]), with site‐specific ethics approval from each participating hospital. Data linkage was approved by the NSW Population and Health Services Research Ethics Committee (reference, HREC/CIPHS/4).
Results
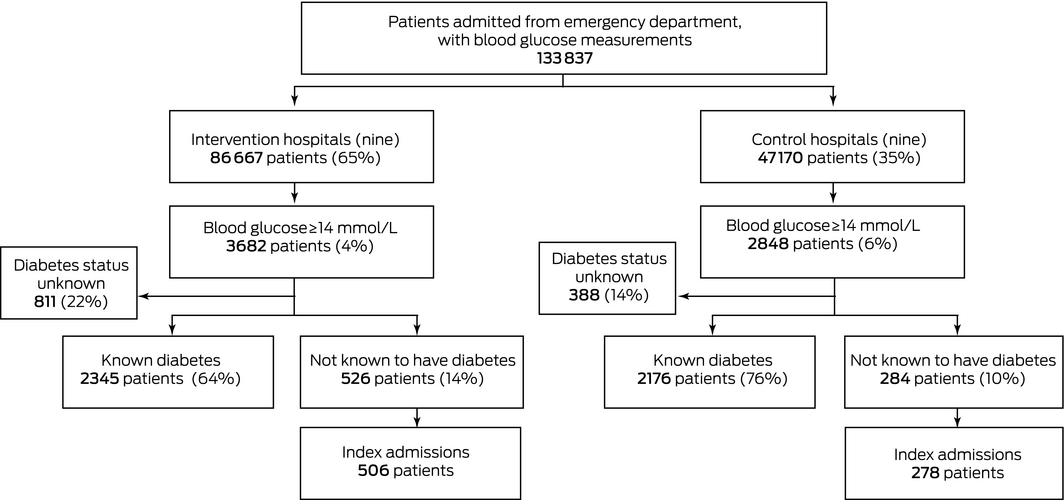
Eighteen hospitals participated in the trial, nine each in the intervention and control arms. The median period of participation was 12 months (range, 1–16 months). We could link 133 837 of 153 063 ED admissions in the NSW Admitted Patients Data Collection (87.4%) with a corresponding blood glucose measurement: 86 667 in intervention hospitals and 47 170 in control hospitals (Box 1). The characteristics of the patients in the two groups were similar, except for the distribution of major diagnostic categories (Supporting Information, table 1).
The index admission blood glucose levels of 784 patients not previously known to have diabetes were 14 mmol/L or more; their mean age was 62.7 years (SD, 19.4 years), and 429 (55%) were men. The mean blood glucose level in these patients was 19.7 mmol/L (SD, 9.6 mmol/L); of the 295 patients for whom HbA1c was measured (38%), the mean level was 72 mmol/mol (SD, 26 mmol/mol). The baseline characteristics of patients with hyperglycaemia in the control and intervention hospitals were similar (Box 2).
The crude proportion of patients with newly diagnosed diabetes and follow‐up plans was lower in the intervention (83 of 506 patients; 16%) than in the control hospitals (73 of 278 patients; 26%), but the difference was not statistically significant after adjusting for clustering, age, and sex (adjusted odds ratio [aOR], 0.83; 95% CI, 0.42–1.7; P = 0.61). Similarly, rates of diagnosis (regardless of documented follow‐up plan) were similar in control (86 of 278 patients, 31%) and intervention hospitals (157 of 506 patients, 31%; aOR, 1.51, 95% CI, 0.83–2.80; P = 0.18). Mortality (during index admission or up to 5 years after discharge) and 30‐day hospital re‐admission rates were also similar for the two groups, as was mean length of index hospital admission stay (Box 3).
In the intervention hospitals, HbA1c was not assessed in 236 patients (47%); the baseline characteristics (age, sex, Charlson index score, blood glucose levels) were similar for patients who were or were not assessed (Supporting Information, table 2). A per protocol analysis, in which the 270 patients in intervention hospitals with HbA1c measurements were compared with all control hospital patients, yielded similar results to the main analysis with regard to diabetes diagnosis and follow‐up plan — intervention, 49 of 270 patients (18%); aOR, 0.83 (95% CI, 0.23–3.01); P = 0.78 — as well as for the secondary outcomes (data not shown).
Discussion
Routine blood glucose testing of patients admitted to hospital from EDs resulted in 243 of 784 patients (31%) with newly detected hyperglycaemia (≥ 14 mmol/L) being diagnosed with diabetes. Adding automatic requests for HbA1c assessment and notifying diabetes services at intervention hospitals did not lead to a higher proportion of patients receiving new diabetes diagnoses or plans for diabetes follow‐up, nor did it significantly affect patient outcomes.
Hospitalisation provides an opportunity for diagnosing previously unrecognised diabetes in patients. The incidence of new diabetes diagnoses in our study was comparable with that of older studies in which 20–42% of hospital patients with newly documented hyperglycaemia were further investigated or received an intervention.10,11,12 A more recent Australian hospital audit found that hyperglycaemia was acknowledged for only half the patients not known to have diabetes but who had at least one blood glucose measurement of 11.1 mmol/L or more.13 Our results suggest that routine blood glucose testing of patients admitted from EDs, an inexpensive intervention, can identify some patients with unrecognised diabetes. However, they also indicate that routinely requesting HbA1c assessment of ED patients, without well developed and adequately resourced plans for their management and referral, does not lead to increased diagnosis of diabetes or to better hospital outcomes for admitted patients.
Cohort studies of HbA1c assessment‐based screening of ED patients for diabetes have been undertaken since we commenced our trial. In a South Australian study, HbA1c was automatically assessed in ED patients with random blood glucose levels of 5.5 mmol/L or more;14 11% of tested patients not previously known to have diabetes met the HbA1c criterion for diabetes. Another Australian study, in which HbA1c was also assessed in patients with at least 5.5 mmol/L blood glucose, found that 38% of ED patients either had known diabetes or met the HbA1c criterion for diabetes; diabetes had not previously been recognised in one‐third of these cases.15 Neither study examined documentation of diabetes or initiation of treatment. In a third Australian study, HbA1c screening indicated that 5% of hospital inpatients aged 55 years or more had unrecognised diabetes.16
Our study was undertaken before the HbA1c criterion for diagnosing diabetes was adopted in Australia (2012).17 Routine glucose and HbA1c assessment, or a higher rate of protocol HbA1c measurement (in our study, HbA1c was assessed in only half the patients in the intervention arm, possibly because blood in an EDTA tube was often not available), might achieve more frequent recognition of undetected diabetes.
Applying a blood glucose threshold of 14 mmol/L for HbA1c assessment was a pragmatic decision that acknowledged clinicians' concerns that diabetes units would be overburdened should a lower but more meaningful threshold, such as 11.1 mmol/L, be applied. Notifying hospital diabetes services of patients with hyperglycaemia, even with our higher glucose threshold, did not increase the rates of new diabetes diagnoses, treatment initiation, or follow‐up, suggesting that diabetes services were already working at full capacity with regard to inpatient care. The primary function of diabetes services has traditionally been outpatient chronic disease management support. Being made aware of potential patients who may require inpatient diabetes management could not lead to improved outcomes for patients without more staff being available to review their cases, and lowering the blood glucose threshold for testing would not have improved this situation.
A further reason that documented diabetes follow‐up was not more frequent in intervention hospitals may have been that care for patients with type 2 diabetes was transferred from specialists to general practitioners. The shift over the past 15 years to a GP management model of diabetes care,18 together with limited hospital resources, has led many hospital diabetes services to focus on patients with complex needs, discharging patients with milder disease to general practice. Poor communication between teams caring for patients with diabetes and the completion of discharge summaries to GPs by medical staff not involved in their care may have also contributed to documentation of follow‐up plans not being more frequent in intervention hospitals.
The hospital mortality rate of 17% for patients admitted with blood glucose levels of 14 mmol/L or more indicates that hyperglycaemia requires more attention in hospitals. Improved glucose control has been found to achieve better clinical outcomes in trials in some hospital settings.5 The lack of specialist inpatient diabetes teams in intervention hospitals may have been one reason that hospital outcomes for patients with hyperglycaemia were not better than in control hospitals. Only one of the participating hospitals, randomised to the control arm, had an inpatient diabetes team. It was recommended in 2012 that such teams be established in Australia.19 Care by inpatient diabetes teams have been found to improve glycaemic control and outcomes for patients, including reduced lengths of stay and re‐admission rates.20,21 In the British National Health Service, 72% of hospitals have diabetes inpatient specialist nurses.22
Strengths and limitations
As our study involved most tertiary hospitals in NSW, and a large number of patients were screened, our findings can probably be generalised to other Australian hospitals. However, we did not have data on baseline diabetes detection rates, so we are unable to determine whether routine blood glucose testing increased the number of diabetes diagnoses at both control and intervention hospitals. We were unable to ascertain the diabetes status of 18% of patients with hyperglycaemia, chiefly because we could not obtain their paper medical records. Additionally, the dramatic shifts in odds ratios after statistical adjustment suggest that the effects of some confounding variables were not removed by randomisation.
Conclusion
Since 2001, the United Kingdom has recognised that greater investment in inpatient diabetes services and training is needed to improve outcomes by publishing a National Service Framework for Diabetes that incorporates service planning objectives for inpatients with diabetes.23 This framework has been supplemented by programs for improving and promoting the importance of inpatient diabetes diagnosis and care, such as the ThinkGlucose resources,24 an annual national diabetes audit,22 and a guide for executive leaders.25 Similarly, NSW Health established the NSW Diabetes Taskforce in 2016, developing training resources, tools for supporting local auditing of inpatient diabetes care, and standardised processes for identifying people with diabetes in hospital, including blood glucose screening.26
Our study indicates that blood glucose and HbA1c screening alone does not improve diabetes case detection or care for patients admitted to hospital from EDs. It remains to be determined whether greater emphasis on training elements in the glucose screening program can improve outcomes without additional staff resources or specialist inpatient diabetes teams being provided.
Box 1 – Flow chart for patients in eighteen hospitals whose blood glucose level was measured at the time of their admission to hospital
Box 2 – Characteristics of patients without previously identified diabetes with admission blood glucose levels of 14 mmol/L or more
|
|
Total |
Intervention hospitals |
Control hospitals |
P |
|||||||||||
|
|
|||||||||||||||
|
Admissions of patients without known diabetes with blood glucose ≥ 14 mmol/L |
810 |
526 |
284 |
|
|||||||||||
|
Index admissions |
784 |
506 |
278 |
|
|||||||||||
|
Age (years), mean (SD) |
62.7 (19.4) |
63.4 (19.3) |
61.5 (19.7) |
0.79 |
|||||||||||
|
Sex |
|
|
|
0.22 |
|||||||||||
|
Men |
429 (54.7%) |
268 (52.9%) |
161 (57.9%) |
|
|||||||||||
|
Women |
355 (45.2%) |
238 (47.0%) |
117 (42.0%) |
|
|||||||||||
|
Major diagnostic category |
|
|
|
0.80 |
|||||||||||
|
Nervous system |
62 (7.9%) |
45 (8.9%) |
17 (6.1%) |
|
|||||||||||
|
Respiratory system |
118 (15.1%) |
74 (15%) |
44 (16%) |
|
|||||||||||
|
Circulatory system |
188 (24.0%) |
122 (24.1%) |
66 (24%) |
|
|||||||||||
|
Digestive system, hepato‐biliary, pancreas |
56 (7.1%) |
36 (7.1%) |
20 (7.2%) |
|
|||||||||||
|
Musculoskeletal system, connective tissue |
39 (4.9%) |
28 (5.5%) |
11 (4.0%) |
|
|||||||||||
|
Kidney and urinary tract |
35 (4.5%) |
23 (4.5%) |
12 (4.3%) |
|
|||||||||||
|
Injuries, poison, toxic effect of drugs |
44 (5.6%) |
25 (4.9%) |
19 (6.8%) |
|
|||||||||||
|
Other |
242 (30.9%) |
153 (30.2%) |
89 (32%) |
|
|||||||||||
|
Charlson Index |
|
|
|
0.13 |
|||||||||||
|
0 |
471 (60.1%) |
310 (61.2%) |
161 (57.9%) |
|
|||||||||||
|
1 |
147 (18.8%) |
82 (16%) |
65 (23%) |
|
|||||||||||
|
2 or more |
166 (21.2%) |
114 (22.5%) |
52 (19%) |
|
|||||||||||
|
Blood glucose (mmol/L), mean (SD) |
19.7 (9.6) |
19.9 (9.7) |
19.5 (9.4) |
0.64 |
|||||||||||
|
HbA1c measured |
295 (37.6%) |
270 (53.3%) |
25 (9.0%) |
0.009 |
|||||||||||
|
HbA1c (mmol/mol), mean (SD) |
72 (26) |
69 (24) |
96 (29) |
0.22 |
|||||||||||
|
|
|||||||||||||||
|
HbA1c = glycated haemoglobin; SD = standard deviation. |
|||||||||||||||
Box 3 – Outcomes for patients without previously identified diabetes whose admission blood glucose levels were 14 mmol/L or more
|
|
Total |
Control hospitals |
Intervention hospitals |
Odds ratio (95% CI) |
P |
Adjusted odds ratio* (95% CI) |
P |
||||||||
|
|
|||||||||||||||
|
Number of patients |
784 |
278 |
506 |
|
|
|
|
||||||||
|
New diagnosis of diabetes or suspected diabetes, with documented follow‐up plan |
156 (20%) |
73 (26%) |
83 (16%) |
0.55 |
0.001 |
0.83 |
0.61 |
||||||||
|
New diagnosis of diabetes or suspected diabetes† |
243 (31%) |
86 (31%) |
157 (31%) |
1.00 |
0.98 |
1.51 |
0.18 |
||||||||
|
Died during index hospital admission |
137 (18%) |
51 (18%) |
86 (17%) |
0.91 |
0.63 |
0.89 |
0.55 |
||||||||
|
Died since index hospital admission‡ |
184 (23%) |
61 (22%) |
123 (24%) |
1.14 |
0.46 |
1.07 |
0.72 |
||||||||
|
Re‐admitted within 30 days |
218 (28%) |
62 (22%) |
156 (31%) |
1.55 |
0.01 |
1.34 |
0.21 |
||||||||
|
Length of hospital stay during index admission (days), mean (SD) |
6.1 (8.5) |
6.4 (9.1) |
6.0 (8.2) |
— |
— |
—§ |
0.51 |
||||||||
|
|
|||||||||||||||
|
CI = confidence interval; SD = standard deviation. * Adjusted for clustering within hospitals, age, and sex. † With or without documented follow‐up plan. ‡ Censored at 31 March 2016 (maximum 5 years' follow‐up). § Adjusted difference in means, –0.48 days; 95% CI, –1.89 to 0.93 days. |
|||||||||||||||
Received 27 November 2018, accepted 25 June 2019
- N Wah Cheung1,2
- Lesley V Campbell3
- Gregory R Fulcher4
- Patrick McElduff5
- Barbara Depczynski6,7,8
- Shamasunder Acharya9
- John Carter10
- Bernard Champion11
- Roger Chen12
- David Chipps1
- Jeff Flack13
- Jen Kinsella14
- Margaret Layton15
- Mark McLean16
- Robert G Moses17
- Kris Park11
- Ann M Poynten6
- Carol Pollock2,4
- Debbie Scadden18
- Katherine T Tonks19
- Mary Webber14
- Chris White6
- Vincent Wong7
- Sandy Middleton20,21
- 1 Westmead Hospital, Sydney, NSW
- 2 University of Sydney, Sydney, NSW
- 3 St Vincent's Hospital, Sydney, NSW
- 4 Royal North Shore Hospital, Sydney, NSW
- 5 University of Newcastle, Newcastle, NSW
- 6 Prince of Wales Private Hospital, Sydney, NSW
- 7 Liverpool Hospital, Sydney, NSW
- 8 Fairfield Hospital, Sydney, NSW
- 9 John Hunter Hospital, Newcastle, NSW
- 10 Hornsby Hospital, Sydney, NSW
- 11 Nepean Hospital, Penrith, NSW
- 12 Concord Repatriation General Hospital, Sydney, NSW
- 13 Bankstown‐Lidcombe Hospital, Sydney, NSW
- 14 Ryde Hospital, Sydney, NSW
- 15 Gosford Hospital, Gosford, NSW
- 16 Western Sydney University School of Medicine, Penrith, NSW
- 17 Wollongong Hospital, Wollongong, NSW
- 18 Murrumbidgee Local Health District, Wagga Wagga, NSW
- 19 Garvan Institute of Medical Research, Sydney, NSW
- 20 St Vincent's Health Australia, Sydney, NSW
- 21 Australian Catholic University Nursing Research Institute, Sydney, NSW
This study was funded by a National Health and Medical Research grant (1013443) and the NSW Agency for Clinical Innovation, which also funded the project officer for the project, who was involved in data collection. We acknowledge the contributions of the following colleagues who supported the study as research assistants, site investigators, or pathology department employees: Nancy Cinnadaio, Ivan Kuo, Paul Tridgell, Tony Morrow, Graham Jones, Rita Horvath, Michael Earl, and Mark Bishop. NSW Health provided access to the linked datasets. Cause of Death Unit Record Files were provided by the Australian Coordinating Registry for the Cause of Death Unit Record File on behalf of the NSW Registry of Births, Deaths and Marriages, the NSW Coroner, and the National Coronial Information System.
No relevant disclosures.
- 1. Umpierrez GE, Isaacs SD, Bazargan N, et al. Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 2002; 87: 978–982.
- 2. Rando L, Keith C, Sardjono DA, et al. Diabetes ward management: room for improvement. J Pharm Pract Res 2004; 34: 95–99.
- 3. Cheung NW, Li S, Ma G, Crampton R. The relationship between admission blood glucose levels and hospital mortality. Diabetologia 2008; 51: 952–955.
- 4. Bach LA, Ekinci E, Engler D, et al. The high burden of inpatient diabetes mellitus: the Melbourne Public Hospitals Diabetes Inpatient Audit. Med J Aust 2014; 201: 334–338. https://www.mja.com.au/journal/2014/201/6/high-burden-inpatient-diabetes-mellitus-melbourne-public-hospitals-diabetes
- 5. Wagstaff A, Cheung NW. Diabetes and hyperglycemia in the critical care setting: has the evidence for glycemic control vanished? (Or … is going away?). Curr Diab Rep 2014; 14: 444.
- 6. Greci LS, Kailasam M, Malkani S, et al. Utility of HbA1c levels for diabetes case finding in hospitalized patients with hyperglycemia. Diabetes Care 2003; 26: 1064–1068.
- 7. George PM, Valabhjit J, Dawood M, Henry JA. Screening for type 2 diabetes in the accident and emergency department. Diabet Med 2005; 22: 1766–1769.
- 8. Wong V, Ross DL, Park K, et al. Hyperglycemia: still an important predictor of adverse outcomes following AMI in the reperfusion era. Diabetes Res Clin Pract 2004; 64: 85–91.
- 9. Drury P, Levi C, McInnes L, et al. Management of fever, hyperglycaemia and swallowing dysfunction following hospital admission for acute stroke in New South Wales. Australia. Int J Stroke 2014; 9: 23–31.
- 10. Bravata DM, Kim N, Concata J, Brass LM. Hyperglycaemia in patients with acute ischaemic stroke: how often do we screen for undiagnosed diabetes? Q J Med 2003; 96: 491–497.
- 11. Hennessy AR, Reynolds RM, Walker JD. Blood glucose measurement in acute medicine: inadequate detection and management. Diabetic Med 2002; 19: 697–703.
- 12. Levetan CS, Passaro M, Jablonski K, et al. Unrecognized diabetes among hospitalized patients. Diabetes Care 1998; 21: 246–249.
- 13. Tonks KT, Jones GJ, McGeechan K, Campbell LV. Hyperglycaemia in inpatients: still a sticky situation. Int Med J 2010; 10: 521–526.
- 14. Valentine NA, Alhawassi TM, Roberts GW, et al. Detecting undiagnosed diabetes using glycated haemoglobin: an automated screening test in hospitalized patients. Med J Aust 2011; 194: 160–164. https://www.mja.com.au/journal/2011/194/4/detecting-undiagnosed-diabetes-using-glycated-haemoglobin-automated-screening
- 15. Hng TM, Hor A, Ravi S, et al. Diabetes case finding in the emergency department, using HbA1c: an opportunity to improve diabetes detection, prevention, and care. BMJ Open Diabetes Res Care 2016; 4: e000191.
- 16. Nanayakkara N, Nguyen H, Churilov L, et al. Inpatient HbA1c testing: a prospective observational study. BMJ Open Diabetes Res Care 2015; 3: e000113.
- 17. d'Emden MC, Shaw JE, Colman PG, et al. The role of HbA1c in the diagnosis of diabetes mellitus in Australia. Med J Aust 2012; 197: 220–221. https://www.mja.com.au/journal/2012/197/4/role-hba1c-diagnosis-diabetes-mellitus-australia
- 18. Fountaine T, Bennett CC. Health care homes: lessons from the Diabetes Care Project. Med J Aust 2016; 205: 389–391. https://www.mja.com.au/journal/2016/205/9/health-care-homes-lessons-diabetes-care-project
- 19. Cheung NW, Chipps D, Cornelius S, et al. Australian Diabetes Society guidelines for routine glucose control in hospital. Australian Diabetes Society, 2012. https://diabetessociety.com.au/documents/ADSGuidelinesforRoutineGlucoseControlinHospitalFinal2012.pdf (viewed June 2018).
- 20. Davies M, Dixon S, Currie CJ, et al. Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial. Diabet Med 2001; 18: 301–307.
- 21. Flanagan D, Moore E, Baker S, et al. Diabetes care in hospital: the impact of a dedicated inpatient care team. Diabet Med 2008; 25: 147–151.
- 22. NHS Digital. National diabetes inpatient audit England and Wales (NaDIA): 2017. Mar 2018. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/national-diabetes-inpatient-audit-nadia-2017 (viewed June 2018).
- 23. National Health Service. National Service Framework for Diabetes: standards. Dec 2001. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/198836/National_Service_Framework_for_Diabetes.pdf (viewed June 2018).
- 24. National Health Service. ThinkGlucose [website]. 2010. Archived: https://webarchive.nationalarchives.gov.uk/20150401104927/http://www.institute.nhs.uk/quality_and_value/think_glucose/welcome_to_the_website_for_thinkglucose.html (viewed June 2018).
- 25. National Health Service. Executive leaders' guide. 2010. https://www.england.nhs.uk/improvement-hub/wp-content/uploads/sites/44/2017/11/Think-Glucose-Executive-Leaders-Guide.pdf (viewed June 2018).
- 26. NSW Agency for Clinical Innovation. Inpatient management of diabetes mellitus: monitoring and evaluation plan. Sydney: ACI, 2017. http://eih.health.nsw.gov.au/__data/assets/pdf_file/0010/373096/170628-Diabetes-ME-plan.pdf (viewed June 2018).





Abstract
Objective: To determine whether routine blood glucose assessment of patients admitted to hospital from emergency departments (EDs) results in higher rates of new diagnoses of diabetes and documentation of follow‐up plans.
Design, setting: Cluster randomised trial in 18 New South Wales public district and tertiary hospitals, 31 May 2011 – 31 December 2012; outcomes follow‐up to 31 March 2016.
Participants: Patients aged 18 years or more admitted to hospital from EDs.
Intervention: Routine blood glucose assessment at control and intervention hospitals; automatic requests for glycated haemoglobin (HbA1c) assessment and notification of diabetes services about patients at intervention hospitals with blood glucose levels of 14 mmol/L or more.
Main outcome measure: New diagnoses of diabetes and documented follow‐up plans for patients with admission blood glucose levels of 14 mmol/L or more.
Results: Blood glucose was measured in 133 837 patients admitted to hospital from an ED. The numbers of new diabetes diagnoses with documented follow‐up plans for patients with blood glucose levels of 14 mmol/L or more were similar in intervention (83/506 patients, 16%) and control hospitals (73/278, 26%; adjusted odds ratio [aOR], 0.83; 95% CI 0.42–1.7; P = 0.61), as were new diabetes diagnoses with or without plans (intervention, 157/506, 31%; control, 86/278, 31%; aOR, 1.51; 95% CI, 0.83–2.80; P = 0.18). 30‐day re‐admission (31% v 22%; aOR, 1.34; 95% CI, 0.86–2.09; P = 0.21) and post‐hospital mortality rates (24% v 22%; aOR, 1.07; 95% CI, 0.74–1.55; P = 0.72) were also similar for patients in intervention and control hospitals.
Conclusion: Glucose and HbA1c screening of patients admitted to hospital from EDs does not alone increase detection of previously unidentified diabetes. Adequate resourcing and effective management pathways for patients with newly detected hyperglycaemia and diabetes are needed.
Trial registration: Australian New Zealand Clinical Trials Registry, ACTRN12611001007921.