Abstract
Objective: To examine whether the Ways of Thinking and Ways of Doing (WoTWoD) cultural respect framework improves clinically appropriate anticipatory care in general practice and the cultural respect levels of medical practice staff.
Design: Mixed methods, cluster randomised controlled trial with a participatory action research approach.
Setting, participants: Fifty‐six general practices in Sydney and Melbourne, 2014–2017.
Intervention: WoTWoD encompasses a toolkit (ten scenarios illustrating cross‐cultural behaviour in clinical practice), one half‐day workshop, cultural mentor support for practices, and a local care partnership between participating Medicare locals/primary health networks and local Aboriginal Community Controlled Health Services for guiding the program and facilitating community engagement. The intervention lasted 12 months at each practice.
Major outcomes: Rates of claims for MBS item 715 (health assessment for Aboriginal and Torres Strait Islander People) and recording of chronic disease risk factors; changes in cultural quotient (CQ) scores of practice staff.
Results: Complete results were available for 28 intervention (135 GPs, 807 Indigenous patients) and 25 control practices (210 GPs, 1554 Indigenous patients). 12‐Month rates of MBS item 715 claims and recording of risk factors for the two groups were not statistically significantly different, nor were mean changes in CQ scores, regardless of staff category and practice attributes.
Conclusion: The WoTWoD program did not increase the rate of Indigenous health checks or improve cultural respect scores in general practice. Conceptual, methodologic, and contextual factors that influence cultural mentorship, culturally respectful clinical practice, and Indigenous health care require further investigation.
Trial registration: Australia New Zealand Clinical Trials Registry ACTRN12614000797673.
The known: The gap in life expectancy between Indigenous and non‐Indigenous Australians remains large. Urban Indigenous Australian‐controlled health services are under‐resourced, and mainstream primary care services are often not culturally sensitive.
The new: A practice‐based cultural respect program — including a workshop and toolkit of scenarios, with advice from a cultural mentor, and guided by a care partnership of Indigenous and general practice organisations — did not significantly influence Indigenous health check rates or cultural respect levels.
The implications: Cultural respect programs may require more than 12 months to increase Indigenous health check rates and the cultural quotient scores of general practice clinic staff.
Closing the health and care gaps between Aboriginal and Torres Strait Islander (Indigenous) Australians and non‐Indigenous Australians has been a longstanding challenge.1,2 In 2018, a decade after Australian governments committed themselves to Closing the Gap, mortality and life expectancy for Indigenous Australians had not markedly improved, and nearly 80% of the difference in mortality between adult Indigenous and non‐Indigenous Australians was attributable to chronic disease.3
The Practice Incentives Program–Indigenous Health Incentive (PIP‐IHI), introduced in May 2010, assists general practitioners undertake chronic disease care planning for their Indigenous patients. Initial uptake was poor: only 64% of general practices expected to register (1275 of 2000) did so during 2010–11.4 However, the proportion had increased by May 2012.5 The rebate for health assessments for Aboriginal and Torres Strait Islander People (Medicare Benefits Schedule [MBS] item 715),6 constitutes an additional strategy for improving the access of Indigenous Australians to primary health care matched to their needs. GPs can engage suitably qualified practice nurses or Aboriginal Health Workers to assist with the assessment, including patient history‐taking, clinical examination and investigations, and with providing patients with education and resources for managing their own health. The proportion of Indigenous Australians for whom payment for MBS item 715 was claimed increased from nearly 11% in 2010–11 to nearly 29% in 2016–17 (New South Wales, 26.8%; Victoria, 17.1%).7 However, the rate is still low and access to comprehensive care planning for Indigenous Australians is poor.
Aboriginal Community Controlled Health Services (ACCHSs) are important providers of primary health care to Indigenous communities.8 However, most Indigenous Australians living in urban areas also use standard primary care and GP services. In 2016, Indigenous Australians comprised 3% of the Australian population (744 956 people);8 38% lived in New South Wales (229 951) or Victoria (53 663).9 About one‐third of Indigenous Australians live in major cities, but only 16 of 138 ACCHSs are in major cities; urban ACCHSs have lower staff/client ratios than regional and remote ACCHSs.8
Indigenous Australians frequently encounter cultural disrespect in mainstream primary care services.10,11 The 2012–13 Australian Aboriginal and Torres Strait Islander Health Survey1 reported that 16% of Indigenous Australians had experienced racism in health settings; 20% of these respondents reported that doctors, nurses and other hospital or clinic staff were discriminatory, and 7% avoided seeking health care because of unfair treatment. Of 755 adult Indigenous Victorians surveyed in 2011, 29% had experienced racism in health settings.12 Lack of cultural respect in health care restricts access to and reduces the quality of care for Indigenous Australians.1
We have previously identified trust, access, flexibility, time, support, outreach, and working together as key aspects of cultural respect.13 Although the Indigenous Chronic Disease Package (2009–2014) supported increased cultural awareness training for health workers, it did not change attitudes or behaviour sufficiently to bridge the cultural gap between health professionals and Indigenous people.14
We developed the Ways of Thinking and Ways of Doing (WoTWoD) cultural respect program with a trans‐theoretical approach, harmonising many similar conceptual frameworks and the terminology applied to Indigenous and cross‐cultural health in Australia. The theoretical underpinnings of WoTWoD were described in the article describing our pilot study.15 The WoTWoD framework translates the systemic, organisational, and clinical elements of the Australian Health Ministers’ Advisory Council Cultural Competency Framework16 into routine clinical practice. Cultural respect reflects the attitudes and behaviour of the entire medical practice, from reception to consulting room. In addition, general practice organisations must work in partnership with Indigenous community‐controlled organisations to reduce health care disparities, address social determinants of poor health, and increase access to safe, effective and culturally respectful care.17 This is fundamental to Indigenous Australians’ right to the highest standard of health.11,18
We undertook a cluster randomised controlled trial to examine whether the WoTWoD program improves clinically appropriate anticipatory care in general practice and the cultural respect of medical practice staff.
Methods
Study design
We conducted a mixed methods cluster randomised controlled trial, with a participatory action research approach. The investigators and Indigenous cultural mentors cooperated with communities, general practices, Medicare Locals, and ACCHSs to optimise engagement with the trial.
Participants and setting
The trial was conducted in Sydney and Melbourne during April 2014 – May 2017. The Sydney recruitment area comprised five Medicare Locals with about 1400 general practices and 40 000 Indigenous people; the Melbourne recruitment area included four Medicare Locals with about 500 general practices and 7000 Indigenous people.19 The Medicare Locals were restructured into larger primary health networks (PHNs) in 2015.20 General practices were recruited through the Medicare Local/PHN; the principal GP or practice manager provided informed consent on behalf of the practice.
Outcomes
Outcome measures reflecting the key dimensions of access to care and cultural respect were measured for each practice:
-
the rate of MBS item 715 claims and of documentation of chronic disease risk factors per active Indigenous patient during the 12 months preceding the intervention (baseline) and during the 12 months of the intervention; and
-
the change in mean CQ scores of clinic staff, assessed at baseline and 12 months.
Sample size
To detect a 30% difference in the proportions of patients for whom MBS item 715 was claimed (β = 0.80; α = 0.05 [2‐sided]), we calculated that 144 patients per group were needed. Assuming each practice would identify at least five Indigenous patients, we aimed to recruit 58 general practices (29 intervention, 29 control practices).
Randomisation
Practices were randomised to the intervention or control groups, without stratification or matching, with the online tool Sealed Envelope (https://sealedenvelope.com/simple-randomiser/v1). Randomisation was undertaken by an independent third party, but the investigators were not blinded to allocation.
The intervention
WoTWoD identifies four dimensions for embedding cultural respect in general practice: the community, interface with the community, consulting and clinical environment, and professional organisations. WoTWoD encompasses a toolkit, one half‐day workshop, cultural mentor support for the practice, and a local care partnership of participating Medicare Locals/PHNs and local ACCHSs for guiding the program and facilitating community engagement.15
The toolkit includes ten scenarios that illustrate cross‐cultural behaviour in clinical practice. Based on events described during comprehensive community consultations, the scenarios underpin the practical guidance for embedding cultural respect in policies and service delivery. The workshop educated intervention practice staff about cultural respect principles and using the WoTWoD cultural respect toolkit for translating principles into practice. Practice staff met the Indigenous cultural mentor who supported them during the study period in person and by phone (monthly scheduled support calls).
For the intervention group, a moderated, closed online discussion group was established to discuss the toolkit scenarios once a month, but was hardly used. A public WoTWoD website was available to intervention and control participants, and was visited mainly by GPs interested in the WoTWoD as a Royal Australian College of General Practitioners (RACGP) Quality Improvement and Continuing Professional Development activity and by people in organisations interested in the WoTWoD program and toolkit.
The cultural mentor visited each practice at least once. Additional visits were usually requested because the practice manager or other key staff members had left the practice, so that new practice staff needed to be introduced to the study. The support sought by participating practices typically concerned locating appropriate local Indigenous services, ways to engage with local Indigenous communities, and further training for staff.
While the fidelity — that is, the degree to which the intervention was delivered as planned21 — was consistent and acceptable at the practice level, the participating Medicare Locals and PHNs differed in how they organised and prioritised Indigenous health care partnerships. One Sydney PHN incorporated the WoTWoD program as a standing item into the agenda of its Aboriginal Health Committee, the membership of which included the PHN Closing the Gap team, local Indigenous elders, and representatives from local Aboriginal community‐controlled organisations. A second Sydney PHN treated the WoTWoD as an external project. In Melbourne, practices dealt directly with the research team without formal involvement of the PHNs.
Data collection
The following data were extracted from the practice information system of each practice: the numbers of Indigenous Australians, claims for MBS item 715 and administratively related MBS items (GP management plan [MBS item 721] and team care arrangement [MBS item 723]), and instances of documentation of chronic disease risk factors.
At baseline and 12 months, practice staff completed a 20‐question cultural quotient (CQ) questionnaire (7‐point Likert scales; CQ score range, 20–140) that measured the capacity of the practice staff to deal with four dimensions of cultural diversity: metacognition (strategy), cognition, motivation, and behaviour.22 The instrument had been tested and validated by general practices in preliminary pilot studies (Supporting Information).15
Data analysis
The rates of claims for MBS items 715, 721 and 723, and of documentation of chronic disease risk factors per active Indigenous patient were calculated at baseline and at 12 months for each practice. Active patients are defined by the RACGP as those who attended the practice at least three times during the preceding two years. We did not distinguish between existing and newly identified Indigenous patients. We compared the rates of claims for MBS items 715, 721 and 723 and of risk factor documentation for the two groups over 12 months. The multivariate analysis of the changes in mean practice CQ score between baseline and 12 months in the two groups incorporated a within‐cluster effect and was adjusted for practice size, being a GP registrar training practice, the proportion of staff who had had cultural awareness training, and baseline CQ score.
Statistical analyses were completed in SPSS 25.0 (IBM) and SAS 9.4 (SAS Institute).
Ethics approval
The Human Research Ethics Committees of the Aboriginal Health and Medical Research Council of NSW (reference, 1005/14), the RACGP (reference, 14/009), UNSW Sydney (reference, HC14036) and the University of Melbourne (reference, 1441978) approved this study.
Results
Recruitment
Recruitment started in June 2014 and data collection was completed in May 2017. Twenty‐eight practices each were allocated to the intervention (135 GPs, 603 Indigenous patients at baseline) and control groups (199 GPs, 1828 Indigenous patients at baseline). Three control practices (one in Sydney, two in Melbourne) were lost to follow‐up at 12 months, but no intervention practices (Box 1).
At baseline, 20 of 28 intervention and 22 of 28 control practices were group practices. Each practice had at least one practice nurse or practice manager. Control practices generally had more GPs and patients than intervention practices; at baseline 40 control practice staff (15%) and 56 intervention practice staff (27%) had received cultural awareness training in the past 12 months. Twenty‐three intervention and 17 control practices were accredited and had registered for the PIP‐IHI, and all practices had systems for identifying Indigenous patients; 21 intervention practices and 23 control practices had systems for following up Indigenous patients. At baseline, 0.49% of active intervention practice patients were Indigenous Australians, as were 0.71% of active control practice patients (Box 2).
Claims for MBS items 715, 721 and 723, and recording of chronic disease risk factors
By the 12‐month follow‐up, 275 of 801 current active Indigenous patients (34.3%) attending intervention practices had received an MBS item 715 health check, as had 348 of 1255 (27.7%) active Indigenous patients attending control practices. The rates of recording of chronic disease factors were also similar for both groups (Box 3).
There were no significant differences between intervention and control practices in the rates of claims for MBS items 715, 721 and 723 or in the documentation of specific chronic disease risk factors after adjusting for practice attributes (practice size, being a GP registrar training practice, staff cultural awareness training) and mean baseline CQ scores (Box 4).
Cultural quotient assessment of practice staff
Because of the level of staff turnover, only 132 practice staff completed the CQ at both baseline and 12 months. The difference in baseline CQ score between these staff and the 131 who completed only the baseline assessment was not statistically significant (independent two sample t test; P = 0.60).
In the adjusted multivariate analysis of change in CQ scores, the changes for the intervention group were not statistically significantly different from those for the control group (Box 5). Further, there were no significant differences between categories of practice staff (GP, practice manager, practice nurse, receptionist) in changes in CQ scores (data not shown).
Discussion
Our cluster randomised controlled trial of an Indigenous cultural respect program did not find any statistically significant differences between control and intervention groups by 12 months in the rate of claims for MBS items 715, 721 and 723, the rates of recording of risk factors, or in changes in mean CQ scores The lack of effect of the intervention may be attributable to study design limitations, complex and indirect relationships between the intervention and the outcome measures, or contextual factors that influenced the fidelity of the intervention at the Medicare Local/PHN level and its ability to achieve measurable changes in the target behaviours.
We need to better understand the nature and the relative effects of the WoTWoD elements (the Indigenous cultural mentor;23 the toolkit and workshop15), both individually and together, on the outcome measures. Qualitative data collected as part of the mixed methods study design (not reported in this article) will assist understanding the conceptual, methodologic, and contextual reasons for our negative findings. Changes in the rate of Indigenous health checks (MBS item 715) are an appropriate measure for assessing the state of Indigenous health care, but the clinical and organisational reasons for their low usage rate were probably also reasons for our negative findings, and require further investigation.
The length of the trial (12 months) may not have been sufficient to detect significant changes in professional practice dependent on organisational changes that require time to formulate and implement. In addition, the number of Indigenous patients was small in the mainstream general practices in which the trial was conducted.
Randomisation was not stratified by practice size, and the number of large practices in the control group was greater than in the intervention group. However, practice size was not a significant factor in our multivariate analyses.
The study was conducted during the restructuring of Medicare Locals as PHNs in 2015, a period of significant change in general practice, primary care, and Indigenous health care. The associated high turnover of staff in general practices and Medicare Locals/PHNs may have influenced the intensity and fidelity of the intervention at the Medicare Local/PHN level. More importantly, many PHNs were implementing interventions for culturally respectful chronic disease management (Indigenous community engagement, local knowledge, strong local leadership, shared responsibilities, sustainable resources, and integrated data and systems),24,25 reducing the potential impact of our program. Local and regional coordination is recommended for avoiding duplicated and fragmented Close the Gap activities, particularly if a robust evaluation of outcomes is planned.
The conceptual, methodologic, and contextual lessons of our study will inform the next phase of the WoTWoD research and development program. They may also inform other initiatives for embedding and evaluating multidimensional cultural respect programs in other settings.
Conclusion
Further collaborative and participatory mixed methods research is required to examine the complexities of co‐creating, implementing, and evaluating programs that integrate “thinking and doing” cultural respect in the context of the changing needs and priorities of general practice and Indigenous communities.
Trial registration
Australian New Zealand Clinical Trials Registry ACTRN12614000797673.
Box 1 – CONSORT flow diagram of the Ways of Thinking and Ways of Doing (WoTWoD) cluster randomised controlled trial
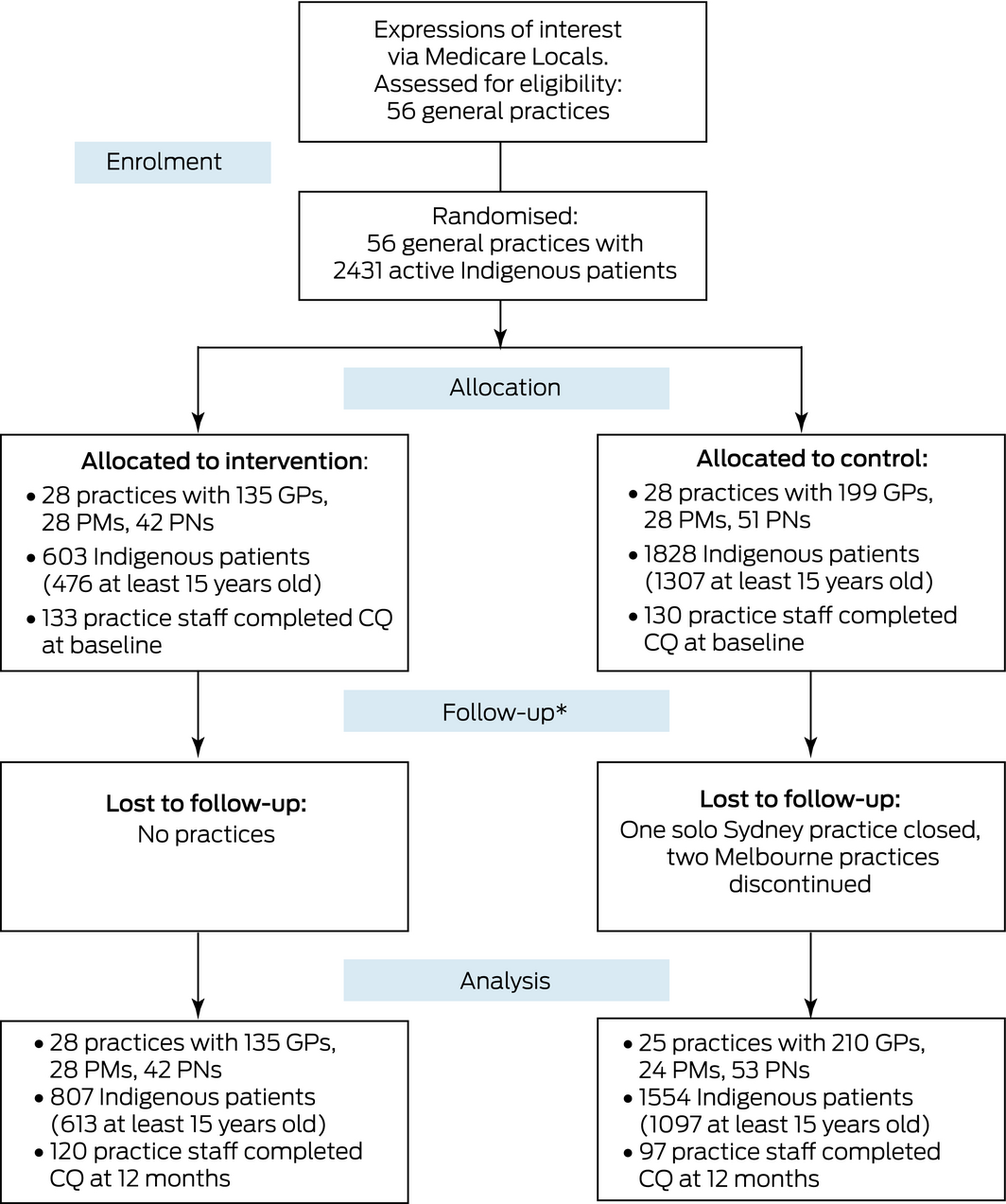
CQ = cultural quotient assessment; PM = practice manager; PN = practice nurse. * Staff turnover was high in both groups.◆
Box 2 – Characteristics of the practices included in the Ways of Thinking and Ways of Doing (WoTWoD) program
|
Characteristics |
Intervention practices |
Control practices |
|||||||||||||
|
Baseline |
At 12 months |
Baseline |
At 12 months |
||||||||||||
|
|
|||||||||||||||
|
Number of practices |
28 |
28 |
28 |
25 |
|||||||||||
|
Active patients (attended at least three times in past 2 years) |
122 111 |
124 780 |
255 811 |
227 455 |
|||||||||||
|
Indigenous active patients (proportion of all active patients) |
603 (0.49%) |
807 (0.65%) |
1828 (0.71%) |
1554 (0.68%) |
|||||||||||
|
0–14 years old |
127 (21.0%) |
188 (23.3%) |
512 (28.5%) |
419 (27.0%) |
|||||||||||
|
15–54 years old |
363 (60.2%) |
483 (59.9%) |
1088 (59.5%) |
912 (58.7%) |
|||||||||||
|
55 or more years old |
113 (18.8%) |
130 (16.1%) |
219 (12.0% |
185 (11.9%) |
|||||||||||
|
Missing data |
0 |
6 (0.7%) |
0 |
0 |
|||||||||||
|
Solo practices |
8 |
6 |
6 |
6 |
|||||||||||
|
Number of GPs, mean (SD) |
4.8 (2.9) |
5.2 (3.9) |
7.1 (6.2) |
8.4 (7.8) |
|||||||||||
|
Number of practice managers (FTEs), mean (SD) |
1.0 (0.3) |
1.0 (0.4) |
1.0 (0.5) |
0.9 (0.4) |
|||||||||||
|
Number of practice nurses (FTEs), mean (SD) |
1.5 (1.5) |
1.8 (1.5) |
1.6 (1.6) |
2.1 (2.2) |
|||||||||||
|
On‐site allied health services |
19 |
17 |
17 |
15 |
|||||||||||
|
Accredited as a general practice |
27 |
28 |
23 |
23 |
|||||||||||
|
Registered for PIP‐IHI |
23 |
24 |
17 |
18 |
|||||||||||
|
First year GP registrar employed |
12 |
11 |
9 |
13 |
|||||||||||
|
Identification of new Indigenous patients |
|
|
|
|
|||||||||||
|
Registration form |
27 |
26 |
22 |
18 |
|||||||||||
|
Asked by staff |
4 |
9 |
12 |
14 |
|||||||||||
|
Identification of existing Indigenous patients |
|
|
|
|
|||||||||||
|
Medical records |
15 |
10 |
9 |
10 |
|||||||||||
|
Asked by GPs |
12 |
14 |
18 |
15 |
|||||||||||
|
System for following up Indigenous patients by letter or phone |
21 |
28 |
23 |
21 |
|||||||||||
|
Number of staff who received cultural awareness training* in past 12 months (proportion of staff) |
56 (27%) |
91 (36%) |
40 (15%) |
37 (13%) |
|||||||||||
|
|
|||||||||||||||
|
FTE = full‐time equivalent position; PIP‐IHI = Practice Incentives Program–Indigenous Health Incentive; SD = standard deviation. * Including WoTWoD training. ◆ |
|||||||||||||||
Box 3 – Aboriginal health checks, management plans, team care arrangements, and risk factor assessments during the 12 months of the Ways of Thinking and Ways of Doing (WoTWoD) program*
|
Characteristics |
Intervention practices |
Control practices |
|||||||||||||
|
|
|||||||||||||||
|
Number of practices |
28 |
25 |
|||||||||||||
|
Active patients |
|
|
|||||||||||||
|
All active patients |
124 780 |
227 455 |
|||||||||||||
|
Indigenous active patients (proportion of active patients) |
807 (0.65%) |
1554 (0.68%) |
|||||||||||||
|
MBS services provided to Indigenous patients |
|||||||||||||||
|
Aboriginal health check (item 715) |
275/801 (34.3%) |
348/1255 (27.7%) |
|||||||||||||
|
GP management plan (item 721) |
146/787 (18.6%) |
167/907 (18.4%) |
|||||||||||||
|
Team care arrangement (item 723) |
137/787 (17.4%) |
149/898 (16.6%) |
|||||||||||||
|
Chronic disease risk factors recorded |
|||||||||||||||
|
Body mass index |
505/801 (63.0%) |
765/1293 (59.1%) |
|||||||||||||
|
Waist circumference |
135/801 (16.8%) |
283/1239 (22.8%) |
|||||||||||||
|
Blood pressure |
505/801 (63.0%) |
770/1293 (59.6%) |
|||||||||||||
|
Smoking |
594/801 (74.2%) |
726/1289 (56.3%) |
|||||||||||||
|
Alcohol intake |
380/750 (50.7%) |
543/1254 (43.3%) |
|||||||||||||
|
Cardiovascular risk factors |
183/801 (22.8%) |
293/1239 (23.6%) |
|||||||||||||
|
Blood lipid levels |
337/801 (42.0%) |
408/1254 (32.5%) |
|||||||||||||
|
Fasting blood glucose level |
228/801 (28.5%) |
264/1258 (21.0%) |
|||||||||||||
|
|
|||||||||||||||
|
MBS = Medical Benefits Schedule. * Denominators vary because of missing data. ◆ |
|||||||||||||||
Box 4 – Mean clinic rates of claims for MBS items 715, 721 and 723, and of recording of chronic disease risk factors over 12 months: multivariate analysis of group effect
|
Characteristics |
Intervention practices |
Control practices |
P (adjusted)* |
||||||||||||
|
|
|||||||||||||||
|
Number of practices |
28 |
25 |
|
||||||||||||
|
Claim rate (per Indigenous active patient), mean number (SD) |
|
|
|||||||||||||
|
MBS item 715 |
0.23 (0.25) |
0.15 (0.18) |
0.56 |
||||||||||||
|
MBS item 721 |
0.18 (0.19) |
0.24 (0.25) |
0.12 |
||||||||||||
|
MBS item 723 |
0.17 (0.18) |
0.22 (0.23) |
0.14 |
||||||||||||
|
Clinic rate of documentation of risk factors (per Indigenous active patient), mean (SD) |
|
|
|||||||||||||
|
Body mass index |
0.51 (0.31) |
0.50 (0.29) |
0.42 |
||||||||||||
|
Waist circumference |
0.14 (0.16) |
0.19 (0.24) |
0.39 |
||||||||||||
|
Blood pressure |
0.52 (0.26) |
0.64 (0.25) |
0.20 |
||||||||||||
|
Smoking |
0.66 (0.30) |
0.65 (0.34) |
0.95 |
||||||||||||
|
Alcohol intake |
0.46 (0.29) |
0.50 (0.36) |
0.34 |
||||||||||||
|
Cardiovascular risk factors |
0.19 (0.15) |
0.20 (0.17) |
0.67 |
||||||||||||
|
Blood lipid levels |
0.34 (0.18) |
0.40 (0.27) |
0.82 |
||||||||||||
|
Fasting blood glucose level |
0.22 (0.17) |
0.29 (0.28) |
0.84 |
||||||||||||
|
|
|||||||||||||||
|
MBS = Medical Benefits Schedule; SD= standard deviation. * Adjusted for the baseline mean cultural quotient score of the practice staff, practice size, being a GP registrar training practice, the proportion of staff who had had cultural awareness training, and the baseline value of the assessed characteristic. ◆ |
|||||||||||||||
Box 5 – Cultural quotient (CQ) score: multivariate analysis of group effect
|
CQ dimensions |
Change in CQ score from baseline (points), mean (standard error) |
P (adjusted)* |
|||||||||||||
|
Intervention practices |
Control practices |
||||||||||||||
|
|
|||||||||||||||
|
Metacognition |
1.67 (0.51) |
1.40 (0.54) |
0.72 |
||||||||||||
|
Cognition |
3.69 (0.97) |
0.99 (1.05) |
0.06 |
||||||||||||
|
Motivation |
2.15 (0.72) |
1.52 (0.75) |
0.55 |
||||||||||||
|
Behaviour |
2.21 (0.72) |
1.14 (0.75) |
0.31 |
||||||||||||
|
Total |
9.49 (2.29) |
4.94 (2.46) |
0.18 |
||||||||||||
|
|
|||||||||||||||
|
* Adjusted for the mean baseline cultural quotient score of the practice staff, practice size, being a GP registrar training practice, and the proportion of staff who had had cultural awareness training. ◆ |
|||||||||||||||
Received 13 March 2018, accepted 24 October 2018
- Siaw‐Teng Liaw1,2
- Vicki Wade3
- John S Furler4
- Iqbal Hasan2
- Phyllis Lau4
- Margaret Kelaher5
- Wei Xuan6
- Mark F Harris1,2
- 1 UNSW Sydney, Sydney, NSW
- 2 Centre for Primary Health Care and Equity, UNSW Sydney, Sydney, NSW
- 3 Menzies School of Health Research, Darwin, NT
- 4 University of Melbourne, Melbourne, VIC
- 5 Centre for Health Policy, University of Melbourne, Melbourne, VIC
- 6 Ingham Institute of Applied Medical Research, Sydney, NSW
We acknowledge the contributions of Lisa Jackson‐Pulver and the cultural mentors Phillip Orcher, Faye Daniels, Rhonda McPherson, Aunty Diane Kerr, and Nina Fitzgerald that ensured the cultural appropriateness of the design, implementation and interpretation of our study. The trial was funded by the National Health and Medical Research Council (APP1065491).
No relevant disclosures.
- 1. Australian Bureau of Statistics. 4727.0.55.001. Australian Aboriginal and Torres Strait Islander Health Survey: first results, Australia, 2012–13. Nov 2013. http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4727.0.55.001Main+Features12012-13?OpenDocument (viewed Dec 2018).
- 2. Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander health performance framework report 2008: detailed analyses. Canberra: AIHW, 2009.
- 3. Department of the Prime Minister and Cabinet (Australia). Closing the Gap: Prime Minister's report 2018. https://closingthegap.pmc.gov.au/sites/default/files/ctg-report-2018.pdf (viewed Dec 2018).
- 4. KPMG. National monitoring and evaluation of the Indigenous Chronic Disease Package: first monitoring report 2010–11. Canberra: Department of Health (Australia), 2013. http://www.health.gov.au/internet/main/publishing.nsf/Content/icdp-baseline-report (viewed Dec 2018).
- 5. Menzies School of Health Research. Sentinel sites evaluation: final report, February 2013. http://www.health.gov.au/internet/main/publishing.nsf/Content/icdp-sentinel-sites-project (viewed Dec 2018).
- 6. Department of Health (Australia). Aboriginal and Torres Strait Islander people. Information on health assessments and follow‐up allied health services. Updated Apr 2015. http://www.health.gov.au/internet/main/publishing.nsf/Content/mbsprimarycare_ATSI_mbsha_resource_kit (viewed Dec 2018).
- 7. Australian Institute of Health and Welfare. Indigenous health check (MBS 715) data tool (Cat. No. WEB 63). Updated 6 Dec 2017. https://www.aihw.gov.au/getmedia/b25f8967-8aa8-4382-9507-d28b9fc4a090/aihw-indigenous-healthcheck-tool-data-tables-2017.xls.aspx (viewed Dec 2018).
- 8. Australian Institute of Health and Welfare. Healthy futures — Aboriginal Community Controlled Health Services: report card 2016 (Cat No. IHW 171). Canberra: AIHW, 2016.
- 9. Australian Bureau of Statistics. Australian demographic statistics, June quarter 2016. 15 Dec 2016. http://www.abs.gov.au/AUSSTATS/subscriber.nsf/log?openagent&31010_jun%202016.pdf&3101.0&Publication&6DAF7F7C4A59465DCA25808900122564&&Jun%202016&15.12.2016&Latest.pdf (viewed Dec 2018).
- 10. Kendall E, Marshall CA. Factors that prevent equitable access to rehabilitation for Aboriginal Australians with disabilities: the need for culturally safe rehabilitation. Rehabilitation Psychology 2004; 49: 5–13.
- 11. McGrath P, Holewa H, Kail‐Buckley S. “They should come out here”: research findings on lack of local palliative care services for Australian Aboriginal people. Am J Hosp Palliat Care 2007; 24: 105–113.
- 12. Kelaher MA, Ferdinand AS, Paradies Y. Experiencing racism in health care: the mental health impacts for Victorian Aboriginal communities. Med J Aust 2014; 201: 44–47. https://www.mja.com.au/journal/2014/201/1/experiencing-racism-health-care-mental-health-impacts-victorian-aboriginal
- 13. Liaw S, Lau P, Pyett P, et al. Successful chronic disease care for Aboriginal Australians requires cultural competence. Aust N Z J Public Health 2011; 35: 238–248.
- 14. Downing R, Kowal E. A postcolonial analysis of Indigenous cultural awareness training for health workers. Health Soc Rev 2012; 20: 5–15.
- 15. Liaw S, Hasan I, Wade V, et al. Improving cultural respect to improve Aboriginal health in general practice: a multi‐methods and multi‐perspective pragmatic study. Aust Fam Physician 2015; 44: 387–392.
- 16. Australian Health Ministers’ Advisory Council Standing Committee on Aboriginal and Torres Strait Islander Health Working Party. AHMAC cultural respect framework for Aboriginal and Torres Strait Islander health, 2004–2009. Adelaide: Department of Health, South Australia, 2004. http://iaha.com.au/wp-content/uploads/2013/03/000211_culturalrespectframework.pdf (viewed Dec 2018).
- 17. Carson B, Dunbar T, Chenhall R, Bailie R. Social determinants of Indigenous health. Sydney: Allen and Unwin, 2007.
- 18. Couzos S, Thiele D. The International Covenant on Economic, Social and Cultural Rights and the right to health: is Australia meeting its obligations to Aboriginal peoples? Med J Aust 2007; 186: 522–524. https://www.mja.com.au/journal/2007/186/10/international-covenant-economic-social-and-cultural-rights-and-right-health
- 19. Australian Government. Statistics, boundary and concordance files. Oct 2013. Archived: https://web.archive.org/web/20140226184705/http://www.medicarelocals.gov.au/internet/medicarelocals/publishing.nsf/Content/digital-boundaries (viewed Dec 2018).
- 20. Department of Health (Australia). PHN background. Updated 19 July 2018. http://www.health.gov.au/internet/main/publishing.nsf/Content/PHN-Background (viewed Dec 2018).
- 21. Horner S, Rew L, Torres R. Enhancing intervention fidelity: a means of strengthening study impact. J Spec Pediatr Nurs 2006; 11: 80–89.
- 22. Ang S, Van Dyne L. Handbook of cultural intelligence: theory, measurement and applications. New York (NY): ME Sharpe, 2008.
- 23. Liaw ST, Wade V, Lau P, et al. Safe and effective cultural mentorship in general practice. Aust Fam Physician 2016; 45: 431–436.
- 24. National Health and Medical Research Council. Cultural competency in health: a guide for policy, partnerships and participation. Canberra: NHMRC, 2005. https://nhmrc.gov.au/about-us/publications/cultural-competency-health#block-views-block-file-attachments-content-block-1 (viewed Dec 2018).
- 25. Bailie R, Si D, Dowden M, et al. Improving organisational systems for diabetes care in Australian Indigenous communities. BMC Health Serv Res 2007; 7: 67.





Anamika Anamika
The interventions of the program appear to have lacked efficient implementation and robust evaluation processes, and help us to understand the value of adequately powered randomisation, sample sizing, active participation and effective feedback from medical staff and patients, local and regional coordination, and the need to be prepared for unanticipated influencers such as high staff turnover during the program. (1)
Furthermore, reducing barriers to improved cultural respect such as communication, discrimination and externally developed programs can be facilitated by:
• Accessible health services that are affordable and culturally appropriate
• Active community participation by ensuring Indigenous ownership and governance to build capacity of local communities
• Continuous quality improvement by undertaking program evaluation and encouraging research with an emphasis on Indigenous equity in professional practice
• Increasing the size of the Indigenous health workforce, which is fundamental to closing gaps in Indigenous life expectancy.
Facilitating self-determination and empowerment through increased employment, training and educational benefits are also great enablers to engage community members in health services. (2) (3)
Incorporating key features of Aboriginal Community Controlled Health Services (ACCHS) as an individual component of healthcare might be beyond the scope of this program but would support a culturally respectful health system and improve Aboriginal health outcomes in Australia. (4) (5) Successful programs like The Strong Women, Strong Babies, Strong Culture Program in remote Aboriginal communities, reflect the following three components as legitimate elements of healthcare, enabling effective governance and integrated organisational commitment:
1. Adequate funding for community-based staff
2. Infrastructure for effective implementation of the program
3. Appropriate governance mechanisms to facilitate local control over the Programs. (5)
Research shows that a Community Controlled Model based on multi-sectoral collaboration and a mutual aim to expand cultural dimensions of Indigenous communities can provide a holistic approach to improving Indigenous health and well-being. Achieving such agendas as a national priority is bound to bring celebration and joy to the Native spirits of Australia. (4) (5)
References:
1. Liaw S, Wade V, Furler JS, Hasan I, Lau P, Kelaher M, et al. Cultural respect in general practice: a cluster randomised controlled trial. The Medical Journal of Australia. 2019 March 25; 210(6): p. 263-268.
2. Freeman T, Edwards T, Baum F, Lawless A, Jolley G, Javanparast S, et al. Cultural respect strategies in Australian Aboriginal primary health care services: beyond education and training of practitioners. Australian and New Zealand Journal of Public Health. 2014; 38(4): p. 355-361.
3. Harfield SG, Davy C, McArthur A, Munn Z, Brown A, Brown N. Characteristics of Indigenous primary health care service delivery models: a systematic scoping review. Globalization and Health. 2018 January; 14(12).
4. Reid JB, Taylor K, Hayes C. Chapter 11: Indigenous health systems and services. In Willis E, Reynolds L, Keleher H. Understanding the Australian Health Care System.: Elsevier Australia; 2012.
5. Lowell A, Kildea S, Liddle M, Cox B, Paterson B. Supporting aboriginal knowledge and practice in health care: lessons from a qualitative evaluation of the strong women, strong babies, strong culture program. BMC Pregnancy Childbirth. 2015 February 5; 15(19).
Competing Interests: No relevant disclosures.
Ms Anamika Anamika
Monash University