Standardised national surveillance of health care‐associated Staphylococcus aureus bloodstream infections (HA‐SABs)1 has found that rates are declining in Australia.2 The incidence of community‐associated SABs (CA‐SABs), however, has not been investigated. These infections frequently have complicated courses (eg, metastatic sites of infection)3 and high mortality (about 20%).4
During calendar years 2016 and 2017, the Victorian Healthcare Associated Infection Surveillance System (VICNISS) and Healthcare Infection Surveillance Western Australia (HISWA) received reports from affiliated hospitals about increases in the frequency of CA‐SABs. We sought to formally review trends in their incidence and to determine whether populations at particular risk could be identified. We analysed quarterly data for the period 1 January 2011 – 31 December 2016 from 93 Victorian public hospitals (VICNISS) and 58 Western Australian public hospitals (HISWA). As a quality assurance evaluation of surveillance data, no patient‐identifying or hospital‐level data were captured; formal ethics review was therefore not required.
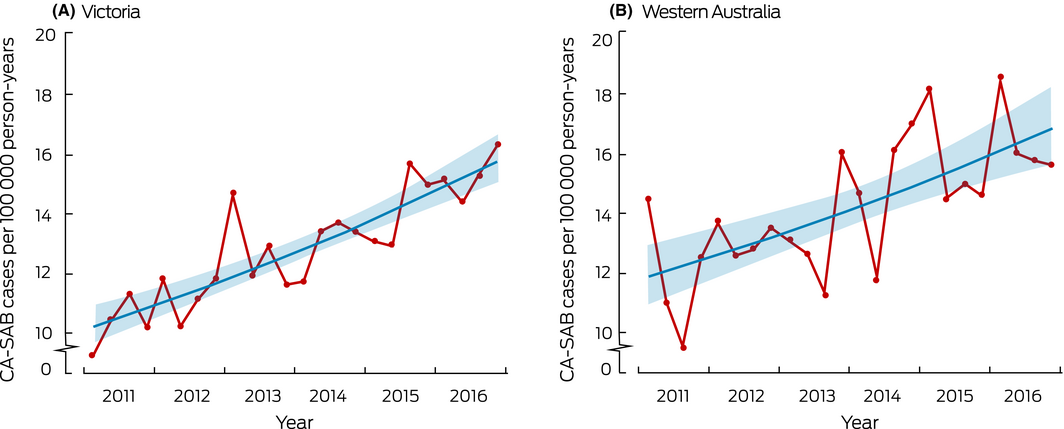
A total of 10 320 SAB events were reported (7262 in Victoria, 3058 in WA); 6800 infections (65.9%) were community‐associated, corresponding to an aggregate crude rate of 13.3 CA‐SABs per 100 000 person‐years (Victoria, 12.9; WA, 14.3 CA‐SABs per 100 000 person‐years). The incidence in each state increased significantly during the study period: 8% (95% confidence interval [CI], 6–10%) per year in Victoria and 6% (95% confidence interval [CI], 4–9%) per year in WA (Box).
Most CA‐SABs (5698, 83.8%) were caused by methicillin‐susceptible S. aureus (MSSA). There was a small but statistically significant annual increase in the proportion of MSSA CA‐SABs in Victoria (4% per year; 95% CI, 3–8%), but not in WA; that is, the incidence of CA‐SABs caused by MSSA rose more rapidly in Victoria than the overall incidence of CA‐SABs.
The incidence of CA‐SABs was higher among older patients and in men, and was particularly high for men over 60: the standardised incidence in this group was 50.9 cases (95% CI, 48.5–53.4) in Victoria and 56.7 cases (95% CI, 52.6–61.0) per 100 000 person‐years in WA, twice the incidence among women of the same age (Victoria, 24.7 [95% CI, 23.2–26.4]; WA, 24.9 [95% CI, 22.4–27.7] cases per 100 000 person‐years).
Our study is the first to evaluate the epidemiology of CA‐SAB in more than one Australian state. Other investigators have similarly reported a greater disease burden for older people and men.4 It is notable that residents of aged care facilities have been identified as being at particular risk;5 infections in this group would be classified as CA‐SABs by our analysis. One limitation of our study was that only infections in patients presenting to public hospitals are captured by surveillance systems, perhaps missing some community‐onset infections, but the vast majority of patients with SABs would require admission to hospital. Some infected persons would have been managed entirely in private health care, meaning that we will have underestimated the incidence of CA‐SABs.
The increases in incidence we describe may reflect the emergence of virulent S. aureus strains in the community or changes in host risk factors. Characterising the isolates responsible for infection would assist identify virulence factors and the relatedness of isolates. Further evaluation of infection risks in people over 60 years of age is also needed for developing targeted prevention strategies.
Received 5 July 2018, accepted 13 September 2018
- 1. Australian Commission on Safety and Quality in Health Care. Implementation guide for surveillance of Staphylococcus aureus bacteraemia. Sydney: ACSQHC, 2013. https://www.safetyandquality.gov.au/wp-content/uploads/2012/02/SAQ019_Implementation_guide_SAB_v10.pdf (viewed June 2018).
- 2. Worth LJ, Spelman T, Bull AL, Richards MJ. Staphylococcus aureus bloodstream infection in Australian hospitals: findings from a Victorian surveillance system. Med J Aust 2014; 200: 282–284. https://www.mja.com.au/journal/2014/200/5/staphylococcus-aureus-bloodstream-infection-australian-hospitals-findings
- 3. Tong SYC, Davis JS, Eichenberger E, et al. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev 2015; 28: 603–661.
- 4. Turnidge JD, Kotsanas D, Munckhof W, et al. Staphylococcus aureus bacteraemia: a major cause of mortality in Australia and New Zealand. Med J Aust 2009; 191: 368–373. https://www.mja.com.au/journal/2009/191/7/staphylococcus-aureus-bacteraemia-major-cause-mortality-australia-and-new
- 5. Agostino JW, Ferguson JK, Eastwood K, Kirk MD. The increasing importance of community‐acquired methicillin‐resistant Staphylococcus aureus infections. Med J Aust 2017; 207: 388–393. https://www.mja.com.au/journal/2017/207/9/increasing-importance-community-acquired-methicillin-resistant-staphylococcus





We acknowledge the infection control consultants in Victorian and Western Australian hospitals who collected the data we analysed. VICNISS is fully funded by the Victorian Department of Health and Human Services; HISWA is a program in the Public Health Division of the Department of Health Western Australia.
No relevant disclosures.