The known Unintentional and deliberate poisoning is a major health problem in Australia.
The new The different patterns of poisoning exposure in Australia at different ages, as reflected in calls to Poisons Information Centres, are detailed for the first time. The circumstances of exposure and the types of substances involved differ markedly between age groups.
The implications Poisons Information Centre data can inform appropriately targeted public health planning and interventions for different age groups.
Australian Poisons Information Centres (PICs) were established during the 1960s as part of an international response to a sharp increase in the number of childhood poisonings. Australia currently has four PICs (New South Wales, Queensland, Victoria, Western Australia) that together provide a national 24-hour free advice service to the public and health professionals. The core functions of PICs include risk assessment, providing management and treatment information for all types of poisoning (including by medicines, chemicals, venomous animals, plants) as well as general advice on medications and toxic hazard situations.1
Poisons exposure data are regularly published overseas; annually, for instance, in the United States and the United Kingdom.2,3 In contrast, Australian publications on the epidemiology of poisoning have been limited to hospital data, either from a single service (eg, the Hunter Area Toxicology Service4), aggregated coded data on presentations (eg, by the Australian Institute of Health and Welfare [AIHW]5), or as individual PIC annual reports. Hospital data are highly selective, biased toward symptomatic, more severe, and deliberate self-poisoning cases, and do not reflect the full spectrum of Australian poisoning exposures.
As the available Australian data are not suitable for assessing potentially modifiable factors that increase the risk of unintentional poisoning, we determined the characteristics of poisoning exposures in Australia by examining the types of calls received by PICs, analysing poisoning exposures by age group, circumstances of exposure, and the types of substances involved.
Methods
Data source, extraction and harmonisation
Each PIC caller receives advice from a Specialist in Poison Information (SPI), a pharmacy or science graduate with specific training in toxicology; risk assessment is a core part of their training. SPIs are also supported by protocols, and complex calls from health professionals may be referred to clinical toxicologists. SPIs prospectively record call information and advice in a database during the call, and practice standards include peer review of calls.1 The recorded data serve as brief medical records and as tools for audits and toxico-vigilance. Each PIC maintains a separate database; the key fields recorded by each centre are listed in the online Appendix, tables 1–3.
Cases are classified as poisoning exposures if the exposure has the potential to cause toxicity, whether or not it results in major toxicity. Age groups are defined as neonates, 0–4 weeks; infants, 4 weeks to 11 months; toddlers, 1–4 years; children, 5–14 years; adolescents, 15–19 years; adults, 20–74 years; older adults, over 74 years of age.
Data for calls received during the 2015 calendar year were retrospectively extracted from each PIC database. Prior to analysis, key database fields were harmonised with New South Wales PIC categories (as the NSWPIC receives the greatest number of calls). Missing data were coded as “unknown”. Calls about poisoning exposures of animals were excluded, but calls about humans exposed to veterinary products were included in our analysis.
Data analysis
For each age group we examined the frequencies of call categories, caller types and sex, circumstances and routes of exposure, substance types, and recommended management setting.
Substances were classified according to the Therapeutic Goods Administration (TGA) Standard for Uniform Scheduling of Medicines and Poisons, which stipulates the required restrictions and warnings for medicines and poisons.6 The categories employed were Unscheduled, Schedule 2 (pharmacy medicine), Schedule 3 (pharmacist-only medicine), Schedule 4 (prescription-only medicine), Schedules 5–7 (respectively: caution, poison, dangerous poison; pooled because it was difficult to determine the schedules of products containing several components), Schedule 8 (controlled drug), Schedule 9 (prohibited substance), and not applicable (eg, animal bites and plants). Of the 1817 substances implicated in 179 195 of 182 294 reported exposures (98.3%), we classified the 1720 most frequently cited substances for our analysis; the remaining 97 were not classified because they were so rarely involved. When a substance appeared in more than one schedule, the highest schedule was allocated, except for paracetamol (Schedule 2) and benzodiazepines (Schedule 4), which were assigned to their most frequently designated schedule. Australian Bureau of Statistics demographic statistics (June 2015)7 were used for calculating population rates. Data were analysed in Excel 2013 (Microsoft) and GraphPad Prism 7.02 (GraphPad Software).
Ethics approval
Ethics approval was granted by the Sydney Children’s Hospitals Network Human Research Ethics Committee (reference, LNR/16/SCHN/44).
Results
All calls to Poisons Information Centres
In 2015, 204 906 calls (including re-calls about the same exposure) were made to the four PICs (861 calls/100 000 population); 69.0% were received from the general public and 27.9% from health professionals. Call volumes by state reflected the proportions of people living in each state (online Appendix, table 4). Most calls (170 469 calls, 83.2%) were about poisoning exposures; 31 514 (15.4%) were calls for general information, of which 21 361 (67.8%) were medicine information requests (online Appendix, table 5). The most frequent caller types were family members (44.9%) and the person involved (19.0%) (online Appendix, table 6).
Poisoning exposure calls
A total of 170 469 calls concerned 164 363 poisoning exposures in humans (691 exposures/100 000 population). The most frequent exposure circumstances were unintentional exposure (64.4% of exposures) and medication error (18.1%) (online Appendix, table 7); most exposures were by oral ingestion (81.0%) (online Appendix, table 8). The substances most frequently involved were household cleaning agents (10.2% of substances involved) and paracetamol-containing analgesics (7.3%) (Box 1); the age groups most frequently affected were adults (40.1%) and toddlers (36.0%), but the exposure rates were highest for infants (5276 cases/100 000 population) and toddlers (4779 cases/100 000 population) (Box 2).
Of the 164 363 exposures, 17 949 callers (10.9% of exposures) were advised to go to hospital and 110 836 (67.4%) to stay at home (online Appendix, table 9). A total of 26 620 calls (15.6%) were about people in hospitals, of which 3862 (14.5%) were referred to toxicologists. The proportions of calls from hospitals (44.7%) and of people referred to hospital (23.9%) were each greatest for adolescents (Box 2). Most people calling about neonates (74.5%), infants (88.5%), toddlers (86.4%), or children (72.9%) were advised to stay at home.
Exposure substances and scheduling
Most calls about neonates (73%), infants (76%), toddlers (78%), and children (63%) involved non-medicinal and over-the-counter medicines. The proportion of exposures related to prescription items increased with age, from 13% for neonates and 7% for infants to 62% for older adults (Box 3). Exposures to substances in Schedules 5–7 constituted the largest single category of unintentional exposures in adolescents (22%), adults (40%), and older adults (31%) (Box 4). Unintentional exposures to Schedule 3 (pharmacist-only drugs, such as cold preparations including pseudoephedrine), Schedule 8 (controlled drugs, such as oxycodone), and Schedule 9 (prohibited substances, such as heroin) were the least frequent in all age groups (Box 4). In contrast, deliberate self-poisoning predominantly involved Schedule 4 (prescription-only medicines) and Schedule 2 (pharmacy medicines) items (Box 5).
For the purposes of preventive strategies, it is useful to examine the frequency of exposure by age (Box 2; online Appendix, tables 10–16) and the circumstances of exposure (Box 6). The proportion of exposures caused by deliberate self-poisoning was greatest for adolescents (49.1% of exposures), most involving pharmaceuticals such as antidepressants, paracetamol, non-steroidal anti-inflammatory drug (NSAIDs), and antipsychotics (Box 6; online Appendix, table 14). Exposures of adults under 74 were mostly unintentional (41%), medication errors (25%; 102 exposures/100 000 population), and deliberate self-poisoning (20%) (Box 6). Most exposures in older adults were medication errors (64%; 151 exposures/100 000 population), particularly with cardiovascular (23.6%), anticoagulant (4.6%), antidiabetic (4.1%), and opioid (3.6%) prescription medications or with paracetamol-containing analgesics (7.2%) (Box 6; online Appendix, table 16).
Sex differences
In the adolescent group, 77% of deliberate self-poisonings, 66% of adverse reactions, and 61% of unintentional exposures were in girls, while 60% of recreational exposures were in boys. Most calls about exposures of older adults, including adverse reactions (63%), unintentional (61%) and deliberate self-poisoning (55%), food poisoning (91%), and medication errors (68%) were about women; most workplace exposures (69%) involved men (online Appendix, table 17).
Discussion
Public health initiatives for preventing poisoning must be based on evidence about the nature of exposures in the community and in hospitals. Our study provides a comprehensive overview of age group-specific patterns of poisoning exposures in Australia, based on more than three times the number of hospital cases recorded by national health statistics.5 The most likely reason for this difference is that International Classification of Disease (ICD) hospital coding captures poisoning poorly,8 and only admitted patients are assigned an ICD code (many patients are sent home after observation). ICD coding does not generally identify specific agents. The ratios of pharmaceuticals to non-pharmaceuticals in our dataset and in national admitted patient data5 were similar, but further relevant details are not collected with ICD codes. PIC data prospectively coded by specialists in poisons information provide accurate and specific substance data for both hospital and community exposures.
The distribution of exposed persons by age group, exposure circumstances, exposure substances, exposure routes, and recommended management was broadly similar to that reported for calls about poisoning in other developed countries.2,3,9 Our data confirm that most poisoning exposures in Australia (as elsewhere) are unintentional, and a smaller proportion are caused by medication error or deliberate self-poisoning. The high proportion of callers advised to stay at home, averting unnecessary hospital presentations, relies heavily on good poisoning risk assessment expertise.
We found significant variation in exposure circumstances with age. Medication error was most common in neonates and older adults, but management was quite different. Only 3.8% of neonates were referred to hospital, most callers being advised to stay at home, although 16.2% of calls about neonates were from hospital. As self-administration is unlikely, most poison exposures in neonates and infants result from administration by family members or carers.
Referral to health facilities were more common for exposures in older adults, possibly reflecting the toxicity of the substances involved, as well as drug and disease interactions. Exposures in children under 5 years of age were very common, but most callers were advised to stay at home, probably reflecting the relatively benign nature of the exposures. Adolescents and adults were more frequently referred to hospital or were already in hospital, consistent with the higher rates of deliberate self-poisoning in these age groups.
Scheduling should reduce access to poisons, but it is difficult to evaluate its effectiveness in preventing poisoning in a cross-sectional study. Schedule 8 medications were least often implicated in unintentional and deliberate self-poisoning in all age groups, suggesting that scheduling an item as Schedule 8 — with stringent criteria for prescribing, storage and dispensing — is effective in reducing access and poisonings. Up-scheduling the anxiolytic alprazolam from Schedule 4 to 8 has reduced the numbers of prescriptions and of PIC calls related to this agent.10 The restrictions on Schedules 5–7 agents (predominately non-pharmaceutical chemicals, such as pesticides) are mainly labelling requirements and do not generally reduce their availability; many are as freely accessible in supermarkets as unscheduled and Schedule 2 products. Schedule 2 and 4 products predominated in cases of deliberate self-poisoning (Box 5), reflecting a strong preference for medications to chemical products for this purpose.
The proportion of deliberate self-poisoning exposures was highest among adolescents, and the hospital referral rate was consequently highest for this age group, consistent with other findings on adolescent deliberate self-poisoning.11,12 Poisoning with over-the-counter medications (including paracetamol and NSAIDs) was common in this group, suggesting that reducing sales of these agents to adolescents would be a useful prevention strategy.12 High rates of poisoning with antidepressants and antipsychotics indicate that prescribing these agents should be restricted to those most likely to benefit, and their toxicity profile should be considered when prescribing them for adolescents at higher risk of deliberate self-poisoning.
Substances involved in exposures of adults under 74 years of age were often prescribed and misused medications, such as selective serotonin re-uptake inhibitors, antipsychotics (especially quetiapine), and benzodiazepines. These medications are frequently prescribed outside guideline recommendations.13 Practitioners and others who facilitate access to these agents should be encouraged to adhere to guideline recommendations.
The proportion of exposures in adults over 74 years of age attributable to medication error (64%) was more than twice that for younger adults (25%), although the difference was reduced by correcting for population size (151 v 102 exposures/100 000 population). The medications most frequently involved were those commonly used by people in this age group, including cardiovascular, antihypertensive, anticoagulant, lipid-lowering, analgesic, and anti-inflammatory medications.14 Outcomes in this age group are generally more severe than for younger people.4 Prevention strategies specific to this population could include improved packaging and labelling, standardised container designs, and improved legibility (online Appendix, table 18).
Poisoning should be considered in a framework that takes socio-economic and psychological factors that facilitate access to or availability of toxins into account. For example, low socio-economic status and a non-English-speaking background are potentially risk factors for poisoning.15 Public health frameworks for injury reduction, such as the Haddon matrix, have been successfully applied to reducing rates of deliberate self-poisoning.16 Our findings suggest that different poisoning profiles apply in different age groups, warranting a range of public health responses that modify physical and social environments, the agents, and age-specific human-related factors. Haddon matrices of interventions for reducing the incidence of the most common poisoning type in specific age groups (online Appendix, tables 18–20) highlight the range of opportunities available.
Better quality data on resource use, morbidity and mortality, and for other outcomes of poisoning in Australia are required. Prospective investigations of the circumstances of poisoning and the effectiveness of interventions may identify more successful age-specific preventive strategies. For example, ingestion of a single verapamil tablet by a child is potentially fatal, but this medication is provided in blister packaging not subject to performance testing.17 Further, the effectiveness of changes in the 2008 childproof packaging regulations17 has not been evaluated. Combining the data from PIC calls and hospital and coronial data could assist in this regard.
Most funding for Australian PICs is directed to providing the phone information service. PICs have recently increased their public awareness and education activities on various media platforms. PICs have identified unexpected and emerging hazards18 and emerging problems related to deliberate self-poisoning,19 have responded to changes in drug regulation,10 and have recommended packaging changes.20 Such activities are ad hoc and largely unfunded. Better support for nationwide preventive activities, such as education, toxico-vigilance, and policy effectiveness research, is needed, as they could be highly cost-effective approaches to reducing poisoning rates.
Limitations
Our study has several limitations. An unknown proportion of Australian poisonings do not lead to PIC calls; hospitals with specialist toxicology centres do not need to contact PICs; experienced general practitioners and hospital clinicians may not consult PICs. Our study therefore underestimates the full extent of poisoning in Australia. Data were gathered from four different databases with different substance lists. To ensure accurate recoding of data, we checked product classifications against the substance and advice, and also clarified individual PIC practices by consulting heads of departments. Merging data on individual substances into broad categories may have caused some error in our estimates, but the consequent data loss would have been minimal. Callers do not always identify their call as being a re-call, so that exposure numbers may have been overestimated, but by no more than 1% (assessment by PIC heads of departments). There are no outcomes data for poisoning exposures reported to PICs, as PICs do not routinely follow up calls; it would be useful were PICs able to do so through linkage with hospital data.
Conclusion
Our findings highlight the ongoing role of and need for PICs in providing toxicology expertise to the public and to health professionals. We provide a broad overview of poisoning exposures in the Australian population and have identified age-based poisoning profiles that require multifaceted public health intervention responses. PICs are optimally positioned to inform the effectiveness of such actions and interventions, but are an underutilised resource for these and other toxico-vigilance activities.
Box 1 – Substances most frequently cited in 164 363 exposures reported to four Australian Poisons Information Centres (re-calls excluded), 2015; all age groups
|
Substance type |
Exposures |
Proportion of exposure substances |
Most common substance in this class |
||||||||||||
|
|
|||||||||||||||
|
Total number |
164 363 |
|
|
||||||||||||
|
Household cleaning substances |
18 542 |
10.2% |
Bleaches, 2685 (14.5%) |
||||||||||||
|
Paracetamol-containing analgesics |
13 322 |
7.3% |
Paracetamol, 10712 (80.4%) |
||||||||||||
|
Antidepressants |
7732 |
4.2% |
Sertraline,* 1162 (15.0%) |
||||||||||||
|
Cosmetic/personal care product/toiletries |
7607 |
4.2% |
Soap, 1118 (14.7%) |
||||||||||||
|
Non-steroidal anti-inflammatory drugs (NSAIDs) |
7167 |
3.9% |
Ibuprofen, 5208 (72.7%) |
||||||||||||
|
Cardiovascular agents |
6260 |
3.4% |
β-Blockers, 1382 (22.1%), including metoprolol,* 465 (7.4%) |
||||||||||||
|
Bites/stings |
6104 |
3.3% |
Spiders, 2625 (43.0%) |
||||||||||||
|
Sedatives |
5221 |
2.9% |
Benzodiazepines, 4344 (83.2%), including diazepam,* 2374 (45.5%) |
||||||||||||
|
Pesticides |
5061 |
2.8% |
Pyrethrins/pyrethroids, 2285 (45.1%) |
||||||||||||
|
Antipsychotics |
4956 |
2.7% |
Quetiapine, 2688 (54.2%) |
||||||||||||
|
|
|||||||||||||||
|
* Victorian data excluded because it contained insufficient information on these substances. Total number of exposure substances: 182 292. |
|||||||||||||||
Box 2 – Poisoning exposures and recommended management setting for 164 363 exposures reported to four Australian Poisons Information Centres (re-calls excluded), 2015; by age group
|
Age group |
Exposures |
Age standardised rate (per 100 000 population*) |
Recommended management |
||||||||||||
|
Stay at home |
In hospital |
Referred to hospital |
Other† |
||||||||||||
|
|
|||||||||||||||
|
Neonate |
216 (0.1%) |
925.5 |
74.5% |
16.2% |
3.8% |
5.5% |
|||||||||
|
Infant |
14 775 (9.0%) |
5275.7 |
88.5% |
5.7% |
3.6% |
2.2% |
|||||||||
|
Toddler |
59 121 (36.0%) |
4779.4 |
86.4% |
6.0% |
5.0% |
2.6% |
|||||||||
|
Child |
13 561 (8.3%) |
461.9 |
72.9% |
13.0% |
9.2% |
4.9% |
|||||||||
|
Adolescent |
6745 (4.1%) |
457.0 |
25.7% |
44.7% |
23.9% |
5.7% |
|||||||||
|
Adult |
65 908 (40.1%) |
405.1 |
49.3% |
25.5% |
16.7% |
8.5% |
|||||||||
|
Older adult |
3676 (2.2%) |
235.9 |
62.4% |
14.4% |
14.3% |
8.9% |
|||||||||
|
Unknown |
361 (0.2%) |
NA |
30.5% |
23.0% |
28.3% |
18.2% |
|||||||||
|
Total |
164 363 |
691.1 |
67.4% |
16.2% |
10.9% |
5.5% |
|||||||||
|
|
|||||||||||||||
|
NA = not applicable. * Population at June 2015.8 † At general practice, referred to general practitioner, or unknown. |
|||||||||||||||
Box 3 – Proportions of substances (by broader medicinal categories) cited in calls to four Australian Poisons Information Centres (re-calls excluded), 2015; by age group
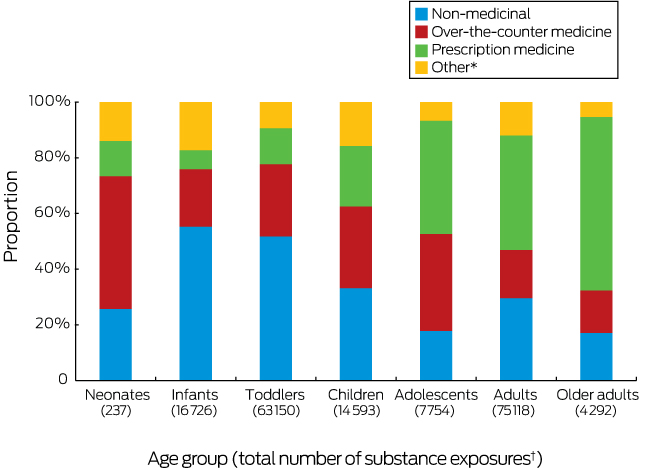
* Includes bites and stings, and poisoning by plants and foreign materials. † Numbers of exposures for individual age groups can exceed numbers of people in because a person can be exposed to several agents in one exposure.
Box 4 – Schedule status7 of substances cited in calls to four Australian Poisons Information Centres (re-calls excluded) about unintentional poisoning, 2015; by age group
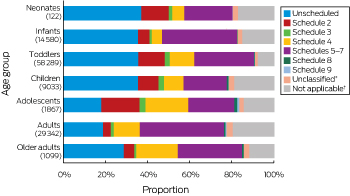
* Substances that we did not classify because they were so rarely cited in calls. † Includes animal bites and plant materials.
Box 5 – Schedule status7 of substances cited in calls to four Australian Poisons Information Centres (re-calls excluded) about intentional poisoning, 2015; by age group (excluding children aged 0–4 years)
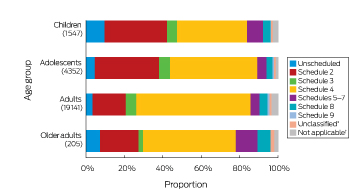
* Substances that we did not classify because they were so rarely cited in calls. † Includes animal bites and plant materials.
Box 6 – Exposure circumstances for 164 363 exposures reported to four Australian Poisons Information Centres (re-calls excluded), 2015; by age group
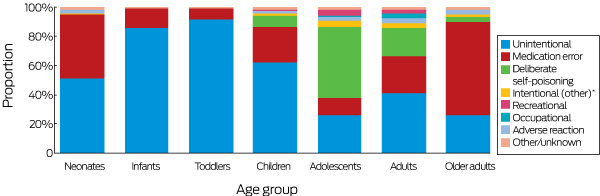
* Intentional medication misuse or intended use outside of recommended/prescribed dosage; excludes recreational use. For definitions of other circumstances, see online Appendix, table 7. The total numbers of exposures for each age group are listed in .
Received 30 October 2017, accepted 29 March 2018
- Alanna Huynh1,2
- Rose Cairns1,2
- Jared A Brown1
- Ann-Maree Lynch3
- Jeff Robinson4
- Carol Wylie5
- Nicholas A Buckley1,2,6
- Andrew H Dawson1,2,6
- on behalf of the Synthesis of the Network of Australian Poisons Services' Health Outcomes and Treatment (SNAPSHOT) investigators
- 1 NSW Poisons Information Centre, Children's Hospital at Westmead, Sydney, NSW
- 2 Sydney Medical School, University of Sydney, Sydney, NSW
- 3 Western Australian Poisons Information Centre, Sir Charles Gairdner Hospital, Perth, WA
- 4 Victorian Poisons Information Centre, Austin Health, Melbourne, VIC
- 5 Queensland Poisons Information Centre, Lady Cilento Children's Hospital, Brisbane, QLD
- 6 Royal Prince Alfred Hospital, Sydney, NSW
Our study was supported by a National Health and Medical Research Council program grant (1055176). We thank the staff of the New South Wales, Queensland, Victorian, and Western Australian Poisons Information Centres.
No relevant disclosures.
- 1. Robinson J, Wylie C, Lynch C, Lynch AM. Practice standards for Australian Poisons Information Centres 2014. https://www.childrens.health.qld.gov.au/wp-content/uploads/PDF/poisons/poison-prac-standards-2014.pdf (viewed Oct 2017).
- 2. Mowry JB, Spyker DA, Brooks DE, et al. 2015 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd annual report. Clin Toxicol 2016; 54: 924-1109.
- 3. National Poisons Information Service (UK). NPIS annual reports. http://www.npis.org/annualreports.html (viewed Mar 2018).
- 4. Pillans PI, Page CB, Ilango S, et al. Self-poisoning by older Australians: a cohort study. Med J Aust 2017; 206: 164-169. <MJA full text>
- 5. Australian Institute of Health and Welfare. Trends in hospitalised injury, Australia 1999–00 to 2012–13 (AIHW Cat. No. INJCAT 171). Canberra: AIHW, 2015.
- 6. Therapeutic Goods Administration. Poisons standard. February 2017 (F2017L00057). https://www.legislation.gov.au/Details/F2017L00057 (viewed May 2017).
- 7. Australian Bureau of Statistics. 3101.0. Australian demographic statistics, Jun 2015. Dec 2015. http://www.abs.gov.au/AUSSTATS/abs@.nsf/allprimarymainfeatures/6CBA90A25BAC951DCA257F7F001CC559?opendocument (viewed Nov 2016).
- 8. Du W, Pearson SA, Buckley NA, et al. Diagnosis-based and external cause-based criteria to identify adverse drug reactions in hospital ICD-coded data: application to an Australia population-based study. Public Health Res Pract 2017; 27: 2721716.
- 9. Ontario Poison Centre. Annual report 2008. http://www.ontariopoisoncentre.ca/pdf/43679-OPC_AR2008EN.pdf (viewed Nov 2016).
- 10. Schaffer AL, Buckley NA, Cairns R, Pearson SA. Interrupted time series analysis of the effect of rescheduling alprazolam in Australia: taking control of prescription drug use. JAMA Intern Med 2016; 176: 1223-1225.
- 11. Hawton K, Bergen H, Waters K, et al. Epidemiology and nature of self-harm in children and adolescents: findings from the multicentre study of self-harm in England. Eur Child Adolesc Psychiatry 2012; 21: 369-377.
- 12. Hiremath M, Craig S, Graudins A. Adolescent deliberate self-poisoning in South-East Melbourne. Emerg Med Australas 2016; 28: 704-710.
- 13. Nicholas R, Lee N, Roche A. Pharmaceutical drug misuse problems in Australia: complex issues, balanced responses. Adelaide: National Centre for Education and Training on Addiction, Flinders University, 2011. http://nceta.flinders.edu.au/files/6113/2823/3742/EN448_Nicholas_2011.pdf (viewed Aug 2017).
- 14. Morgan TK, Williamson M, Pirotta M, et al. A national census of medicines use: a 24-hour snapshot of Australians aged 50 years and older. Med J Aust 2012; 196: 50-53. <MJA full text>
- 15. Tyrrell EG, Orton E, Sayal K, et al. Differing patterns in intentional and unintentional poisonings among young people in England, 1998–2014: a population-based cohort study. J Publ Health (Oxf) 2017; 39: e1-e9.
- 16. Runyan CW. Back to the future — revisiting Haddon’s conceptualization of injury epidemiology and prevention. Epidemiol Rev 2003; 25: 60-64.
- 17. Australian Government. Child-resistant packaging requirements for medicines (Therapeutic Goods Order No. 80). 27 Aug 2008. https://www.legislation.gov.au/Details/F2014C00067 (viewed Feb 2018).
- 18. Cairns R, Brown JA, Buckley NA. Dangerous toys: the expanding problem of water-absorbing beads. Med J Aust 2016; 205: 528. <MJA full text>
- 19. Cairns R, Buckley N. Increased self-poisoning in young Australians. Why, 2KS? [abstract: 15th International Asia Pacific Association of Medical Toxicology International Scientific Conference, Singapore, 2016]; p. 71. http://www.apamt.org/wp-content/uploads/2017/07/15th_Oral_Abstract_4B-03.pdf (viewed Mar 2018).
- 20. Cairns R, Brown J, Robinson J, et al. A decade of Australian methotrexate dosing errors. Med J Aust 2016; 204: 384. <MJA full text>





Abstract
Objectives: To characterise the types of calls received by Australian Poisons Information Centres (PICs) in Australia, and to analyse poisoning exposures by age group, circumstances of exposure, and the types of substances involved.
Design, setting: Retrospective analysis of call records from all four Australian PICs (national coverage).
Main outcome measures: Basic demographic information; exposure circumstances, substance types involved in each age group; recommendations for management (eg, stay at home, go to hospital).
Results: There were 204 906 calls to Australian PICs in 2015, 69.0% from the general public, 27.9% from health professionals; 16.2% of calls originated from hospitals. 170 469 calls (including re-calls about an exposure) related to 164 363 poison exposure events; 64.4% were unintentional, 18.1% were the consequences of medication error, and 10.7% involved deliberate self-poisoning. Most exposures were of 20–74-year-old adults (40.1%) or 1–4-year-old toddlers (36.0%). The PICs advised callers to stay at home for 67.4% of exposures, and to present to hospital for 10.9%. The most common substances involved in exposures overall were household cleaners (10.2%) and paracetamol-containing analgesics (7.3%). Exposures of infants and toddlers were most frequently to household cleaning substances (17.8%, 15.3% respectively) and personal care items (6.6%, 7.3%); callers were usually advised to stay at home (88.5%, 86.4%). Deliberate self-poisoning (49.1%) and hospital referral (23.9%) were most frequent for adolescents. Exposures of adults (20–74 years) frequently involved psychotropic pharmaceuticals (17.8%) or painkillers (15.1%). Exposures in adults over 74 were typically medication errors involving cardiovascular (23.6%), anticoagulant (4.6%), or antidiabetic (4.1%) medications.
Conclusions: Poisoning is a significant public health problem throughout life, but the nature of the hazards differs markedly between age groups. PIC data could inform strategic public health interventions that target age-specific poisoning hazards.