Patients are considered to have difficult-to-treat (difficult) asthma if their asthma remains uncontrolled despite high intensity asthma therapy (ie, high dose inhaled corticosteroids plus second controller), or if high intensity therapy is required to achieve control (Box 1).1 These patients comprise a heterogeneous group, in whom intrinsically severe asthma biology, incorrect diagnoses, patient behaviour and other contributory factors may all lead to poor asthma control.
Biologically severe asthma is a subset of difficult asthma and a diagnosis of exclusion. In international guidelines, this group of patients has been referred to as having severe asthma,2 which should only be diagnosed if the asthma remains uncontrolled on high intensity medications after the exclusion of alternative diagnoses and optimisation of contributory factors. The distinction between difficult and severe asthma has important therapeutic implications. For example, expensive and novel therapies such as biologicals should be reserved for use in severe asthma only, and would not be appropriate for all patients with undifferentiated difficult asthma.
In the general community, a European study estimated that 17.4% of the adult asthma population had difficult asthma.3 Of these, only 20.5% had severe asthma, accounting for 3.6% of the adult asthma population.3
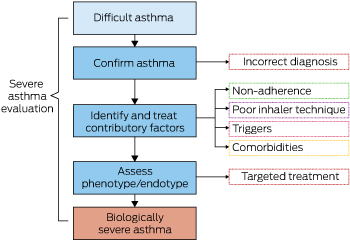
The evaluation of patients with difficult asthma can be initiated in the primary care setting, although the diagnosis of severe asthma is usually confirmed following specialist evaluation.2,4 Box 2 outlines key elements of the diagnostic process for severe asthma; in this review, we describe each step in further detail. A glossary of key terms is provided in Box 3.
Step one: confirm asthma diagnosis
The first step in establishing a diagnosis of asthma is to stratify patients according to the likelihood of asthma based on clinical symptoms and signs.5 Asthma usually presents with a combination of shortness of breath, wheeze, chest tightness or cough. However, various other pulmonary and non-pulmonary conditions can give rise to asthma-like symptoms; clinical clues suggesting alternative diagnoses should therefore be actively sought during clinical consultation (Box 4).
The next step is to seek evidence of variable airflow obstruction (VAO). The importance of this is emphasised in major guidelines6,7 because diagnosis based solely on clinical impression results in substantial misdiagnosis.8 In two different studies, one-third of patients with doctor-diagnosed asthma were found to have no evidence of asthma after objective assessment.8,9 Misdiagnosis occurs at the specialist level as well: 5% and 12% of specialist-referred patients were found to have alternative diagnoses after difficult asthma assessment in an Australian and a United Kingdom-based study, respectively.10,11 Historical evidence of VAO lends support to a diagnosis of asthma, although re-evaluation should be considered if there is substantial change in asthma symptoms in the interim.
VAO is most commonly demonstrated on spirometry, with bronchodilator reversibility (BDR) of greater than 12% and 200 mL. This test can be performed in primary care clinics using a portable office spirometer, but interpretation of results requires caution as BDR lacks sensitivity (< 50%) in differentiating asthma from healthy controls,12,13 and lacks specificity in differentiating asthma from chronic obstructive pulmonary disease.12,14 Thus, negative BDR does not exclude a diagnosis of asthma, while positive BDR may require further evaluation to differentiate from other obstructive airway diseases. Peak flow monitoring should be performed if spirometry is not available or BDR is negative, but it is highly effort-dependent and requires greater patient engagement.15
When spirometry is normal without BDR, a bronchial challenge test may be undertaken to demonstrate VAO. This may be performed with agents that directly cause airway smooth muscle constriction, such as methacholine (known as direct challenge testing) or with agents that act on airway smooth muscle through the release of inflammatory mediators, such as mannitol (indirect challenge testing). Direct challenge tests have a very high sensitivity; a negative test therefore makes the diagnosis of current asthma highly unlikely.16 A positive indirect challenge test confirms the diagnosis of asthma, and closely reflects airway inflammation and disease activity.17
It is increasingly acknowledged that there are limitations to using VAO to diagnose asthma.18 In particular, irreversible airflow obstruction due to airway remodelling can develop in asthma,19 and a distinct subset of patients with reduced lung function and negligible response to bronchodilator testing has been described.20 Nevertheless, objective demonstration of impaired airway physiology should always be sought in patients presenting with difficult asthma.
Step two: identify and treat contributory factors
Non-adherence, poor inhaler technique, exposure to triggers, and comorbid conditions can all contribute to poor asthma control. Evaluation of these contributory factors should be undertaken during every clinic consultation at both primary and specialist care levels.
Non-adherence
Non-adherence is a major problem in asthma. Studies worldwide consistently show that patients often take < 30% of their daily prescribed doses of asthma controllers.21,22 Adherence rates in patients with difficult asthma are also disappointingly low. In a Melbourne-based study, close to half of the patients with difficult asthma were non-adherent to their asthma controllers.23 In another study following hospitalisation for a severe asthma exacerbation, patient adherence to inhaled corticosteroids (ICS) was just 50% one week after discharge.24
Regular use of even low dose ICS protects against asthma deaths25 and reduces the risk of asthma exacerbations,26 with an adherence rate of = 75% giving the greatest reduction in risk of exacerbations.22 Medication non-adherence leads to adverse clinical outcomes and is associated with asthma mortality. In patients with difficult asthma, non-adherence is an independent predictor of near-fatal asthma.27
Addressing medication non-adherence first requires accurate measurement, but this may be challenging in many settings. Various methods have been proposed, each with its disadvantages.28 Patient self-report is the most convenient way to assess adherence, but this often involves over-reporting.29,30 Pharmacy prescription refill records provide an objective way to measure adherence and have been validated for use in various centres.31 However, prescription refill review cannot ensure that the medication is actually taken, and prescription records may not be readily accessible in all health care systems. Electronic dose monitors provide accurate recordings of the time and frequency of doses taken, and recorded data can be downloaded by the patient and clinician for review.32 Some electronic dose monitors also come with audio-visual reminders to improve patient adherence. Their main drawbacks are cost and the lack of a suitable device for every inhaler. Fractional exhaled nitric oxide (FENO) is a biomarker measured non-invasively from a patient’s exhaled breath. A high value (usually > 50 parts per billion) indicates eosinophilic inflammation and predicts response to corticosteroids. Suppression of FENO under directly observed controller therapy has been used as an indicator of ICS non-adherence before direct observation, although the utility of this test is limited to patients with raised baseline FENO.33
Interventions to address non-adherence should focus on its cause. Unintentional non-adherence may arise as a result of financial constraints, poor comprehension of the drug regimen, physical inability to manage medications, or simple forgetfulness. Measures to simplify drug regimens, such as using a single controller inhaler instead of multiple inhalers34,35 and the use of once-daily dosing instead of twice-daily dosing,36,37 have been shown to improve adherence. Solutions to overcome forgetfulness include using audio-visual reminders,21 keeping the inhaler in the bathroom (not recommended for dry powder inhalers) and integrating the medication as part of a daily routine.38
Intentional non-adherence arises from patients’ beliefs, which may be related to medication side effects, perceived necessity, medication effectiveness, and lack of motivation.29 A shared treatment decision-making process between the clinician and patient has been shown to improve adherence and asthma outcomes.39 This process involves sharing relevant information, expressing treatment preferences, deciding on treatment options and agreeing on treatment plans.39 Individualised self-management education also improves long term adherence.40
Inhaler technique
Inhalation is the preferred route for asthma controllers because of rapid delivery to the lungs and minimisation of systemic drug effects. Unfortunately, inhaler device techniques are not intuitive and incorrect inhaler use is a common problem. In a recent systematic review of errors in inhaler use, the prevalence of correct inhaler use was only 31%.41 The frequency of common errors was equally high for metered dose inhalers and dry powder inhalers.41
Initial selection of an inhaler device should take into consideration patient factors (age, comorbidities, preferences and adherence), disease-related factors (severity of airflow obstruction, which may impair inspiratory effort) and device factors (optimal inspiratory flow required).42 Inhaler techniques are best taught using verbal or written instruction coupled with physical demonstration, rather than verbal or written instructions alone.43 If physical demonstration is not available, instructional videos are superior to written instructions alone.44 Checking and reinforcing patients’ inhaler technique should occur at every opportunity, because inhaler technique declines over time.43 Inhaler technique checklists and instructional videos are available on the National Asthma Council Australia website (https://www.nationalasthma.org.au/living-with-asthma/how-to-videos).
Health care providers should be heartened to know that correcting inhaler technique improves asthma outcomes. In a randomised study conducted by community pharmacists, repeated education sessions lasting just 2.5 minutes per session carried out over 6 months markedly improved patients’ inhaler techniques, with accompanying improvement in peak flow readings, asthma quality of life and perceived asthma control.45
Triggers
Asthma control is adversely affected by ongoing exposure to triggers such as allergens, irritants and medications (Box 5). Asthma triggers may be more common than previously thought; in an online survey conducted in Europe, 87% of participants reported more than five asthma triggers, with asthma control worsening as the number of (and exposure frequency to) triggers increased.46 Therefore, a detailed exposure history, including work history, should always be elicited.
In many patients, allergen exposure results in sensitisation; that is, the production of allergen-specific IgE which binds to high affinity IgE receptors on mast cells and basophils. Subsequent allergen exposure cross-links these IgE molecules, triggering the release of inflammatory mediators. In severe asthma cohorts, up to 80% of patients are sensitised to aeroallergens.20,47 However, allergen sensitisation based on skin prick testing or enzyme-linked immunosorbent assays does not always mean that atopy is the main driver of disease severity.48 Other useful indicators of allergy-driven asthma include early disease onset and the presence of other atopic comorbidities, such as allergic rhinitis and atopic dermatitis. Common allergens include house dust mite, moulds, animal dander, and pollen. Complete avoidance of sensitising allergens has been shown to improve asthma outcomes,49 but measures aimed at reducing indoor allergens have so far been ineffective.50
Commonly reported irritants include smoking and environmental pollution.46 Current smokers should be counselled about smoking cessation because they experience more asthma symptoms than never-smokers and ex-smokers.51,52 Environmental tobacco smoke and outdoor air pollution are also associated with poorer asthma control.53,54 Environmental tobacco smoke has been shown to worsen lung function, decrease quality of life, increase health care utilisation,55 and has even been implicated in an acute asthma death in the United States.56
Medications such as aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) and ß-blockers may trigger asthma symptoms in susceptible patients. Between 14% and 30% of patients with severe asthma are reported to be aspirin intolerant.57,58 Patients with aspirin-exacerbated respiratory disease usually present in the third or fourth decade of life with asthma, chronic rhinosinusitis and nasal polyps. Exposure to NSAIDs also results in nasal symptoms along with wheeze and chest tightness. Severe asthma may persist despite the avoidance of NSAIDs,59,60 and both patients and physicians should be cognisant that non-oral NSAID exposure (eg, via topical routes) may also trigger asthma symptoms.61,62 Diagnosis of aspirin-exacerbated respiratory disease is often suspected based on patients’ reports of previous asthma exacerbations after NSAID exposure, although not all patients with aspirin-exacerbated respiratory disease have a history of NSAID reaction.63 This condition should be considered in all patients with chronic sinusitis, nasal polyps and asthma. The diagnosis of aspirin-exacerbated respiratory disease is confirmed with a single-blind, placebo-controlled challenge using oral aspirin, bronchial L-lysine–aspirin or nasal L-lysine–aspirin, although challenge tests are generally discouraged in patients with poor lung function (forced expiratory volume in 1 second < 70% predicted).64
Non-selective ß-blockers (eg, propranolol) should be avoided in asthma, although cardioselective ß-blockers (eg, bisoprolol, atenolol) may still be used in patients with cardiovascular indications. Non-selective ß-blockers have been shown to reduce lung function to a greater extent than cardioselective ß-blockers65 as well as increase the risk of exacerbations in high doses.66 Clinicians and patients should also be aware that topical administration of non-selective ß-blocker eye drops for glaucoma has similar detrimental effects on lung function.67
Work-related asthma comprises both occupational asthma and work-exacerbated asthma and is an important diagnosis to consider in all working asthma patients. In occupational asthma, there is a causal relationship between workplace factors and asthma, such as an allergen in the workplace; 10–25% of new onset asthma in adults68,69 may be attributable to occupational asthma. In work-exacerbated asthma, asthma onset precedes workplace exposure but is aggravated by work-related factors such as irritant exposure.70 Work-exacerbated asthma is present in 14% of patients with asthma.71,72 An extensive list of occupational asthma and work-exacerbated asthma workplace triggers has been published.71,73,74 Early identification of work triggers is important because persistent exposure to triggers leads to greater lung function decline.75 Evaluation of suspected work-related asthma involves: confirming a diagnosis of asthma; determining whether asthma symptoms are work-related; identifying workplace triggers; and differentiating occupational asthma from work-exacerbated asthma.76
Features suggesting work-related symptoms include an improvement in symptoms away from work and worsening of symptoms at work, although the diagnostic accuracy of work-related symptoms is poor.77,78 Objective tests include serial measurements of peak flow, serial measurements of non-specific bronchial hyper-responsiveness, detection of specific IgE to occupational allergens, and specific inhalational challenge.70
Comorbidities
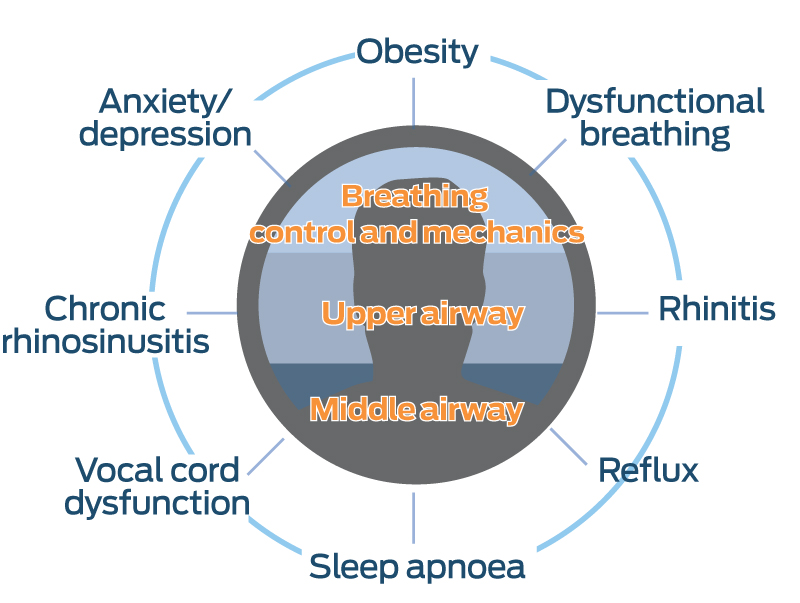
Extra-pulmonary comorbidities are common in asthma and even more frequent in difficult asthma.79,80 In a difficult asthma cohort in Melbourne, 80% of patients had two or more extra-pulmonary comorbidities.10 These comorbidities may be classified into those involving breathing control and lung mechanics, the upper airway, and the middle airway (Box 6). They include dysfunctional breathing, anxiety and depression, obesity, rhinitis, chronic rhinosinusitis, gastro-oesophageal reflux disease, obstructive sleep apnoea, and vocal cord dysfunction. The detection of these comorbidities is an essential part of difficult asthma assessment, because they may both mimic asthma and worsen asthma control. Some comorbidities even contribute to phenotypes of severe asthma, as with obesity or chronic rhinosinusitis with nasal polyps.81
Vocal cord dysfunction, dysfunctional breathing and exertional dyspnoea due to obesity may all be misdiagnosed as asthma. Patients with vocal cord dysfunction can present with asthma-like symptoms such as wheezing and dyspnoea. A delay in diagnosis results in unnecessary treatment with high dose corticosteroids.82,83 Vocal cord dysfunction often also coexists with severe asthma and may be present in up to 50% of these patients.84 Dysfunctional breathing is a breathing pattern disorder, the most commonly recognised pattern being hyperventilation. About 1–2% of patients seen in difficult asthma clinics had symptoms attributable to dysfunctional breathing without objective evidence of asthma.10,79 Dysfunctional breathing also coexists with asthma in 30–64% of patients with difficult asthma, resulting in increased symptoms and health care utilisation.85,86 Obesity is a risk factor for wheeze and dyspnoea, but not airflow obstruction or airway hyper-responsiveness.87,88 Obese individuals are more likely to be incorrectly diagnosed as having asthma when they present acutely with respiratory symptoms, compared with non-obese individuals.89 Nevertheless, obesity is highly prevalent in patients with severe asthma, affecting 30–39% of patients,47,80 and also contributes to asthma symptoms and exacerbations.90,91
All the comorbidities discussed above can increase asthma symptoms or exacerbations, leading to worse asthma control. Rhinitis,47,86 chronic rhinosinusitis,20,86 gastro-oesophageal reflux disease,80,92 obstructive sleep apnoea86 and anxiety and depression93 are present in > 30% of patients with severe asthma. Many studies have shown a beneficial impact of comorbidity treatment on asthma outcomes, although the majority of studies were observational in nature.80,81,94
Despite their clinical importance, comorbidities are commonly under-recognised in difficult asthma. Clinicians, including asthma specialists, are prone to overlook sinonasal disease, obstructive sleep apnoea, vocal cord dysfunction and dysfunctional breathing.95 Diagnosis of comorbidities in difficult asthma inevitably requires thorough systematic evaluation, which can be achieved through exhaustive assessment by various specialists, as is performed in certain centres.96 This method is resource intensive and not feasible in most health care settings. A more affordable approach is to screen for comorbidities using validated screening questionnaires (Box 7),97-102 followed by confirmatory clinical consultation and targeted multidisciplinary evaluation as needed.81 In difficult asthma, this bespoke approach has been shown to improve both comorbidity control and asthma outcomes.94
Screening and management of some comorbidities can be performed even in primary care. Rhinitis, chronic rhinosinusitis, gastro-oesophageal reflux disease and obesity are readily identified based on history and physical examination, and treatment can be comfortably initiated by most primary care physicians.
Step three: establish asthma phenotype
Clinical and inflammatory phenotypes
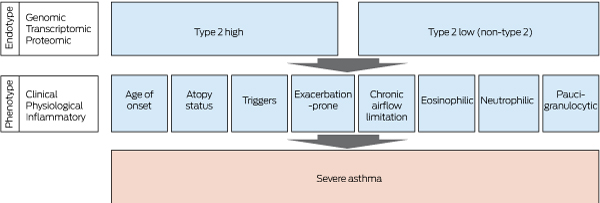
Severe asthma can be considered a syndrome, analogous to anaemia or arthritis, with contributions by various disease entities arising as a result of multiple pathophysiological mechanisms. The impetus in recent asthma research has been to differentiate patients according to their observable traits, in order to tailor therapy appropriately. The process of characterising observable traits is termed phenotyping.103
Asthma phenotypes have been described since the early 20th century. Rackeman first observed differences in the clinical characteristics of asthmatics in the 1920s and introduced the terms “extrinsic” and “intrinsic” asthma to differentiate patients with and without identifiable environmental triggers, respectively.104 An increasing understanding of airway inflammation in asthma led to the distinction between various inflammatory phenotypes. The importance of airway eosinophilia in asthma was noted by Brown in the 1950s.105 Other researchers subsequently demonstrated that severe asthma could be divided into eosinophilic and non-eosinophilic phenotypes, with distinct accompanying clinical and physiological characteristics.106,107 We now know that inflammation in asthma can be further divided into eosinophilic, neutrophilic, mixed and pauci-granulocytic based on sputum108 and blood profiles.109
Patients have traditionally been phenotyped based on characteristics such as age of asthma onset, atopy status, presence of chronic airflow limitation and eosinophilic inflammation103 (Box 8). However, phenotyping based on individual predefined characteristics is subjective and obscures less evident patterns. Cluster analysis is an unbiased statistical method used to identify homogeneous groups. Using cluster analysis, the following phenotypes have been repeatedly identified in various severe asthma cohorts: early onset atopic,110,111 late onset severe eosinophilic,110 obese non-eosinophilic,110,111 and chronic airflow limitation.112-114
The early onset atopic phenotype describes asthma starting in childhood.110 In the Severe Asthma Research Program cohort, daily symptoms and rescue bronchodilator use predominated over exacerbations.111 The late onset eosinophilic phenotype is of adult onset and found mainly in patients with severe asthma.110 These patients are older and have poorer lung function.110,114,115 Patients also commonly have severe sinusitis and nasal polyposis.114 Concomitant neutrophilic airway inflammation has been observed in some of these patients.113,115 Patients with the obese non-eosinophilic phenotype are usually female and less likely to be atopic.110,111 Despite minimal airway inflammation, they are highly symptomatic with frequent health care utilisation.110,112 Age of asthma onset is not a constant feature in this phenotype.110,112,114 The chronic airflow limitation phenotype fits the current definition of chronic obstructive pulmonary disease and is in itself heterogeneous. It has been associated with both eosinophilic and neutrophilic inflammation,112,113 as well as early and late onset asthma.116 This phenotype is likely influenced by various factors including childhood lung function trajectory, smoking and airway inflammation.117,118
Endotypes
Clinical phenotypes highlight the heterogeneity of severe asthma but do not necessarily reflect the underlying disease process. With greater understanding of asthma immunology and the advent of -omics biology (genomics, transcriptomics, proteomics), researchers are now starting to discover various asthma endotypes. Endotypes refer to disease subgroups with distinct underlying biological mechanisms. Deconstructing asthma into aetiological and pathophysiological mechanisms assists in identifying targets for treatment119 (Box 8).
The aetiologies and exact mechanisms underlying severe and non-severe asthma are still poorly understood, but can be simplistically divided into type 2 high and type 2 low (non-type 2) inflammatory processes.120 Type 2 high inflammation features the prominent secretion of cytokines that are typically produced by type 2 helper (Th2) lymphocyte cells (interleukin [IL]-4, IL-5 and IL-13). Type 2 high inflammation may drive both allergic and non-allergic eosinophilic airway responses.121 In allergic asthma, exposure to an allergen results in production of IL-4 and IL-13 by Th2 cells. These cytokines stimulate B cells to produce IgE that drives the allergic cascade. Th2 cells also produce IL-5, which increases the production, differentiation, maturation and activation of eosinophils. In non-allergic eosinophilic asthma, type 2 innate lymphoid cells appear responsible for the production of type 2 cytokines IL-5 and IL-13.120 Much less is known about type 2 low inflammation, which includes pauci-granulocytic and neutrophilic subtypes.122
Biomarkers
Sputum eosinophils, blood eosinophils, FENO and serum periostin are biomarkers available clinically to diagnose type 2 inflammation. These biomarkers are also used to predict responses to treatment. In the UK Refractory Asthma Stratification Programme, a composite of blood eosinophil, serum periostin and FENO will be used to optimise corticosteroids in severe asthma.123 Likewise, these biomarkers have been shown to predict treatment response to monoclonal antibodies. More recently, sputum gene signatures have been found to predict response to oral corticosteroids better than sputum and blood eosinophils.124 Newer diagnostic and predictive biomarkers will be needed to guide the selection of increasing numbers of biologicals.
Targeted therapies
Phenotyping allows clinicians to select patients who are most likely to respond to novel targeted therapies. Assessment of a patient's atopy status and peripheral blood eosinophil counts can aid in determining the most appropriate biological for targeted treatment. In the US for example, the anti-IgE monoclonal antibody omalizumab and the anti-eosinophilic biologicals mepolizumab, benralizumab and reslizumab are all approved by the Food and Drug Administration. In Australia, only omalizumab and mepolizumab are approved by the Therapeutic Goods Administration and funded under the Pharmaceutical Benefits Scheme. An in-depth discussion of biological therapy is provided by Upham and Chung in this supplement.125
Integrating diagnostic evaluation across primary and specialist care
Diagnosis and management of patients with severe asthma require coordinated efforts between primary care and specialist care (Box 9). This framework of care often involves bidirectional referrals between general practitioners and specialists to tap each level’s expertise.
In primary care, apart from taking a relevant history and examination, relatively accessible investigations such as chest radiography and electrocardiography can be performed in patients with persistent asthma symptoms to exclude asthma mimics. GPs with office spirometers or peak flow meters should also use these to look for evidence of variable airflow obstruction. Repeated evaluation of adherence, education and reinforcement of inhaler technique, management of asthma triggers (especially active smoking), treatment of comorbidities such as rhinitis, chronic rhinosinusitis and gastro-oesophageal reflux disease, as well as weight management advice for obese patients, can be instituted in primary care.79,126,127
In addition, patients with more complex comorbidities who have already been evaluated by specialists may also benefit from a primary care management plan and a multidisciplinary team care arrangement. This enables the patient to access government-subsidised allied health interventions. This is particularly important for patients who live in regional areas who may not have regular or convenient access to allied health professionals in tertiary centres. These include a referral to a dietitian for patients who are obese, psychology support for patients with mental health disorders, a speech therapist for patients diagnosed with vocal cord dysfunction, and a respiratory physiotherapist for patients diagnosed with dysfunctional breathing.
When patients continue to have uncontrolled asthma on Global Initiative for Asthma treatment step 4 (high dose ICS plus an additional controller) despite the above, or if there are doubts about asthma diagnosis or suspicion of occupational asthma, referral to a specialist should be considered.126 Specialist physicians are better equipped to manage patients with severe asthma, although subspecialised care may be required for a proportion of patients. Patients with suspected work-related asthma may need referral to an occupational medicine specialist. Comorbidities such as vocal cord dysfunction and dysfunctional breathing often require multidisciplinary input.79,127 Phenotyping using skin prick testing, serum-specific IgE, blood eosinophils and FENO are available in most specialist clinics but more advanced phenotyping methods (eg, sputum inflammometry) are only performed in a few research centres.
Conclusion
The diagnostic evaluation for severe asthma outlined in this article should be undertaken for patients presenting with difficult asthma. The exploration of asthma diagnosis and contributory factors can be readily initiated in community primary care, and completed in specialist secondary care. Further detailed endotyping of severe asthma, and initiation of phenotype-targeted treatment, may only be possible in specialised centres. Importantly, many gaps remain at each step of the evaluation process for severe asthma, and the development of new systems of care may be needed to fully address these shortcomings.
Box 1 – Definition of difficult asthma and its relationship to severe asthma
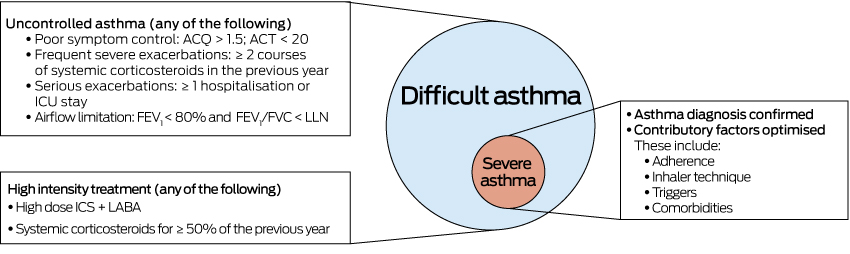
ACQ = Asthma Control Questionnaire; ACT = Asthma Control Test; FEV1 = forced expiratory volume in 1 second; FVC = forced vital capacity; ICU = intensive care unit; ICS = inhaled corticosteroids; LABA = long-acting ß-agonists; LLN = lower limit of normal.
Box 3 – Glossary
|
|
|||||||||||||||
|
Asthma biomarker |
A biological characteristic that is objectively measured and evaluated as an indicator of normal biological or pathological processes, or a response to a therapeutic intervention. Biomarkers in asthma include fractional exhaled nitric oxide, peripheral blood eosinophils and sputum eosinophils. |
||||||||||||||
|
Asthma comorbidity |
A disease that coexists with asthma, such as rhinitis or chronic rhinosinusitis. |
||||||||||||||
|
Asthma endotype |
Distinct functional or pathophysiological mechanism driving the disease process. For example, patients with aspirin-exacerbated respiratory disease have dysregulated arachidonic acid metabolism which leads to overproduction of inflammatory leukotrienes. |
||||||||||||||
|
Asthma phenotype |
Observable characteristics of a patient, such as age of asthma onset, atopy status, persistence of airflow limitation on spirometry and inflammatory cell type. |
||||||||||||||
|
Treatable trait |
A trait that can be treated based on phenotype or endotype. These traits include airflow limitation, eosinophilic airway inflammation and airway bacterial colonisation. |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 4 – Mimics of asthma and clinical clues for diagnosis
|
Conditions that can mimic asthma |
Clinical clues |
||||||||||||||
|
|
|||||||||||||||
|
Non-pulmonary |
|
||||||||||||||
|
Cardiac failure |
Pre-existing cardiac disease, orthopnoea, paroxysmal nocturnal dyspnoea, peripheral oedema |
||||||||||||||
|
Congenital heart disease |
Cardiac murmurs |
||||||||||||||
|
Dysfunctional breathing |
Dizziness, light-headedness, peripheral tingling |
||||||||||||||
|
Vocal cord dysfunction |
Stridor, throat tightness, voice change, lack of wheezing in the chest, symptoms triggered by strong odours |
||||||||||||||
|
Adverse drug reaction: eg, angiotensin-converting enzyme inhibitor |
Prominent dry cough |
||||||||||||||
|
Pulmonary |
|
||||||||||||||
|
Chronic obstructive pulmonary disease |
History of heavy smoking or other relevant exposures |
||||||||||||||
|
Bronchiectasis |
Coarse crepitations, digital clubbing |
||||||||||||||
|
Endobronchial lesions: eg, tumour, foreign body |
Systemic symptoms: eg, weight loss, haemoptysis, choking episode, focal wheeze |
||||||||||||||
|
Acquired tracheobronchomalacia |
History of trauma: eg, intubation, history of intrathoracic tumours |
||||||||||||||
|
Bronchiolitis obliterans |
Relevant history: eg, connective tissue disease, toxin exposure, post-infectious, post-transplant |
||||||||||||||
|
Eosinophilic granulomatosis with polyangiitis |
Markedly raised peripheral blood eosinophils, sinusitis, neuropathy |
||||||||||||||
|
Allergic bronchopulmonary aspergillosis |
Markedly raised peripheral blood eosinophils and total serum IgE |
||||||||||||||
|
Hypereosinophilic syndrome |
Markedly raised peripheral blood eosinophils |
||||||||||||||
|
Non-asthmatic eosinophilic bronchitis |
Airway eosinophilia with no evidence of variable airflow obstruction |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 5 – Potential asthma triggers
AllergensIndoor:- House dust mite
- Moulds: eg, Aspergillus
- Animal dander: eg, cat, dog
- Cockroaches
- Pollen
- Moulds: eg, Alternaria, Cladosporium
- High molecular weight: eg, enzymes, flour, animal proteins, latex
- Low molecular weight: eg, diisocyanates, acid anhydrides, wood dust, disinfection agents
- Active smoking
- Second-hand smoke
- Environmental pollution
- Cleaning products
- Strong odours: eg, perfumes
- Non-steroidal anti-inflammatory drugs
- ß-blockers
- Angiotensin-converting enzyme inhibitors
- Cold air
- Weather changes
- Humidity
- Thunderstorms: eg, thunderstorm asthma
- Exercise
- Strong emotions
- Food and food additives: eg, sulfites
Box 7 – Available questionnaires for comorbidity screening
|
Comorbidity |
Questionnaire |
||||||||||||||
|
|
|||||||||||||||
|
Sinonasal disease (includes rhinosinusitis and allergic rhinitis) |
Sinonasal questionnaire96 |
||||||||||||||
|
Gastroesophageal reflux |
Gastro-oesophageal reflux disease questionnaire97 |
||||||||||||||
|
Obstructive sleep apnoea |
Berlin Questionnaire98 |
||||||||||||||
|
Vocal cord dysfunction |
Pittsburgh Vocal Cord Dysfunction Index99 |
||||||||||||||
|
Dysfunctional breathing |
Nijmegen Questionnaire100 |
||||||||||||||
|
Anxiety and depression |
Hospital Anxiety and Depression Scale101 |
||||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Box 9 – Severe asthma diagnostic evaluation at primary care and specialist care
|
|
Primary care management |
Specialist management |
|||||||||||||
|
|
|||||||||||||||
|
Confirm asthma diagnosis |
Chest x-ray |
Spirometry (pre/post bronchodilator) |
|||||||||||||
|
Identify and treat contributory factors |
|
|
|||||||||||||
|
Non-adherence |
Assess based on patient report |
Electronic dose monitors |
|||||||||||||
|
Poor inhaler technique |
Education and reassessment |
Education and reassessment |
|||||||||||||
|
Triggers |
Smoking cessation |
Work-related asthma assessment |
|||||||||||||
|
Comorbidities |
Initiate treatment for rhinitis, chronic rhinosinusitis, gastro-oesophageal reflux disease, obesity |
Referral to other departments |
|||||||||||||
|
Assess phenotype/endotype |
Blood eosinophil |
Skin prick test |
|||||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Provenance: Commissioned; externally peer reviewed.
- Tunn Ren Tay1
- Joy W-Y Lee2,3
- Mark Hew2
- 1 Changi General Hospital, Singapore, Singapore
- 2 The Alfred Hospital, Melbourne, VIC
- 3 Monash University, Melbourne, VIC
Joy Lee has delivered educational talks for GlaxoSmithKline and AstraZeneca. Mark Hew has undertaken contracted research for AstraZeneca, Sanofi, Novartis and GlaxoSmithKline; delivered educational talks for GlaxoSmithKline, AstraZeneca and Novartis; and participated on advisory boards/consultancies for AstraZeneca, GlaxoSmithKline and Seqirus; his employer (Alfred Health) has been reimbursed for all of these.
- 1. Israel E, Reddel HK. Severe and difficult-to-treat asthma in adults. N Engl J Med 2017; 377: 965-976.
- 2. Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 2014; 43: 343-373.
- 3. Hekking PP, Wener RR, Amelink M, et al. The prevalence of severe refractory asthma. J Allergy Clin Immunol 2015; 135: 896-902.
- 4. Wark PA, Hew M, Maltby S, et al. Diagnosis and investigation in the severe asthma clinic. Expert Rev Respir Med 2016; 10: 491-503.
- 5. Tomita K, Sano H, Chiba Y, et al. A scoring algorithm for predicting the presence of adult asthma: a prospective derivation study. Prim Care Respir J 2013; 22: 51-58.
- 6. Global Initiative for Asthma. Global strategy for asthma management and prevention (2018 update). http://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/ (viewed May 2018).
- 7. British Thoracic Society, Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma: a national clinical guideline. https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign-asthma-guideline-2016/ (viewed May 2018).
- 8. Aaron SD, Vandemheen KL, FitzGerald JM, et al. Reevaluation of diagnosis in adults with physician-diagnosed asthma. JAMA 2017; 317: 269-279.
- 9. Marklund B, Tunsater A, Bengtsson C. How often is the diagnosis bronchial asthma correct? Fam Pract 1999; 16: 112-116.
- 10. Radhakrishna N, Tay TR, Hore-Lacy F, et al. Profile of difficult to treat asthma patients referred for systematic assessment. Respir Med 2016; 117: 166-173.
- 11. Robinson DS, Campbell DA, Durham SR, et al. Systematic assessment of difficult-to-treat asthma. Eur Respir J 2003; 22: 478-483.
- 12. Fingleton J, Weatherall M, Beasley R. Bronchodilator responsiveness: interpret with caution. Thorax 2012; 67: 667-668.
- 13. Hunter CJ, Brightling CE, Woltmann G, et al. A comparison of the validity of different diagnostic tests in adults with asthma. Chest 2002; 121: 1051-1057.
- 14. Tan WC, Vollmer WM, Lamprecht B, et al. Worldwide patterns of bronchodilator responsiveness: results from the Burden of Obstructive Lung Disease study. Thorax 2012; 67: 718-726.
- 15. Jenkins C, Seccombe L, Tomlins R. Investigating asthma symptoms in primary care. BMJ 2012; 344: e2734.
- 16. Cockcroft DW. Direct challenge tests: Airway hyperresponsiveness in asthma: its measurement and clinical significance. Chest 2010; 138: 18S-24S.
- 17. Galera R, Casitas R, Martinez-Ceron E, et al. Does airway hyperresponsiveness monitoring lead to improved asthma control? Clin Exp Allergy 2015; 45: 1396-1405.
- 18. Pavord ID, Beasley R, Agusti A, et al. After asthma: redefining airways diseases. Lancet 2017; 391: 350-400.
- 19. Tan WC, Sin DD, Bourbeau J, et al. Characteristics of COPD in never-smokers and ever-smokers in the general population: results from the CanCOLD study. Thorax 2015; 70: 822-829.
- 20. Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med 2010; 181: 315-323.
- 21. Foster JM, Usherwood T, Smith L, et al. Inhaler reminders improve adherence with controller treatment in primary care patients with asthma. J Allergy Clin Immunol 2014; 134: 1260-1268.e3.
- 22. Williams LK, Peterson EL, Wells K, et al. Quantifying the proportion of severe asthma exacerbations attributable to inhaled corticosteroid nonadherence. J Allergy Clin Immunol 2011; 128: 1185-1191.e2.
- 23. Lee J, Tay TR, Radhakrishna N, et al. Nonadherence in the era of severe asthma biologics and thermoplasty. Eur Respir J 2018; 51: 1701836.
- 24. Krishnan JA, Riekert KA, McCoy JV, et al. Corticosteroid use after hospital discharge among high-risk adults with asthma. Am J Respir Crit Care Med 2004; 170: 1281-1285.
- 25. Suissa S, Ernst P, Benayoun S, et al. Low-dose inhaled corticosteroids and the prevention of death from asthma. N Engl J Med 2000; 343: 332-336.
- 26. Engelkes M, Janssens HM, de Jongste JC, et al. Medication adherence and the risk of severe asthma exacerbations: a systematic review. Eur Respir J 2015; 45: 396-407.
- 27. Murphy AC, Proeschal A, Brightling CE, et al. The relationship between clinical outcomes and medication adherence in difficult-to-control asthma. Thorax 2012; 67: 751-753.
- 28. Sumino K, Cabana MD. Medication adherence in asthma patients. Curr Opin Pulm Med 2013; 19: 49-53.
- 29. Foster JM, Smith L, Bosnic-Anticevich SZ, et al. Identifying patient-specific beliefs and behaviours for conversations about adherence in asthma. Intern Med J 2012; 42: e136-144.
- 30. Patel M, Perrin K, Pritchard A, et al. Accuracy of patient self-report as a measure of inhaled asthma medication use. Respirology 2013; 18: 546-552.
- 31. Gamble J, Stevenson M, McClean E, Heaney LG. The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med 2009; 180: 817-822.
- 32. Foster JM, Smith L, Usherwood T, et al. The reliability and patient acceptability of the SmartTrack device: a new electronic monitor and reminder device for metered dose inhalers. J Asthma 2012; 49: 657-662.
- 33. McNicholl DM, Stevenson M, McGarvey LP, Heaney LG. The utility of fractional exhaled nitric oxide suppression in the identification of nonadherence in difficult asthma. Am J Respir Crit Care Med 2012; 186: 1102-1108.
- 34. Marceau C, Lemiere C, Berbiche D, et al. Persistence, adherence, and effectiveness of combination therapy among adult patients with asthma. J Allergy Clin Immunol 2006; 118: 574-581.
- 35. Stoloff SW, Stempel DA, Meyer J, et al. Improved refill persistence with fluticasone propionate and salmeterol in a single inhaler compared with other controller therapies. J Allergy Clin Immunol 2004; 113: 245-251.
- 36. Guest JF, Davie AM, Ruiz FJ, Greener MJ. Switching asthma patients to a once-daily inhaled steroid improves compliance and reduces healthcare costs. Prim Care Respir J 2005; 14: 88-98.
- 37. Price D, Robertson A, Bullen K, et al. Improved adherence with once-daily versus twice-daily dosing of mometasone furoate administered via a dry powder inhaler: a randomized open-label study. BMC Pulm Med 2010; 10: 1.
- 38. Brooks TL, Leventhal H, Wolf MS, et al. Strategies used by older adults with asthma for adherence to inhaled corticosteroids. J Gen Intern Med 2014; 29: 1506-1512.
- 39. Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med 2010; 181: 566-577.
- 40. Janson SL, McGrath KW, Covington JK, et al. Individualized asthma self-management improves medication adherence and markers of asthma control. J Allergy Clin Immunol 2009; 123: 840-846.
- 41. Sanchis J, Gich I, Pedersen S, Aerosol Drug Management Improvement Team. Systematic review of errors in inhaler use: has patient technique improved over time? Chest 2016; 150: 394-406.
- 42. Dekhuijzen PN, Vincken W, Virchow JC, et al. Prescription of inhalers in asthma and COPD: towards a rational, rapid and effective approach. Respir Med 2013; 107: 1817-1821.
- 43. Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK. Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma 2010; 47: 251-256.
- 44. Chrystyn H, Price DB, Molimard M, et al. Comparison of serious inhaler technique errors made by device-naive patients using three different dry powder inhalers: a randomised, crossover, open-label study. BMC Pulm Med 2016; 16: 12.
- 45. Basheti IA, Reddel HK, Armour CL, Bosnic-Anticevich SZ. Improved asthma outcomes with a simple inhaler technique intervention by community pharmacists. J Allergy Clin Immunol 2007; 119: 1537-1538.
- 46. Price D, Dale P, Elder E, Chapman KR. Types, frequency and impact of asthma triggers on patients’ lives: a quantitative study in five European countries. J Asthma 2014; 51: 127-135.
- 47. Shaw DE, Sousa AR, Fowler SJ, et al. Clinical and inflammatory characteristics of the European U-BIOPRED adult severe asthma cohort. Eur Respir J 2015; 46: 1308-1321.
- 48. Humbert M, Boulet LP, Niven RM, et al. Omalizumab therapy: patients who achieve greatest benefit for their asthma experience greatest benefit for rhinitis. Allergy 2009; 64: 81-84.
- 49. Grootendorst DC, Dahlen SE, Van Den Bos JW, et al. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy 2001; 31: 400-408.
- 50. Custovic A, Wijk RG. The effectiveness of measures to change the indoor environment in the treatment of allergic rhinitis and asthma: ARIA update (in collaboration with GA(2)LEN). Allergy 2005; 60: 1112-1115.
- 51. Siroux V, Pin I, Oryszczyn MP, et al. Relationships of active smoking to asthma and asthma severity in the EGEA study. Epidemiological study on the Genetics and Environment of Asthma. Eur Respir J 2000; 15: 470-7.
- 52. Silverman RA, Boudreaux ED, Woodruff PG, et al. Cigarette smoking among asthmatic adults presenting to 64 emergency departments. Chest 2003; 123: 1472-1479.
- 53. Eisner MD, Klein J, Hammond SK, et al. Directly measured second hand smoke exposure and asthma health outcomes. Thorax 2005; 60: 814-821.
- 54. Orellano P, Quaranta N, Reynoso J, et al. Effect of outdoor air pollution on asthma exacerbations in children and adults: Systematic review and multilevel meta-analysis. PLoS One 2017; 12: e0174050.
- 55. Comhair SA, Gaston BM, Ricci KS, et al. Detrimental effects of environmental tobacco smoke in relation to asthma severity. PLoS One 2011; 6: e18574.
- 56. Stanbury M, Chester D, Hanna EA, Rosenman KD. How many deaths will it take? A death from asthma associated with work-related environmental tobacco smoke. Am J Ind Med 2008; 51: 111-116.
- 57. Kupczyk M, Kuprys I, Gorski P, Kuna P. Aspirin intolerance and allergy to house dust mites: important factors associated with development of severe asthma. Ann Allergy Asthma Immunol 2004; 92: 453-458.
- 58. Mascia K, Haselkorn T, Deniz YM, et al. Aspirin sensitivity and severity of asthma: evidence for irreversible airway obstruction in patients with severe or difficult-to-treat asthma. J Allergy Clin Immunol 2005; 116: 970-975.
- 59. Szczeklik A, Nizankowska E, Duplaga M. Natural history of aspirin-induced asthma. AIANE Investigators. European Network on Aspirin-Induced Asthma. Eur Respir J 2000; 16: 432-436.
- 60. Szczeklik A, Stevenson DD. Aspirin-induced asthma: advances in pathogenesis, diagnosis, and management. J Allergy Clin Immunol 2003; 111: 913-921; quiz 22.
- 61. Tan JHY, Hsu AAL. Nonsteroidal anti-inflammatory drug (NSAID) exacerbated respiratory disease phenotype: topical NSAID and asthma control – a possible oversight link. Respir Med 2016; 118: 1-3.
- 62. Sitenga GL, Ing EB, Van Dellen RG, et al. Asthma caused by topical application of ketorolac. Ophthalmology 1996; 103: 890-892.
- 63. Dursun AB, Woessner KA, Simon RA, et al. Predicting outcomes of oral aspirin challenges in patients with asthma, nasal polyps, and chronic sinusitis. Ann Allergy Asthma Immunol 2008; 100: 420-425.
- 64. Nizankowska-Mogilnicka E, Bochenek G, Mastalerz L, et al. EAACI/GA2LEN guideline: aspirin provocation tests for diagnosis of aspirin hypersensitivity. Allergy 2007; 62: 1111-1118.
- 65. Morales DR, Jackson C, Lipworth BJ, et al. Adverse respiratory effect of acute beta-blocker exposure in asthma: a systematic review and meta-analysis of randomized controlled trials. Chest 2014; 145: 779-786.
- 66. Morales DR, Lipworth BJ, Donnan PT, et al. Respiratory effect of beta-blockers in people with asthma and cardiovascular disease: population-based nested case control study. BMC Med 2017; 15: 18.
- 67. Morales DR, Dreischulte T, Lipworth BJ, et al. Respiratory effect of beta-blocker eye drops in asthma: population-based study and meta-analysis of clinical trials. Br J Clin Pharmacol 2016; 82: 814-822.
- 68. Balmes J, Becklake M, Blanc P, et al. American Thoracic Society Statement: Occupational contribution to the burden of airway disease. Am J Respir Crit Care Med 2003; 167: 787-797.
- 69. Kogevinas M, Zock JP, Jarvis D, et al. Exposure to substances in the workplace and new-onset asthma: an international prospective population-based study (ECRHS-II). Lancet 2007; 370: 336-341.
- 70. Moscato G, Pala G, Barnig C, et al. EAACI consensus statement for investigation of work-related asthma in non-specialized centres. Allergy 2012; 67: 491-501.
- 71. Henneberger PK, Redlich CA, Callahan DB, et al. An official American Thoracic Society statement: work-exacerbated asthma. Am J Respir Crit Care Med 2011; 184: 368-378.
- 72. Lemiere C, Begin D, Camus M, et al. Occupational risk factors associated with work-exacerbated asthma in Quebec. Occup Environ Med 2012; 69: 901-907.
- 73. Baur X, Bakehe P. Allergens causing occupational asthma: an evidence-based evaluation of the literature. Int Arch Occup Environ Health 2014; 87: 339-363.
- 74. Crewe J, Carey R, Glass D, et al. A comprehensive list of asthmagens to inform health interventions in the Australian workplace. Aust N Z J Public Health 2016; 40: 170-173.
- 75. Di Giampaolo L, Cavallucci E, Braga M, et al. The persistence of allergen exposure favors pulmonary function decline in workers with allergic occupational asthma. Int Arch Occup Environ Health 2012; 85: 181-188.
- 76. Friedman-Jimenez G, Harrison D, Luo H. Occupational asthma and work-exacerbated asthma. Semin Respir Crit Care Med 2015; 36: 388-407.
- 77. Bolen AR, Henneberger PK, Liang X, et al. The validation of work-related self-reported asthma exacerbation. Occup Environ Med 2007; 64: 343-348.
- 78. Vandenplas O, Ghezzo H, Munoz X, et al. What are the questionnaire items most useful in identifying subjects with occupational asthma? Eur Respir J 2005; 26: 1056.
- 79. Bardin PG, Rangaswamy J, Yo SW. Managing comorbid conditions in severe asthma. Med J Aust 2018; 209 (2 Suppl): S11-S17.
- 80. van der Meer AN, Pasma H, Kempenaar-Okkema W, et al. A 1-day visit in a severe asthma centre: effect on asthma control, quality of life and healthcare use. Eur Respir J 2016; 48: 726-733.
- 81. Tay TR, Hew M. Comorbid “treatable traits” in difficult asthma: Current evidence and clinical evaluation. Allergy 2017; doi:10.1111/all.13370 [Epub ahead of print].
- 82. Christopher KL, Wood RP 2nd, Eckert RC, et al. Vocal-cord dysfunction presenting as asthma. N Engl J Med 1983; 308: 1566-1570.
- 83. Morris MJ, Christopher KL. Diagnostic criteria for the classification of vocal cord dysfunction. Chest 2010; 138: 1213-1223.
- 84. Low K, Lau KK, Holmes P, et al. Abnormal vocal cord function in difficult-to-treat asthma. Am J Respir Crit Care Med 2011; 184: 50-56.
- 85. Stanton AE, Vaughn P, Carter R, Bucknall CE. An observational investigation of dysfunctional breathing and breathing control therapy in a problem asthma clinic. J Asthma 2008; 45: 758-765.
- 86. Tay TR, Radhakrishna N, Hore-Lacy F, et al. Comorbidities in difficult asthma are independent risk factors for frequent exacerbations, poor control and diminished quality of life. Respirology 2016; 21: 1384-1390.
- 87. Schachter L, Salome C, Peat J, Woolcock A. Obesity is a risk for asthma and wheeze but not airway hyperresponsiveness. Thorax 2001; 56: 4-8.
- 88. Sin DD, Jones RL, Man S. Obesity is a risk factor for dyspnea but not for airflow obstruction. Arch Intern Med 2002; 162: 1477-1481.
- 89. Pakhale S, Doucette S, Vandemheen K, et al. A comparison of obese and nonobese people with asthma: exploring an asthma-obesity interaction. Chest 2010; 137: 1316-1323.
- 90. Farah CS, Kermode JA, Downie SR, et al. Obesity is a determinant of asthma control independent of inflammation and lung mechanics. Chest 2011; 140: 659-666.
- 91. Lessard A, Turcotte H, Cormier Y, Boulet LP. Obesity and asthma: a specific phenotype? Chest 2008; 134: 317-323.
- 92. Moore WC, Bleecker ER, Curran-Everett D, et al. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute’s Severe Asthma Research Program. J Allergy Clin Immunol 2007; 119: 405-413.
- 93. de Carvalho-Pinto RM, Cukier A, Angelini L, et al. Clinical characteristics and possible phenotypes of an adult severe asthma population. Respir Med 2012; 106: 47-56.
- 94. Tay TR, Lee J, Radhakrishna N, et al. A structured approach to specialist-referred difficult asthma patients improves control of comorbidities and enhances asthma outcomes. J Allergy Clin Immunol Pract 2017; 5: 956-964.e3.
- 95. Radhakrishna N, Tay TR, Hore-Lacy F, et al. Validated questionnaires heighten detection of difficult asthma comorbidities. J Asthma 2017; 54: 294-299.
- 96. Robinson DS, Campbell DA, Durham SR, et al. Systematic assessment of difficult-to-treat asthma. Eur Respir J 2003; 22: 478-483.
- 97. Dixon AE, Sugar EA, Zinreich SJ, et al. Criteria to screen for chronic sinonasal disease. Chest 2009; 136: 1324-1332.
- 98. Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 2009; 30: 1030-1038.
- 99. Netzer NC, Stoohs RA, Netzer CM, et al. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999; 131: 485-491.
- 100. Traister RS, Fajt ML, Landsittel D, Petrov AA. A novel scoring system to distinguish vocal cord dysfunction from asthma. J Allergy Clin Immunol Pract 2014; 2: 65-69.
- 101. van Dixhoorn J, Duivenvoorden HJ. Efficacy of Nijmegen Questionnaire in recognition of the hyperventilation syndrome. J Psychosom Res 1985; 29: 199-206.
- 102. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002; 52: 69-77.
- 103. Wenzel SE. Asthma: defining of the persistent adult phenotypes. Lancet 2006; 368: 804-813.
- 104. Rackemann FM. Intrinsic asthma. J Allergy 1940; 11: 147-162.
- 105. Brown HM. Treatment of chronic asthma with prednisolone; significance of eosinophils in the sputum. Lancet 1958; 2: 1245-1247.
- 106. Wenzel SE, Schwartz LB, Langmack EL, et al. Evidence that severe asthma can be divided pathologically into two inflammatory subtypes with distinct physiologic and clinical characteristics. Am J Respir Crit Care Med 1999; 160: 1001-1008.
- 107. Turner MO, Hussack P, Sears MR, et al. Exacerbations of asthma without sputum eosinophilia. Thorax 1995; 50: 1057-1061.
- 108. Simpson JL, Scott R, Boyle MJ, Gibson PG. Inflammatory subtypes in asthma: assessment and identification using induced sputum. Respirology 2006; 11: 54-61.
- 109. Nadif R, Siroux V, Oryszczyn MP, et al. Heterogeneity of asthma according to blood inflammatory patterns. Thorax 2009; 64: 374-380.
- 110. Haldar P, Pavord ID, Shaw DE, et al. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med 2008; 178: 218-224.
- 111. Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med 2010; 181: 315-323.
- 112. Amelink M, de Nijs SB, de Groot JC, et al. Three phenotypes of adult-onset asthma. Allergy 2013; 68: 674-680.
- 113. Moore WC, Hastie AT, Li X, et al. Sputum neutrophil counts are associated with more severe asthma phenotypes using cluster analysis. J Allergy Clin Immunol 2014; 133: 1557-1563 e5.
- 114. Wu W, Bleecker E, Moore W, et al. Unsupervised phenotyping of Severe Asthma Research Program participants using expanded lung data. J Allergy Clin Immunol 2014; 133: 1280-1288.
- 115. Loza MJ, Djukanovic R, Chung KF, et al. Validated and longitudinally stable asthma phenotypes based on cluster analysis of the ADEPT study. Respir Res 2016; 17: 165.
- 116. Tay T, Choo X, Ihsan R, et al. Characteristics of non-smoking adult asthma patients with chronic airflow limitation. J Asthma 2017; 54: 1026-1032.
- 117. McGeachie MJ, Yates KP, Zhou X, et al. Patterns of growth and decline in lung function in persistent childhood asthma. N Engl J Med 2016; 374: 1842-1852.
- 118. Perret JL, Dharmage SC, Matheson MC, et al. The interplay between the effects of lifetime asthma, smoking, and atopy on fixed airflow obstruction in middle age. Am J Respir Crit Care Med 2013; 187: 42-48.
- 119. Lotvall J, Akdis CA, Bacharier LB, et al. Asthma endotypes: a new approach to classification of disease entities within the asthma syndrome. J Allergy Clin Immunol 2011; 127: 355-360.
- 120. Robinson D, Humbert M, Buhl R, et al. Revisiting Type 2-high and Type 2-low airway inflammation in asthma: current knowledge and therapeutic implications. Clin Exp Allergy 2017; 47: 161-175.
- 121. Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol 2015; 16: 45-56.
- 122. Chung KF. Neutrophilic asthma: a distinct target for treatment? Lancet Respir Med 2016; 4: 765-767.
- 123. Heaney LG, Djukanovic R, Woodcock A, et al. Research in progress: Medical Research Council United Kingdom Refractory Asthma Stratification Programme (RASP-UK). Thorax 2016; 71: 187-189.
- 124. Berthon BS, Gibson PG, Wood LG, et al. A sputum gene expression signature predicts oral corticosteroid response in asthma. Eur Respir J 2017; 49: 1700180.
- 125. Upham JW, Chung LP. Optimising treatment for severe asthma. Med J Aust 2018; 209 (2 Suppl): S22-S27.
- 126. Tay TR, Abramson MJ, Hew M. Closing the million patient gap of uncontrolled asthma. Med J Aust 2016; 204: 216-217. <MJA full text>
- 127. Chung LP, Johnson P, Summers Q. Models of care for severe asthma: the role of primary care. Med J Aust 2018; 209 (2 Suppl): S34-S40.





Summary