The known Australian Aboriginal and Torres Strait Islander (Indigenous Australian) children have a higher risk of contracting vaccine-preventable diseases than other Australian children. While vaccination coverage rates for Indigenous children are improving, timely vaccination remains a problem.
The new The Aboriginal Immunisation Healthcare Worker Program, funded by NSW Health since 2012, has contributed to improving the timely vaccination of Indigenous children in NSW. In 2016, there was no statistically significant difference in coverage between Indigenous and non-Indigenous children at three age milestones (9, 15, and 51 months) in NSW.
The implications Dedicated programs can improve coverage and timeliness of vaccination of Indigenous Australian children.
Aboriginal and Torres Strait Islander children experience higher rates of vaccination-preventable diseases than non-Indigenous children in Australia.1 Disparities in vaccination coverage, particularly the timeliness of vaccination of Indigenous children, have been a persistent concern.2-4 Reducing the differences in health quality between Indigenous and non-Indigenous Australians has been a national priority since the Close the Gap initiative was adopted by the Council of Australian Governments in 2008.5
New South Wales is the most populous state in Australia and also has the largest resident Indigenous population.6 The Aboriginal Immunisation Healthcare Worker (AIHCW) Program, funded by NSW Health ($1.3 million per year), has had up to 13 full-time-equivalent AIHCW positions in public health units across NSW since 2012. These positions were established to reduce the disparities in vaccination coverage and timeliness between Indigenous and non-Indigenous children. AIHCWs do not require formal qualifications, their role being to work with their communities and with individuals to promote the better use of existing vaccination services, rather than to directly provide vaccination services. Key activities of AIHCWs, most of whom are Indigenous Australians, include contacting parents of Indigenous children before scheduled vaccinations (pre-call notices), following up Indigenous children recorded on the Australian Immunisation Register as not being up to date with vaccinations, improving Indigenous identification, equipping providers with tools for monitoring timely vaccination of Indigenous children, and promoting vaccination in their Indigenous communities. Two evaluations7,8 have found strong support for the AIHCW Program among public health unit staff and external stakeholders.
Key performance indicators for the AIHCW Program focus on improving coverage and vaccination timeliness for Indigenous children in NSW, and reducing the differences in these indicators between Indigenous and non-Indigenous children. The aims of our study were to assess vaccination coverage and timeliness among Indigenous and non-Indigenous children in NSW and to compare these parameters with the rest of Australia, with a particular focus on changes in differences between Indigenous and non-Indigenous children after the introduction of the AIHCW Program in NSW.
Methods
Annual vaccination coverage estimates between 2008 and 2016 were calculated for Indigenous and non-Indigenous children in NSW and the rest of Australia from Australian Immunisation Register data (status: 30 September 2017). The Australian Immunisation Register, a national whole-of-life vaccination register, is a nearly complete population register; all persons registered with Medicare have a record with the register.9 As the completeness of Indigenous identification in the register increased substantially after 2005,10 the 1% of children whose Indigenous status was not specified were deemed to be non-Indigenous for the purposes of our analysis.
The cohort method employed since the inception of the national register was used to calculate vaccination coverage. To allow for late notification of vaccinations, a 3-month lag period was applied;11 that is, cohort vaccination status was assessed at 9 months of age (for vaccines due at 6 months), 15 months of age (for vaccines due at 12 months), and at 51 months of age (for vaccines due at 48 months). These assessment milestones correspond to those of the NSW AIHCW Program key performance indicators, but are earlier than those usually employed for vaccination coverage reporting in Australia (12, 24, 60 months),12 placing greater emphasis on the timeliness of vaccination in coverage estimates. The proportions of children classified as fully vaccinated were calculated by dividing the number completely vaccinated at each of the three assessment milestone ages (Box 1) by the total number of Australian Immunisation Register-registered children in their age group. If a child’s record indicated that they had received the final dose of a vaccine that requires more than one dose, it was assumed that earlier doses had also been received, an assumption that has been shown to be valid.13,14
Estimates of full vaccination coverage at 9, 15 and 51 months of age (with 95% confidence intervals, CIs) were calculated for each year between 2008 and 2016 for Indigenous and non-Indigenous children in NSW and in the rest of Australia. Coverage for Indigenous and non-Indigenous children in NSW and the rest of Australia at each of the three assessment milestones during the two periods, 2008–2011 (pre-AIHCW Program) and 2012–2016 (AIHCW Program), were compared. Differences (with 95% CIs) between the proportions of Indigenous and non-Indigenous children classified as fully vaccinated at each of the three milestones in NSW and in the rest of Australia were calculated for each year between 2008 and 2016. The mean annual difference between coverage estimates for Indigenous and non-Indigenous children during the pre-AIHCW Program (2008–2011) and AIHCW Program (2012–2016) periods were calculated.
All analyses were performed in SAS 9.4 (SAS Institute) and Excel 2010 (Microsoft). Non-overlapping 95% CIs were deemed to indicate a statistically significant difference.
Ethics approval
Ethics approval for this study was obtained from the NSW Aboriginal Health and Medical Research Council (reference, 1191/16).
Results
The proportions of Indigenous and non-Indigenous children in NSW classified as fully vaccinated at 9 and 15 months were relatively stable during the pre-AIHCW period (2008–2011) and rose significantly during the initial years of the AIHCW Program (2012–2016). For Indigenous children aged 9 months, coverage rose from 78.9% (95% CI, 76.1–81.8%) in 2008 to 89.5% (95% CI, 87.0–92.0%) in 2016, and for non-Indigenous children from 85.6% (95% CI, 85.0–86.1%) to 91.1% (95% CI, 90.5–91.7%) (Box 2). For Indigenous children aged 15 months, coverage rose from 78.8% (95% CI, 75.9–81.7%) in 2008 to 88.4% (95% CI, 85.9–90.9%), and for non-Indigenous children from 82.5% (95% CI, 81.9–83.0%) to 88.7% (95% CI, 88.1–89.3%) (Box 3). The pattern for full vaccination coverage of Indigenous and non-Indigenous children at 15 months of age in the rest of Australia was similar to that in NSW (Box 3), but the proportion of Indigenous children in the rest of Australia classified as fully vaccinated at 9 months of age also increased markedly during 2008–2011 (Box 2). The proportion of Indigenous and non-Indigenous children in NSW and the rest of Australia classified as fully vaccinated at 51 months of age increased significantly during both the 2008–2011 and 2012–2016 periods (Box 4).
During the pre-AIHCW period, the mean annual difference in full vaccination coverage between Indigenous and non-Indigenous children at 9 months of age in NSW was 6.6 percentage points (95% CI, 5.2–8.0); after the AIHCW Program was introduced, it was 3.7 percentage points (95% CI, 2.5–4.8). While there was a similar reduction in the rest of Australia, the difference between Indigenous and non-Indigenous coverage was considerably larger during both time periods than in NSW. In 2016, the difference in full vaccination coverage between Indigenous and non-Indigenous 9-month-old Australians in NSW was 1.6 percentage points (95% CI, –1.0 to 4.1; ie, coverage was not significantly different), but 7.6 percentage points (95% CI, 6.0–9.3) in the rest of Australia (Box 5).
At 15 months of age, the average annual difference in full vaccination coverage between Indigenous and non-Indigenous children in NSW during the pre-AIHCW period was 4.6 percentage points (95% CI, 3.1–6.0); after the AIHCW Program was introduced, it was 2.2 percentage points (95% CI, 1.0–3.4), a statistically non-significant reduction. In the rest of Australia, the average annual difference during both periods was about 6.0 percentage points. In 2016, the difference in full vaccination coverage between Indigenous and non-Indigenous 15-month-old Australians in NSW was 0.4 percentage points (95% CI, –2.2 to 2.9; ie, coverage was not significantly different), but 4.5 percentage points (95% CI, 2.8–6.2) in the rest of Australia (Box 5).
At 51 months of age, the average annual difference in full vaccination coverage between Indigenous and non-Indigenous children in NSW during the pre-AIHCW period was 8.5 percentage points (95% CI, 7.2–9.8); after the AIHCW Program was introduced, it was 0.6 percentage points (95% CI, –0.6 to 1.8 percentage points; ie, coverage was not significantly different). In the rest of Australia, the average annual difference also decreased significantly, from 6.7 percentage points (95% CI, 5.9–7.5) during 2008–2011 to 2.2 percentage points (95% CI, 1.4–2.9) during 2012–2016. In 2016, there was no statistically significant difference in full coverage between Indigenous and non-Indigenous 51-month-old Australians in NSW or in the rest of Australia (Box 5).
Discussion
We found that timely vaccination coverage in Indigenous children, measured at earlier assessment milestones than those usually used when reporting coverage in Australia, improved substantially in NSW after the AIHCW Program was introduced in 2012. The gap in timely coverage between Indigenous and non-Indigenous children also declined substantially, and coverage was not statistically significantly different in 2016. Complete vaccination coverage in Indigenous children in the rest of Australia also improved, but the reduction in the gap between Indigenous and non-Indigenous children was more pronounced in NSW, particularly at the 15- and 51-month milestones.
Timely vaccination is important because there are greater risks of complications and serious outcomes for many vaccine-preventable diseases if they are contracted early in life. Several Australian studies have emphasised the importance of monitoring timeliness of vaccination as a benchmark for evaluating the effectiveness of vaccination programs, particularly in Indigenous Australian children.3,15-18 However, the usual assessment milestones (12, 24, 60 months) allow a 6–12-month lag period after vaccines are due, as opposed to the 3-month lag period in our study, and can therefore mask differences in timeliness.3
Indigenous Australian children face a number of barriers to vaccination. A targeted vaccination program had a moderate impact on improving the uptake of the 7-valent pneumococcal conjugate vaccine in an urban NSW setting, but the authors of the study highlighted a number of system-level barriers, such as accurately identifying Indigenous children.19 Improving Indigenous identification is a key activity of AIHCWs, as is contacting and directing Indigenous families with young infants to culturally appropriate vaccination services. A pre-call strategy (contacting parents of Indigenous children before their scheduled vaccination dates), as practised by many AIHCWs, has been found to be of particular benefit in increasing vaccination coverage of Indigenous children.20
The rise in full vaccination coverage during the pre-AIHCW period among Indigenous and non-Indigenous children in NSW and the rest of Australia, particularly at the 51-month milestone, is probably attributable to a focus on improved timeliness of vaccination facilitated by a change to the overdue rules of the register in January 2009; specifically, children were now deemed overdue for their pre-school boosters at 49 rather than 60 months of age. This change had an impact on eligibility for parental incentive payments and outcome payments for providers.21
Limitations
Limitations of our study include its ecological nature; by combining data for all states and territories other than NSW, differences between these jurisdictions were concealed. Other initiatives that aimed to improve vaccination coverage and timeliness in NSW during the study period included the Save the Date to Vaccinate campaign and smartphone app22 (introduced in April 2013), as well as vaccination requirements for childcare enrolment23 (implemented from 1 January 2014). While targeting all children, these initiatives may have created a supportive environment for the AIHCW Program. The federal “No Jab, No Pay” policy,24 which aimed to improve vaccination coverage nationally by introducing annual vaccination prerequisites for receiving family assistance payments, and the removal of conscientious objection provisions, were not implemented until 1 January 2016, the final year of data analysed in our study. While No Jab, No Pay might differentially affect Indigenous people because of socio-economic factors,25 this national initiative would not be expected to have a differential impact in NSW and the rest of Australia on differences in coverage between Indigenous and non-Indigenous Australians.
Conclusion
It is therefore probable that the NSW AIHCW Program has contributed to the improvements in Indigenous childhood vaccination coverage and timeliness in NSW since 2012 being more pronounced than in the rest of Australia. This suggests that the commitment of significant resources to a dedicated program specifically targeted to the needs of Indigenous Australians, staffed by Indigenous workers who know their communities and are able to engage with them in a culturally appropriate way, may help overcome barriers to timely vaccination and have a marked impact on closing the vaccination coverage gap between Indigenous and non-Indigenous Australian children.
Box 1 – Vaccinations required by the 9, 15 and 51 months of age milestones for the child to be deemed fully vaccinated
|
|
|||||||||||||||
|
9 months
|
|||||||||||||||
|
|
|||||||||||||||
|
DTPa = diphtheria–tetanus–pertussis (acellular), paediatric formulation; hepB = hepatitis B; Hib = Haemophilus influenzae type b; IPV = inactivated poliovirus; MMR = measles–mumps–rubella. |
|||||||||||||||
Box 2 – Proportion of children at 9 months of age who were fully vaccinated (with 95% confidence intervals), for New South Wales and the rest of Australia, by Indigenous status, 2008–2016
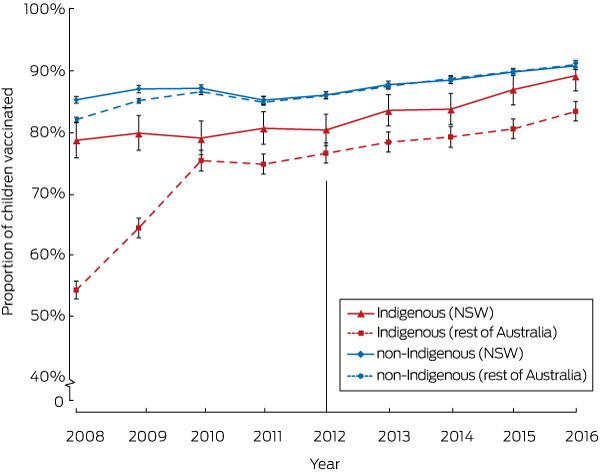
Coverage assessed in each calendar year for cohorts born between 1 July of preceding year to 30 June of the reference year. Vertical line indicates initial year of the Aboriginal Immunisation Healthcare Worker Program. Source: Australian Immunisation Register, as at 30 September 2017.
Box 3 – Proportion of children at 15 months of age who were fully vaccinated (with 95% confidence intervals), for New South Wales and the rest of Australia, by Indigenous status, 2008–2016
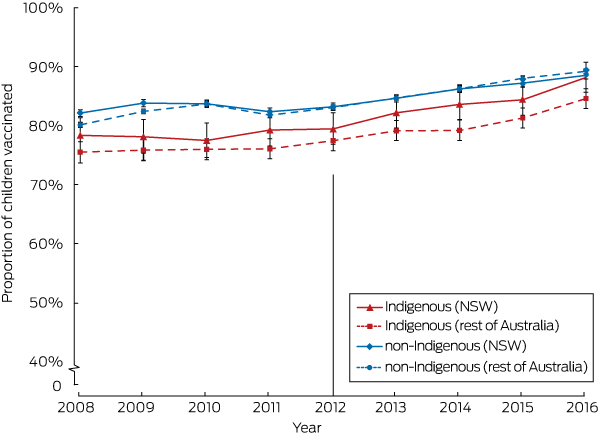
Coverage assessed in each calendar year for cohorts born in the preceding calendar year (1 January – 31 December). Vertical line indicates initial year of the Aboriginal Immunisation Healthcare Worker Program. Source: Australian Immunisation Register, as at 30 September 2017.
Box 4 – Proportion of children at 51 months of age who were fully vaccinated (with 95% confidence intervals), for New South Wales and the rest of Australia, by Indigenous status, 2008–2016
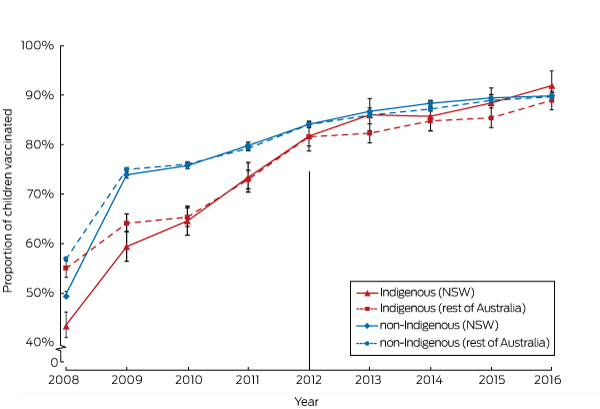
Coverage assessed in each calendar year for cohorts born in the four calendar years (1 January – 31 December) prior to the reference year. Vertical line indicates initial year of the Aboriginal Immunisation Healthcare Worker Program. Source: Australian Immunisation Register, as at 30 September 2017.
Box 5 – Annual differences between Indigenous and non-Indigenous Australians in full vaccination coverage estimates at three age milestones, in NSW and the rest of Australia, 2008–2016
|
|
9 months of age* |
15 months of age† |
51 months of age‡ |
||||||||||||
|
NSW |
Rest of Australia |
NSW |
Rest of Australia |
NSW |
Rest of Australia |
||||||||||
|
|
|||||||||||||||
|
Difference in percentage points (95% confidence interval) |
|||||||||||||||
|
2008 |
6.6 (3.7–9.5) |
27.9 (26.4–29.4) |
3.7 (0.8–6.6) |
4.5 (2.7–6.3) |
5.5 (3.2–7.8) |
1.7 (0.1–3.3) |
|||||||||
|
2009 |
7.2 (4.3–10.2) |
20.8 (19.2–22.5) |
5.6 (2.8–8.4) |
6.4 (4.7–8.2) |
12.8 (10.1–15.5) |
9.6 (7.9–11.2) |
|||||||||
|
2010 |
8.1 (5.3–10.9) |
11.3 (9.5–13.0) |
6.1 (3.2–9.0) |
7.5 (5.7–9.3) |
9.9 (7.2–12.5) |
9.4 (7.8–11.1) |
|||||||||
|
2011 |
4.6 (1.9–7.3) |
10.1 (8.4–11.8) |
3.0 (0.3–5.7) |
5.6 (3.9–7.3) |
5.7 (3.0–8.4) |
5.6 (3.9–7.2) |
|||||||||
|
2012 |
5.7 (3.1–8.3) |
9.4 (7.7–11.1) |
3.7 (1.0–6.3) |
5.5 (3.7–7.2) |
2.1 (–0.6 to 4.8) |
2.2 (0.4–3.9) |
|||||||||
|
2013 |
4.2 (1.6–6.8) |
9.2 (7.4–10.9) |
2.4 (–0.2 to 5.0) |
5.4 (3.7–7.2) |
0.6 (–2.3 to 3.5) |
3.2 (1.5–5.0) |
|||||||||
|
2014 |
4.7 (2.1–7.4) |
9.6 (7.9–11.3) |
2.6 (0.0–5.2) |
6.9 (5.2–8.6) |
2.3 (–0.4 to 5.1) |
2.1 (0.4–3.9) |
|||||||||
|
2015 |
2.9 (0.3–5.5) |
9.4 (7.7–11.1) |
2.8 (0.2–5.4) |
6.6 (4.9–8.3) |
0.9 (–1.8 to 3.6) |
3.1 (1.4–4.9) |
|||||||||
|
2016 |
1.6 (–1.0 to 4.1) |
7.6 (6.0–9.3) |
0.4 (–2.2 to 2.9) |
4.5 (2.8–6.2) |
–1.8 (–4.4 to 0.8) |
0.6 (–1.1 to 2.3) |
|||||||||
|
2008–2011, mean |
6.6 (5.2–8.0) |
17.4 (16.5–18.2) |
4.6 (3.1–6.0) |
6.0 (5.1–6.9) |
8.5 (7.2–9.8) |
6.7 (5.9–7.5) |
|||||||||
|
2012–2016, mean |
3.7 (2.5–4.8) |
8.9 (8.2–9.7) |
2.2 (1.0–3.4) |
5.7 (4.9–6.4) |
0.6 (–0.6 to 1.8) |
2.2 (1.4–2.9) |
|||||||||
|
|
|||||||||||||||
|
* Coverage assessed in each calendar year for cohorts born between 1 July of preceding year to 30 June of the reference year. † Coverage assessed in each calendar year for cohorts born in the preceding calendar year (1 January – 31 December). ‡ Coverage assessed in each calendar year for cohorts born in the four calendar years (1 January – 31 December) prior to the reference year. Source: Australian Immunisation Register, as at 30 September 2017. |
|||||||||||||||
Received 17 January 2018, accepted 23 April 2018
- Alexandra J Hendry1
- Frank H Beard1,2
- Aditi Dey1,2
- Dennis Meijer3
- Sue Campbell-Lloyd3
- Katrina K Clark1
- Brynley P Hull1
- Vicky Sheppeard3
- 1 National Centre for Immunisation Research and Surveillance, The Children's Hospital at Westmead, Sydney, NSW
- 2 University of Sydney, Sydney, NSW
- 3 Health Protection, New South Wales Ministry of Health, Sydney, NSW
We acknowledge the work and commitment of all past and present Aboriginal health care workers employed under the New South Wales Aboriginal Immunisation Healthcare Worker Program, without whom the progress toward closing the vaccination gap between Indigenous and non-Indigenous children in NSW, as documented in our article, would not have been possible.
No relevant disclosures.
- 1. Naidu L, Chiu C, Habig A, et al. Vaccine preventable diseases and vaccination coverage in Aboriginal and Torres Strait Islander people, Australia 2006–2010. Commun Dis Intell Q Rep 2013; 37: S1-S95.
- 2. Hull BP, McIntyre PB. Timeliness of childhood immunisation in Australia. Vaccine 2006; 24: 4403-4408.
- 3. O’Grady KA, Krause V, Andrews R. Immunisation coverage in Australian Indigenous children: time to move the goal posts. Vaccine 2009; 27: 307-312.
- 4. Harris MF, Webster V, Jalaludin B, et al. Immunisation coverage among a birth cohort of Aboriginal infants in an urban community. J Paediatr Child Health 2014; 50: 306-313.
- 5. Aboriginal and Torres Strait Islander Social Justice Commissioner; Steering Committee for Indigenous Health Equality. Closing the Gap: National Indigenous health equality targets. Canberra: Human Rights and Equal Opportunity Commission, 2008. https://www.humanrights.gov.au/publications/closing-gap-national-indigenous-health-equality-targets-2008 (viewed Dec 2016).
- 6. Australian Bureau of Statistics. 3101.0. Australian demographic statistics: June quarter 2017. 14 Dec 2017. http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/0DEC5B368C5C2D72CA2581F5001011EB/$File/31010_jun%202017.pdf (viewed Dec 2017).
- 7. Menzies R, Knox S, Kelaher B, et al. Process evaluation of the New South Wales Aboriginal Immunisation Healthcare Worker Program. Sydney: National Centre for Immunisation Research and Surveillance, 2015. http://www.health.nsw.gov.au/immunisation/Documents/process-evaluation-aihcw-program.pdf (viewed Dec 2016).
- 8. Tashani M, Dey A, Clark K, Beard F. Stage 2. Evaluation of the NSW Aboriginal Immunisation Healthcare Worker Program. Process evaluation. Sydney: National Centre for Immunisation Research and Surveillance, 2017. http://www.health.nsw.gov.au/immunisation/Documents/stage-2-evaluation-aihcw-program.pdf (viewed Sept 2017).
- 9. Australian Department of Human Services. Australian Immunisation Register for health professionals. Updated May 2018. https://www.humanservices.gov.au/organisations/health-professionals/services/medicare/australian-immunisation-register-health-professionals (viewed May 2018).
- 10. Rank C, Menzies RI. How reliable are Australian Childhood Immunisation Register coverage estimates for Indigenous children? An assessment of data quality and coverage. Commun Dis Intell Q Rep 2007; 31: 283-287.
- 11. O’Brien ED, Sam GA, Mead C. Methodology for measuring Australia’s childhood immunisation coverage. Commun Dis Intell Q Rep 1998; 22: 36-37.
- 12. Hull B, Hendry A, Dey A, et al. Immunisation coverage annual report, 2014. Commun Dis Intell Q Rep 2017; 41: E68-E90.
- 13. Hull BP, McIntyre PB. Immunisation coverage reporting through the Australian Childhood Immunisation Register — an evaluation of the third-dose assumption. Aust N Z J Public Health 2000; 24: 17-21.
- 14. Hull BP, Lawrence GL, MacIntyre CR, McIntyre PB. Estimating immunisation coverage: is the “third dose assumption” still valid? Commun Dis Intell Q Rep 2003; 27: 357-361.
- 15. Abbott P, Menzies R, Davison J, et al. Improving immunisation timeliness in Aboriginal children through personalised calendars. BMC Public Health 2013; 13: 598-605.
- 16. Bailie R, Si D, Dowden M, et al. A systems approach to improving timeliness of immunisation. Vaccine 2009; 27: 3669-3674.
- 17. Lovie-Toon Y, Hall K, Chang A, et al. Immunisation timeliness in a cohort of urban Aboriginal and Torres Strait Islander children. BMC Public Health 2016; 16: 1159-1169.
- 18. Menzies R, Andrews R. Immunisation issues for Indigenous Australian children. J Paediatr Child Health 2014; 50: E21-E25.
- 19. Thomas P, Joseph TL, Menzies RI. Evaluation of a targeted immunisation program for Aboriginal and Torres Strait Islander infants in an urban setting. NSW Public Health Bull 2008; 19: 96-99.
- 20. Cashman PM, Allan NA, Clark KK, et al. Closing the gap in Australian Aboriginal infant immunisation rates — the development and review of a pre-call strategy. BMC Public Health 2016; 16: 514-520.
- 21. Hull BP, Dey A, Beard FH, et al. Immunisation coverage annual report, 2013. Commun Dis Intell Q Rep 2016; 40: E146-E169.
- 22. New South Wales Ministry of Health. Save the date to vaccinate. Feb 2014. http://www.health.nsw.gov.au/immunisation/Pages/brochure-immunisation.aspx (viewed Mar 2018).
- 23. New South Wales Ministry of Health. Questions and answers about vaccination requirements for child care. 2018. http://www.health.nsw.gov.au/immunisation/Pages/childcare_qa.aspx (viewed Mar 2018).
- 24. Australian Government Department of Health. No Jab, No Pay — New Immunisation requirements for Family Assistance Payments. Fact sheet for providers. Dec 2017. https://beta.health.gov.au/resources/publications/no-jab-no-pay-new-requirements-fact-sheet (viewed Apr 2018).
- 25. Beard FH, Hull BP, Leask J, et al. Trends and patterns in vaccination objection, Australia, 2002–2013. Med J Aust 2016; 204: 275. <MJA full text>





Abstract
Objectives: To assess vaccination coverage and timeliness among Indigenous and non-Indigenous children in New South Wales and the rest of Australia, with a particular focus on changes in the vaccination coverage gaps after the introduction of the Aboriginal Immunisation Healthcare Worker (AIHCW) Program in NSW in 2012.
Design: Cross-sectional analysis of Australian Immunisation Register data (2008–2016).
Main outcome measures: Annual estimates of full vaccination coverage at 9, 15 and 51 months of age for Indigenous and non-Indigenous children in NSW and the rest of Australia; differences in coverage between Indigenous and non-Indigenous children at each milestone.
Results: The proportion of Indigenous and non-Indigenous children classified as fully vaccinated at 9, 15, and 51 months increased significantly in both NSW and the rest of Australia after the introduction of the AIHCW Program. The mean annual difference in full vaccination coverage between Indigenous and non-Indigenous children in NSW aged 9 months declined from 6.6 (95% CI, 5.2–8.0) during 2008–2011 to 3.7 percentage points (95% CI, 2.5–4.8) during 2012–2016; for those aged 15 months it declined from 4.6 (95% CI, 3.1–6.0) to 2.2 percentage points (95% CI, 1.0–3.4), and for those aged 51 months it declined from 8.5 (95% CI, 7.2–9.8) to 0.6 percentage points (95% CI, –0.6 to 1.8). Reductions in the differences in coverage were not as marked in the rest of Australia. In 2016, there was no statistically significant difference in coverage at any of the three milestones in NSW: at 9 months the difference was 1.6 percentage points (95% CI, –1.0 to 4.1); at 15 months, 0.4 percentage points (95% CI, –2.2 to 2.9); and at 51 months, –1.8 percentage points (95% CI, –4.4 to 0.8).
Conclusion: Our findings suggest that a dedicated program can help overcome barriers to timely vaccination and significantly improve timely vaccination rates in Indigenous Australian children.