The known National and international policies emphasise the importance of improving mental health care for young people, but the cost-effectiveness of youth mental health care is unclear.
The new We identified a list of attributes of youth mental health care that may be acceptable to young people and potentially cost-effective.
The implications More economic evaluations are required in youth mental health. Those examining the impact of automated processes, that value the preferences of young people and their families and that examine costs from both societal and health care perspectives may be particularly useful.
Improved prevention and treatment of mental and neurological disorders has been identified as the core health challenge of the 21st century.1 Mental disorders are a major contributor to the global burden of disease,2 with recent analysis suggesting they might account for a third of life-years lost to disability — the greatest burden of any group of illnesses.3 Mental disorders also rank among the most significant causes of death worldwide,4 with those affected dying a decade or more earlier than the general population; and this life expectancy gap may be widening.5 The economic consequences are stark, with the impact on individuals including higher unemployment, premature retirement, lower income and financial insecurity.1,6-9 Enterprises and economies bear major reductions in productivity,10-13 with mental disorders ranking as the main non-communicable disease-related risk to global economic output.14
There is scope for major health and prosperity dividends globally from improved approaches to mental health care. The anticipated economic benefits of population-level strategies to scale up access to existing treatments are substantial.15-18 However, despite growing awareness of the grave personal, societal and economic consequences of mental disorders, governments around the world continue to give inadequate priority to mental health care.19 Globally, the response remains characterised by underfunded, inequitable and inefficient service systems.20 Even in high-income countries, failures of system organisation and financing create barriers to adequate uptake of appropriate treatments.12
Mental health care in Australia conforms to this global pattern, with a poorly designed mental health system that routinely misses opportunities for early intervention and overwhelmingly directs public expenditure towards acute care and welfare payments.21 Only half of all health care system encounters for depression in Australia result in appropriate care being provided.22 Over the past 12 years, successive Australian governments have made efforts to respond to these challenges, by building primary mental health care capacity and developing new approaches to system financing and organisation. Initiatives have included the Better Access program, to enhance the participation of general practitioners in mental health care and improve access to psychiatry and psychological services,23 and establishing the National Mental Health Commission to monitor the performance of, and catalyse improvements in, the mental health system.24
Enhancing access to appropriate and holistic care for young people with or at risk of mental disorders has been identified as a priority focus for global efforts to pre-empt and reduce the impact of mental disorders.25 Three-quarters of mental disorders first emerge in people by their mid 20s,26 negatively affecting these young people’s future educational attainment, workforce participation, income and living standards.27,28 However, mental health supports for young people also remain poorly targeted, with highly variable service use.29 To deal with this problem, youth mental health reforms, including those outlined elsewhere in this supplement, have been initiated in Asia, Australia, New Zealand, Europe, the Middle East and North America.30 The Australian Government is currently funding Primary Health Networks to develop novel service approaches for young people with emerging severe and complex non-psychotic illnesses. These novel youth mental health services will be developed and trialled while the Australian Government implements a new stepped model of care to shape the future financing and organisation of primary mental health care services.31,32 It is therefore likely that innovative approaches to youth mental health service delivery will need to show evidence of value for money to be recommended for widespread adoption. New services may be more likely to demonstrate cost-effectiveness if their design incorporates attributes of youth mental health care for which there is already some supporting economic evidence.
In this study, we aimed to identify potentially cost-effective attributes of youth mental health care by examining economic evaluations of mental health services and supports for young people aged 12–25 years published in the past 20 years.
Methods
We undertook a literature review to identify attributes of youth mental health care for which there is evidence of potential cost-effectiveness. We conducted a search for economic evaluations relevant to youth mental health in the United Kingdom National Health Service (NHS) Economic Evaluations Database, which included economic evaluations published up to the end of 2014. We supplemented this search with a series of focused searches in MEDLINE and Google Scholar for additional economic evaluations relevant to youth mental health services. We also reviewed the citation lists of relevant publications known to us.
We included only peer-reviewed studies published in English since 1997 that included information about both costs and outcomes for at least two alternatives (at least one active intervention and a comparator that could be an active intervention or no care). We included studies where the entire age range of participants was within the bounds of 12 to 25 years (inclusive), where most of the years in the age range of participants were within these bounds, or where the mean or median age of participants was within this age range. Where age ranges were not clearly defined, we included studies if participants were described as “youth”, “young people”, “teenagers”, “adolescents” or “children and adolescents”. We also included any studies of first-episode psychosis services, even when these services had eligible age ranges extending into middle age, as the epidemiology of psychosis suggests that these services are predominantly youth-focused.
We excluded studies that did not meet our age range criteria, were not peer-reviewed, were reviews without linked modelling studies, did not explicitly address mental health, explored costs but not outcomes, reported only uncosted resource use or had no comparator. Studies that evaluated only pharmacological or individual psychological therapies for full-threshold disorders were also excluded. Studies evaluating psychological therapies delivered in a group or family format or for the main purpose of prevention were included.
From each of the studies, we extracted the following data: year of publication, mental health problems of participants, age range of participants, intervention type, study design, type of economic analysis undertaken, time horizon for assessment of costs and outcomes, what kinds of perspectives on costs were reported, and author conclusions.
Included studies were critically appraised by one of us (M H) using the 10-item Drummond checklist,33 scoring 1 point for “condition met”, 0.5 points for “condition partially met” and 0 points for “condition not met”. A random sample of seven studies was reassessed by the coauthors to ensure data quality. Recent guidance for the conduct of economic evaluations recommends that studies include two reference case perspectives: a societal perspective (which counts all costs, including productivity losses) and a health care perspective (which counts only health care-related costs).34 For this reason, we required that for item four on the checklist (Did a study examine all relevant costs and consequences?) to be judged as fully met, a study would need to report and include appropriate costs for two or more perspectives, at least one of which had to be the societal perspective.
For each included study, we identified the attributes that comprised the interventions being examined and analysed these thematically to identify potentially cost-effective attributes of youth mental health care. As first-episode psychosis services can have up to 16 service components,35 and it was not always clear how many of these attributes were present in each case, we assigned these services a catch-all attribute of “early intervention”.
We also briefly examined some of the excluded economic studies and other studies of the preferences of young people for evidence of potentially important economic topics not addressed by our included studies.
Results
We identified 40 economic evaluations of mental health services targeted at youth populations that met our inclusion criteria (Box 1).36-75 There was heterogeneity of design, type of economic analysis and perspectives on costs across the studies. Twenty-four of the included studies were wholly or partially based on randomised controlled trial (RCT) designs and nine studies used historic or parallel controls. There were 11 modelling studies, including four that used modelling to extend the analysis of RCT results. Twenty-one studies involved cost-effectiveness analysis, 16 used cost–utility analysis, eight used cost–consequence analysis, and four used cost–benefit analysis. Nine studies used more than one type of economic analysis.
Thirteen studies took a societal perspective on costs (including two that did not explicitly declare this perspective); 13 studies (including one where the perspective was not stated) appeared to adopt narrower perspectives, which included but were not confined to health care (eg, health and social care, health care plus education); 15 studies (including four where the perspective was not explicitly stated) appeared to adopt a health care or subset of health care perspective (eg, public health care, public mental health); and one study (with inadequate justification in our judgement) adopted an employer perspective. Two studies adopted more than one perspective.
The types of mental health problems addressed by the included studies are shown in Box 2. About a third (n = 14) of the included studies focused on psychotic disorders. The next most common problem addressed was depression (n = 8), followed by substance use disorders (n = 6), eating disorders (n = 6), suicide and self-harm (n = 4), anxiety (n = 2), forensic mental health (n = 2) and general mental illness (n = 2). No studies specifically focused on services for young people with personality disorders.
There was wide variety in the assessed quality of the included studies (Box 3). There was a slight trend for more recent studies to score higher. No study fully met our stringent criteria for item four of the checklist. Twelve studies did not use discounting even when time horizons exceeded 1 year. Seven studies did not report incremental costs and incremental benefits and eight did not explore the uncertainty of cost and benefit estimates.
The only topics for which multiple economic evaluations of the same intervention for broadly similar target populations reported consistent economic findings were prevention and early intervention in psychosis (Box 1). There was good evidence of cost-effectiveness for first-episode psychosis services36-45 and some cost-effectiveness evidence for interventions to prevent or delay transition to psychotic disorder among high-risk individuals.46,47 Additionally, there was some economic evidence for strategies to further improve the cost-effective delivery of services to these groups of young people.48,49
There was emerging encouraging evidence for the cost-effectiveness of a range of care attributes for young people with mental health problems other than psychosis. However, this evidence base did not have the consistent replication of cost-effectiveness findings that was seen with studies on early psychosis services, and it is likely that some attributes may be cost-effective for some groups of young people but not others.
Timely assessment strategies, including screening, were attributes of interventions for a range of mental health problems examined in 10 of the included studies (Box 4).47,49-57 The economic evidence for such approaches was generally favourable, although there were exceptions.52,55 Schools-based screening and prevention interventions were examined for anxiety,58 depression,47,53,62,63 eating disorders52,59 and substance use disorders.60 A UK RCT61,62 and Australian modelling studies47,53,63 came to different conclusions about the potential cost-effectiveness of schools-based prevention strategies for depression, although challenges relating to acceptability and implementation of such strategies were highlighted in both contexts. There was similarly mixed evidence for schools-based prevention strategies for eating disorders.52,56,59
Five economic evaluations explored services that included the attribute of home-based delivery for a range of distinct populations of young people,50,64-67 with a mixture of supportive and non-supportive evidence for this mode of delivery (Box 1). Thirteen studies explored interventions that included support for families — mainly family therapy and education for a range of mental health problems. In general, there was supportive evidence for family-based interventions, although in several studies, individual therapy or self-help options were suggested to be more cost-effective alternatives.66,68,69 A group delivery context (including in classrooms) was an attribute of interventions for a range of mental health problems in nine studies,47,52,58,60-63,70,71 again with cost-effectiveness evidence that varied between populations. Other attributes of interventions examined were automated processes,63 case management,48,50,65-67 crisis response,51 financing,72 holistic care approaches,48,58,72 information provision,54,57,61,62,67,69,71 peer support and mentoring57,71 and staff training and support49 (Box 4).
In addition to the studies that met our inclusion criteria, our review identified other resources that could help flesh out the current state of economic evidence in youth mental health. These were studies that examined only costs or did not cost resource use,76-89 did not include a comparator,90,91 were not explicitly focused on mental health outcomes,92,93 pre-dated 1997,94-97 examined individual treatments for full-threshold disorders,98-115 were evidence reviews,116-126 were not peer-reviewed120,127-129 or were primarily focused on matters relating to system financing.77,130 To integrate the findings from our review of included studies with the themes identified in our briefer review of excluded studies and preference studies, we prepared a list of attributes of youth mental health care that may be acceptable to young people and potentially cost-effective (Box 5).
Discussion
In this review, we identified good cost-effectiveness evidence for mental health care for young people with, or at risk of, psychosis, and a developing evidence base for a wide range of attributes of care for young people with other mental health problems. Overall, the findings from our review highlight the need to further develop the economic evidence base in youth mental health. There is a need for replication of cost-effectiveness findings in service system contexts beyond early psychosis services.
Future economic evaluations in youth mental health should also address the methodological problems we identified. First, we found that none of our included studies adequately implemented cost analyses from both a societal perspective and a health care perspective. A societal perspective is important because mental disorders are associated with major costs outside the health system, while a health care perspective will be important to decision makers because mental health care is largely funded from public health care budgets in many countries. Second, despite a growing evidence base on the mental health service preferences of young people and their families,131-141 valuation of such preferences was not integrated into any of the economic evaluations we reviewed. Data on young people’s preferences, particularly when elicited and valued using discrete choice experiment study designs, enable comprehensive approaches to economic evaluation that value both health and non-health (eg, service experience) aspects of mental health programs for young people. More broadly, preferences are relevant to the acceptability, desirability, design and targeting of health services. In largely publicly funded health systems, there is a normative question about how preferences should shape health policy (ie, whose preferences hold most sway: the users of services, clinical experts or the wider population in whose name governments raise taxes to fund health care services).142-144
There are also practical reasons why young people’s preferences should influence youth mental health service system design. To encourage early and effective engagement of young people with emerging mental health problems, it has been recommended that the planning and commissioning of youth mental health services should explicitly account for young people’s preferences.145 Involving young people in the design, provision and assessment of health services has been recommended as a strategy for making these services more closely aligned with their preferences.146,147 It should be noted that the available evidence suggests that young people’s preferences can vary significantly, potentially shaped by factors such as age and sex.134,141 Some preference studies have identified broadly delineated subgroups of young people with similar overall profiles of preferences for youth mental health information and services,132,137 which may enhance the targeting of services. There is a strong case for a sustained program of preference-based research using discrete choice experiment designs for use in service planning and economic evaluation of youth mental health care. High-quality discrete choice experiments in youth mental health have been undertaken in recent years,132,135-138 and the list of attributes of youth mental health care we identified might be a useful resource for researchers planning further such experiments.
Only one of our included studies examined an intervention involving an automated process. There is a case for more economic evaluations of interventions that incorporate automated processes in both front-end service delivery and back-end office systems. Although many young people may prefer to receive mental health help in more traditional face-to-face formats,134 some young people prefer to access assessment and mental health supports through websites and applications.132,137 Evidence from physical health care cautions that computer algorithm-based assessment and triage tools are generally risk-averse and may encourage unnecessary health care usage.148 However, there is some evidence relating to the potential of computer-based functional assessment.149 Evidence from physical health care suggests that new collaborative technologies to promote integrated care between autonomous and geographically dispersed primary care services may help improve outcomes for patients with chronic conditions.150
To improve the efficiency of mental health services for young people, cost-effective interventions and service models need to be implemented successfully. There is emerging evidence about the factors that predict successful deployments of strategies to improve collaborations and supporting processes in health care,151-153 which include a perceived low burden of implementation, adequate resources and appropriate implementation support. There is limited evidence on the cost-effectiveness of such strategies in mental health.154,155
Cost-effectiveness is not the same as cost saving and, because of the high prevalence of mental disorders in young people, even highly cost-effective approaches may be expensive to implement. There is therefore a need for economic research to explore how youth mental health service system improvements can be financed. There might be scope to examine the potential for novel financing instruments, such as social impact bonds,156,157 to share risk and mobilise new sources of capital for early intervention investments. Further, regionally based commissioning marketplaces — the context within which primary mental health care in Australia now operates — can be challenging to appropriately implement,158 potentially requiring investment in developing local service system insight and relationships.159
A limitation of our study was that our literature review was exploratory in nature and not exhaustive. Recent economic evaluations may be under-represented in our sample because of our principle reliance on the NHS Economic Evaluations Database, which only included evaluations published before the end of 2014, although this limitation was partially overcome through supplementary focused searches in MEDLINE and elsewhere. Future reviews might provide a more complete description of the breadth, quality and implications of the economic evidence base relating to attributes of youth mental health care.
Findings from our study may be helpful in informing the planning of novel youth mental health services and for youth-focused refinements to the Australian Government’s stepped model of care. The complexity of mental health service planning is a reason why the computer-based National Mental Health Services Planning Framework tool has been developed, to help regional service planners operationalise the stepped model of care consistently with current evidence.160 There may be scope for new dynamic simulation modelling tools to address computationally intensive questions on the feasibility and potential impacts of alternative strategies to increase the efficiency of the youth mental health service system. Such techniques are increasingly deployed in epidemiology, health economics and health services research to explore research questions that involve the analysis of complex systems.161,162
In conclusion, we found there is encouraging cost-effectiveness evidence for a range of attributes of youth mental health care. However, further economic research is required to substantiate many cost-effectiveness findings and to identify the groups of young people to whom services can be optimally targeted. Other policy and research priorities include trialling novel services and ensuring future economic evaluations examine both societal and health care perspectives and better integrate preferences data.
Box 1 – Characteristics of included economic evaluation studies
Study |
Year |
Mental disorder |
Ages (years) |
Intervention type |
Design |
Analysis |
Time horizon |
Cost perspective |
Authors’ conclusions |
||||||
64 |
1999 |
Deliberate self-harm |
< 17 |
Home-based, family-centred social work v routine outpatient care |
RCT |
CEA |
6 months |
Service provision sectors |
Family-based social work is as cost-effective as routine care for children and adolescents who have deliberately poisoned themselves |
||||||
40 |
1999 |
Psychosis |
Not stated |
FEP service v routine care |
Historic control |
CEA |
1 year |
Public health care |
An FEP service is cost-effective |
||||||
72 |
2000 |
Comorbid substance use disorder and mental illness |
12–17 |
Continuum of care v routine fee-for-service care |
Parallel control |
CCA |
6 months |
Health care provider (implied) |
Assessing the cost-effectiveness of prevention services for at-risk clients would be an appropriate step for systems of managed care |
||||||
57 |
2003 |
Suicide |
15–19 |
Combination of community education, mentoring, screening and social work |
Historic control |
CUA, CBA |
Lifetime |
Societal |
Benefits of this suicide prevention program outweigh the costs |
||||||
65 |
2004 |
Cannabis use disorder |
12–18 |
Three types of family therapy and case management v two types of individual treatment (motivational enhancement therapy and CBT) |
RCT |
CEA |
1 year |
Societal |
Individual treatment more cost-effective than family support network therapy–case management; and adolescent community reinforcement approach family therapy–case management more cost-effective than individual treatment and multidimensional family therapy–case management |
||||||
67 |
2004 |
Mental health crisis |
10–17 |
MST v inpatient care |
RCT |
CEA |
1 year, |
Public health care |
MST is associated with better outcomes at lower costs in the short term, followed by equivalent costs and outcomes |
||||||
70 |
2005 |
MDD |
13–18 |
Group CBT for prevention |
RCT |
CEA, CUA |
1 year |
Societal |
Brief prevention program to reduce risk of depression in offspring of parents with depression is cost-effective |
||||||
45 |
2006 |
Psychosis |
Mean, 28.3 |
FEP service v routine care |
Historic and parallel controls |
CCA |
3 years |
Health care (implied) |
Implementing FEP services is clinically and economically feasible |
||||||
37 |
2006 |
Psychosis |
16–50 |
FEP service v routine care |
Historic control |
CCA |
2 years |
Hospital (implied) |
FEP services may be beneficial to patients and to health care system |
||||||
75 |
2007 |
AN |
12–18 |
Inpatient v specialist outpatient v general outpatient |
RCT |
CEA |
2 years |
Health, social care and education |
Results support provision of specialist outpatient care for young people with AN |
||||||
69 |
2007 |
BN, eating disorder NOS |
13–20 |
Family therapy v CBT-guided self-care |
RCT |
CCA |
1 year |
Health and social care, and patient (implied) |
CBT-guided self-care has slight advantage over family therapy based on lower cost, greater acceptability and faster reductions in binging |
||||||
68 |
2008 |
Anxiety |
8–18 |
Family CBT v individual CBT |
RCT |
CEA, CUA |
1 year, |
Societal |
Family CBT not more cost-effective than individual CBT for clinically anxious children |
||||||
71 |
2008 |
Suicide |
Mean, 21 |
Education and peer support |
Model |
CBA |
Lifetime |
Societal |
Benefits are greater than costs in both programs |
||||||
48 |
2009 |
Psychosis |
Mean, 28 |
Two types of case management (standard v social recovery-oriented) |
RCT |
CUA |
9 months |
Health and social care |
Social recovery-oriented case management may be more cost-effective that routine case management for patients with FEP, but more research is needed |
||||||
41 |
2009 |
Psychosis |
Mean, 22 |
FEP service v routine care |
Historic control |
CEA |
6 years, |
Public mental health care |
FEP services deliver better recovery rates at lower costs than standard mental health care |
||||||
66 |
2010 |
Substance use disorder |
12–18 |
Two types of individual and family therapy v home-based care and case management |
RCT |
CCA |
1 year |
Health care organisation (implied) |
Home-based care and case management not as cost-effective as combined clinic-based individual and family treatment |
||||||
39 |
2010 |
Psychosis |
16–40 |
FEP service v routine care |
RCT |
CEA |
1 year, |
Public health care, social care and justice |
An FEP service has a high probability of being cost-effective |
||||||
54 |
2010 |
Alcohol use disorder |
18–19 |
Two types of screening combined with counselling or advice and education |
RCT + model |
CEA, CUA |
1 year |
Provider and societal |
Brief intervention in emergency department for alcohol-involved youth represents a good investment |
||||||
36 |
2011 |
Psychosis |
17–30 |
FEP service v routine care |
Historic control |
CEA |
5 years |
Public health care |
FEP service is superior and may produce cost savings |
||||||
50 |
2011 |
Forensic mental health |
13–16 |
Screening and home-based family-focused care and clinic-based treatment v routine practice |
Pilot RCT |
CCA |
1 year |
Societal (implied) |
Under-treated offenders with mental health problems can be successfully identified and treated |
||||||
60 |
2011 |
Substance use disorder |
12 |
Family education v schools-based health education v family education and schools-based health education |
RCT + Model |
CBA |
5 years, |
Employer |
Substance use prevention programming is economically feasible |
||||||
47 |
2011 |
MDD, psychosis |
Child/adolescent (MDD), youth (psychosis) |
Screening and group psychological therapy (depression prevention), screening and individual CBT and pharmacological therapy (psychosis prevention) |
Model |
CUA |
5 years (MDD), |
Health care |
Screening and group psychological therapy for depression prevention is recommended for adoption, as is the psychosis prevention program, subject to the latter being further evaluated |
||||||
59 |
2011 |
BN |
10–14 |
Schools-based prevention (education and physical activity) |
RCT + model |
CUA |
10 years |
Societal |
Primary prevention programs such as this intervention should be considered by policymakers |
||||||
44 |
2011 |
Psychosis |
15–25 |
FEP service v routine care |
Historic control |
CEA |
2 years |
Public mental health care |
FEP services are likely to be cost-effective |
||||||
53 |
2012 |
MDD |
11–17 |
Screening and individual CBT |
Model |
CUA |
5 years |
Health care |
Screening and psychological therapy represent good value for money as a preventive measure for depression in 11–17-year-olds |
||||||
38 |
2013 |
Psychosis |
18–45 |
FEP service v routine care |
RCT |
CEA |
5 years |
Public sector |
FEP service has a high probability of being cost-effective |
||||||
73 |
2013 |
Alcohol use disorder |
Teenagers |
Family skills training |
RCT |
CEA |
1 year, |
Societal |
The family skills training program is potentially cost-effective for reducing alcohol use and binge drinking episodes in African American teenagers |
||||||
58 |
2013 |
Anxiety, depression |
13–18 |
Physical activity plus school health services v school health services |
RCT |
CUA |
1 year, |
Societal |
A twice-weekly dance intervention may be a cost-effective adjunct to school health services |
||||||
62 |
2013 |
Depression |
12–16 |
School classroom-based CBT v classroom health education |
RCT |
CEA, CUA |
1 year |
Health and social care |
Classroom-based CBT was not shown to be cost-effective |
||||||
74 |
2014 |
AN |
12–18 |
Two types of family therapy (family-based treatment v systemic family therapy) |
RCT |
CCA |
1 year, |
Health care |
Family-based treatment produces similar outcomes to systemic family therapy at lower cost for AN |
||||||
61 |
2014 |
Depression |
12–16 |
Classroom CBT v classroom health education |
RCT |
CEA, CUA |
1 year |
Health and social care |
Universal provision of classroom CBT is unlikely to be more cost-effective than usual school prevention for depression |
||||||
51 |
2014 |
Suicide |
12–17 |
Emergency department rapid response crisis team v routine care (outpatient or referral) |
RCT |
CEA |
6 months |
Societal and hospital |
Rapid response crisis team appears cost-effective from perspective of hospital, but no different than routine care from societal perspective |
||||||
56 |
2014 |
Eating disorder |
10–17 |
School-based screening |
Model |
CEA, CUA |
10 years |
Payer |
Cost-effectiveness of school-based eating disorder screening is comparable to many acceptable paediatric health interventions |
||||||
46 |
2015 |
Psychosis |
14–35 |
Individual CBT and routine care v routine care |
RCT |
CEA, CUA |
1 year, |
Societal (implied) |
CBT is a cost-saving adjunct to routine care for individuals at high risk of transition to FEP |
||||||
49 |
2015 |
Psychosis |
16–35 |
Information for GPs and liaison between primary and secondary care v information for GPs |
RCT + model |
CEA |
2 years |
Public health and social care |
An intensive intervention to improve liaison between primary and secondary care for people with early signs of psychosis was clinically effective and cost-effective |
||||||
55 |
2015 |
MDD |
10–21 |
Screening of young people who offend |
Model |
CUA |
1 year |
Public health care and youth justice |
There is a lack of evidence about the cost-effectiveness of screening for mental health problems in young people who offend |
||||||
42 |
2016 |
Psychosis |
15–40 |
FEP service v routine care |
RCT |
CEA, CBA |
2 years, |
Health care system |
Benefits of FEP services exceed costs, especially at future generic drug prices |
||||||
43 |
2016 |
Psychosis |
16–35 |
FEP service v routine care |
Parallel control |
CCA |
3 years |
Societal |
FEP services are associated with better outcomes at lower costs |
||||||
63 |
2017 |
MDD |
11–17 |
Schools-based universal (group) and indicated (individual) prevention (face-to-face v digital) |
Model |
CUA |
10 years |
Health care and education |
Schools-based psychological interventions appear to be cost-effective prevention strategies for depression, but depend on appropriate implementation |
||||||
52 |
2017 |
AN, BN |
15–18 |
Screening and group cognitive dissonance |
Model |
CUA |
10 years |
Health care |
Schools-based cognitive dissonance is not a cost-effective preventive strategy for AN and BN |
||||||
AN = anorexia nervosa. BN = bulimia nervosa. CBA = cost–benefit analysis. CBT = cognitive behavioural therapy. CCA = cost–consequence analysis. CEA = cost-effectiveness analysis. CUA = cost–utility analysis. FEP = first-episode psychosis. GP = general practitioner. MDD = major depressive disorder. MST = multisystemic therapy. NOS = not otherwise specified. RCT = randomised controlled trial. | |||||||||||||||
Box 3 – Critical appraisal of included studies: score on 10-item Drummond checklist33
Study |
Year |
Score for checklist item number* |
Mean |
||||||||||||
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 |
10 |
||||||
64 |
1999 |
1 |
1 |
1 |
0.5 |
1 |
1 |
na |
1 |
1 |
1 |
0.94 |
|||
40 |
1999 |
1 |
1 |
0.5 |
0.5 |
1 |
1 |
na |
1 |
1 |
1 |
0.89 |
|||
72 |
2000 |
0 |
0.5 |
0.5 |
0 |
0 |
0 |
0 |
0 |
0 |
0.5 |
0.15 |
|||
57 |
2003 |
1 |
1 |
0.5 |
0.5 |
0 |
1 |
1 |
1 |
1 |
1 |
0.8 |
|||
65 |
2004 |
1 |
1 |
1 |
0 |
1 |
1 |
na |
0.5 |
0 |
1 |
0.72 |
|||
67 |
2004 |
1 |
1 |
1 |
0.5 |
0.5 |
1 |
0 |
0.5 |
0 |
0.5 |
0.6 |
|||
70 |
2005 |
1 |
1 |
1 |
0.5 |
1 |
1 |
na |
1 |
1 |
1 |
0.94 |
|||
45 |
2006 |
0.5 |
0.5 |
0.5 |
0.5 |
0.5 |
0.5 |
0 |
0 |
0 |
0 |
0.3 |
|||
37 |
2006 |
0.5 |
1 |
0.5 |
0.5 |
1 |
1 |
0 |
0 |
0 |
0.5 |
0.5 |
|||
75 |
2007 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.95 |
|||
69 |
2007 |
0.5 |
1 |
1 |
0.5 |
0.5 |
1 |
na |
0 |
0 |
0.5 |
0.56 |
|||
68 |
2008 |
1 |
1 |
1 |
0.5 |
0.5 |
0.5 |
1 |
1 |
1 |
1 |
0.85 |
|||
71 |
2008 |
1 |
1 |
1 |
0.5 |
0 |
1 |
1 |
1 |
1 |
0.5 |
0.8 |
|||
48 |
2009 |
1 |
1 |
1 |
0.5 |
0.5 |
1 |
na |
1 |
1 |
1 |
0.89 |
|||
41 |
2009 |
1 |
1 |
0.5 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.9 |
|||
66 |
2010 |
0.5 |
1 |
1 |
0.5 |
1 |
1 |
na |
0 |
0 |
0 |
0.56 |
|||
39 |
2010 |
1 |
1 |
1 |
0.5 |
0.5 |
1 |
0 |
1 |
1 |
1 |
0.8 |
|||
54 |
2010 |
1 |
1 |
1 |
0.5 |
1 |
1 |
na |
1 |
1 |
1 |
0.94 |
|||
36 |
2011 |
1 |
1 |
0.5 |
0.5 |
1 |
1 |
0.5 |
1 |
0.5 |
0.5 |
0.75 |
|||
50 |
2011 |
0.5 |
1 |
1 |
0.5 |
1 |
0 |
0 |
0 |
0.5 |
0 |
0.45 |
|||
60 |
2011 |
1 |
1 |
1 |
0 |
0 |
0 |
1 |
1 |
1 |
0.5 |
0.65 |
|||
47 |
2011 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.95 |
|||
59 |
2011 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
0.5 |
0.9 |
|||
44 |
2011 |
1 |
1 |
0.5 |
0.5 |
1 |
1 |
0 |
1 |
1 |
1 |
0.8 |
|||
53 |
2012 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
0.5 |
0.9 |
|||
38 |
2013 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.95 |
|||
73 |
2013 |
1 |
1 |
1 |
0.5 |
1 |
1 |
0 |
1 |
1 |
0.5 |
0.8 |
|||
58 |
2013 |
1 |
1 |
1 |
0.5 |
1 |
1 |
0 |
1 |
1 |
1 |
0.85 |
|||
62 |
2013 |
1 |
1 |
1 |
0.5 |
1 |
1 |
na |
1 |
1 |
1 |
0.94 |
|||
74 |
2014 |
0.5 |
1 |
1 |
0.5 |
0.5 |
1 |
0 |
0 |
0 |
0 |
0.45 |
|||
61 |
2014 |
1 |
1 |
1 |
0.5 |
0.5 |
1 |
na |
1 |
0.5 |
1 |
0.83 |
|||
51 |
2014 |
1 |
1 |
1 |
0.5 |
1 |
1 |
na |
1 |
1 |
1 |
0.94 |
|||
56 |
2014 |
1 |
1 |
0 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.85 |
|||
46 |
2015 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.95 |
|||
49 |
2015 |
1 |
1 |
1 |
0.5 |
1 |
1 |
0 |
1 |
1 |
1 |
0.85 |
|||
55 |
2015 |
1 |
1 |
0.5 |
0.5 |
1 |
1 |
na |
1 |
1 |
1 |
0.89 |
|||
42 |
2016 |
1 |
1 |
1 |
0.5 |
0.5 |
0.5 |
na |
1 |
1 |
1 |
0.83 |
|||
43 |
2016 |
1 |
1 |
0.5 |
0.5 |
1 |
1 |
0 |
0.5 |
1 |
0.5 |
0.7 |
|||
63 |
2017 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.95 |
|||
52 |
2017 |
1 |
1 |
1 |
0.5 |
1 |
1 |
1 |
1 |
1 |
1 |
0.95 |
|||
na = not applicable. * Checklist items: 1. Was a well-defined question posed in answerable form? 2. Was a comprehensive description of the competing alternatives given (ie, can you tell who did what to whom, where and how often)? 3. Was the effectiveness of the program or services established? 4. Were all the important and relevant costs and consequences for each alternative identified? 5. Were costs and consequences measured accurately in appropriate physical units (eg, hours of nursing time, number of physician visits, lost work-days, gained life-years)? 6. Were the costs and consequences valued credibly? 7. Were costs and consequences adjusted for differential timing? 8. Was an incremental analysis of costs and consequences of alternatives performed? 9. Was allowance made for uncertainty in the estimates of costs and consequences? 10. Did the presentation and discussion of study results include all issues of concern to users? | |||||||||||||||
Box 5 – Attributes of youth mental health care that may be acceptable to young people and potentially cost-effective
Attribute |
Implementation |
||||||||||||||
Access |
|||||||||||||||
Affordability and convenience |
Fees: low or no out-of-pocket costs to young people |
||||||||||||||
Helpful information |
Education: developing mental health literacy and supporting self-help |
||||||||||||||
Holistic and timely initial assessment |
Scope: including mental and physical health, psychosocial risk and protective factors; enhancing detection accuracy through use of multiple tiers of screening |
||||||||||||||
Welcoming environment |
Age-appropriateness: availability of youth-specific environments |
||||||||||||||
Care |
|||||||||||||||
Coordinated care |
Modality: information exchange, care coordination and case management |
||||||||||||||
Crisis support |
Pathways: availability of and linkages between non-acute and acute services, including helplines, youth-specific inpatient beds, youth subacute beds and discharge to outpatient and home-based supports |
||||||||||||||
Family engagement and support |
Type: family therapy, education and peer support |
||||||||||||||
Guideline-based care |
Decisions: use of decision-support and shared decision-making aids |
||||||||||||||
Holistic approach |
Functioning: support for accommodation, cognitive, education, employment, family and social needs |
||||||||||||||
Pre-emptive approach |
Prevention: universal, indicated or selected, as appropriate |
||||||||||||||
Youth peer support |
Format: group intervention delivery |
||||||||||||||
Capability |
|||||||||||||||
Appropriate financing |
Incentives: fee for service, salary or outcome-based |
||||||||||||||
Attuned, skilled and diverse staff |
Competences: evidence-based, developmentally informed and youth-friendly care |
||||||||||||||
Automated tools and processes |
Client-facing: automated assessment, referral and support |
||||||||||||||
Collaborative working |
Modality: co-location, information sharing, secondary consultation, shared records and systems, referral networks and partnerships |
||||||||||||||
Quality assurance |
Improvement: leadership and processes for continuous improvement |
||||||||||||||
Youth participation |
Depth: information gathering, consultation, partnership or user control |
||||||||||||||
Provenance: Commissioned; externally peer reviewed.
- Matthew P Hamilton1
- Sarah E Hetrick1,2
- Cathrine Mihalopoulos3
- David Baker1
- Vivienne Browne1,2
- Andrew M Chanen1,2
- Kerryn Pennell1
- Rosemary Purcell1,2
- Heather Stavely1
- Patrick D McGorry1,2
- 1 Orygen, The National Centre of Excellence in Youth Mental Health, Melbourne, VIC
- 2 Centre of Youth Mental Health, University of Melbourne, Melbourne, VIC
- 3 Deakin Health Economics, Deakin University, Melbourne, VIC
This study was funded by Orygen.
Patrick McGorry is the executive director of Orygen, the National Centre of Excellence in Youth Mental Health, which is the lead agency for four headspace centres; he is also a director of the board of headspace, the National Youth Mental Health Foundation.
- 1. Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol 2011; 21: 655-679.
- 2. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 2013; 382: 1575-1586.
- 3. Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry 2016; 3: 171-178.
- 4. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 2015; 72: 334-341.
- 5. Charlson FJ, Baxter AJ, Dua T, et al. Excess mortality from mental, neurological, and substance use disorders in the Global Burden of Disease Study 2010. In: Patel V, Chisholm D, Dua T, et al, editors. Mental, neurological, and substance use disorders: disease control priorities (volume 4). 3rd ed. Washington, DC: World Bank, 2015.
- 6. Schofield DJ, Shrestha RN, Percival R, et al. The personal and national costs of mental health conditions: impacts on income, taxes, government support payments due to lost labour force participation. BMC Psychiatry 2011; 11: 72.
- 7. Schofield DJ, Shrestha RN, Percival R, et al. Quantifying the effect of early retirement on the wealth of individuals with depression or other mental illness. Br J Psychiatry 2011; 198: 123-128.
- 8. Schofield DJ, Kelly SJ, Shrestha RN, et al. How depression and other mental health problems can affect future living standards of those out of the labour force. Aging Ment Health 2011; 15: 654-662.
- 9. Gatt L, Jan S, Mondraty N, et al. The household economic burden of eating disorders and adherence to treatment in Australia. BMC Psychiatry 2014; 14: 338.
- 10. Neil AL, Carr VJ, Mihalopoulos C, et al. Costs of psychosis in 2010: findings from the second Australian National Survey of Psychosis. Aust N Z J Psychiatry 2014; 48: 169-182.
- 11. Neil AL, Carr VJ, Mihalopoulos C, et al. What difference a decade? The costs of psychosis in Australia in 2000 and 2010: comparative results from the first and second Australian national surveys of psychosis. Aust N Z J Psychiatry 2014; 48: 237-248.
- 12. Wang PS, Simon G, Kessler RC. The economic burden of depression and the cost-effectiveness of treatment. Int J Methods Psychiatr Res 2003; 12: 22-33.
- 13. Manning M, Smith C, Mazerolle P. The societal costs of alcohol misuse in Australia. Trends & Issues in Crime and Criminal Justice 2013; (454). http://www.aic.gov.au/publications/current%20series/tandi/441-460/tandi454.html (accessed Oct 2017).
- 14. Bloom DE, Cafiero ET, Jané-Llopis E, et al. The global economic burden of non-communicable diseases. Geneva: World Economic Forum, 2011. http://apps.who.int/medicinedocs/en/d/Js18806en/ (accessed Oct 2017).
- 15. Mental Health Commission of Canada. Making the case for investment in mental health in Canada. Ottawa: MHCC, 2013. https://www.mentalhealthcommission.ca/English/media/3179 (accessed Oct 2017).
- 16. Chisholm D. Investing in mental health: evidence for action. Geneva: World Health Organization, 2013. http://www.who.int/mental_health/publications/financing/investing_in_mh_2013/en/ (accessed Oct 2017).
- 17. Chisholm D, Sweeny K, Sheehan P, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry 2016; 3: 415-424.
- 18. Sanderson K, Andrews G, Corry J, Lapsley H. Reducing the burden of affective disorders: is evidence-based health care affordable? J Affect Disord 2003; 77: 109-125.
- 19. Whiteford H, Ferrari A, Degenhardt L. Global burden of disease studies: implications for mental and substance use disorders. Health Aff (Millwood) 2016; 35: 1114-1120.
- 20. Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet 2007; 370: 878-889.
- 21. National Mental Health Commission. Contributing Lives, Thriving Communities – Report of the National Review of Mental Health Programmes and Services. Sydney: NMHC, 2014. http://www.mentalhealthcommission.gov.au/our-reports/contributing-lives,-thriving-communities-review-of-mental-health-programmes-and-services.aspx (accessed Oct 2017).
- 22. Runciman WB, Hunt TD, Hannaford NA, et al. CareTrack: assessing the appropriateness of health care delivery in Australia. Med J Aust 2012; 197: 100-105. <MJA full text>
- 23. Pirkis J, Harris M, Hall W, Ftanou M. Evaluation of the Better Access to Psychiatrists, Psychologists and General Practitioners through the Medicare Benefits Schedule Initiative: final report. Melbourne: Centre for Health Policy, Programs and Economics, University of Melbourne, 2011. http://www.health.gov.au/internet/main/publishing.nsf/content/mental-ba-eval-sum (accessed Oct 2017).
- 24. Roxon N, Macklin J, Butler M. Budget: national mental health reform [ministerial statement]. Canberra: Australian Government Department of Health, 2011.
- 25. Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet 2007; 369: 1302-1313.
- 26. Kessler RC, Amminger GP, Aguilar-Gaxiola S, et al. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 2007; 20: 359-364.
- 27. Gibb SJ, Fergusson DM, Horwood LJ. Burden of psychiatric disorder in young adulthood and life outcomes at age 30. Br J Psychiatry 2010; 197: 122-127.
- 28. Leach LS, Butterworth P. The effect of early onset common mental disorders on educational attainment in Australia. Psychiatry Res 2012; 199: 51-57.
- 29. Knapp M, Snell T, Healey A, et al. How do child and adolescent mental health problems influence public sector costs? Interindividual variations in a nationally representative British sample. J Child Psychol Psychiatry 2015; 56: 667-676.
- 30. Hetrick SE, Bailey AP, Smith KE, et al. Integrated (one-stop shop) youth health care: best available evidence and future directions. Med J Aust 2017; 207 (10 Suppl): S5-S18.
- 31. Australian Government Department of Health. Australian Government response to Contributing Lives, Thriving Communities – Review of Mental Health Programmes and Services. Canberra: Department of Health, 2016. http://www.health.gov.au/internet/main/publishing.nsf/content/mental-review-response (accessed Oct 2017).
- 32. Australian Government Department of Health. PHN primary mental health care flexible funding pool implementation guidance: stepped care. Canberra: Department of Health, 2016. http://www.health.gov.au/internet/main/publishing.nsf/content/phn-mental_tools (accessed Oct 2017).
- 33. Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press, 2005.
- 34. Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA 2016; 316: 1093-1103.
- 35. Stavely H, Hughes F, Pennell K, et al. EPPIC model & service implementation guide. Mebourne: Orygen Youth Health Research Centre, 2013.
- 36. Cocchi A, Mapelli V, Meneghelli A, Preti A. Cost-effectiveness of treating first-episode psychosis: five-year follow-up results from an Italian early intervention programme. Early Interv Psychiatry 2011; 5: 203-211.
- 37. Goldberg K, Norman R, Hoch JS, et al. Impact of a specialized early intervention service for psychotic disorders on patient characteristics, service use, and hospital costs in a defined catchment area. Can J Psychiatry 2006; 51: 9.
- 38. Hastrup LH, Kronborg C, Bertelsen M, et al. Cost-effectiveness of early intervention in first-episode psychosis: economic evaluation of a randomised controlled trial (the OPUS study). Br J Psychiatry 2013; 202: 35-41.
- 39. McCrone P, Craig TK, Power P, Garety PA. Cost-effectiveness of an early intervention service for people with psychosis. Br J Psychiatry 2010; 196: 377-382.
- 40. Mihalopolous C, McGorry PD, Carter RC. Is phase-specific, community-oriented treatment of early psychosis an economically viable method of improving outcome? Acta Psychiatr Scand 1999; 100: 47-55.
- 41. Mihalopoulos C, Harris M, Henry L, et al. Is early intervention in psychosis cost-effective over the long term? Schizophr Bull 2009; 35: 909-918.
- 42. Rosenheck R, Leslie D, Sint K, et al. Cost-effectiveness of comprehensive, integrated care for first episode psychosis in the NIMH RAISE Early Treatment Program. Schizophr Bull 2016; 42: 896-906.
- 43. Tsiachristas A, Thomas T, Leal J, Lennox BR. Economic impact of early intervention in psychosis services: results from a longitudinal retrospective controlled study in England. BMJ Open 2016; 6: e012611.
- 44. Wong KK, Chan SK, Lam MM, et al. Cost-effectiveness of an early assessment service for young people with early psychosis in Hong Kong. Aust N Z J Psychiatry 2011; 45: 673-680.
- 45. Cullberg J, Mattsson M, Levander S, et al. Treatment costs and clinical outcome for first episode schizophrenia patients: a 3-year follow-up of the Swedish “Parachute Project” and two comparison groups. Acta Psychiatr Scand 2006; 114: 274-281.
- 46. Ising HK, Smit F, Veling W, et al. Cost-effectiveness of preventing first-episode psychosis in ultra-high-risk subjects: multi-centre randomized controlled trial. Psychol Med 2015; 45: 1435-1446.
- 47. Mihalopoulos C, Vos T, Pirkis J, Carter R. The economic analysis of prevention in mental health programs. Annu Rev Clin Psychol 2011; 7: 169-201.
- 48. Barton GR, Hodgekins J, Mugford M, et al. Cognitive behaviour therapy for improving social recovery in psychosis: cost-effectiveness analysis. Schizophr Res 2009; 112: 158-163.
- 49. Perez J, Jin HJ, Russo DA, et al. Clinical effectiveness and cost-effectiveness of tailored intensive liaison between primary and secondary care to identify individuals at risk of a first psychotic illness (the LEGs study): a cluster-randomised controlled trial. Lancet Psychiatry 2015; 2: 984-993.
- 50. Gray D, Dawson KL, Grey TC, McMahon WM. The Utah Youth Suicide Study: best practices for suicide prevention through the juvenile court system. Psychiatr Serv 2011; 62: 1416-1418.
- 51. Latimer EA, Gariépy G, Greenfield B. Cost-effectiveness of a rapid response team intervention for suicidal youth presenting at an emergency department. Can J Psychiatry 2014; 59: 310-318.
- 52. Le LK, Barendregt JJ, Hay P, et al. The modelled cost-effectiveness of cognitive dissonance for the prevention of anorexia nervosa and bulimia nervosa in adolescent girls in Australia. Int J Eat Disord 2017; 50: 834-841.
- 53. Mihalopoulos C, Vos T, Pirkis J, Carter R. The population cost-effectiveness of interventions designed to prevent childhood depression. Pediatrics 2012; 129: e723-e730.
- 54. Neighbours CJ, Barnett NP, Rohsenow DJ, et al. Cost-effectiveness of a motivational intervention for alcohol-involved youth in a hospital emergency department. J Stud Alcohol Drugs 2010; 71: 384-394.
- 55. Richardson R, Trepel D, Perry A, et al. Screening for psychological and mental health difficulties in young people who offend: a systematic review and decision model. Health Technol Assess 2015; 19(1): 1-128.
- 56. Wright DR, Austin SB, LeAnn Noh H, et al. The cost-effectiveness of school-based eating disorder screening. Am J Public Health 2014; 104: 1774-1782.
- 57. Zaloshnja E, Miller TR, Galbraith MS, et al. Reducing injuries among Native Americans: five cost-outcome analyses. Accid Anal Prev 2003; 35: 631-639.
- 58. Philipsson A, Duberg A, Moller M, Hagberg L. Cost-utility analysis of a dance intervention for adolescent girls with internalizing problems. Cost Eff Resour Alloc 2013; 11: 4.
- 59. Wang LY, Nichols LP, Austin SB. The economic effect of Planet Health on preventing bulimia nervosa. Arch Pediatr Adolesc Med 2011; 165: 756-762.
- 60. Guyll M, Spoth R, Crowley DM. Economic analysis of methamphetamine prevention effects and employer costs. J Stud Alcohol Drugs 2011; 72: 577-585.
- 61. Anderson R, Ukoumunne OC, Sayal K, et al. Cost-effectiveness of classroom-based cognitive behaviour therapy in reducing symptoms of depression in adolescents: a trial-based analysis. J Child Psychol Psychiatry 2014; 55: 1390-1397.
- 62. Stallard P, Phillips R, Montgomery AA, et al. A cluster randomised controlled trial to determine the clinical effectiveness and cost-effectiveness of classroom-based cognitive-behavioural therapy (CBT) in reducing symptoms of depression in high-risk adolescents. Health Technol Assess 2013; 17(47): 1-109.
- 63. Lee YY, Barendregt JJ, Stockings EA, et al. The population cost-effectiveness of delivering universal and indicated school-based interventions to prevent the onset of major depression among youth in Australia. Epidemiol Psychiatr Sci 2017; 26: 545-564.
- 64. Byford S, Harrington R, Torgerson D, et al. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry 1999; 174: 56-62.
- 65. Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat 2004; 27: 197-213.
- 66. Godley SH, Garner BR, Passetti LL, et al. Adolescent outpatient treatment and continuing care: main findings from a randomized clinical trial. Drug Alcohol Depend 2010; 110: 44-54.
- 67. Sheidow AJ, Bradford WD, Henggeler SW, et al. Treatment costs for youths receiving multisystemic therapy or hospitalization after a psychiatric crisis. Psychiatr Serv 2004; 55: 548-554.
- 68. Bodden DH, Dirksen CD, Bogels SM, et al. Costs and cost-effectiveness of family CBT versus individual CBT in clinically anxious children. Clin Child Psychol Psychiatry 2008; 13: 543-564.
- 69. Schmidt U, Lee S, Beecham J, et al. A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders. Am J Psychiatry 2007; 164: 591-598.
- 70. Lynch FL, Hornbrook M, Clarke GN, et al. Cost-effectiveness of an intervention to prevent depression in at-risk teens. Arch Gen Psychiatry 2005; 62: 1241-1248.
- 71. Sari N, de Castro S, Newman F, Mills G. Should we invest in suicide prevention programs? J Socio Econ 2008; 37: 262-275.
- 72. King RD, Gaines LS, Lambert EW, et al. The co-occurrence of psychiatric and substance use diagnoses in adolescents in different service systems: frequency, recognition, cost, and outcomes. J Behav Health Serv Res 2000; 27: 417-430.
- 73. Ingels JB, Corso PS, Kogan SM, Brody GH. Cost-effectiveness of the strong African American families-teen program: 1-year follow-up. Drug Alcohol Depend 2013; 133: 556-561.
- 74. Agras WS, Lock J, Brandt H, et al. Comparison of 2 family therapies for adolescent anorexia nervosa: a randomized parallel trial. JAMA Psychiatry 2014; 71: 1279-1286.
- 75. Byford S, Barrett B, Roberts C, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. Br J Psychiatry 2007; 191: 436-440.
- 76. Bertelsen M, Jeppesen P, Petersen L, et al. Five-year follow-up of a randomized multicenter trial of intensive early intervention vs standard treatment for patients with a first episode of psychotic illness: the OPUS trial. Arch Gen Psychiatry 2008; 65: 762-771.
- 77. Catalano R, Libby A, Snowden L, Cuellar AE. The effect of capitated financing on mental health services for children and youth: the Colorado experience. Am J Public Health 2000; 90: 1861-1865.
- 78. Chatterji P, Caffray CM, Crowe M, et al. Cost assessment of a school-based mental health screening and treatment program in New York City. Ment Health Serv Res 2004; 6: 155-166.
- 79. Grimes KE, Schulz MF, Cohen SA, et al. Pursuing cost-effectiveness in mental health service delivery for youth with complex needs. J Ment Health Policy Econ 2011; 14: 73-83.
- 80. Kanuri N, Taylor CB, Cohen JM, Newman MG. Classification models for subthreshold generalized anxiety disorder in a college population: Implications for prevention. J Anxiety Disord 2015; 34: 43-52.
- 81. Larsen TK, Melle I, Auestad B, et al. Early detection of psychosis: positive effects on 5-year outcome. Psychol Med 2011; 41: 1461-1469.
- 82. Lock J, Couturier J, Agras WS. Costs of remission and recovery using family therapy for adolescent anorexia nervosa: a descriptive report. Eat Disord 2008; 16: 322-330.
- 83. Marzola E, Knatz S, Murray SB, et al. Short-term intensive family therapy for adolescent eating disorders: 30-month outcome. Eur Eat Disord Rev 2015; 23: 210-218.
- 84. McCrone P, Singh SP, Knapp M, et al. The economic impact of early intervention in psychosis services for children and adolescents. Early Interv Psychiatry 2013; 7: 368-373.
- 85. Park AL, McCrone P, Knapp M. Early intervention for first-episode psychosis: broadening the scope of economic estimates. Early Interv Psychiatry 2016; 10: 144-151.
- 86. Phillips LJ, Cotton S, Mihalopoulos C, et al. Cost implications of specific and non-specific treatment for young persons at ultra high risk of developing a first episode of psychosis. Early Interv Psychiatry 2009; 3: 28-34.
- 87. Serretti A, Mandelli L, Bajo E, et al. The socio-economical burden of schizophrenia: a simulation of cost-offset of early intervention program in Italy. Eur Psychiatry 2009; 24: 11-16.
- 88. Valmaggia LR, McCrone P, Knapp M, et al. Economic impact of early intervention in people at high risk of psychosis. Psychol Med 2009; 39: 1617-1626.
- 89. Wellander L, Wells MB, Feldman I. Does prevention pay? Costs and potential cost-savings of school interventions targeting children with mental health problems. J Ment Health Policy Econ 2016; 19: 91-102.
- 90. Brimblecombe N, Knapp M, Murguia S, et al. The role of youth mental health services in the treatment of young people with serious mental illness: 2-year outcomes and economic implications. Early Interv Psychiatry 2017; 11: 393-400.
- 91. Green J, Jacobs B, Beecham J, et al. Inpatient treatment in child and adolescent psychiatry–a prospective study of health gain and costs. J Child Psychol Psychiatry 2007; 48: 1259-1267.
- 92. Franzini L, Marks E, Cromwell PF, et al. Projected economic costs due to health consequences of teenagers’ loss of confidentiality in obtaining reproductive health care services in Texas. Arch Pediatr Adolesc Med 2004; 158: 1140-1146.
- 93. Moodie ML, Fisher J. Are youth mentoring programs good value-for-money? An evaluation of the Big Brothers Big Sisters Melbourne Program. BMC Public Health 2009; 9: 41.
- 94. Adams M, Kutcher S, Antoniw E, Bird D. Diagnostic utility of endocrine and neuroimaging screening tests in first-onset adolescent psychosis. J Am Acad Child Adolesc Psychiatry 1996; 35: 67-73.
- 95. Armstrong B. Financing mental health services for youth: problems and possibilities. Hosp Community Psychiatry 1978; 29: 191-194.
- 96. Bickman L. A continuum of care: more is not always better. Am Psychol 1996; 51: 13-21.
- 97. Rund BR, Moe L, Sollien T, et al. The Psychosis Project: outcome and cost-effectiveness of a psychoeducational treatment programme for schizophrenic adolescents. Acta Psychiatr Scand 1994; 89: 211-218.
- 98. Byford S, Barrett B, Roberts C, et al. Cost-effectiveness of selective serotonin reuptake inhibitors and routine specialist care with and without cognitive behavioural therapy in adolescents with major depression. Br J Psychiatry 2007; 191: 521-527.
- 99. Domino ME, Burns BJ, Silva SG, et al. Cost-effectiveness of treatments for adolescent depression: results from TADS. Am J Psychiatry 2008; 165: 588-596.
- 100. Domino ME, Foster EM, Vitiello B, et al. Relative cost-effectiveness of treatments for adolescent depression: 36-week results from the TADS randomized trial. J Am Acad Child Adolesc Psychiatry 2009; 48: 711-720.
- 101. Erder MH, Xie J, Signorovitch JE, et al. Cost effectiveness of guanfacine extended-release versus atomoxetine for the treatment of attention-deficit/hyperactivity disorder: application of a matching-adjusted indirect comparison. Appl Health Econ Health Policy 2012; 10: 381-395.
- 102. Faber A, van Agthoven M, Kalverdijk LJ, et al. Long-acting methylphenidate-OROS in youths with attention-deficit hyperactivity disorder suboptimally controlled with immediate-release methylphenidate: a study of cost effectiveness in the Netherlands. CNS Drugs 2008; 22: 157-170.
- 103. French MT, Zavala SK, McCollister KE, et al. Cost-effectiveness analysis of four interventions for adolescents with a substance use disorder. J Subst Abuse Treat 2008; 34: 272-281.
- 104. Gowers SG, Clark AF, Roberts C, et al. A randomised controlled multicentre trial of treatments for adolescent anorexia nervosa including assessment of cost-effectiveness and patient acceptability - the TOuCAN trial. Health Technol Assess 2010; 14(15): 1-98.
- 105. Green JM, Wood AJ, Kerfoot MJ, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ 2011; 342: d682.
- 106. Haby MM, Tonge B, Littlefield L, et al. Cost-effectiveness of cognitive behavioural therapy and selective serotonin reuptake inhibitors for major depression in children and adolescents. Aust N Z J Psychiatry 2004; 38: 579-591.
- 107. Kutcher S, Robertson HA. Electroconvulsive therapy in treatment-resistant bipolar youth. J Child Adolesc Psychopharmacol 1995; 5: 167-175.
- 108. Lachaine J, De G, Sikirica V, et al. Treatment patterns, resource use, and economic outcomes associated with atypical antipsychotic prescriptions in children and adolescents with attention-deficit hyperactivity disorder in Quebec. Can J Psychiatry 2014; 59: 597-608.
- 109. Lynch FL, Dickerson JF, Clarke G, et al. Incremental cost-effectiveness of combined therapy vs medication only for youth with selective serotonin reuptake inhibitor-resistant depression: treatment of SSRI-resistant depression in adolescents trial findings. Arch Gen Psychiatry 2011; 68: 253-262.
- 110. Olmstead TA, Sindelar JL, Easton CJ, Carroll KM. The cost-effectiveness of four treatments for marijuana dependence. Addiction 2007; 102: 1443-1453.
- 111. Polsky D, Glick HA, Yang J, et al. Cost-effectiveness of extended buprenorphine-naloxone treatment for opioid-dependent youth: data from a randomized trial. Addiction 2010; 105: 1616-1624.
- 112. Prasad S, Arellano J, Steer C, Libretto SE. Assessing the value of atomoxetine in treating children and adolescents with ADHD in the UK. Int J Clin Pract 2009; 63: 1031-1040.
- 113. Sikirica V, Haim Erder M, Xie J, et al. Cost effectiveness of guanfacine extended release as an adjunctive therapy to a stimulant compared with stimulant monotherapy for the treatment of attention-deficit hyperactivity disorder in children and adolescents. Pharmacoeconomics 2012; 30(8): e1-e15.
- 114. Stikkelbroek Y, Bodden DH, Dekovic M, van Baar AL. Effectiveness and cost effectiveness of cognitive behavioral therapy (CBT) in clinically depressed adolescents: individual CBT versus treatment as usual (TAU). BMC Psychiatry 2013; 13: 314.
- 115. Yu AP, Ben-Hamadi R, Wu EQ, et al. Impact of initiation timing of SSRI or SNRI on depressed adolescent healthcare utilization and costs. J Med Econ 2011; 14: 508-515.
- 116. Amos A. Assessing the cost of early intervention in psychosis: a systematic review. Aust N Z J Psychiatry 2012; 46: 719-734.
- 117. Bee P, Bower P, Byford S, et al. The clinical effectiveness, cost-effectiveness and acceptability of community-based interventions aimed at improving or maintaining quality of life in children of parents with serious mental illness: a systematic review. Health Technol Assess 2014; 18(8): 1-250.
- 118. Beecham J. Annual research review: child and adolescent mental health interventions: a review of progress in economic studies across different disorders. J Child Psychol Psychiatry 2014; 55: 714-732.
- 119. Kilian R, Losert C, Park AL, et al. Cost-effectiveness analysis in child and adolescent mental health problems: an updated review of literature. Int J Ment Health Promot 2010; 12(4): 45-57.
- 120. Knapp M, Ardino V, Brimblecombe N, et al. Youth mental health: new economic evidence. London: Personal Social Services Research Unit, London School of Economics and Political Science, 2016. http://www.pssru.ac.uk/publications/pub-5160/ (accessed Oct 2017).
- 121. Lee S, Aos S, Pennucci A. What works and what does not? Benefit–cost findings from WSIPP. Olympia, Wash: Washington State Institute for Public Policy, 2015. http://www.wsipp.wa.gov/Reports/562 (accessed Oct 2017).
- 122. Knapp M. Economic evaluations for children and adolescents with mental health problems. J Child Psychol Psychiatry 1997; 38: 3-25.
- 123. Mihalopoulos C, Chatterton ML. Economic evaluations of interventions designed to prevent mental disorders: a systematic review. Early Interv Psychiatry 2015; 9: 85-92.
- 124. Mihalopoulos C, McCrone P, Knapp M, et al. The costs of early intervention in psychosis: restoring the balance. Aust N Z J Psychiatry 2012; 46: 808-811.
- 125. Romeo R, Byford S, Knapp M. Annotation: economic evaluations of child and adolescent mental health interventions: a systematic review. J Child Psychol Psychiatry 2005; 46: 919-930.
- 126. Zechmeister I, Kilian R, McDaid D; MHEEN group. Is it worth investing in mental health promotion and prevention of mental illness? A systematic review of the evidence from economic evaluations. BMC Public Health 2008; 8: 20.
- 127. Hilferty F, Cassells R, Muir K, et al. Is headspace making a difference to young people’s lives? Final report of the independent evaluation of the headspace program. Sydney: Social Policy Research Centre, University of New South Wales, 2015. https://www.headspace.org.au/assets/Uploads/Evaluation-of-headspace-program.pdf (accessed Oct 2017).
- 128. McDaid D, Park AL, Iemmi V, et al. Growth in the use of early intervention for psychosis services: an opportunity to promote recovery amid concerns on health care sustainability. London: Personal Social Services Research Unit, London School of Economics and Political Science, 2016. http://www.pssru.ac.uk/archive/pdf/5164.pdf (accessed Oct 2017).
- 129. PricewaterhouseCoopers. Youth mental health project: cost-benefit analysis. Wellington: Social Policy Evaluation and Research Unit (Superu), 2016. http://www.superu.govt.nz/publication/ymh_cost_benefit_analysis_2016 (accessed Oct 2017).
- 130. Burns ME, Wolfe BL. The effects of the Affordable Care Act adult dependent coverage expansion on mental health. J Ment Health Policy Econ 2016; 19: 3-20.
- 131. Ambresin AE, Bennett K, Patton GC, et al. assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health 2013; 52: 670-681.
- 132. Becker MP, Christensen BK, Cunningham CE, et al. Preferences for early intervention mental health services: a discrete-choice conjoint experiment. Psychiatr Serv 2016; 67: 184-191.
- 133. Boyd CP, Hayes L, Nurse S, et al. Preferences and intention of rural adolescents toward seeking help for mental health problems. Rural Remote Health 2011; 11: 1582.
- 134. Bradford S, Rickwood D. Adolescent’s preferred modes of delivery for mental health services. Child Adolesc Ment Health 2014; 19: 39-45.
- 135. Cunningham CE, Chen Y, Deal K, et al. The interim service preferences of parents waiting for children’s mental health treatment: a discrete choice conjoint experiment. J Abnorm Child Psychol 2013; 41: 865-877.
- 136. Cunningham CE, Niccols A, Rimas H, et al. Using a discrete choice conjoint experiment to engage stakeholders in the design of an outpatient children’s health center. HERD 2017; Jan 10. https://doi.org/10.1177/1937586716686350 [Epub ahead of print].
- 137. Cunningham CE, Walker JR, Eastwood JD, et al. Modeling mental health information preferences during the early adult years: a discrete choice conjoint experiment. J Health Commun 2014; 19: 413-440.
- 138. Cunningham CE, Zipursky RB, Christensen BK, et al. Modeling the mental health service utilization decisions of university undergraduates: a discrete choice conjoint experiment. J Am Coll Health 2017; May 16. https://doi.org/10.1080/07448481.2017.1322090 [Epub ahead of print].
- 139. Hyman SI, Manion I, Davidson S, Brandon S. ‘Youth-friendly’ characteristics of professionals in mental health settings. Vulnerable Child Youth Stud 2007; 2: 261-272.
- 140. Watsford C, Rickwood D. What do young people seeking professional help want and expect from therapy? World Acad Sci Eng Technol 2012; 6: 1146-1150.
- 141. Watsford C, Rickwood D. Young people’s expectations, preferences and actual experience of youth mental health care. Int J Adolesc Youth 2015; 20: 284-294.
- 142. Hadorn DC. The role of public values in setting health care priorities. Soc Sci Med 1991; 32: 773-781.
- 143. Wiseman V, Mooney G, Berry G, Tang KC. Involving the general public in priority setting: experiences from Australia. Soc Sci Med 2003; 56: 1001-1012.
- 144. Dolan P. Whose preferences count? Med Decis Making 1999; 19: 482-486.
- 145. Woodhouse A. Right here: how to … commission better mental health and wellbeing services for young people. London: Paul Hamlyn Foundation and the Mental Health Foundation, 2014. http://www.phf.org.uk/publications/commission-better-mental-health-wellbeing-services-young-people/ (accessed Oct 2017).
- 146. Anderson JE, Lowen CA. Connecting youth with health services: systematic review. Can Fam Physician 2010; 56: 778-784.
- 147. World Health Organization. Quality assessment guidebook: a guide to assessing health services for adolescent clients. Geneva: WHO, 2009. http://www.who.int/maternal_child_adolescent/documents/fch_cah_9789241598859/en/ (accessed Oct 2017).
- 148. Semigran HL, Linder JA, Gidengil C, Mehrotra A. Evaluation of symptom checkers for self diagnosis and triage: audit study. BMJ 2015; 351: h3480.
- 149. Keefe RS, Davis VG, Atkins AS, et al. Validation of a computerized test of functional capacity. Schizophr Res 2016; 175: 90-96.
- 150. Wickramasinghe LK, Schattner P, Hibbert ME, et al. Impact on diabetes management of General Practice Management Plans, Team Care Arrangements and reviews. Med J Aust 2013; 199: 261-265. <MJA full text>
- 151. Curran GM, Sullivan G, Mendel P, et al. Implementation of the CALM intervention for anxiety disorders: a qualitative study. Implement Sci 2012; 7: 1-11.
- 152. Gustafson DH, Quanbeck AR, Robinson JM, et al. Which elements of improvement collaboratives are most effective? A cluster-randomized trial. Addiction 2013; 108: 1145-1157.
- 153. Montague AE, Varcin KJ, Parker A. Putting technology into practice: evidence and opinions on integrating technology with youth health services. Melbourne: Young and Well Cooperative Research Centre, 2014.
- 154. Alegria A, Frank R, McGuire T. Managed care and systems cost-effectiveness: treatment for depression. Med Care 2005; 43: 1225-1233.
- 155. Konig HH, Born A, Heider D, et al. Cost-effectiveness of a primary care model for anxiety disorders. Br J Psychiatry 2009; 195: 308-317.
- 156. Gustaffson-Wright E, Gardiner S, Putcha V. The potential and limitations of impact bonds: lessons from the first five years of experience worldwide. Washington, DC: Brookings, 2015. https://www.brookings.edu/research/the-potential-and-limitations-of-impact-bonds-lessons-from-the-first-five-years-of-experience-worldwide/ (accessed Oct 2017).
- 157. Davies R. Social impact bonds: private finance that generates social returns [briefing]. Brussels: European Parliamentary Research Service, 2014. http://www.europarl.europa.eu/thinktank/en/document.html?reference=EPRS_BRI(2014)538223 (accessed Oct 2017).
- 158. Ham C. World class commissioning: a health policy chimera? J Health Serv Res Policy 2008; 13: 116-121.
- 159. Orygen. Commissioning and youth mental health: addressing an undertreated health issue. Melbourne: Orygen, 2016. https://www.orygen.org.au/Policy-Advocacy/Policy-Reports/Commissioning-and-YouthMH (accessed Oct 2017).
- 160. Australian Government Department of Health. Fifth National Mental Health Plan: draft for consultation. Canberra: Department of Health, 2016. http://www.health.gov.au/internet/main/publishing.nsf/content/mental-fifth-national-mental-health-plan (accessed Oct 2017).
- 161. Marshall DA, Burgos-Liz L, IJzerman MJ, et al. Selecting a dynamic simulation modeling method for health care delivery research-part 2: report of the ISPOR Dynamic Simulation Modeling Emerging Good Practices Task Force. Value Health 2015; 18: 147-160.
- 162. Marshall DA, Burgos-Liz L, IJzerman MJ, et al. Applying dynamic simulation modeling methods in health care delivery research-the SIMULATE checklist: report of the ISPOR simulation modeling emerging good practices task force. Value Health 2015; 18: 5-16.





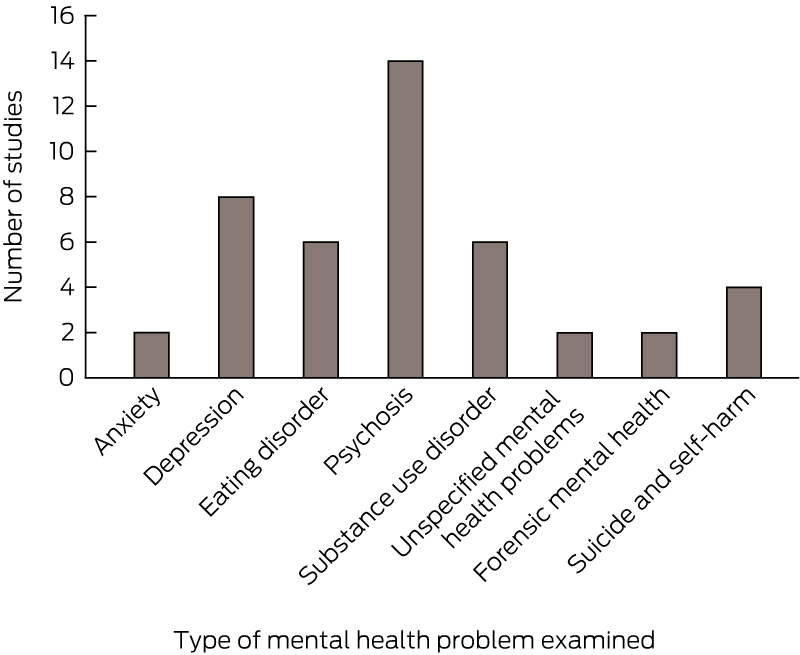
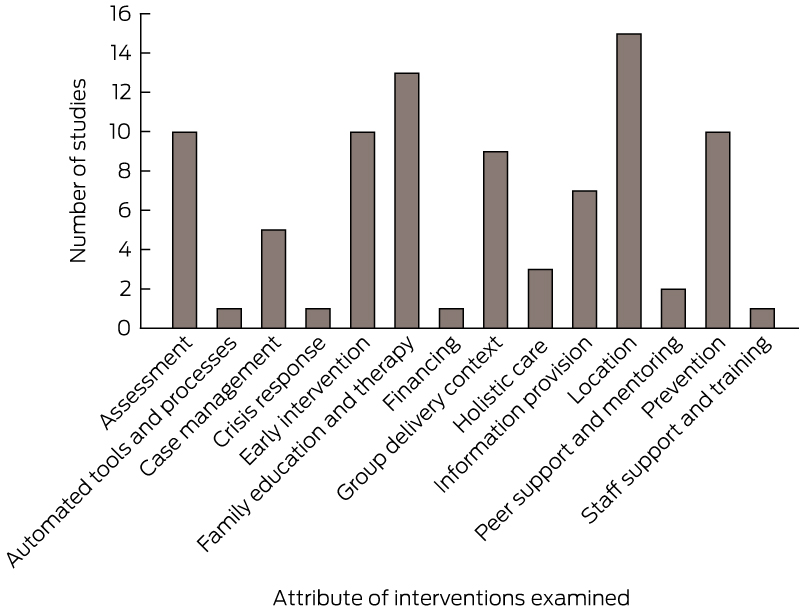
Abstract
Objective: To identify attributes of youth mental health care for which there is evidence of potential cost-effectiveness.
Study design: We performed a literature review of economic evaluations that examined both costs and outcomes for attributes of youth mental health care other than pharmacological or individual psychological therapies for full-threshold disorders.
Data sources: We searched the United Kingdom National Health Service Economic Evaluations Database for evaluations published to the end of 2014; and MEDLINE, Google Scholar and the citation lists of relevant publications for peer-reviewed studies published in English since 1997.
Data synthesis: Forty economic evaluations met inclusion criteria. Psychosis was the mental disorder with the most developed economic evidence base, with good evidence of cost-effectiveness for first-episode psychosis services. There was a developing cost-effectiveness evidence base for other disorders. The most common attributes of the interventions examined in the included studies were the location of services, engagement and support of families, assessment, prevention, early intervention, group delivery format and information provision. We used our findings to formulate a list of attributes of youth mental health care that may be acceptable to young people and potentially cost-effective.
Conclusion: There is at least suggestive cost-effectiveness evidence for a range of attributes of youth mental health care. Further economic research is needed to substantiate most cost-effectiveness findings and to improve targeting of care among young people. Future economic evaluations should examine costs from both societal and health care perspectives and incorporate evidence regarding young people’s preferences.