The known For decades, the Heart Foundation has used mass media interventions to improve community awareness of the warning signs of heart attacks. Whether these interventions improve ambulance use by patients with chest pain was unknown.
The new A comprehensive public awareness campaign about responding to acute myocardial infarction symptoms was associated with a 10.7% increase in monthly emergency medical service attendances for people with chest pain, and an 11.3% increase in attendances for suspected acute coronary syndromes, as determined by paramedics.
The implications Mass media interventions may be effective in influencing appropriate health-seeking behaviour in response to chest pain symptoms.
Acute myocardial infarction (AMI) is a leading cause of premature death in developed countries.1 Early mortality from AMI is usually the result of a lethal arrhythmia, which typically occurs before medical contact, but after the onset of prodromal symptoms such as chest pain.2 Delays in seeking medical attention after prodromal symptoms begin is also a key barrier to the success of contemporary reperfusion therapies for AMI.3,4 Early access to emergency medical services (EMS) is crucial for patients with AMI, and is associated with reduced time to receiving reperfusion therapy and more effective treatment of cardiac arrest.5,6 Despite this, access to EMS varies considerably across developed countries, and as many as half of all AMI patients use methods of transport other than an ambulance to reach hospital.5
Since the early 1980s, there has been considerable interest in mass media interventions for educating the community about the importance of seeking EMS care soon after the onset of AMI prodromal symptoms.7 The results of studies of their effectiveness for improving EMS use by people with suspected AMI symptoms are inconsistent, but most reports indicate that they are not beneficial.8-16 Many studies, however, were limited by unadjusted before-and-after designs and the absence of contemporary media components, including television and digital media.17 In Australia, heart attack awareness campaigns since 1975 have been short in duration, have involved little mass media exposure, and were of limited effectiveness in improving health-seeking behaviour.18
In 2009, the National Heart Foundation of Australia (the Heart Foundation) launched a nationwide mass media campaign for educating the community about the importance of early EMS activation after the onset of AMI symptoms. The campaign, first introduced in Melbourne, ran intermittently until August 2013, and consisted of a 23-month intervention focused on television and digital media activity.19 In this study, we assessed the impact of this public education campaign on EMS use by people with non-traumatic chest pain.
Methods
Study design
We performed a time series analysis of the number of EMS attendances in Melbourne each month between 1 January 2008 and 31 December 2013. We included all patients with an emergency ambulance response for non-traumatic chest pain identified at the time of the emergency call.
Setting
Melbourne has a population of about 4.0 million people over an area of 9990 km2. Melbourne has a two-tiered EMS system, employing about 1800 advanced life support paramedics and 400 intensive care paramedics equipped with 12-lead electrocardiographs. In-field decisions are guided by medically approved clinical practice guidelines, although transport decisions are made autonomously by paramedics in the field after assessing the patient. During 2012–13, the Victorian EMS responded to almost 370 000 emergency incidents in the Melbourne region, an average of more than 1000 each day. EMS dispatch protocols are determined by the Medical Priority Dispatch System (MPDS), which is widely used by EMS agencies across the world. Major medical symptoms are categorised by the MPDS using a structured electronic call-taking algorithm that standardises priority dispatching. Emergency calls are classified according to more than 30 major medical presentations, including non-traumatic chest pain (MPDS Card 10). Emergency call-takers are trained to treat non-traumatic chest pain and other potential angina symptoms (eg, neck, jaw or arm pain) as ischaemic heart disease equivalents. Non-traumatic chest pain symptoms are the leading cause of EMS use in Melbourne, accounting for about 15% of the emergency caseload.
Data sources
Electronic computer-aided dispatch (CAD) records identified emergency cases with chest pain as the chief symptom. Because the chief symptom can change during the emergency call, we included cases in which the final classification met the inclusion criteria. In-field treatment data for patients attended by an EMS are recorded by paramedics using tablet computers that are later synchronised with an integrated electronic data warehouse.20 In addition to collecting CAD data, we extracted information from in-field treatment data for all ambulance attendances, including age, sex, pre-existing conditions, and the principal pre-hospital assessment or diagnosis made by paramedics. A pre-existing history of ischaemic heart disease was present if any of the following conditions or procedures were documented: angina, AMI, angioplasty, coronary artery bypass grafting surgery or cardiac arrest.
Mass media intervention
A detailed description of the Heart Foundation’s Warning signs of heart attack campaign is included in the online Appendix, and has also been described elsewhere.21 Briefly, the campaign used a multi-faceted media strategy, including television, radio, newspaper and social media components. A dedicated “Warning Signs” website and social media page were also central components of the campaign, and allowed people to interactively learn the warning signs of a heart attack and to download an “action plan” that advised patients about what to do when experiencing possible AMI prodromal symptoms (Figure S1 in the Appendix).19 The campaign aimed to improve community awareness of the prodromal symptoms associated with AMI, but also addressed several barriers to taking immediate action, including the risks associated with ignoring symptoms and the perception that symptoms are not serious enough to warrant calling an ambulance.
Between 11 October 2009 and 3 August 2013, a total of 294 campaign days were delivered across Melbourne (Table S1 in the Appendix). Media purchasing was based on target audience rating points (TARPS), which quantify the proportion of the target audience likely to be exposed to the campaign. The primary target audience comprised men and women aged 45–64 years.
Statistical analysis
Statistical analyses were undertaken in Stata 14 (StataCorp). We compared the baseline characteristics and pre-hospital assessments of patients on campaign and non-campaign days in χ2 and Mann–Whitney U tests as appropriate. P < 0.05 (two-sided) was deemed statistically significant.
Incidence rate ratios (IRRs) for the effect of campaign activity on the monthly volume of ambulance attendances were calculated by negative binomial regression. We specified a time variable in the model that adjusted for the long term trend and population growth, and a categorical variable (annual seasons) was also included. A term correcting for differences in month length was generated by dividing the number of days in each month by 28. Auto-correlation of error terms was corrected by calculating Newey–West standard errors, and the augmented Dickey–Fuller test verified a stationary time series.22 Finite lags of the exposure variable were also explored to identify residual effects in the months after the end of the campaign. A total of six lag months were tested, but no significant lag effects were identified beyond the second lag month. Campaign effects are described as either immediate effects — observed during the month of campaign activity — or as cumulative effects — the sum of the effects observed during the month of campaign activity and two lag months.
Because each campaign varied in duration, the media used, TARPS and calendar year, we tested these characteristics as alternative exposure variables in our models. Stratified analyses across age groups, sex, pre-existing conditions, and pre-hospital assessments were performed to identify the impact of campaign activity in key patient populations.
To depict changes in trend over time we used locally weighted scatterplot smoothing of the monthly number of ambulance attendances for chest pain after adjusting for the underlying trend and seasonal effects. To elucidate the long term influence of campaign activity on ambulance use, we segmented our exposure variable about a key change point, October 2009, the commencement of campaign activity. The level of and trend in ambulance use in the pre-campaign period (January 2008 – September 2009) was compared with that for the intervention period (October 2009 – December 2013) by methods described elsewhere.23 The advantage of this analysis was that it allowed comparison of the entire intervention period with an historical control, while allowing for adjustments for temporal trend and seasonal effects.
Ethics approval
The study was approved by the Monash University Human Research Ethics Committee (reference, CF12/2778).
Results
Baseline characteristics
Between January 2008 and December 2013, there were a total of 253 428 EMS attendances for non-traumatic chest pain. The median number of monthly attendances was 3609 (interquartile range, 3011–3891), and there were more attendances in months with campaign activity than in those without (3880 v 3234; P < 0.001). Box 1 summarises the baseline characteristics of patients on campaign and non-campaign days.
Effect of campaign activity on ambulance use
IRRs for the immediate and cumulative effects of campaign activity on EMS use are presented in Box 2. The temporal trend was significant, with a 0.6% monthly increase (95% CI, 0.5–0.7%; P < 0.001) in ambulance use for chest pain over the study period. When compared with non-campaign months, months with campaign activity were associated with an immediate 10.7% increase (95% CI, 6.5–14.9%; P < 0.001) in ambulance use for chest pain. The cumulative effect of campaign activity was equivalent to a 15.4% increase (95% CI, 10.1–20.9%; P < 0.001) in ambulance use during the month of campaign activity and two lag months.
Locally weighted scatterplot smoothing of monthly attendances for chest pain, corrected for trend and seasonal effects, is shown in Box 3. When compared with the pre-campaign period (January 2008 – September 2009), the post-campaign period (October 2009 – December 2013) was associated with an 18.7% step increase (95% CI, 13.8–23.8%; P < 0.001) in ambulance use and a significant increase in the monthly trend for ambulance use of 0.3% (95% CI, 0.0–0.5%; P = 0.02).
Influence of campaign features on ambulance use
The effect of campaign activity on ambulance use was variable over the 5-year campaign schedule, with the greatest effect observed in the first campaign year (Box 2). The type of media used, TARP level, and the number of consecutive months of campaign activity did not influence the change in ambulance use. Conversely, there was a dose-dependent relationship between number of days of continuous exposure and ambulance use, with longer campaign periods (14 days or more) associated with higher cumulative ambulance use (20.7%; 95% CI, 12.6–29.3%) than shorter campaign periods (12.9%; 95% CI, 7.8–18.1%; P = 0.03).
Influence of campaign activity on sub-populations
The stratified analysis of our data is presented in Box 4. The immediate effect of campaign activity on ambulance use was similar across sex and age groups. The largest cumulative effect was in patients aged 31–45 years. Although the numbers of patients transported and not transported by ambulance both increased during campaign activity, the cumulative effect was higher for non-transported patients. The influence of campaign activity on ambulance use also varied between clinical presentations (Box 5). The immediate effect of campaign activity on ambulance use for patients with suspected acute coronary syndromes and heart failure was an increase of 11.3% (95% CI, 6.9–15.9%; P < 0.001) and 13.7% (95% CI, 0.9–28.1%; P = 0.03) respectively. Although campaign activity did not influence ambulance use overall for patients with ST-segment elevation myocardial infarction (STEMI), ambulance use for STEMI patients increased during the 2009 (by 35.1%; 95% CI, 15.9–57.4%; P < 0.001) and 2011 (by 10.8%; 95% CI:, 1.8–20.6%; P = 0.02) campaigns. The absolute increase in ambulance use according to clinical presentation is reported in Figure S2 in the online Appendix.
Discussion
A long term mass media campaign aiming to raise the community’s awareness of AMI symptoms and the need to take appropriate action resulted in a significant increase in ambulance use by patients with non-traumatic chest pain. Ambulance use increased by 10.7% during the month of campaign activity, with small residual effects in the two following months. When compared with the pre-campaign period, the intervention period was associated with an immediate step increase in ambulance use of 18.7% and a long term monthly increase of 0.3%. Factors such as the type of media used, TARP level, and the number of consecutive months with campaign activity did not influence the outcome.
Our study is one of only a few to find that mass media interventions can influence community health-seeking behaviour for chest pain. A one-month community-based education program in Minnesota in the United States resulted in a 14% increase in EMS use by patients with chest pain.16 Similarly, the Rapid Early Action for Coronary Treatment (REACT) randomised controlled trial in the US found a 20% increase in the odds of EMS use in communities exposed to an 18-month mass media campaign.8 In contrast, a number of mass media interventions in other countries have been relatively ineffective in increasing EMS use for chest pain. For instance, a 12-month predominantly print media campaign was ineffective in increasing ambulance use in Sweden for patients with symptoms suggestive of an AMI.13 A 12-month mass media intervention in Switzerland was also ineffective in increasing EMS use by patients presenting to the emergency department with chest pain.14
The conflicting results of previous studies should be interpreted in the context of their limitations. For instance, the campaigns described in five studies did not include any television activity, while two investigations involved only print or local community campaigns.10,12,13,15,16 In addition, six studies of mass media interventions conducted simple before-and-after analyses that did not control for the underlying trend and seasonal effects of time series data.11-16 In contrast, the Warning Signs campaigns were delivered over a 23-month intervention period, and primarily involved television and digital media. An estimated $3 million was spent on media for the Warning Signs campaign in the Melbourne region alone, substantially more than described in previous reports.8,9,11,16
Although the campaign was effective in increasing ambulance use in key at-risk populations, similar increases also occurred in low risk populations, such as younger patients and those with suspected gastrointestinal disorders. While this shows the difficulty in developing a public health message that is sufficiently specific for reaching people with an AMI, our system benefits from highly trained paramedics who are able to autonomously triage and assess the need for transport to hospital. Our findings suggest that the proportion of people with chest pain taken to hospital by ambulance was lower on campaign days, which indicates that pre-hospital triage by EMS personnel could reduce unnecessary hospital presentations. In less sophisticated EMS systems, the impact of mass media campaigns on the number of hospital presentations could be far greater if EMS personnel were not authorised to make transport decisions autonomously or under medical supervision.
We acknowledge several limitations to our study. The lack of hospital outcome data means we were unable to verify clinical assessments by paramedics or to determine whether the campaigns were associated with an increase in EMS use by patients with a confirmed AMI. Nevertheless, a recent clinical trial in our region reported the highly positive predictive value of pre-hospital STEMI diagnoses (75%),24 and paramedic assessment of ischaemic heart disease concords well with hospital diagnosis records.25 In addition, although our analyses recorded all significant campaign-related activities over the 6-year study period, it is possible that other pro bono work was sporadically undertaken during this period and was not systematically recorded. Finally, we did not assess whether campaign activity led to a significant reduction in the time taken to seek medical attention, although such an evaluation has been described elsewhere.21
Despite these limitations, our study shows that a comprehensive public awareness campaign using a multi-faceted mass media strategy was effective in influencing short and long term EMS use by patients with non-traumatic chest pain. Although our findings support the value of mass media intervention for improving health service use, it remains to be determined whether these campaigns led to an increase in ambulance use by people with an AMI, or whether they improved clinical outcomes.
Box 1 – Characteristics of patients with chest pain attended by an emergency medical service in Melbourne, January 2008 – December 2013
Characteristic |
All days |
Non-campaign days |
Campaign days |
P |
|||||||||||
Total number of patients |
253428 |
213587 |
39841 |
||||||||||||
Age in years, median (IQR) |
63 (47–78) |
64 (47–78) |
62 (46–77) |
<0.001 |
|||||||||||
Missing data |
258 (0.1%) |
224 (0.1%) |
34 (0.1%) |
— |
|||||||||||
Sex (men) |
124678 (49.2%) |
105377 (49.4%) |
19301 (48.5%) |
0.001 |
|||||||||||
Missing data |
130 (0.1%) |
113 (0.1%) |
17 (<0.1%) |
— |
|||||||||||
Time of call |
|||||||||||||||
00:00–07:59 |
62334 (24.6%) |
52598 (24.6%) |
9736 (24.4%) |
0.42 |
|||||||||||
08:00–15:59 |
97088 (38.3%) |
81828 (38.3%) |
15260 (38.3%) |
0.97 |
|||||||||||
16:00–23:59 |
94005 (37.1%) |
79160 (37.1%) |
14845 (37.3%) |
0.45 |
|||||||||||
Pre-existing conditions |
|||||||||||||||
Ischaemic heart disease |
78001 (32.7%) |
66499 (33.0%) |
11502 (30.9%) |
<0.001 |
|||||||||||
Other heart disease |
9045 (3.8%) |
7605 (3.8%) |
1440 (3.9%) |
0.40 |
|||||||||||
Heart failure |
16610 (7.0%) |
14095 (7.0%) |
2515 (6.8%) |
0.09 |
|||||||||||
Arrhythmia |
28027 (11.7%) |
23618 (11.7%) |
4409 (11.8%) |
0.54 |
|||||||||||
Pacemaker or implantable defibrillator |
10805 (4.5%) |
9129 (4.5%) |
1676 (4.5%) |
0.78 |
|||||||||||
Dyslipidaemia |
71258 (29.9%) |
59886 (29.7%) |
11372 (30.5%) |
0.002 |
|||||||||||
Hypertension |
104106 (43.6%) |
87750 (43.6%) |
16356 (43.9%) |
0.22 |
|||||||||||
Diabetes mellitus |
41847 (17.5%) |
35457 (17.6%) |
6390 (17.2%) |
0.04 |
|||||||||||
Renal insufficiency |
6387 (2.7%) |
5435 (2.7%) |
952 (2.6%) |
0.12 |
|||||||||||
Stroke or transient ischaemic attack |
14889 (6.2%) |
12658 (6.3%) |
2231 (6.0%) |
0.03 |
|||||||||||
Cancer |
18841 (7.9%) |
15986 (7.9%) |
2855 (7.7%) |
0.07 |
|||||||||||
Asthma |
23733 (9.9%) |
20082 (10.0%) |
3651 (9.8%) |
0.32 |
|||||||||||
Chronic obstructive pulmonary disease |
15934 (6.7%) |
13393 (6.6%) |
2541 (6.8%) |
0.22 |
|||||||||||
Mental illness |
50115 (21.0%) |
42040 (20.9%) |
8075 (21.7%) |
<0.001 |
|||||||||||
Substance abuse |
8042 (3.4%) |
6722 (3.3%) |
1320 (3.5%) |
0.04 |
|||||||||||
Gastro-oesophageal reflux |
37008 (15.5%) |
30877 (15.3%) |
6131 (16.5%) |
<0.001 |
|||||||||||
No pre-existing conditions |
5273 (2.2%) |
4605 (2.3%) |
668 (1.8%) |
<0.001 |
|||||||||||
Missing data |
14733 (5.8%) |
12144 (5.7%) |
2589 (6.5%) |
— |
|||||||||||
Transport to a medical facility |
213330 (84.2%) |
180169 (84.4%) |
33161 (83.2%) |
<0.001 |
|||||||||||
Box 2 – Immediate and cumulative effects of campaign characteristics on ambulance use for chest pain
Characteristic |
Immediate effect (campaign month) |
Cumulative effect (campaign month and following 2 months) |
|||||||||||||
Incidence rate ratio (95% CI) |
P |
Incidence rate ratio (95% CI) |
P |
||||||||||||
Any campaign activity |
1.11 (1.07–1.15) |
<0.001 |
1.15 (1.10–1.21) |
<0.001 |
|||||||||||
Type of mass media used |
|||||||||||||||
Television or radio alone |
1.10 (1.04–1.16) |
0.001 |
1.14 (1.06–1.22) |
<0.001 |
|||||||||||
Television with radio/press |
1.11 (1.07–1.15) |
<0.001 |
1.16 (1.10–1.22) |
<0.001 |
|||||||||||
Campaign activity days in the observation month |
|||||||||||||||
<14 days |
1.09 (1.05–1.14) |
<0.001 |
1.13 (1.08–1.18) |
<0.001 |
|||||||||||
≥14 days |
1.13 (1.08–1.17) |
<0.001 |
1.21 (1.13–1.29) |
<0.001 |
|||||||||||
Consecutive months with campaign activity |
|||||||||||||||
1 month |
1.10 (1.05–1.15) |
<0.001 |
1.25 (1.11–1.41) |
<0.001 |
|||||||||||
2 months |
1.11 (1.06–1.16) |
<0.001 |
1.12 (1.00–1.25) |
0.05 |
|||||||||||
3 months or more |
1.11 (1.07–1.16) |
<0.001 |
1.14 (1.09–1.19) |
<0.001 |
|||||||||||
Maximum TARPS |
|||||||||||||||
≤50 |
1.11 (1.06–1.17) |
<0.001 |
1.14 (1.08–1.20) |
<0.001 |
|||||||||||
>50 |
1.10 (1.06–1.15) |
<0.001 |
1.17 (1.10–1.23) |
<0.001 |
|||||||||||
Year of campaign |
|||||||||||||||
2009 |
1.17 (1.14–1.20) |
<0.001 |
1.25 (1.20–1.29) |
<0.001 |
|||||||||||
2010 |
1.12 (1.07–1.17) |
<0.001 |
1.15 (1.10–1.21) |
<0.001 |
|||||||||||
2011 |
1.04 (1.00–1.09) |
0.06 |
1.10 (1.03–1.17) |
0.004 |
|||||||||||
2012 |
1.09 (1.04–1.12) |
<0.001 |
1.17 (1.09–1.25) |
<0.001 |
|||||||||||
2013 |
1.10 (1.03–1.17) |
0.002 |
1.10 (1.01–1.18) |
0.02 |
|||||||||||
TARPS = target audience rating points. Models adjusted for temporal trend, seasonal effects and length of observation month. | |||||||||||||||
Box 3 – Locally weighted scatterplot smoothing of the monthly number of ambulance attendances for chest pain after adjustment for the underlying trend and seasonal effects*
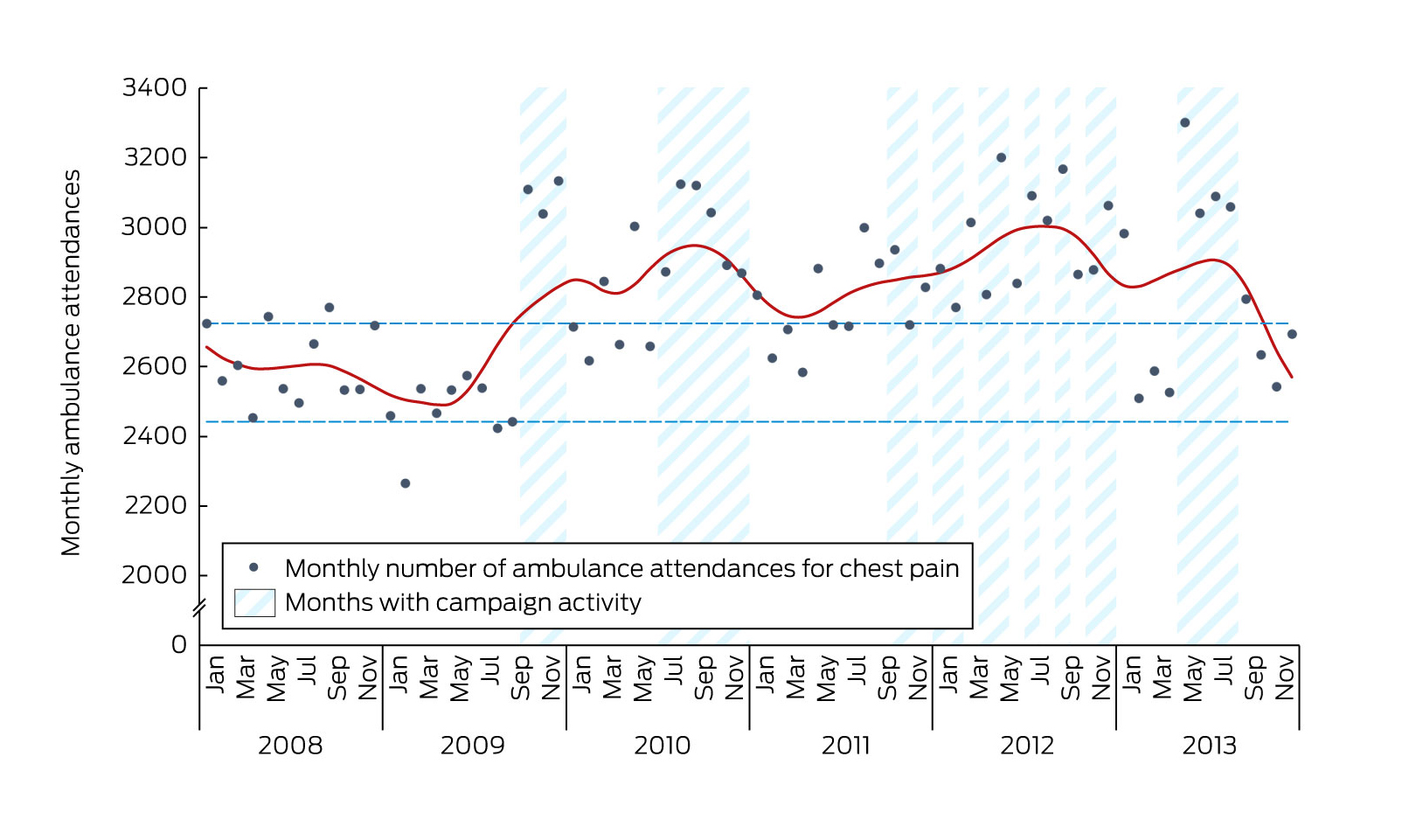
Dotted lines = 10th and 90th percentile ambulance attendances during the pre-campaign period. *Data points are for the monthly number of attendances for chest pain after adjusting for seasonal effects and the long term trend; ie, they are adjusted to eliminate the effects of temporal variation, in order to clarify how much of the variation in emergency medical service use is the result of media activity alone. For this reason, the numbers of chest pain presentations in this figure are lower than the unadjusted estimates provided in the first paragraph of the Results section.
Box 4 – Stratified analysis of the effect of campaign activity on ambulance use for chest pain*
Characteristic |
Immediate effect (campaign month) |
Cumulative effect (campaign month and following 2 months) |
|||||||||||||
Incidence rate ratio (95% CI) |
P |
Incidence rate ratio (95% CI) |
P |
||||||||||||
Age |
|||||||||||||||
≤30 years |
1.09 (1.05–1.14) |
<0.001 |
1.16 (1.07–1.25) |
<0.001 |
|||||||||||
31–45 years |
1.13 (1.08–1.19) |
<0.001 |
1.22 (1.15–1.30) |
<0.001 |
|||||||||||
46–60 years |
1.13 (1.07–1.19) |
<0.001 |
1.18 (1.10–1.26) |
<0.001 |
|||||||||||
61–75 years |
1.09 (1.04–1.14) |
<0.001 |
1.12 (1.06–1.18) |
<0.001 |
|||||||||||
> 75 years |
1.10 (1.06–1.14) |
<0.001 |
1.14 (1.08–1.19) |
<0.001 |
|||||||||||
Sex |
|||||||||||||||
Men |
1.10 (1.06–1.14) |
<0.001 |
1.15 (1.10–1.20) |
<0.001 |
|||||||||||
Women |
1.11 (1.07–1.16) |
<0.001 |
1.16 (1.10–1.22) |
<0.001 |
|||||||||||
Pre-existing conditions |
|||||||||||||||
Ischaemic heart disease |
1.09 (1.05–1.12) |
<0.001 |
1.12 (1.07–1.17) |
<0.001 |
|||||||||||
Other heart disease |
1.08 (1.00–1.17) |
0.05 |
1.12 (0.99–1.27) |
0.08 |
|||||||||||
Heart failure |
1.11 (1.06–1.17) |
<0.001 |
1.12 (1.03–1.22) |
0.01 |
|||||||||||
Arrhythmia |
1.08 (1.03–1.13) |
0.001 |
1.11 (1.04–1.18) |
0.001 |
|||||||||||
Pacemaker or implantable defibrillator |
1.13 (1.08–1.19) |
<0.001 |
1.16 (1.07–1.27) |
<0.001 |
|||||||||||
Dyslipidaemia |
1.12 (1.06–1.18) |
<0.001 |
1.17 (1.09–1.25) |
<0.001 |
|||||||||||
Hypertension |
1.10 (1.06–1.15) |
<0.001 |
1.14 (1.08–1.20) |
<0.001 |
|||||||||||
Diabetes mellitus |
1.09 (1.05–1.14) |
<0.001 |
1.13 (1.06–1.20) |
<0.001 |
|||||||||||
Renal insufficiency |
1.08 (1.02–1.15) |
0.009 |
1.10 (1.00–1.21) |
0.06 |
|||||||||||
Stroke or transient ischaemic attack |
1.08 (1.02–1.15) |
0.006 |
1.15 (1.08–1.23) |
<0.001 |
|||||||||||
Cancer |
1.04 (0.99–1.11) |
0.15 |
1.05 (0.97–1.14) |
0.26 |
|||||||||||
Asthma |
1.10 (1.04–1.16) |
0.001 |
1.19 (1.12–1.26) |
<0.001 |
|||||||||||
Chronic obstructive pulmonary disease |
1.10 (1.06–1.15) |
<0.001 |
1.15 (1.07–1.24) |
<0.001 |
|||||||||||
Mental illness |
1.12 (1.07–1.17) |
<0.001 |
1.16 (1.08–1.25) |
<0.001 |
|||||||||||
Substance abuse |
1.08 (1.01–1.14) |
0.02 |
1.14 (1.05–1.24) |
0.002 |
|||||||||||
Gastro-oesophageal reflux |
1.11 (1.05–1.17) |
<0.001 |
1.17 (1.08–1.26) |
<0.001 |
|||||||||||
No pre-existing conditions |
1.11 (0.97–1.27) |
0.14 |
1.14 (0.98–1.34) |
0.09 |
|||||||||||
Transport to hospital |
|||||||||||||||
Not transported |
1.14 (1.08–1.20) |
<0.001 |
1.22 (1.15–1.29) |
<0.001 |
|||||||||||
Transported |
1.10 (1.06–1.14) |
<0.001 |
1.14 (1.09–1.20) |
<0.001 |
|||||||||||
*Models adjusted for temporal trend, seasonal effects and length of observation month. | |||||||||||||||
Box 5 – Influence of campaign activity on the immediate effect (campaign month) in ambulance use for various clinical presentations as assessed by paramedics*
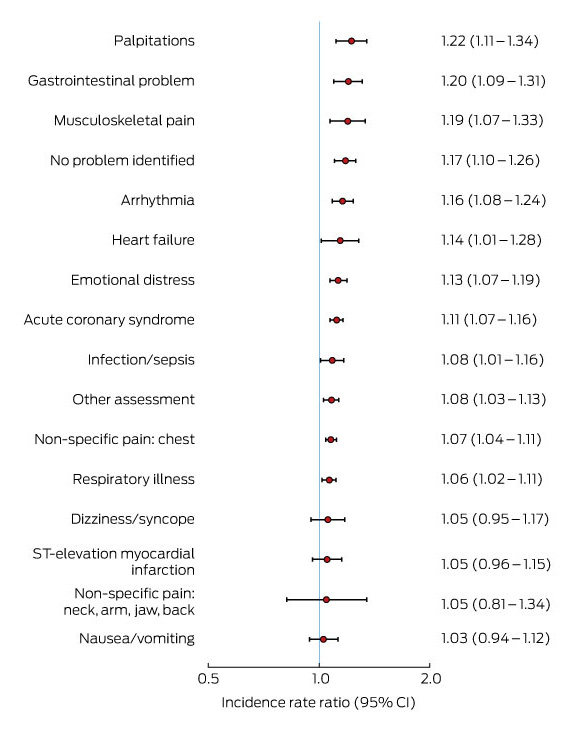
*Clinical presentations are the principal paramedic diagnoses for each patient, and are mutually exclusive, with the exception of ST-elevation myocardial infarction, a subset of acute coronary syndrome presentations.
Received 22 March 2016, accepted 15 July 2016
- Ziad Nehme1,2
- Peter A Cameron2,3
- Muhammad Akram2,3
- Harry Patsamanis4
- Janet E Bray2
- Ian T Meredith5
- Karen Smith1
- 1 Ambulance Service of Victoria, Melbourne, VIC
- 2 Monash University, Melbourne, VIC
- 3 Australian Collaboration for Research into Injury in Sport and its Prevention, Federation University, Ballarat, VIC
- 4 National Heart Foundation of Australia, Melbourne, VIC
- 5 Monash Medical Centre, Melbourne, VIC
The Heart Foundation of Australia provided details of the campaigns, but had no role in the reporting or analysis of data. Harry Patsamanis is employed by the Heart Foundation and was previously manager of the campaign. Ian Meredith appeared in -related media in a voluntary capacity without remuneration or other incentives. Janet Bray receives salary support from a National Health Medical and Research Council (NHMRC)-funded project (1029983) and from an NHMRC/National Heart Foundation Public Health Fellowship (1069985). Janet Bray was commissioned by the Heart Foundation to conduct a recent campaign evaluation, but received no personal financial incentives for this work.
- 1. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics — 2015 update: a report from the American Heart Association. Circulation 2015; 131: e29-e322.
- 2. Muller D, Agrawal R, Arntz HR. How sudden is sudden cardiac death? Circulation 2006; 114: 1146-1150.
- 3. Zijlstra F, Patel A, Jones M, et al. Clinical characteristics and outcome of patients with early (<2h), intermediate (2–4h) and late (>4h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J 2002; 23: 550-557.
- 4. De Luca G, Suryapranata H, Ottervanger JP, et al. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation 2004; 109: 1223-1225.
- 5. Canto JG, Zalenski RJ, Ornato JP, et al. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation 2002; 106: 3018-3023.
- 6. Nehme Z, Andrew E, Bernard S, et al. Comparison of out-of-hospital cardiac arrest occurring before and after paramedic arrival: epidemiology, survival to hospital discharge and 12-month functional recovery. Resuscitation 2015; 89: 50-57.
- 7. Finn JC, Bett JH, Shilton TR, et al; National Heart Foundation of Australia Chest Pain Every Minute Counts Working Group. Patient delay in responding to symptoms of possible heart attack: can we reduce time to care? Med J Aust 2007; 187: 293-298. <MJA full text>
- 8. Luepker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention on patient delay and emergency medical service use in acute coronary heart disease: The Rapid Early Action for Coronary Treatment (REACT) Trial. JAMA 2000; 284: 60-67.
- 9. Eppler E, Eisenberg MS, Schaeffer S, et al. 911 and emergency department use for chest pain: results of a media campaign. Ann Emerg Med 1994; 24: 202-208.
- 10. Meischke H, Dulberg EM, Schaeffer SS, et al. “Call fast, call 911”: A direct mail campaign to reduce patient delay in acute myocardial infarction. Am J Public Health 1997; 87: 1705-1709.
- 11. Ho MT, Eisenberg MS, Litwin PE, et al. Delay between onset of chest pain and seeking medical care: the effect of public education. Ann Emerg Med 1989; 18: 727-731.
- 12. Herlitz J, Blohm M, Hartford M, et al. Follow-up of a 1-year media campaign on delay times and ambulance use in suspected acute myocardial infarction. Eur Heart J 1992; 13: 171-177.
- 13. Herlitz J, Hartford M, Blohm M, et al. Effect of a media campaign on delay times and ambulance use in suspected acute myocardial infarction. Am J Cardiol 1989; 64: 90-93.
- 14. Gaspoz JM, Unger PF, Urban P, et al. Impact of a public campaign on pre-hospital delay in patients reporting chest pain. Heart 1996; 76: 150-155.
- 15. Blohm M, Hartford M, Karlson BW, et al. A media campaign aiming at reducing delay times and increasing the use of ambulance in AMI. Am J Emerg Med 1994; 12: 315-318.
- 16. Wright RS, Kopecky SL, Timma M, et al. Impact of community-based education on health care evaluation in patients with acute chest pain syndromes: the Wabasha Heart Attack Team (WHAT) project. Fam Pract 2001; 18: 537-539.
- 17. Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database Syst Rev 2002; (1): CD000389.
- 18. Bett JH, Tonkin AM, Thompson PL, et al. Failure of current public educational campaigns to impact on the initial response of patients with possible heart attack. Intern Med J 2005; 35: 279-282.
- 19. National Heart Foundation of Australia. Heart attack warning signs [website]. http://heartfoundation.org.au/your-heart/heart-attack-warning-signs (accessed Feb 2016).
- 20. Cox S, Martin R, Somaia P, et al. The development of a data-matching algorithm to define the “case patient”. Aust Health Rev 2013; 37: 54-59.
- 21. Bray JE, Stub D, Ngu P, et al. Mass media campaigns’ influence on prehospital behavior for acute coronary syndromes: an evaluation of the Australian Heart Foundation’s Warning Signs campaign. J Am Heart Assoc 2015; 4: e001927.
- 22. Jandoc R, Burden AM, Mamdani M, et al. Interrupted time series analysis in drug utilization research is increasing: systematic review and recommendations. J Clin Epidemiol 2015; 68: 950-956.
- 23. Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002; 27: 299-309.
- 24. Stub D, Smith K, Bernard S, et al. Air versus oxygen in ST-segment elevation myocardial infarction. Circulation 2015; 131: 2143-2150.
- 25. Schaider JJ, Riccio JC, Rydman RJ, et al. Paramedic diagnostic accuracy for patients complaining of chest pain or shortness of breath. Prehosp Disaster Med 1995; 10: 245-250.





Abstract
Objectives: To evaluate the impact of comprehensive public awareness campaigns by the National Heart Foundation of Australia on emergency medical service (EMS) use by people with chest pain.
Design, setting and participants: A retrospective analysis of 253428 emergency ambulance attendances for non-traumatic chest pain in Melbourne, January 2008 – December 2013. Time series analyses, adjusted for underlying trend and seasonal effects, assessed the impact of mass media campaigns on EMS use.
Main outcome measure: Monthly ambulance attendances.
Results: The median number of monthly ambulance attendances for chest pain was 3609 (IQR, 3011–3891), but was higher in campaign months than in non-campaign months (3880 v 3234, P<0.001). After adjustments, campaign activity was associated with a 10.7% increase (95% CI, 6.5–14.9%; P<0.001) in monthly ambulance use for chest pain, and a 15.4% increase (95% CI, 10.1–20.9%; P<0.001) when the two-month lag periods were included. Clinical presentations for suspected acute coronary syndromes, as determined by paramedics, increased by 11.3% (95% CI, 6.9–15.9%; P<0.001) during campaigns. Although the number of patients transported to hospital by ambulance increased by 10.0% (95% CI, 6.1–14.2%; P<0.001) during campaign months, the number of patients not transported to hospital also increased, by 13.9% (95% CI, 8.3–19.8%; P<0.001).
Conclusion: A public awareness campaign about responding to prodromal acute myocardial infarction symptoms was associated with an increase in EMS use by people with chest pain and suspected acute coronary syndromes. Campaign activity may also lead to increased EMS use in low risk populations.