In July 2008, a condition-onset flag was added to the specifications of the International Statistical Classification of Diseases and Related Health Problems (10th revision, Australian modification) (ICD-10) codes. This created the opportunity to distinguish between hospital-acquired complications and comorbidities present on admission in routinely coded administrative data. To help analyse this flag, the Australian Centre for Economic Research on Health (under sponsorship by the Australian Commission on Safety and Quality in Health Care) developed a classification system known as the Classification of Hospital Acquired Diagnoses (CHADx).1 This system provides hospitals with a meaningful way of grouping complications that are coded as arising in hospital into 17 classes (eg, adverse drug events and postprocedural complications) and 145 subclasses, and a way of reducing double counting of codes when they are recorded in related sequences.1,2
The costs associated with hospital-acquired complications are well documented.3-6 One Australian study estimated that complications increase treatment costs by 17%.7 As well as increased costs, overseas studies have shown significantly longer length of stay (LOS) in patients who experience indicator conditions such as adverse drug events,8 hospital-acquired infections9 and postoperative complications.10 However, few studies report effects on LOS for the full range of hospital-acquired complications.
These results suggest that an automated system for reporting hospital-acquired complications would be valuable. Monthly use of CHADx as a tool to monitor trends in hospital-acquired complication rates and patient safety has been suggested.1 While initial results of analysis of jurisdictional data have been reported,1,7 we found no examples of CHADx implementation at the hospital level. To our knowledge, no hospitals have implemented local systems to take advantage of this classification and monitoring tool. This may be due to the apparent complexity of the CHADx system.
Here, we report the initial results of implementation of an automated CHADx reporting system in the South Metropolitan Health Service (SMHS) in Western Australia. In the absence of software to group inpatient separation data, we developed an abstract model that assigns combinations of diagnosis codes to CHADx classes and subclasses.11 We aimed to report the incidence of hospital-acquired complications in all inpatients presenting to the SMHS and investigate the association between hospital-acquired complications and hospital LOS in multiday-stay patients.
We also created a subset of inpatient separation data for multiday-stay patients. To do so, we excluded patients who were admitted and discharged on the same day, patients who presented to the ED with chest pain and stayed past midnight (because this large group of multiday-stay patients predominantly had a short stay), and patients admitted for obstetric or neonatal care. Patients admitted for obstetric or neonatal care were excluded from the LOS analysis as they differed from other multiday-stay patients. For example, unlike other hospital patients, generally speaking, this group are in good health and are not presenting for a “pathological condition”. Also, as described by the CHADx authors, the complications arising from this group of patients are handled differently in the classification system.12 These important differences affect the exposure of interest (ie, risk of experiencing a hospital-acquired complication) and the main outcome measure (ie, hospital LOS).
It was difficult to find a suitable measure that could be used to adjust for patient complexity. All available measures were based on the coded diagnoses — comorbidities present on admission and complications arising in hospital. We reviewed the ICD-10 Deyo version of the Charlson comorbidity index (CCI)13 and found that 7% of diagnoses making up the CCI score were not present on admission (ie, they were hospital acquired). To account for this we removed hospital-acquired complications from the CCI score, and therefore refer to this measure as the adjusted CCI.
For the 2-year study period, our dataset contained 436 841 inpatient separations (Box 1). Patients had a mean age of 53.8 years (SD, 23.0 years) and 229 011 (52.42%) were male. Based on the CHADx mapping rules of our model, 29 172 of the separations (6.68%) had at least one hospital-acquired complication code assigned; these 29 172 separations had a total of 56 326 CHADx codes assigned (ie, a mean of 1.93 CHADx codes per separation). The median adjusted CCI was 0 (range, 12).
The three most frequently occurring hospital-acquired complications as described by the CHADx classes were postprocedural complications; cardiovascular complications; and labour, delivery and postpartum complications. These accounted for 33.35% (18 785) of CHADx codes. The five most frequently occurring subclasses were: hypotension; electrolyte disorders without dehydration; cardiac arrhythmias, conduction disturbances and abnormal heart beat; urinary tract infections; and alterations to mental state (Box 2). These made up 16.80% (9461) of CHADx codes. The 20 most frequently occurring CHADx subclasses accounted for 44.01% (24 788) of CHADx codes.
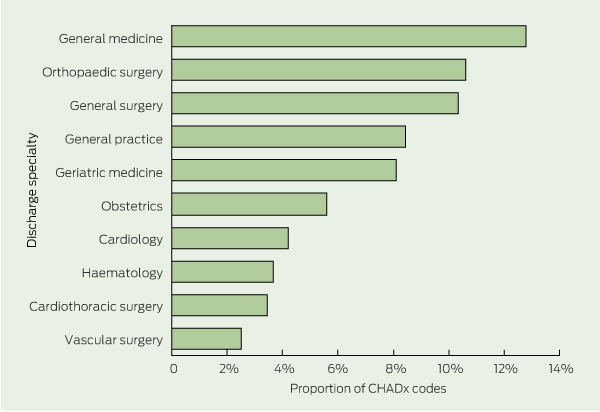
General medicine was the specialty with the most hospital-acquired complications. Orthopaedic surgery, general surgery, cardiothoracic surgery and vascular surgery were among the top 10 specialties (Box 3). These 10 specialties reported 69.69% (39 253) of CHADx codes.
The DRGs with the 10 largest numbers of CHADx codes represented fewer than 2.60% of all DRGs (our sample consisted of 385 different DRGs) but accounted for 38.62% (21 751) of CHADx codes (Box 4). The rehabilitation DRG had the largest number of CHADx codes, with 7.36% of the total.
According to unadjusted rates of complications in separations for multiday-stay patients, the group with hospital-acquired complications had a higher mean age (65.4 years v 53.3 years), lower proportion of emergency admissions (64.17% v 72.16%), lower proportion of patients discharged home (58.37% v 83.01%) and higher proportion of surgical patients (43.63% v 25.87%) than the group with no hospital-acquired complications (Box 5).
Crude mean LOS was longer in the group with hospital-acquired complications than the group without (17.4 days v 5.4 days) (Box 5). An unadjusted IRR of 4.91 (95% CI, 4.77–5.06) indicated an almost fivefold increase in LOS for the group with complications. After adjusting for age, hospital, Indigenous status, DRG category, separation type, admission type, sex and adjusted CCI score, there was an almost fourfold increase (IRR, 3.84; 95% CI, 3.73–3.96) (Box 6).
Our findings of increased LOS are consistent with data from other studies.3,14-16 An observational study that used multivariable matching to measure excess LOS, cost and mortality attributable to hospital-acquired complications highlighted the significant impact that complications have on LOS — up to 10 extra days were attributed to complications such as postoperative sepsis, selected infections due to medical care and postoperative wound dehiscence.16
In addition to estimating the relationship between complications and LOS, implementing the CHADx system has allowed us to report on the incidence and frequency of hospital-acquired complications on an ongoing basis. To aid analysis, we include CHADx in our hospital business intelligence tools. These tools are refreshed daily and allow users to analyse CHADx rates by specialty, DRG, ward and other clinically meaningful factors. These tools have been useful for identifying the potential benefits of hospital-wide patient safety initiatives such as the WA Patient Blood Management Program.17
The ability to report patterns and trends of hospital-acquired complications is valuable for many reasons. Although not the sole element, a key part in consistently improving patient safety and quality of care is the feedback of meaningful data to clinicians and other decisionmakers.18 Also, hospital-acquired complications play a role in funding in some countries. The Medicare system in the United States excludes funding for specific hospital-acquired complications in an attempt to remove incentives for substandard care.19 It is possible that future payment models in Australia may include similar incentives, given that the Independent Hospital Pricing Authority has evaluated the US Medicare approach.20
These insights could be used to identify combinations of complications and types of procedures or patients for which a review of standard practice may be warranted. For example, hospital-acquired anaemia was among the most common complications and patients who had knee replacements were one of the higher-risk groups in terms of complications. Such findings provide direction for future research on preventing complications.21
Second, for complications to be identified, two important steps are required: good clinical documentation in the patient notes and translation of the notes into ICD-10 codes by professional coders. For this reason, the coded data are likely to underrepresent the number of hospital-acquired complications.22 This underestimation, however, is difficult to measure. One of the reasons for this is that the CHADx system was designed to monitor the full range of hospital-acquired complications1 and its level of accuracy is likely to vary between groups of complications. For example, it has been shown that coded data are a poor indicator of hospital-acquired infections23 and that coded data are more reliable for surgical patients than medical patients.24 In addition, classification systems based on coded data are influenced by variations in the accuracy and completeness of clinical documentation and coding between hospitals and jurisdictions.12
2 CHADx subclasses with the 20 largest numbers of CHADx codes
4 DRGs with the 10 largest numbers of CHADx codes
Neonate, admit weight > 2499 g without significant operating room procedure |
|||||||||||||||
DRG = Diagnosis-related group. CHADx = Classification of Hospital Acquired Diagnoses. |
|||||||||||||||
5 Characteristics of inpatient separations for multiday-stay patients with and without hospital-acquired complications*
Hospital-acquired complication |
|||||||||||||||
Received 7 November 2012, accepted 9 May 2013
- Kevin M Trentino1
- Stuart G Swain1
- Sally A Burrows2
- Peter C Sprivulis3
- Frank F S Daly4
- 1 Performance Unit, South Metropolitan Health Service, Perth, WA.
- 2 School of Medicine and Pharmacology, University of Western Australia, Perth, WA.
- 3 School of Primary, Aboriginal and Rural Health Care, University of Western Australia, Perth, WA.
- 4 Royal Perth Group, South Metropolitan Health Service, Perth, WA.
No relevant disclosures.
- 1. Jackson TJ, Michel JL, Roberts RF, et al. A classification of hospital-acquired diagnoses for use with routine hospital data. Med J Aust 2009; 191: 544-548. <MJA full text>
- 2. Australian Commission on Safety and Quality in Health Care. Classification of Hospital Acquired Diagnoses (CHADx). http://www.safetyandquality.gov.au/wp-content/uploads/2010/01/35566-CHADx.pdf (accessed Dec 2010).
- 3. Rivard PE, Luther SL, Christiansen CL, et al. Using patient safety indicators to estimate the impact of potential adverse events on outcomes. Med Care Res Rev 2008; 65: 67-87.
- 4. Carey K, Stefos T. Measuring the cost of hospital adverse patient safety events. Health Econ 2011; 20: 1417-1430.
- 5. Shreve J, Van Den Bos J, Gray T, et al. The economic measurement of medical errors. Schaumburg, Ill: Society of Actuaries, 2010. http://www.soa.org/research/research-projects/health/research-econ-measurement.aspx (accessed Oct 2013).
- 6. Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: the annual cost of measurable medical errors. Health Aff (Millwood) 2011; 30: 596-603.
- 7. Jackson T, Nghiem HS, Rowell DS, et al. Marginal costs of hospital acquired conditions: information for priority-setting for patient safety programmes and research. J Health Serv Res Policy 2011; 16: 141-146.
- 8. Classen DC, Pestotnik SL, Evans RS, et al. Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA 1997; 277: 301-306.
- 9. Herwaldt LA, Cullen JJ, Scholz D, et al. A prospective study of outcomes, healthcare resource utilization, and costs associated with postoperative nosocomial infections. Infect Control Hosp Epidemiol 2006; 27: 1291-1298.
- 10. Dimick JB, Chen SL, Taheri PA, et al. Hospital costs associated with surgical complications: a report from the private-sector National Surgical Quality Improvement Program. J Am Coll Surg 2004; 199: 531-537.
- 11. Swain S, Trentino K. Developing an abstract model for implementing the CHADx classification system. http://www.safetyandquality.gov.au/our-work/information-strategy/health-information-standards/classification-of-hospital-acquired-diagnoses-chadx (accessed Feb 2013).
- 12. Michel JL, Cheng D, Jackson TJ. Comparing the coding of complications in Queensland and Victorian admitted patient data. Aust Health Rev 2011; 35: 245-252.
- 13. Sundararajan V, Henderson TM, Perry C, et al. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol 2004; 57: 1288-1294.
- 14. Ehsani JP, Jackson T, Duckett SJ. The incidence and cost of adverse events in Victorian hospitals 2003–04. Med J Aust 2006; 184: 551-555. <MJA full text>
- 15. Layde PM, Meurer LN, Guse C, et al. Medical injury identification using hospital discharge data. In: Henricksen K, Battles JB, Marks E, Lewin DI, editors. Advances in patient safety: from research to implementation. Volume 2: Concepts and methodology. Rockville, Md: Agency for Healthcare Research and Quality, 2005: 119-132.
- 16. Zhan C, Miller MR. Excess length of stay, charges, and mortality attributable to medical injuries during hospitalization. JAMA 2003; 290: 1868-1874.
- 17. Browning RM, Trentino K, Nathan EA, Hashemi N; Western Australian Patient Blood Management Program. Preoperative anaemia is common in patients undergoing major gynaecological surgery and is associated with a fivefold increased risk of transfusion. Aust N Z J Obstet Gynaecol 2012; 52: 455-459.
- 18. Meurer JR, Meurer LN, Grube J, et al. Combining performance feedback and evidence-based educational resources. In: Henricksen K, Battles JB, Marks E, Lewin DI, editors. Advances in patient safety: from research to implementation. Volume 4: Programs, tools, and products. Rockville, Md: Agency for Healthcare Research and Quality, 2005: 237-252.
- 19. Centers for Medicare and Medicaid Services. Hospital-acquired conditions (HAC) in acute inpatient prospective payment system (IPPS) hospitals [fact sheet]. Baltimore, Md: CMS, 2012. https://www.cms.gov/HospitalAcqCond/downloads/HACFactsheet.pdf (accessed Oct 2013).
- 20. Independent Hospital Pricing Authority. Literature review: efficiency, international best practice in ABF and future payment reform. http://www.ihpa.gov.au/internet/ihpa/publishing.nsf/Content/future-payment-reform (accessed Feb 2013).
- 21. Performance Unit, South Metropolitan Health Service. Patient blood management program: reducing anaemia, transfusions and length of stay for knee patients. 2012. https://www.healthroundtable.org/News.aspx (accessed Feb 2013).
- 22. O’Leary KJ, Devisetty VK, Patel AR, et al. Comparison of traditional trigger tool to data warehouse based screening for identifying hospital adverse events. BMJ Qual Saf 2013; 22: 130-138.
- 23. Stevenson KB, Khan Y, Dickman J, et al. Administrative coding data, compared with CDC/NHSN criteria, are poor indicators of health care-associated infections. Am J Infect Control 2008; 36: 155-164.
- 24. Weingart SN, Iezzoni LI, Davis RB, et al. Use of administrative data to find substandard care: validation of the complications screening program. Med Care 2000; 38: 796-806.





Abstract
Objectives: To use an automated Classification of Hospital Acquired Diagnoses (CHADx) reporting system to report the incidence of hospital-acquired complications in inpatients and investigate the association between hospital-acquired complications and hospital length of stay (LOS) in multiday-stay patients.
Design: Retrospective cross-sectional study for calendar years 2010 and 2011.
Setting: South Metropolitan Health Service in Western Australia, which consists of two teaching and three non-teaching hospitals.
Main outcome measures: Incidence of hospital-acquired complications and mean LOS for multiday-stay patients.
Results: Of 436 841 inpatient separations, 29 172 (6.68%) had at least one hospital-acquired complication code assigned in the administrative data, and there were a total of 56 326 complication codes. The three most common complications were postprocedural complications; cardiovascular complications; and labour, delivery and postpartum complications. In the subset of data on multiday-stay patients, crude mean LOS was longer in separations for patients with hospital-acquired complications than in separations for those without such complications (17.4 days v 5.4 days). After adjusting for potential confounders, separations for patients with hospital-acquired complications had almost four times the mean LOS of separations for those without such complications (incident rate ratio, 3.84; 95% CI, 3.73–3.96; P < 0.001).
Conclusions: An automated CHADx reporting system can be used to collect data on patients with hospital-acquired complications. Such data can be used to increase emphasis on patient safety and quality of care and identify potential opportunities to reduce LOS.