Venous thromboembolism (VTE) is a significant cause of morbidity and mortality. The clinical features of VTE are variable; many patients remain asymptomatic, while others present with non-specific illness, for which further investigation is required, particularly when pulmonary embolism (PE) is suspected. Diagnostic management of patients with suspected VTE is often inappropriate and does not always conform to recommended guidelines.1,2 The use of structured diagnostic algorithms and decision-support tools improves the accuracy of clinical assessment and the appropriateness of referral of patients with suspected VTE; however, these resources are seldom used by referring clinicians, in spite of evidence that adherence to guidelines significantly improves clinical outcomes.1-3
Several clinical probability scoring systems have been developed for use among patients with suspected VTE, of which the modified Wells score is the most widely used in Australia.4 The use of structured scoring systems and rapid assessment of plasma D-dimer, a cross-linked fibrin degradation product, has been shown to reduce the likelihood of referral for VTE-related imaging in experimental settings.4,5 Such structured assessment has now become standard practice in Western Australian teaching hospital emergency departments, where an online decision-support tool has been available since 2001.1,6 There is a widespread perception among imaging specialists in public hospitals in WA that, in spite of the availability of structured assessments and decision support, the volume of referrals for VTE investigations has increased over recent years, and that many may be inappropriate.2 We aimed to document trends in referrals for VTE-related imaging within WA teaching hospitals to see whether this perception is valid and what impact any increase in testing may have had on the incidence of deaths related to PE.
Population estimates for WA over the period were obtained from the Australian Bureau of Statistics.7
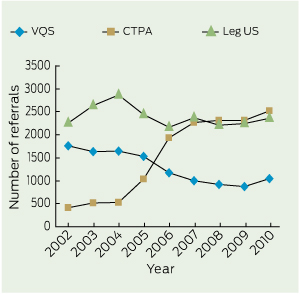
Numbers of referrals for CTPA grew rapidly between 2004 and 2007, after which the rate of growth slowed significantly (Box 1, Box 2). The volume of referrals for VQS showed a corresponding decline between 2004 and 2007. In the last year studied, there was an upswing in the volume of referrals for VQS (Box 1, Box 2).
Overall, during this period, the number of referrals for CTPA increased by more than 500%, from 410 scans in 2002 to 2526 scans in 2010, while referrals for VQS declined by 40%, from 1760 scans in 2002 to 1051 scans in 2010 (Box 1). The total number of referrals for PE-related imaging during this period increased by 65%, from 2170 in 2002 to 3577 in 2010, while referrals for all VTE-related imaging increased by 34%, from 4430 in 2002 to 5934 in 2010 (Box 1). The number of leg ultrasound examinations performed each year remained relatively stable (Box 1), and the increases in all PE-related imaging and all VTE-related imaging during the study period are explained entirely by increased referrals for CTPA.
The number of requests for D-dimer testing increased by 42% during the study period, from 3635 in 2002 to 5174 in 2010 (Box 1). Increased D-dimer testing was not associated with any reduction in the number of VTE-related imaging requests or PE-related imaging requests (Box 3).
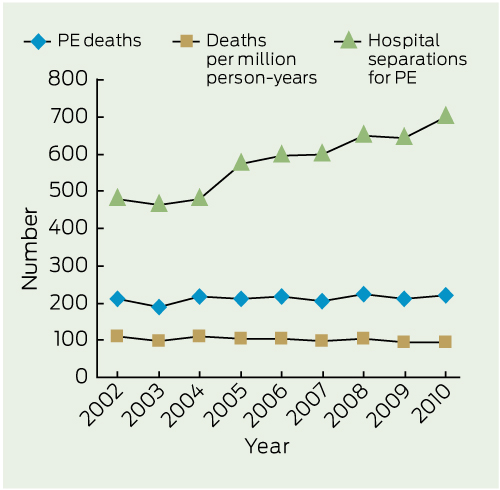
PE separations increased by 45% between 2002 and 2010, from 480 in 2002 to 698 in 2010 (Box 4, Box 5). The proportion of patients referred for PE-related imaging who subsequently had a confirmed diagnosis fell only slightly, from 22.1% in 2002 to 19.5% in 2010.
The population of WA increased by 18.9% during the study period from 1 926 111 people in 2002 to 2 290 572 in 2010 (Box 4). There was a clear increase in the number of hospital separations for PE each year (P < 0.001), while the number of deaths from PE in WA remained stable (P = 0.192 for raw death numbers [slope, 1.817; 95% CI, − 1.160 to 4.793]); P = 0.069 for deaths adjusted for population growth [slope, − 1.387; 95% CI, − 2.915 to 0.142]).
The number of PE-related imaging requests at the four adult teaching hospitals in Perth increased by 65% over the 9-year period studied. The number of PE diagnoses in the same four hospitals over the same period increased by 45%. It has long been the case that only a minority of patients referred for PE-related imaging are subsequently shown to have this condition; over the study period, the proportion of referred patients with a positive scan declined by 2.6%. Similar declines in the prevalence of PE among patients referred for imaging have recently been observed in France8 and the United States.9
Historically, D-dimer assay was suggested as a screening tool for VTE at a time when PE diagnosis was more difficult than it is now, and with the goal of reducing the number of patients who might be referred along complex and potentially invasive diagnostic pathways.10 We anticipated that routine D-dimer testing would have reduced the number of patients referred for VTE-related imaging, but our data showed that imaging has increased in line with increased D-dimer testing. This may reflect a relatively indiscriminate use of D-dimer testing to “rule out” VTE; when used indiscriminately, D-dimer may actually increase referrals for VTE-related imaging due to a high number of false-positive results. Contrary to perceived wisdom among many clinicians, PE is an infrequent diagnosis among patients presenting to emergency departments with a primary complaint of chest pain,11 while spontaneous VTE has been shown to be uncommon in non-elderly populations in Australia.12
Two further points are worthy of mention in relation to structured assessment before referral for VTE-related imaging. Firstly, the Wells score places significant weight on the physician’s overall impression of the likelihood of VTE. While this may be appropriate in the hands of experienced clinicians or researchers, it may not be the case when the score is used by junior medical staff, who may be likely to overestimate the likelihood of VTE. Secondly, when the scoring system is used after receipt of the D-dimer result, medical staff are biased towards producing a positive score,13 so use of the score may not result in the objective assessment hoped for. Therefore, in a setting of low clinical probability, a positive D-dimer test is likely to result in unnecessary imaging, especially in emergency departments, where D-dimer tests may be ordered for any patient with shortness of breath or chest pain before they are assessed by a doctor.14-16
The overall increase in PE-related imaging observed in our study was driven entirely by increased referrals for CTPA. CTPA was first introduced in WA in 1999 and referrals grew rapidly between 2004 and 2007, after which the rate of growth slowed significantly. VQS had been the standard imaging method for suspected PE until the introduction of CTPA and showed a steady corresponding decline in the volume of referrals between 2004 and 2007. During the study period, referrals for VQS declined by 40%, while referrals for CTPA increased by more than 500%. Part of the drift from VQS to CTPA may be explained by the referring clinicians’ dissatisfaction with non-diagnostic VQS reports, a frequent consequence of using PIOPED (prospective investigation of pulmonary embolism diagnosis) reporting criteria,17 which was commonplace in WA teaching hospitals at the start of the study period. On the other hand, CTPA scans have always been reported dichotomously (ie, positive or negative for PE), which may induce the impression of greater accuracy compared with VQS. There has been widespread adoption of dichotomous reporting styles in nuclear medicine departments in WA teaching hospitals since the introduction of VQ single photon emission computed tomography (SPECT) scanning in 2010, at the same time as the medical community became increasingly aware of high radiation doses from rapidly escalating referrals for CT scanning. This may explain the rise in referrals for VQS seen during 2010, although this was not accompanied by any downturn in referrals for CTPA.
The increased number of imaging referrals for CTPA in our hospitals reflects a similar growth in referrals for CT scans in the US, particularly from emergency departments.18 We did not measure the increased radiation burden to patients as a result of this switch in referral patterns, although annual population radiation burden from diagnostic imaging is rising steeply and is now at about the level received from background radiation at sea level.19
The increase in referrals for PE-related imaging was associated with increased hospital separations but no decline in the statewide death rate from PE, indicating increased detection of low-risk PE. A similar phenomenon has been observed in the United Kingdom20 and in the US.9 Indeed, technological advances in both CTPA and VQS have permitted detection of small, clinically insignificant emboli in low-risk patients.21 It has been suggested that many of the small clots seen in the pulmonary arteries during CTPA are physiological, with the lung capillary beds trapping and dissolving emboli by endogenous fibrinolysis, thereby protecting the systemic circulation.22 In addition to unnecessary irradiation, the overdiagnosis of clinically insignificant PE is almost certainly associated with unnecessary complications of anticoagulant therapy,9 although we did not assess this in our study.
1 Number of requests for D-dimer level and referrals for leg ultrasound, VQS and CTPA at four Western Australian teaching hospitals, 2002–2010
3 Number of referrals for D-dimer testing and VTE-related and PE-related imaging in four WA teaching hospitals, 2002-2010
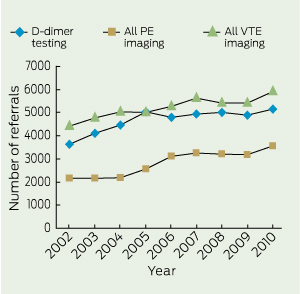
PE = pulmonary embolism. VTE = venous thromboembolism. WA = Western Australia.
Received 22 June 2012, accepted 28 October 2012
- Tatiana Segard1
- William B G Macdonald2
- 1 Nuclear Medicine, Sir Charles Gairdner Hospital, Perth, WA.
- 2 Imaging West, Department of Health, Western Australia, Perth, WA.
We thank Andrew Campbell for his assistance with statistical analysis, and the data custodians of the WA Department of Health and the WA Registry of Births, Deaths and Marriages for provision of the data.
William Macdonald is a member of the editorial board of Diagnostic Imaging Pathways and provides advice regarding nuclear medicine imaging. He receives no payment for this work.
- 1. Roy PM, Meyer G, Vielle B, et al. Appropriateness of diagnostic management and outcomes of suspected pulmonary embolism. Ann Intern Med 2006; 144: 157-164.
- 2. Bairstow PJ, Persaud J, Mendelson R, Nguyen L. Reducing inappropriate diagnostic practice through education and decision support. Int J Qual Health Care 2010; 22: 194-200.
- 3. Roy PM, Durieux P, Gillaizeau F, et al. A computerized handheld decision-support system to improve pulmonary embolism diagnosis: a randomized trial. Ann Intern Med 2009; 151: 677-686.
- 4. Wells PS, Anderson DR, Rodger M, et al. Excluding pulmonary embolism at the bedside without diagnostic imaging: management of patients with suspected pulmonary embolism presenting to the emergency department by using a simple clinical model and d-dimer. Ann Intern Med 2001; 135: 98-107.
- 5. Righini M, Perrier A, De Moerloose P, Bounameaux H. D-Dimer for venous thromboembolism diagnosis: 20 years later. J Thromb Haemost 2008; 6: 1059-1071.
- 6. Government of Western Australia, Department of Health. Diagnostic Imaging Pathways: a clinical decision support tool and educational resource for diagnostic imaging. http://www.imaging pathways.health.wa.gov.au (accessed Sep 2012).
- 7. Australian Bureau of Statistics. Australian demographic statistics. Table 4. Estimated resident population, states and territories (number). (ABS Cat. No. 3101.0.) http://www.ausstats.abs.gov.au/ausstats/ABS@ Archive.nsf/0/3042DF15A46B22D6CA25796 8000D0C57/$File/310104.xls#A2060847T (accessed Feb 2012).
- 8. Le Gal G, Bounameaux H. Diagnosing pulmonary embolism: running after the decreasing prevalence of cases among suspected patients. J Thromb Haemost 2004; 2: 1244-1246.
- 9. Wiener RS, Schwartz LM, Woloshin S. Time trends in pulmonary embolism in the United States: evidence of overdiagnosis. Arch Intern Med 2011; 171: 831-837.
- 10. Bounameaux H, Slosman D, de Moerloose P, Reber G. Diagnostic value of plasma D-dimer in suspected pulmonary embolism. Lancet 1988; 2: 628-629.
- 11. Kohn MA, Kwan E, Gupta M, Tabas JA. Prevalence of acute myocardial infarction and other serious diagnoses in patients presenting to an urban emergency department with chest pain. J Emerg Med 2005; 29: 383-390.
- 12. Ho WK, Hankey GJ, Eikelboom JW. The incidence of venous thromboembolism: a prospective, community-based study in Perth, Western Australia. Med J Aust 2008; 189: 144-147. <MJA full text>
- 13. Douma RA, Kessels JB, Buller HR, Gerdes VE. Knowledge of the D-dimer test result influences clinical probability assessment of pulmonary embolism. Thromb Res 2010; 126: e271-e275.
- 14. Goldstein NM, Kollef MH, Ward S, Gage BF. The impact of the introduction of a rapid D-dimer assay on the diagnostic evaluation of suspected pulmonary embolism. Arch Intern Med 2001; 161: 567-571.
- 15. Smith C, Mensah A, Mal S, Worster A. Is pretest probability assessment on emergency department patients with suspected venous thromboembolism documented before SimpliRED D-dimer testing? CJEM 2008; 10: 519-523.
- 16. Jones P, Elangbam B, Williams NR. Inappropriate use and interpretation of D-dimer testing in the emergency department: an unexpected adverse effect of meeting the “4-h target”. Emerg Med J 2010; 27: 43-47.
- 17. The PIOPED Investigators. Value of the ventilation/perfusion scan in acute pulmonary embolism. Results of the prospective investigation of pulmonary embolism diagnosis (PIOPED). JAMA 1990; 263: 2753-2759.
- 18. Larson DB, Johnson LW, Schnell BM, et al. National trends in CT use in the emergency department: 1995-2007. Radiology 2011; 258: 164-173.
- 19. Mettler FA Jr, Bhargavan M, Faulkner K, et al. Radiologic and nuclear medicine studies in the United States and worldwide: frequency, radiation dose, and comparison with other radiation sources — 1950-2007. Radiology 2009; 253: 520-531.
- 20. Burge AJ, Freeman KD, Klapper PJ, Haramati LB. Increased diagnosis of pulmonary embolism without a corresponding decline in mortality during the CT era. Clin Radiol 2008; 63: 381-386.
- 21. Glassroth J. Imaging of pulmonary embolism: too much of a good thing? JAMA 2007; 298: 2788-2789.
- 22. Suh JM, Cronan JJ, Healey TT. Dots are not clots: the over-diagnosis and over-treatment of PE. Emerg Radiol 2010; 17: 347-352.





Abstract
Objective: To determine trends in referral for venous thromboembolism (VTE) imaging in Western Australian teaching hospitals.
Design and setting: Retrospective audit of the WA picture archiving and communication system, PathWest Laboratory Medicine records, the hospital morbidity database at the four adult teaching hospitals in Perth, WA, and the WA death registry.
Patients: All patients referred for VTE-related imaging, and all hospital separations for pulmonary embolism (PE) during 2002–2010.
Main outcome measures: Number of referrals for computed tomography pulmonary angiography (CTPA), ventilation–perfusion lung scintigraphy, leg ultrasound and plasma D-dimer assay; hospital separations for PE and deaths from PE.
Results: Referrals for VTE-related imaging increased by 34%, while PE-related imaging increased by 65% during the study period, owing entirely to referrals for CTPA, which increased by more than 500%. The number of hospital separations for PE increased by 45% over the same period and the prevalence of PE among referred patients fell from 22.1% in 2002 to 19.5% in 2010. There was no fall in the death rate from PE in WA during the study period (P = 0.19). The number of D-dimer tests performed in the same hospitals increased by 42% over the study period.
Conclusions: The increased number of referrals for PE-related imaging resulted in more diagnoses but no reduction in deaths from PE in WA. Widespread D-dimer testing did not reduce referrals for imaging and is likely to have resulted in increased referrals. Increased imaging leads to overdiagnosis of clinically insignificant PE, and alternative strategies are required to reduce PE death rates.