Cardiovascular disease (CVD) in Australia, as in most developed countries, is the leading cause of death and one of the greatest burdens on the economy.1 While death rates from myocardial infarction are decreasing in Australia, the prevalence of CVD is increasing because of the combined effect of an ageing population, high levels of obesity and diabetes, and longer life expectancies. Additional contributing factors are rapidly changing dietary patterns and increasing rates of sedentariness.2 Phase II (outpatient) cardiac rehabilitation (CR) programs attempt to address these and other factors contributing to poor cardiovascular health3 through individualised medical evaluation, “prescribed” exercise, cardiac risk factor modification, education, counselling and psychological support.
Traditionally, CR programs take place in hospitals or other community centres and are delivered by a multidisciplinary team. Despite overwhelming evidence supporting the effectiveness of such programs,4,5 referral and uptake rates remain poor. Recent data (2003–2005) showed that only 11% of patients across Australia were referred to CR at hospital discharge after a CVD event.6 Moreover, fewer than 20% of all eligible patients complete a CR program in Queensland7 and New South Wales,8 and similarly low rates have been reported in other developed countries.9
A variety of patient, provider, system and community factors contribute to these poor utilisation rates.10 Most importantly, patients find it difficult to attend CR programs, and the traditional mode of delivery of these programs is often quite inconvenient for patients recovering from a heart attack.
Home-based CR programs, developed since the early 1980s,11 have the potential to overcome some of these barriers. Studies of home-based CR models providing telephone or internet support have shown effective risk-factor reduction and positive behavioural outcomes,12,13 as well as cost-effectiveness,14 compared with community-based programs. However, the capabilities of information and communication technologies (ICT) have so far not been fully exploited for this purpose.
We describe here the application of ICT in a recently developed CR model,15 and report on the acceptance of the use of these technologies, from both the patient and the provider perspective, based on the preliminary results of a randomised controlled trial currently underway.
Advanced multimedia communication capabilities of mobile phones, and the widespread availability of broadband networks and the internet, have created exceptional opportunities for interaction between patients and health care professionals. Evidence for the feasibility and effectiveness of mobile-phone applications in the management of asthma, diabetes, heart disease, leg ulcers, sleep apnoea and smoking cessation has been reviewed,16 and recent studies confirmed the feasibility of this method for weight reduction,17 managing the side effects of chemotherapy,18 and maintaining an exercise program for patients with chronic obstructive pulmonary disease.19 Of particular significance was a study of telemonitoring of patients with heart failure via mobile phones that showed effective reduction in the frequency and duration of hospitalisations.20 Web-based applications endow health care providers with additional tools for monitoring and interfacing with patients effectively across distances to produce favourable behavioural outcomes.21
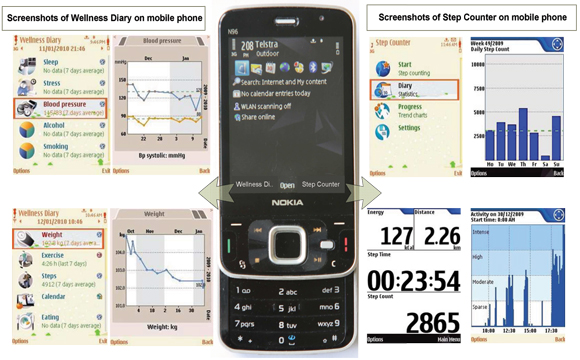
Box 1 describes the core CR components22 and corresponding delivery mechanisms of the CAP program using ICT. Similar to traditional CR programs, initial assessment is conducted face-to-face. At this assessment, patients receive basic information about CVD and are evaluated for planned biomedical, pharmacological and lifestyle management interventions. Patients are given a Nokia N96 smartphone with an integrated accelerometer sensor, Step Counter software to measure physical exercise, and a Wellness Diary application23 into which patients enter their health information. They are also supplied with a blood pressure monitor and scales to measure body weight. The patients enter information daily into the Wellness Diary about their exercise, stress and anxiety levels, their sleep pattern, smoking, alcohol use, diet, and weight and blood pressure levels. Step Counter data are automatically transferred to the Wellness Diary.
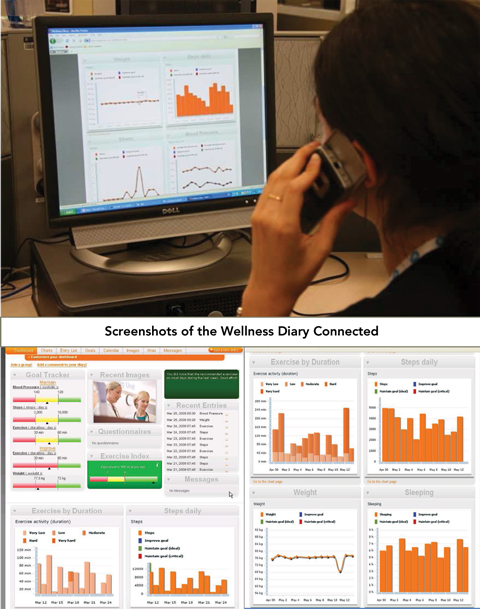
Box 2 shows the smartphone and screenshots from the Step Counter and Wellness Diary. All data are synchronised to a remote server hosting a Wellness Diary Connected web portal.24 Mentors view and assess patients’ measurements and health data on the portal (Box 3) and use this information for individual feedback and goal setting during weekly telephone mentoring sessions. Should they wish to, patients are able to access their own collected information on the Wellness Diary Connected web portal for self-management.
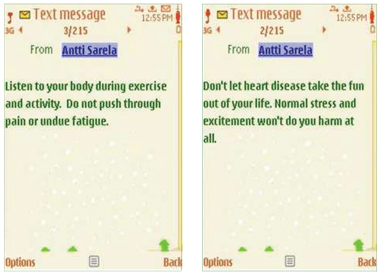
Mobile-phone video and teleconferencing are used for continuous psychological and psychosocial mentoring. Daily motivational text messages (Box 4) are sent to the patients, and pre-stored relaxation audio files and educational multimedia content are provided on the phone for scheduled listening and viewing, respectively. As in traditional CR programs, the patients receive a face-to-face review assessment after 6 weeks.
Results of preliminary data showed that the average usage rate for the Wellness Diary on the mobile phone was 91.5%, which indicates missed data entries for 3–4 days over 6 weeks. When automatic steps logged via the Step Counter are included, the average usage rate increased to 97%, and non-entry was reduced to just 1 day over the 6-week period. The individual variables entered in the Wellness Diary are shown in Box 5.
1 Core components of cardiac rehabilitation (CR) and ways of delivering these components through the Care Assessment Platform (CAP)
- Marlien Varnfield1
- Mohanraj K Karunanithi1
- Antti Särelä1
- Elsa Garcia1
- Anita Fairfull2
- Brian F Oldenburg3
- Darren L Walters4
- 1 Australian e-Health Research Centre, CSIRO ICT Centre, Brisbane, QLD.
- 2 Rehabilitation and Consultation Service, Primary and Community Health Services, Metro North Health Service District, Brisbane, QLD.
- 3 Faculty of Medicine, Nursing and Health Sciences, Monash University, Alfred Hospital, Melbourne, VIC.
- 4 Department of Cardiology, Prince Charles Hospital, Brisbane, QLD.
We acknowledge the contribution of Nokia Research, Telstra, Multi-ed Medical, Mega Electronics, and the Australian Cardiovascular Health and Rehabilitation Association for the devices, software, phone plans and material used in the trial, and training. We thank the project group, clinicians and management at the Australian e-Health Research Centre, and Primary and Community Health Services of the Metro North Health Service District of Queensland Health.
None identified.
- 1. Heart Foundation of Australia. Cardiovascular disease statistics. http://www.heartfoundation.org.au/Heart_Information/Statistics/Pages/default.aspx (accessed Oct 2009).
- 2. Beilin L, Huang RC. Childhood obesity, hypertension, the metabolic syndrome and adult cardiovascular disease. Clin Exp Pharmacol Physiol 2008; 35: 409-411.
- 3. Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004; 364: 937-952.
- 4. Jolliffe JA, Rees K, Taylor RS, et al. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2001; (1): CD001800.
- 5. Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med 2004; 116: 682-692.
- 6. Walters DL, Aroney CN, Chew DP, et al. Variations in the application of cardiac care in Australia. Med J Aust 2008; 188: 218-223. <MJA full text>
- 7. Scott IA, Lindsay KA, Harden HE. Utilisation of outpatient cardiac rehabilitation in Queensland. Med J Aust 2003; 179: 341-345. <MJA full text>
- 8. Johnson NA, Inder KJ, Nagle AL, Wiggers JH. Secondary prevention among cardiac patients not referred to cardiac rehabilitation [letter]. Med J Aust 2009; 190: 161. <MJA full text>
- 9. Thomas RJ. Cardiac rehabilitation/secondary prevention programs: a raft for the rapids: why have we missed the boat? Circulation 2007; 116: 1644-1646.
- 10. Jolly K, Taylor R, Lip GY, et al. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess 2007; 11: 1-118.
- 11. Miller NH, Haskell WL, Berra K, DeBusk RF. Home versus group exercise training for increasing functional capacity after myocardial infarction. Circulation 1984; 70: 645-649.
- 12. Castro CM, Kind AC. Telephone assisted counseling for physical activity. Exerc Sport Sci Rev 2002; 30: 64-68.
- 13. Neubeck L, Redfern J, Fernandez R, et al. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review. Eur J Cardiovasc Prev Rehabil 2009; 16: 281-289.
- 14. Taylor RS, Watt A, Dalal HM, et al. Home-based cardiac rehabilitation versus hospital-based rehabilitation: a cost effectiveness analysis. Int J Cardiol 2007; 119: 196-201.
- 15. Walters DL, Särelä A, Fairfull A, et al. A mobile phone-based care model for outpatient cardiac rehabilitation: the care assessment platform (CAP). BMC Cardiovasc Disord 2010; 10: 5.
- 16. Dellifraine JL, Dansky KH. Home-based telehealth: a review and meta-analysis. J Telemed Telecare 2008; 14: 62-66.
- 17. Patrick K, Raab F, Adams MA, et al. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res 2009; 11: e1.
- 18. Weaver A, Young AM, Rowntree J, et al. Application of mobile phone technology for managing chemotherapy-associated side-effects. Ann Oncol 2007; 18: 1887-1892.
- 19. Nguyen HQ, Gill DP, Wolpin S, et al. Pilot study of a cell phone-based exercise persistence intervention post-rehabilitation for COPD. Int J Chron Obstruct Pulmon Dis 2009; 4: 301-313.
- 20. Scherr D, Kastner P, Kollmann A, et al. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. J Med Internet Res 2009; 3: e34.
- 21. Murray E, Burns J, See TS, et al. Interactive health communication applications for people with chronic disease (review). Cochrane Database Syst Rev 2009; (1): CD004274. http://onlinelibrary.wiley.com/o/cochrane/clsysrev/articles/CD004274/frame.html (accessed Nov 2010).
- 22. Balady GJ, Williams MA, Ades PA, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation 2007; 115: 2675-2682.
- 23. Mattila E, Parkka J, Hermersdorf M, et al. Mobile diary for wellness management — results on usage and usability in two user studies. IEEE Trans Inf Technol Biomed 2008; 12: 501-512.
- 24. Särelä A, Korhonen I, Salminen J, et al. A home-based care model for outpatient cardiac rehabilitation based on mobile technologies. Proceedings of the 3rd International Conference on Pervasive Computing Technologies for Healthcare; 2009 Apr 1–3; London, UK: IEEE Press.





Abstract
The prevalence of cardiovascular disease, a major cause of disease burden in Australia and other developed countries, is increasing due to a rapidly ageing population and environmental, biomedical and modifiable lifestyle factors.
Although cardiac rehabilitation (CR) programs have been shown to be beneficial and effective, rates of referral, uptake and utilisation of traditional hospital or community centre programs are poor.
Home-based CR programs have been shown to be as effective as centre-based programs, and recent advances in information and communication technologies (ICT) can be used to enhance the delivery of such programs.
The Care Assessment Platform (CAP) is an integrated home-based CR model incorporating ICT (including a mobile phone and the internet) and providing all the core components of traditional CR (education, physical activity, exercise training, behaviour modification strategies and psychological counselling).
The mobile phone given to patients has an integrated accelerometer and diary application for recording exercise and health information. A central database, with access to these data, allows mentors to assess patients’ progress, assist in setting goals, revise targets and give weekly personal feedback.
Mentors find the mobile-phone modalities practical and easy to use, and preliminary results show high usage rates and acceptance of ICT by participants.
The provision of ICT-supported home-based CR programs may enable more patients in both metropolitan and remote settings to benefit from CR.