The link between poor hand hygiene of health care workers (HCWs) and the spread of infection in hospitals has been known and widely promulgated for the past 150 years,1,2 and a causal link between good hand hygiene and reduced risk of nosocomial infection has been demonstrated.3 Yet multiple studies have documented the poor compliance of HCWs with hand hygiene practices.4 With increasing rates of infection and morbidity associated with multiresistant organisms (MROs) in hospitals, hand hygiene has become a key patient safety issue worldwide.5,6 In 2005, the World Health Organization launched the first Global Patient Safety Challenge, Clean care is safer care,6 and Australia pledged its commitment to the cause the following year.7 The Clinical Excellence Commission (CEC), established in 2004 by the New South Wales Minister for Health, implemented a statewide campaign in 2005 to make hand hygiene a top priority in all public hospitals in NSW. The CEC saw the issue of hand hygiene to be closely aligned with its mission to build confidence in the NSW health care system by making it demonstrably better and safer for patients and a more rewarding workplace for staff.8
Compliance with hand hygiene guidelines is a remarkably complex issue that relies on a combination of education and training and is influenced by deeply held personal beliefs and the behaviour of peers and superiors.9,10 A number of studies have described efforts to improve hand hygiene, with most citing “success rates” of compliance of no more than 61%, and fewer sustaining the improvement beyond the life of the initial intervention phase.4,11-13
In 1997, Larson and colleagues described the implementation of a multifaceted approach to changing hand-washing behaviour.14 Pittet’s 2001 model from the Infection Control Program of the University of Geneva hospitals demonstrated the value of clinical champions, a “talking walls” poster campaign, and a system of monitoring adherence to hand hygiene practices involving feedback to staff on their performance.4 The CEC-led campaign described here borrowed from the successes of these two models and other initiatives, including the cleanyourhands campaign of the National Health Service in the United Kingdom,4,7,15,16 to implement a statewide multifaceted approach to incorporating hand hygiene into everyday clinician behaviour. We describe the planning and execution of this campaign.
A detailed description of the planning phase of the project is documented elsewhere.17 Campaign methods and standardised audits were used to maximise the reach of the campaign in a systematised manner to all HCWs across the state. Clinical practice improvement techniques were used, based on the historical work by Deming in the 1950s for process improvements in industry and adapted for experienced medical and nursing clinicians.18 The project had the support and approval of the NSW Department of Health (NSW Health).
Integral to all change management programs is identifying organisational support to implement the change and help develop an understanding of the current climate in which the change is to be made.19 The available NSW data on MRO infections were examined, and a pre-intervention survey was administered to all authorities via their network of infection control professionals to assess the current level of activity on hand hygiene.
The principal objectives of the project were:
Authorities were provided with evidence from the WHO guidelines on hand hygiene in health care supporting the provision of AHR in near-patient locations as the key to helping staff decontaminate their hands.6 Additional evidence was given that AHR is more effective, less drying of skin and quicker to use than soap and water.20
The tendency of clinicians to model their behaviour on that of peers and colleagues is well known.21 Thus, engaging local champions and leaders from among the ward staff was promoted as one of the key aims of the intervention. Local champions and leaders were chosen by individual hospitals and wards. The leaders were briefed by the project officer about their expected role in supporting the project — leading by example, promoting hand hygiene to their peers, and displaying posters with photographs of clinical leaders and a supportive message about the project in ward areas.
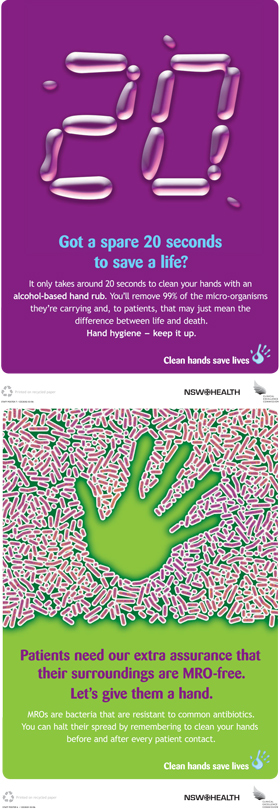
Using the slogan Clean hands save lives and a distinctive logo (Box 1), a social marketing approach was used to promote the campaign. A graphic design agency was engaged early in this phase to develop marketing collateral to support the campaign objectives. Posters targeting key facilitators of and barriers to hand hygiene22 were promoted in a strategy modelled on the successful Geneva campaign.4 In addition to project funding from the CEC, NSW Health provided funding for campaign materials.
Consumer engagement in health care is a key priority of the NSW health care system for all patient care issues,23 and hand hygiene was identified as an appropriate health care subject on which to engage them. Campaign resources specifically targeting consumers — including posters and a patient information brochure — were developed. Staff were encouraged to engage patients and visitors in the campaign, and wore campaign T-shirts and badges with the campaign logo saying “It’s OK to ask” to encourage patients and visitors to ask HCWs about their compliance with hand hygiene practices.
The power of data to drive change is a well recognised clinical practice improvement technique. A simple audit tool was developed to ensure that the burden of data collection was minimised and local ownership of the data (and thereby “the problem”) was maximised. The tool, based on Fulkerson’s risk categories,23 differentiated between high, medium and low risk for infection transfer. As auditing was seen as the province of all clinicians, not just infection control or project personnel, instructions on use of the tool were given to every ward.
The CEC developed a detailed resource guide, based on the cleanyourhands campaign in the UK,16 and a clear implementation plan for local project officers. The project officers’ role was to ensure that campaign strategies were implemented in concert across the state and that appropriate data and reporting requirements were met. Monthly progress reports were tracked against project objectives, including placement of AHR, staff and patient surveys, audit activities, and engagement of staff champions. Project officers reported to their authority and the CEC on the milestones for implementing campaign objectives and issues or problems encountered in individual hospitals. Reports of hand hygiene compliance rates were fed back to staff at ward level.
Results of the hand hygiene compliance audit are reported in detail elsewhere,24 as are results of the patient and staff surveys25 and secondary outcomes relating to infection with MROs.26
The placement of AHR in near-patient locations was evaluated by audits of product placement conducted before and after the campaign in 10 of the 11 authorities (Box 2). (The audit was not relevant to the Ambulance Service of NSW, which had AHR available in all its mobile vehicles.)
Hospital visits before the campaign identified a lack of appropriately placed AHR at the point of care. By the end of the campaign, there were 13 280 AHR containers available in NSW health facilities. The number of AHR containers per available bed (expressed as a percentage of available beds) ranged from 44% (1488/3363) to 142% (380/268), with a state average of 70% (13 280/18 951) (Box 2). Of the AHR containers available at the bedside, 70% (9254/13 280) were secured in brackets and the rest were unsecured, predominantly on patient drawers, medication trolleys or blood pressure trolleys. The audit did not include non-secure products carried with staff while on the ward.
Although 73% of respondents to the pre-implementation survey reported already using AHR at the point of patient care, the use of AHR, based on purchasing patterns, increased during the campaign from 1477 L in February 2006 to 5568 L in February 2007.17
Concerns were also raised through the project officers about systemic absorption of AHR and the potential to contravene blood alcohol driving regulations for staff engaged in home visiting (community health workers) and for pregnant staff members, for whom alcohol consumption is contraindicated. Coincidentally, during the campaign, a safety alert from the United States was broadcast via the Internet about the risk to HCWs of shock or burn from vigorous application of AHR while generating a static electrical charge on synthetic carpet floors. Such concerns were dispelled through promulgation of relevant information.27,28
Campaign materials developed to support the objectives and key messages of the campaign included T-shirts and balloons with the campaign logo, staff and patient information brochures, posters with 15 different messages (Box 3), and a website (http://www.cec.health.nsw.gov.au/programs/clean-hands.html). Messages displayed by the campaign materials emphasised the ease of use and effectiveness of AHR in minimising spread of infection and dispelled myths about the spread of MROs.
Resistance to change is a significant barrier to any improvement strategy. When the necessary change challenges personal behaviour and deeply held (often subconscious) beliefs, resistance is likely to be strong. The hand hygiene behaviour of HCWs is likely to be the product of lessons learned in childhood, and has been described by Whitby and colleagues as either “inherent” or “elective”.15 That is, HCWs make a decision as to whether or not to comply with hand hygiene practices based on personal beliefs and a perception of the risk that the patient poses to them. Rather than reconstruct the psychological paradigm of a practice developed during childhood, we chose to challenge HCWs to disregard their self-protective perception in elective hand hygiene behaviour by using a campaign approach to begin systematising the practice. The issue of the personal development of hand hygiene practice is explored in depth elsewhere.15,29
The strategies employed also mirrored the hierarchy of error reduction strategies as described by Canada’s Institute for Safe Medication Practices (Box 4).30 Lower-order strategies used included education, provision of information, and development of rules and polices. There was standardisation of the message of practice, with overt observation audits emphasising the need to follow hand hygiene practices before and after patient care activities. The near-patient location of AHR, with products secured by brackets in these locations wherever possible, constituted “forcing functions and constraints”.
A hand hygiene campaign was recently rolled out in 75 hospitals in Victoria.31 The campaign correlated the supply of AHR with hand hygiene rates to establish a trend in rates. Although this method may not be reliable, especially in the winter months (when HCWs are less inclined to use AHR or wash with cold water), we believe the measurement indicates that the crucial element of the campaign — making AHR available at the point of care — was successful. Our February 2007 audits showed that, on average, 70% of available beds had AHR either secured near the bed or unsecured but located close to the bed or point of care.
In a 1994 discussion of medical error, Leape advised that proven error reduction strategies needed to be applied at every stage of clinical practice, and reminded the health care profession of Florence Nightingale’s dictum, “first do no harm”.32 Four years later, Vincent and colleagues applied a “human factors” model to the analysis of risk and safety in clinical medicine and postulated that some quality and safety initiatives may have limited impact because they rely on only one level of intervention, such as training or protocol development.33 It is now recognised that the impact of safety initiatives is directly related to a hierarchy of multiple strategies,30 and that a multifaceted approach improves the chances of success in implementing change.
The primary aim of the Victorian campaign31 was reducing infection with methicillin-resistant Staphylococcus aureus. Our campaign was all about engagement — of participants, consumers and leaders — to facilitate change. In our campaign, levels of engagement were variable within and between the organisations involved. Engagement at the executive level, to fast-track recruitment of project officers (on whom the campaign was heavily reliant), was often hard to achieve and even harder to maintain, with only one project officer remaining in the dedicated role throughout the campaign.
During the early stages of organisational culture change, dedicated champions are pivotal to maintaining targeted behaviour. The less-than-optimal rates of hand hygiene compliance observed in our study may reflect the low retention rate of dedicated project officers. A similar pattern was apparent in the Victorian campaign, with hand hygiene compliance rates dropping during periods of absence of key staff.31 Executive support for the short-term increase in expenditure on AHR was also required, yet some executives found this easier to achieve than others. Engagement of clinical leaders, especially doctors, was also variable. The failure to consistently model appropriate behaviour may explain why hand hygiene rates among doctors remained poor.29 With more than 108 000 people working in the NSW health care system, the majority in clinical roles, there were challenges and complexities in embarking on a large-scale program to systematise and standardise what is essentially personal behaviour and thereby change the culture of busy clinicians.
- Annette C Pantle1
- Kimberley R Fitzpatrick1
- Mary-Louise McLaws2
- Clifford F Hughes1
- 1 Clinical Excellence Commission, Sydney, NSW.
- 2 Hospital Infection Epidemiology and Surveillance Unit, School of Public Health and Community Medicine, University of New South Wales, Sydney, NSW.
Our project was a joint initiative of the CEC and NSW Health.
Mary-Louise McLaws has joined the WHO First Global Patient Safety Challenge pilot country project to provide epidemiological advice. Clifford Hughes operates the Australia and New Zealand Heart Valve Registry, which tracks patients with a Björk-Shiley convexo/concave heart valve. He distributes guidelines to these patients through their doctors as developed by the medical supervisory panel of the Bowling–Pfizer Heart Valve Settlement. He is the Principal Investigator of the On-X Heart Valve Study in Australia, for which On-X Life Technologies pays the expenses. He has received funding from Roche Diagnostics for travel expenses to attend meetings.
- 1. Semmelweis IF. The etiology, the concept and the prophylaxis of childbed fever. In: Pest CA, editor. Hartleben’s Verlag-Expedition, 1861. [Translated by Murphy FP; republished Birmingham: Classics of Medicine Library, 1981].
- 2. Best M, Nuehauser D. Ignaz Semmelweis and the birth of infection control. Qual Saf Health Care 2004; 13: 233-234.
- 3. Aiello AE, Larson EL. What is the evidence for a causal link between hygiene and infections? Lancet Infect Dis 2002; 2: 103-110.
- 4. Pittet D. Improving adherence to hand hygiene practice: a multidisciplinary approach. Emerg Infect Dis 2001; 7: 234-240.
- 5. Institute for Healthcare Improvement. How-to guide: improving hand hygiene. A guide for improving practices among health care workers. http://www.shea-online.org/Assets/files/IHI_Hand_Hygiene.pdf (accessed Mar 2009).
- 6. World Health Organization. WHO guidelines on hand hygiene in health care (advanced draft): a summary. Clean hands are safer hands. Geneva: WHO, 2005. http://www.who.int/patientsafety/events/05/HH_en.pdf (accessed Mar 2009).
- 7. Halton J. [Pledge to reduce health care-associated infection.] http://www.who.int/gpsc/statements/Australia_pledge.pdf (accessed Mar 2009).
- 8. Clinical Excellence Commission, NSW Health. Directions statement. Sydney: NSW Health, 2004. http://www.cec.health.nsw.gov.au/pdf/directions_sment.pdf (accessed Aug 2009).
- 9. Snow M, White GL Jr, Alder SC, Stanford JB. Mentor’s hand hygiene practices influence student’s hand hygiene rates. Am J Infect Control 2006; 34: 18-24.
- 10. Goldman D. System failure versus personal accountability — the case for clean hands. N Engl J Med 2006; 355; 121-123.
- 11. Whitby M, McLaws M. Handwashing in healthcare workers: accessibility of sink location does not improve compliance. J Hosp Infect 2004; 58: 247-253.
- 12. Bahal A, Karamchandani D, Fraise A, McLaws M. Hand hygiene compliance: universally better post-contact than pre-contact in healthcare workers in the UK and Australia. Br J Infect Control 2007; 8: 24-28.
- 13. Tibballs J. Teaching hospital medical staff to hand wash. Med J Aust 1996; 164: 395-398. <MJA full text>
- 14. Larson EL, Bryan JL, Adler LM, Blane C. A multifaceted approach to changing handwashing behavior. Am J Infect Control 1997; 25: 3-10.
- 15. Whitby M, McLaws M, Ross MW. Why healthcare workers don’t wash their hands: a behavioural explanation. Infect Control Hosp Epidemiol 2006; 27: 484-492.
- 16. National Patient Safety Agency, National Health Service. Flowing with the go: the complete year two campaign maintenance handbook for cleanyourhands partner trusts. The sequel to Ready, steady, go. London: NPSA, 2006. http://www.library.nhs.uk/healthmanagement/ViewResource.aspx?resID=271362 (follow link under “cleanyourhands campaign”) (accessed Mar 2009).
- 17. Clinical Excellence Commission, NSW Health. Clean hands save lives: final report of the NSW Hand Hygiene Campaign. Sydney: NSW Health, 2007. http://www.cec.health.nsw.gov.au/moreinfo/cleanhands_report.html (accessed Aug 2009).
- 18. Langley GJ, Nolan KM, Nolan TW, Provost LP. The improvement guide: a practical approach to enhancing organizational performance. New York: Jossey-Bass, 1996.
- 19. Weinstein R. Hand hygiene — of reason and ritual. Ann Intern Med 2004; 141: 65-66.
- 20. Boyce J, Kelliher S, Vallande N. Skin irritation and dryness associated with two hand-hygiene regimes: soap-and-water hand washing versus hand antisepsis with an alcoholic hand gel. Infect Control Hosp Epidemiol 2000; 21: 442-448.
- 21. Pittet D, Simon A, Hugonnet S, et al. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med 2004; 141: 1-9.
- 22. NSW Health. Strategic directions for health 2000–2005. Sydney: NSW Health, 2000.
- 23. Rotter ML. Hand washing and hand disinfection. In: Mayhall CG, editor. Hospital epidemiology and infection control. Baltimore: Williams and Wilkins, 1996: 1052-1068.
- 24. Fitzpatrick KR, Pantle AC, McLaws ML, Hughes CF. Culture change for hand hygiene: Clean hands save lives, Part II. Med J Aust 2009; 191 (8 Suppl): S13-S17. <MJA full text>
- 25. McLaws ML, Pantle AC, Fitzpatrick KR, Hughes CF. Improvements in hand hygiene across New South Wales public hospitals: Clean hands save lives, Part III. Med J Aust 2009; 191 (8 Suppl): S18-S25. <MJA full text>
- 26. McLaws ML, Pantle AC, Fitzpatrick KR, Hughes CF. More than hand hygiene is needed to affect methicillin-resistant Staphylococcus aureus clinical indicator rates: Clean hands save lives, Part IV. Med J Aust 2009; 191 (8 Suppl): S26-S31. <MJA full text>
- 27. Ego Pharmaceuticals. Material safety data sheet: aqium gel. http://www.cleanroom.com.au/pdfs/Hand_Hygiene/MSDS_Aqium_Gel_09-08-07.pdf (accessed Mar 2009).
- 28. Turner P, Saeed B, Kelsey MC. Dermal absorption of isopropyl alcohol from a commercial hand rub: implications for its use in hand decontamination. J Hosp Infect 2004; 56: 287-290.
- 29. Sax H, Uçkay I, Richet H, et al. Determinants of good adherence to hand hygiene among healthcare workers who have extensive exposure to hand hygiene campaigns. Infect Control Hosp Epidemiol 2007; 28: 1267-1274.
- 30. Institute for Safe Medication Practices. ISMP medication safety alert. Medication error prevention toolbox. http://www.ismp.org/newsletters/acutecare/articles/19990602.asp (accessed Mar 2009).
- 31. Grayson ML, Jarvie LJ, Martin R, et al. Significant reductions in methicillin-resistant Staphylococcus aureus bacteraemia and clinical isolates associated with a multisite, hand hygiene culture-change program and subsequent successful statewide roll-out. Med J Aust 2008; 188: 633-640. <MJA full text>
- 32. Leape L. Error in medicine. JAMA 1994; 272: 1851-1857.
- 33. Vincent C, Taylor-Adams S, Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ 1998; 316: 1154-1157.






Abstract
Objective: To describe the planning and execution of a statewide campaign aimed at improving compliance with hand hygiene practices in New South Wales public hospitals.
Design and setting: The campaign was conducted in all area health services (AHSs) in NSW (covering 208 public hospitals) between February 2006 and February 2007. Clinical practice improvement methods and campaign strategies were used to improve the availability and use of alcohol-based hand rub (AHR) at the point of patient care, using staff champions and local leaders, engaging patients and families, and measuring compliance. Staff were given regular feedback on their performance. Project officers funded by the Clinical Excellence Commission (CEC) provided local project management support and implemented the campaign in a standardised format orchestrated by the CEC.
Main outcome measures: Proportion of available beds with secured and unsecured AHR containers nearby; amount of AHR used (based on purchasing patterns).
Results: Hospital visits before the campaign identified a lack of appropriately placed AHR at the point of care. The number of AHR containers per available bed in near-patient locations increased to 13 280/18 951 (70%) after the campaign. The quantity of AHR purchased per month across NSW public hospitals increased from 1477 L to 5568 L (a 377% increase).
Conclusion: The CEC was successful in systematising the placement of AHR in all NSW public hospitals at the point of patient care. Although the use of AHR increased substantially, some staff were resistant to changing their hand hygiene practices.