Australian doctors have a long tradition of serving the poor. Many individuals have made considerable contributions to the needs of underprivileged communities both here and abroad. Indeed, health is increasingly recognised as essential to the growth and sustainability of all nations.1 In recent years, medical students across Australia have begun to engage with the challenges of international health in new and innovative ways. Student international health organisations (SIHOs) have formed at most medical schools in response to a renewed interest in serving the needy. These groups demonstrate how an emphasis on global health may both enrich Australian medical schools and equip the next generation of doctors to be leaders in international health.
International health has featured in Australian medical schools for many years, primarily in the form of “elective terms” in developing countries. Students typically spend 6–8 weeks in supervised health care settings of their choice. The benefits of these elective terms have been well described.2-4
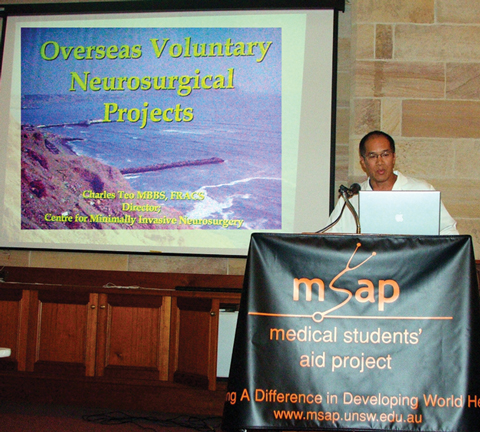
The Medical Students’ Aid Project (MSAP) formed in 2001 in response to the elective term experiences of students at the University of New South Wales.5 These students believed that their experiences in underprivileged nations demanded a collective response. They framed their approach as a “partnership”, recognising the benefits of the overseas experiences for students, and identifying a need for medical supplies at partner hospitals. MSAP quickly garnered support from the student body, university administration and private donors. Its initial success stemmed from the enthusiasm of its student leaders, the support of senior faculty members, regular meetings, and its focus on meeting specific, achievable needs. Now in its seventh year, MSAP continues as a forum for promoting international health and providing basic medical aid. In 2006, MSAP donated to hospitals in 14 countries, including Vanuatu, Ghana and Bolivia (Box 1).
Driven by similar interest, more than 10 not-for-profit student groups have formed in medical schools across Australia since 2001. We wrote to each SIHO chair in May this year, asking about their formation and function. A summary of responses is given in Box 2.
The SIHOs formed a national collaboration in 2005, with the creation of the International Health Network (IHN; http://ihealthnet.net/). Supported by the Australian Medical Students’ Association, the IHN provides a forum for sharing enthusiasm and ideas. It publishes a regular newsletter, hosts a website, and facilitates the Developing World Conference, which brings together more than 500 Australian medical students each year.
Other groups raise funds to support existing health care systems. HOPE (Griffith University) has supported the construction of a medical centre in Ghana (Box 3). Other organisations address determinants of poverty; for example, SANTE (James Cook University) has delivered pens, pencils and books to schools in Papua New Guinea.
Clearly, student organisations must remain mindful of any potential negative effects of their activities, and develop processes to ensure that donations are appropriate and delivered effectively.6 We believe it is vital to work in partnership with existing health care structures, to avoid creating parallel health systems and to respect local autonomy.
Student organisations have achieved great success in the university and broader community. SIHOs enhance community awareness by helping students, other health care workers, and the general public to engage with global health inequality. They also focus students’ attention upon the broader social, political and economic contexts of disease. In the past year, Ignite (Monash University) held a photo exhibition promoting international health awareness, and Insight (University of Adelaide) has held forums on HIV/AIDS and Women’s Health in the Middle East. MSAP holds an annual project launch, with invited keynote speakers (Box 4).
Australian SIHOs are coming of age; however, challenges remain (Box 5). Long-term sustainability is a key issue. SIHOs must develop structures to ensure continuity between successive student cohorts. Problems may arise if the organisation becomes too dependent on an individual or single year group, as corporate memory can be quickly lost. Established groups are facing the challenge of deciding how large they can become yet retain full-time student ownership. We believe that SIHOs must retain student ownership as a central value to retain the energy and dynamism that student autonomy brings.
The three most prominent functions of medical schools are teaching, research and clinical service.7 A fourth concern — social justice — often receives less attention. In 1995, the World Health Organization emphasised the importance of “social accountability” in medical schools, citing an “obligation to direct . . . education, research and service activities towards addressing the priority health concerns of the community, region, and/or nation they have a mandate to serve”. 8 Some authors argue that, when a society confers resources and privileges on medical schools, they must in turn serve the greater social good.9,10
Medical schools have a moral duty to prepare doctors who can care for Australia’s disadvantaged populations. As the world becomes more interdependent and aware of global health inequalities,11 wealthy nations such as Australia arguably also have a moral duty to consider the interests of their poorer regional neighbours.12
A curriculum that emphasises international health will facilitate teaching on many issues that are relevant to Australian medical practice. Houpt and colleagues have argued that medical schools must identify certain domains of international health competency that can be taught to all students.13 These include knowledge of the global burden of disease, travel medicine and immigrant health. Cross-cultural health and refugee health are highly relevant to caring for Australia’s immigrant community. International health also provides an excellent vehicle for promoting general principles of social justice. Schools may also develop additional elective subjects for students with a particular interest in global health. Teaching on public health, tropical medicine, anthropology, and human rights could also be expanded.14 Some important diseases, such as avian influenza and multidrug-resistant tuberculosis, require an understanding of public health principles at a global level. For these reasons, a former WHO Director-General has argued that “the separation between domestic and international health problems is no longer useful”.15
Students are increasingly seeking input into the design of curricula. Some authors have argued that medical schools “must listen to [medical students’] views as the consumers and purchasers of medical education”.13 A number of medical students training in Australia will return to low- and middle-income countries, and need to understand the diversity of health care settings. Further, many Australian students are keen to work in international settings during their early careers. Consequently, there is an increased demand for teaching of international health. Where medical schools endorse these approaches, they help students learn cross-cultural medicine, encourage idealism3 and inform students’ future careers.4
The educational needs of the general medical student body are distinct from those of students with a particular passion for international health. Australian medical schools can do much to help both groups (Box 6).
Medical schools in Sweden, the UK and the Netherlands have built international health into their curricula.12 In the United States, a consortium of 70 medical schools16 has appraised teaching of international health nationwide, and developed teaching modules to better promote a global health agenda. Medact, a UK group, has also developed communal curricular resources for global health teaching.12
In 2003, the Medical Deans of Australia and New Zealand identified a need to collaborate in regards to standards for electives in developing countries.17 However, the task remains incomplete. There is a great potential for this body to oversee guidelines that support Australia’s medical schools in providing integrated international health curricula. James Cook University illustrates how this might be done. Its offers a subject entirely devoted to international public health (Professor Craig Veitch, Professor of Rural Health, James Cook University, personal communication). James Cook University also maintains links with hospitals in East Timor, Papua New Guinea and Fiji, and provides scholarships for students on overseas electives.
There are many practical ways in which universities can support existing elective programs. Firstly, universities must ensure that they adequately prepare students before they leave and provide appropriate debriefing on return. Many universities provide administrative staff to support elective terms. Other valuable approaches by faculties across Australia include funding scholarships, subsidising vaccines or HIV starter packs, cataloguing previous students’ experiences, and recommending worthwhile destinations. Sydney University’s Hoc Mãi initiative with Vietnam exemplifies a sustainable program operated by a medical faculty to support students during their medical electives and build international cooperation.18
There is considerable scope for medical schools and postgraduate training programs to work together to stream students into careers in international health.19 With expanding graduate numbers in coming years, there is opportunity to develop innovative training pathways. Further research is also required to evaluate student interest and identify what particular skills are required for students and junior doctors to serve overseas long term.
3 Primary school children in Dabaa, Ghana, where HOPE (Griffith University) is supporting a new medical centre

5 Long-term challenges facing SIHOs
Transition of experience between each cohort of students.
Stability and long-term sustainability of funding.
Tension between desire for expansion and accepting the limitations of scale for a student organisation.
Outsourcing of fundraising (eg, to schools).
Managing corporate sponsorship ethically.
Acquiring tax-deductability status for donations.
Negotiating the interface with university and other charities.
Building an alumni network to ensure future support from doctors.
Strengthening the International Health Network.
Improving accountability for donated money.
6 How medical schools can promote international health14
Endorse, promote and mentor student international health organisations while supporting their autonomy.
Integrate global health topics into core medical curricula.
Offer courses on global public health and tropical medicine.
Offer various elective courses, such as medical anthropology, international development and health, or health and human rights.
Offer combined degree programs (eg, MD/PhD, MD/MPH) in global health.
Provide academic, logistic, and financial support for international rotations.
Establish a global health administrator or office within the medical school.
Form international partnerships with institutions in developing countries.
Create more scholarships and financial support for international exchanges.
Make an international clinical rotation a routine part of medical education.
- Gregory J Fox1
- James E Thompson2
- Victor C Bourke2
- Gregory Moloney3
- 1 Department of Respiratory Medicine, Royal Prince Alfred Hospital, Sydney, NSW.
- 2 University of New South Wales, Sydney, NSW.
- 3 Sydney Eye Hospital, Sydney, NSW.
We thank Professor Anthony Zwi, University of New South Wales.
None identified.
- 1. Ruger JP. Health and development. Lancet 2003; 362: 678.
- 2. Haq C, Rothenburg D, Gjerde C, et al. New world views: preparing physicians in training for global health work. Fam Med 2000; 32: 566-572.
- 3. Smith JK, Weaver DB. Capturing medical students’ idealism. Ann Fam Med 2006; 4 Suppl 1: S32-S37.
- 4. Ramsey AH, Haw C, Gjerde CL, et al. Career influence of an international health experience during medical school. Fam Med 2004; 35: 412-416.
- 5. Ritchie AG, Fung AT, Fox PN, et al. The Medical Students’ Aid Project: building partnerships with the developing world. Med J Aust 2002; 177: 641-643. <MJA full text>
- 6. Wenar L. Accountability in International Development Aid. Ethics Int Aff 2006; 20: 1-23.
- 7. Kamien M, Boelen C, Heck JE. Measuring the social responsiveness of medical schools. Educ Health (Abingdon) 1999; 12: 9-19.
- 8. Boelen C, Heck JE. Defining and measuring the social accountability of medical schools. Geneva: World Health Organization, 1995.
- 9. Parboosingh J. Medical schools’ social contract: more than just education and research. CMAJ 2003; 168: 852-853.
- 10. Hennen B. Demonstrating social accountability in medical education. CMAJ 1997; 156: 365-367.
- 11. Scholte JA. Globalization: a critical introduction. London: Palgrave Macmillan, 2000.
- 12. Bateman C, Baker T, Hoorenberg E, et al. Bringing global issues to medical teaching. Lancet 2001; 358: 1539-1542.
- 13. Houpt ER, Pearson RD, Hall TL. Three domains of competency in global health education: recommendations for all medical students. Acad Med 2007; 82: 222-225.
- 14. Drain PK, Primack A, Hunt DD, et al. Global health in medical education: a call for more training and opportunities. Acad Med 2007; 82: 226-230.
- 15. Brundtland GH. Speech at United Nations Associations Global Leadership Awards. New York, 2001; Apr 19. http://www.who.int/director-general/speeches/2001/english/20010419_UNAawardsdinnernewyork.en.html (accessed Sep 2007).
- 16. Global Health Education Consortium [website]. http://www.globalhealth-ec.org (accessed Jul 2007).
- 17. Medical Deans Australia and New Zealand. Overseas electives. http://www.medicaldeans.org.au/projects.html#topic6 (accessed Jul 2007).
- 18. Hoc Mãi: The Australia Vietnam Medical Foundation [website]. http://www.hocmai.org (accessed Jul 2007).
- 19. Furin J, Paternek M, Katz JT. Global health equity as the focus of graduate medical education. Med Educ 2005; 39: 1161.






Abstract
Over the past decade, student participation in international health has moved beyond individual elective terms in developing countries to collective responses led by student international health organisations.
There are now at least 10 such organisations, with more than 500 medical students participating at a local or national level each year.
Student international health organisations can deliver short- and long-term benefits to developing countries, while equipping students with skills such as leadership, teamwork and cultural sensitivity.
Activities include delivery of medical equipment, fundraising, educating university communities, and acting as advocates for social justice.
We believe Australian medical schools must formally incorporate international health into their curricula, drawing upon the experiences of schools in Europe and North America.