The failure of effective communication is a recurring theme in the patient safety literature,1-3 specifically as it relates to clinical handover.4 A review of local clinical incidents confirmed that this pattern was particularly evident for acutely ill, deteriorating patients who require transfer to a higher level of care. Important issues were:
The failure to effectively communicate a patient’s condition when seeking advice or “bed-hunting”;
The existence of multiple verbal and written contact points between service providers, each with highly individual and/or profession-dependent processes;
Incomplete handover of accountability;
The lack of an agreed plan of care; and
Variable and overlapping formats of written communication.
The development of clinical handover systems such as standard operating procedures has been shown to reduce system failures.4,5 A review of the literature identified limited tools for clinical handover and a lack of evidence favouring any particular approach. One such tool, the SBAR (situation–background–assessment–recommendation) checklist (developed by Kaiser Permanente in the United States),6,7 prompts the user to provide information on each of these four elements at each handover event. While this tool showed promise, we wished to ensure clinical input and leadership before trialling it in our health care system.
Issues pertaining to clinical handover are particularly relevant to Australia’s largest country health system. The Western Australian Country Health Service (WACHS) (Box 1) covers an area of 2.53 million square kilometres, with a widely dispersed population of 454 000 people. The vast distances between populations create unique challenges in relation to attraction and retention of health care workers and provision of care locally, wherever possible. WACHS employs about 5662 full-time-equivalent staff, including 2310 nurses and 180 salaried and 150 contracted Visiting Medical Officers (VMOs). A high proportion of these are overseas-trained doctors and short-term locum appointments. Each year, WACHS manages an average of 325 000 emergency department visits, 380 000 inpatient bed-days, 96 000 hospital discharges and 10 000 transfers to tertiary hospital facilities, of which 7 000 are by either the Royal Flying Doctor Service of Australia or the St John Ambulance service. An analysis of local incident and clinical review reports indicates that up to 70% of adverse events occur because of miscommunication and at points of transition or handover of care.
In the WACHS context, effective handover procedures are vital. Hence our project set out to:
In October 2007, a collaborative team was formed between WACHS and the Royal Perth Hospital. The team consisted of two part-time project managers with extensive nursing and rural experience from WACHS, and the Assistant Director of Clinical Services and a project officer with marketing experience from Royal Perth Hospital. After a review of the themes identified above, we determined to target acutely ill, deteriorating patients who required transfer to a higher level of care. The brief was to develop a standardised and transferable clinical handover process and checklist. The approach involved clinician consultation8 and a review of processes using a human factors framework.9,10 Potential handover issues and traps were identified by mapping patient journeys from a rural facility to a tertiary hospital. Existing work practices and schedules were also examined, so that handover tools could be incorporated into ingrained habits and patterns.11,12
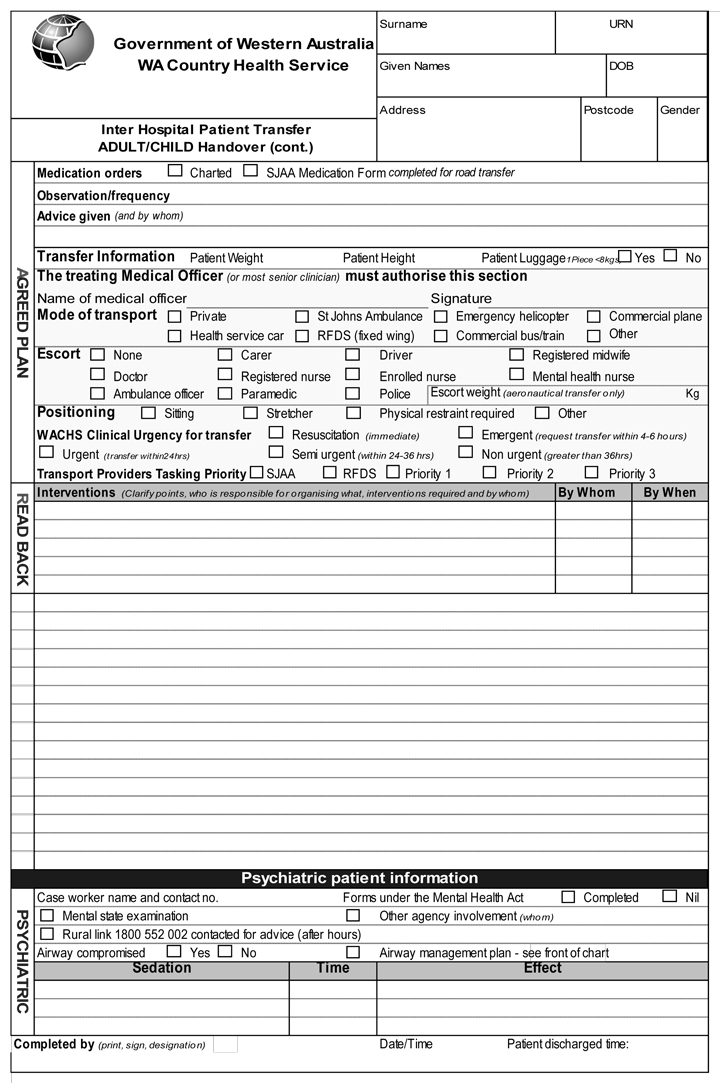
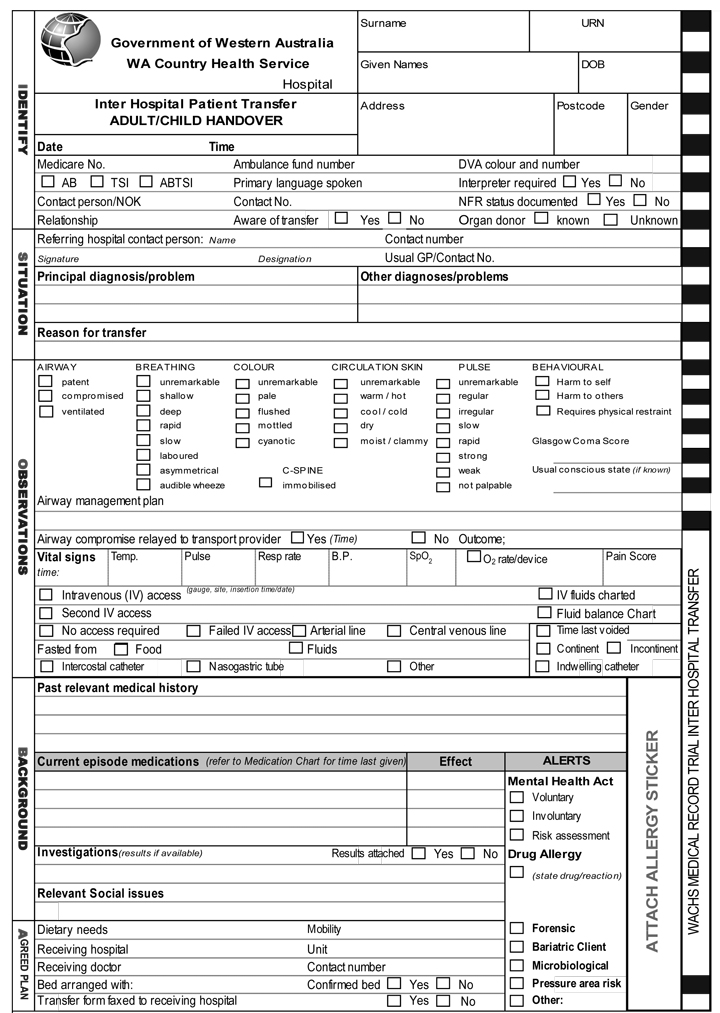
Agreeing to the minimum dataset was non-contentious. Initially, each data element identified was grouped under one of the four SBAR tool headings. However, after consultation and review, it was decided that the existing SBAR tool should be modified and expanded to better fit the local context. The tool was thus expanded to “iSoBAR”, both a word and a mnemonic, which had resonance in the state’s cyclone-prone north-west. The checklist now had two additional prompts compared with the original SBAR. Firstly, the “i”, for “identify yourself and the patient”, placed the patient’s identity, rather than the diagnosis, in primary position and also provided a method of introduction. (This is particularly important when teams are widely spread geographically.) The second new prompt, “o” for “observations”, was included to provide an adequate baseline of factual information on which to devise a plan of care. “S” (“situation”) and “B” (“background”) were unchanged, but “A” (“assessment”) was changed to “agreed plan” and “R” (“recommendation”) was changed to “read back” to reinforce the transfer of information and accountability (Box 2).
Throughout the development of the checklist, staff expressed frustration with inconsistent processes in arranging transfers and handover of patients from one site to another, as well as their concerns about working under pressure, high staff turnover, dealing with critically ill patients in local services with an inadequate level of care available, and the urgent need to find a more appropriate level of care. The project team and staff shared specific examples of adverse events relating to handover and discussed system changes that could improve patient outcomes in these cases. While all staff expressed a need for a more systematic and consistent system of handover, they underlined the need for a pragmatic approach that would reduce duplication and fit into existing work patterns.13
The iSoBAR handover form was developed and printed for trial at six inpatient sites in the Kimberley region, to identify any issues before wider implementation.14 The team spent time in the Kimberley region, meeting with staff on all shifts and attending meetings with medical staff and managers. Any change program in rural and remote Australia requires extensive travel and resilience on the part of project team members. In this case, they covered over 8000 km of air and/or road travel to attend staff handovers on all shifts. Making time to build relationships and support staff by listening and informing rather than telling and directing were key elements of the change management approach.13
The iSoBAR form and toolkit were accepted and widely used by WACHS clinical staff. (For tips on engaging clinicians in this type of project, see Box 3.) The form is currently being used in a number of other settings, including shift handovers, emergency department and theatre-to-ward transfers, and for WACHS allied health referrals. Use of the form has spread to some facilities in metropolitan WA, although the extent of uptake is as yet unknown.
The early adoption of the new iSoBAR form was attributed to extensive clinician involvement and leadership.15 The form has become part of the WACHS clinical staff orientation program and is now included early in the WACHS nurse graduate program of teaching. Networks of regional staff are sharing ideas and have started to evaluate the progress of implementation. At the time of writing, the evaluation is continuing, but early indications are that the form, educational CD and marketing tools are being used extensively and in a wide range of contexts. Staff feel that iSoBAR particularly suits local conditions, has created a greater sense of ownership among rural staff, and has reduced the duplication of paperwork.
The need for a handover checklist has been highlighted by the National Clinical Handover Initiative of the Australian Commission on Safety and Quality in Health Care. This initiative aims to develop new and creative approaches to handover safety and excellence. The Commission has supported a number of handover projects (including iSoBAR), placing Australia at the forefront of clinical handover research. This WA rural project demonstrates that using an organisational change approach to the development and implementation of iSoBAR as a handover checklist is readily achievable with the early involvement of all local stakeholders.8 WACHS is now monitoring the use of iSoBAR and assessing whether a measurable difference in patient outcomes may be demonstrated. Early feedback suggests that staff consider iSoBAR particularly well suited to local conditions and easy to integrate into existing work processes to reduce duplication of paperwork and processes. Whether using a handover checklist improves patient safety and reduces adverse outcomes is yet to be established. However, we anticipate that addressing effective communication through a systematic and standardised approach, led and tested by clinicians, will have a positive impact on both staff and patients.
- Jill M Porteous1
- Edward G Stewart-Wynne2
- Madeleine Connolly1
- Pauline F Crommelin1
- 1 Western Australian Country Health Service, Perth, WA.
- 2 Royal Perth Hospital, Perth, WA.
None identified.
- 1. Vincent C. Patient safety. London: Churchill Livingstone Elsevier, 2006.
- 2. Williams JR. How literacy and communication initiatives improve patient safety. Focus Patient Saf 2005; 8 (3): 3-4.
- 3. The Joint Commission. Preventing infant death and injury during delivery. Sentinel Event Alert 2004; Issue 30. http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_30.htm (accessed Feb 2009).
- 4. World Health Organization Collaborating Centre for Patient Safety Solutions. Communication during patient hand-overs. Patient Saf Solut 2007; 1 (Solution 3). http://www.ccforpatientsafety.org/common/pdfs/fpdf/presskit/PS-Solution3.pdf (accessed Feb 2009).
- 5. National Patient Safety Agency. Safe handover: safe patients. London: British Medical Association, 2004. http://www.idwl.info/JDC%2021%202004-05%20Handover%20Booklet.pdf (accessed Feb 2009).
- 6. Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 2004; 13 Suppl 1: i85-i90.
- 7. Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf 2006; 32: 167-175.
- 8. Ham C. Improving the performance of health services: the role of clinical leadership. Lancet 2003; 361: 1978-1980.
- 9. Gosbee J. Human factors engineering and patient safety. Qual Saf Health Care 2002; 11: 352-354.
- 10. Berwick DM. Not again! Preventing errors lies in redesign — not exhortation. BMJ 2001; 322: 247-248.
- 11. Resar RK. Making noncatastrophic health care processes reliable: learning to walk before running in creating high-reliability organizations. Health Serv Res 2006; 41: 1677-1689.
- 12. Nolan T, Resar R, Haraden C, Griffin FA. Improving the reliability of health care. IHI Innovation Series white paper. Boston: Institute for Healthcare Improvement, 2004.
- 13. Degeling P. Realising the developmental potential of clinical governance. Clin Chem Lab Med 2006; 44: 688-691.
- 14. Lingard L, Espin S, Rubin B, et al. Getting teams to talk: development and pilot implementation of a checklist to promote interprofessional communication in the OR. Qual Saf Health Care 2005; 14: 340-346.
- 15. Newton PJ, Davidson PM, Halcomb EJ, et al. An introduction to the collaborative methodology and its potential use for the management of heart failure. J Cardiovasc Nurs 2006; 21: 161-168.





Abstract
Effective communication at clinical handover is important for improving patient safety and reducing adverse outcomes.
In consultation with doctors, nurses and allied health staff in the Western Australian Country Health Service, we developed a clinical handover checklist, adapted from an existing tool for standardising communication.
The acronym “iSoBAR” (identify–situation–observations–background–agreed plan–read back) summarises the components of the checklist.
We designed a comprehensive iSoBAR handover form to reduce the number of existing clinical handover forms. The new form, with an accompanying toolkit, was initially trialled in the Kimberley region, but is now being adopted more widely.
Early adoption of the new form has been attributed to extensive clinician involvement and leadership.
There is a need for further research to assess whether the use of handover checklists improves patient outcomes.