Mumps is an infectious disease caused by a single-stranded RNA virus belonging to the genus Rubulavirus and the family Paramyxoviridae. It has no animal reservoirs and is therefore purely a human disease. There is only one serotype of the virus, which can be further divided into 10–11 genotypes.1 The term “mumps” is probably derived from a word meaning “grimace”, reflecting the impact of parotitis on facial expression.
Although mumps has generally been regarded in recent years as an uncommon and mild self-limiting illness of early childhood, Australian data for the period 2002–2005 show that 138/419 people with mumps (33%) were hospitalised, of whom three-quarters were aged over 15 years. Complications of mumps in hospitalised patients were recorded in 19/138 cases (14%), with orchitis being the most common complication (10/19), followed by pancreatitis (2/19). There was one death in a patient aged 100 years.2
The estimated global incidence of mumps is 100–1000/100 000 population per year, with epidemic peaks every 2–5 years.3 In temperate climates, the peak incidence of mumps is in winter and spring, whereas cases can occur consistently throughout the year in tropical climates.4
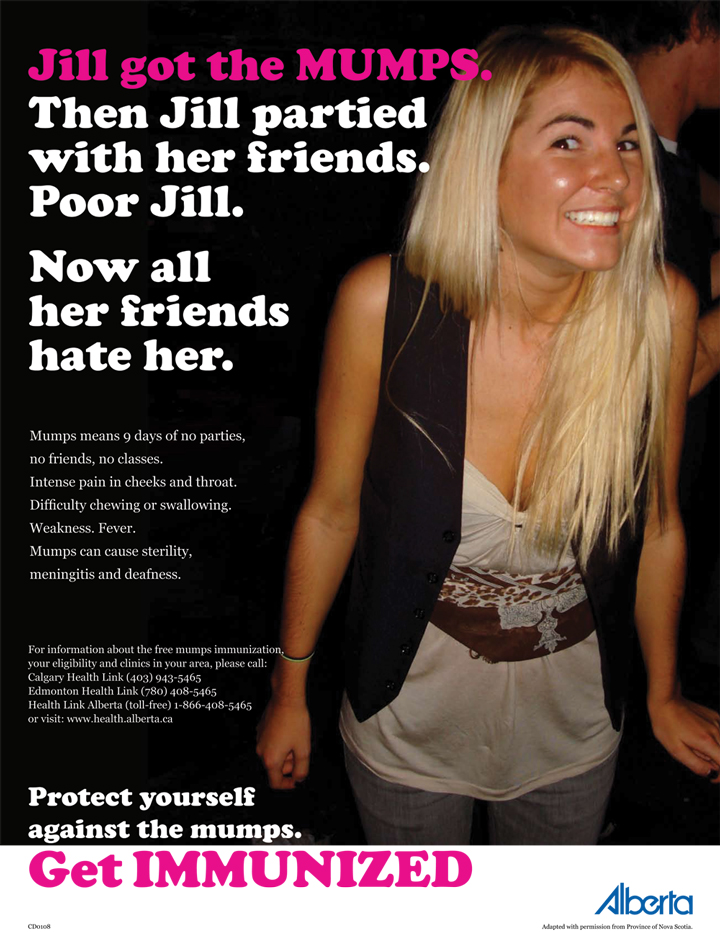
Before the introduction of mass vaccination programs, mumps primarily affected 5–9-year-old children, but more recent (and large) outbreaks have mainly affected adolescents and adults.5,6 In 2004–2005 in the United Kingdom, more than 56 000 clinical cases of mumps were notified, with the majority of confirmed cases occurring in 15–24-year-olds.7 This change is clinically important, as mumps tends to be more severe in adolescents and adults than in children.8 Furthermore, some complications such as orchitis are limited to post-pubertal infection. Posters produced for mumps education campaigns in response to large Canadian outbreaks that also affected many adolescents and adults (http://www.health.alberta.ca/public/disease_conditions.html#mumps) are shown in Box 1.
In Australia, the National Notifiable Diseases Surveillance System (NNDSS) has recorded a consistent rise in mumps notifications over the past few years, with almost 600 notifications in 2007. NNDSS data show that notification rates in adolescents and young adults have increased over time, reflecting a similar pattern overseas. In 2007, 76% of mumps notifications in Australia were for people aged 20 years or older.9
The reasons for this change in mumps epidemiology are multifactorial. They include primary vaccine failure due to true immunological failure or administration of ineffective vaccine;5 secondary vaccine failure due to a loss of immunity despite initial seroconversion;10 and a lack of cross-neutralisation between vaccine strains and wild-type genotypes.1,11,12
Transmission of mumps occurs through droplet infection, fomites or direct contact. The virus enters the body through the upper respiratory tract. After the virus has multiplied within the local reticuloendothelial and lymphoid systems, there is a period of 7–10 days of viraemia, during which other organs can become infected.13
Histologically, mumps parotitis is characterised by diffuse interstitial oedema with a predominantly mononuclear serofibrinous exudate. The ductal lumina contain necrotic debris. There is relative sparing of the glandular cells. The histological appearance of mumps orchitis is fairly similar to that of parotitis.14
Mumps is highly infectious,8 with a single case generating up to 12 secondary cases in a susceptible population. The infectious period lasts from 2 days before the onset of symptoms to 9 days afterwards.15 Even asymptomatic people can transmit the virus.14 Natural infection was once thought to confer lifelong immunity, but we now know that reinfection can occur, although it tends to be milder and more atypical than in primary infection.16
Acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland, lasting two or more days and without other apparent cause.17,18
After an incubation period of 16–18 days (range, 12–25 days), a prodrome of headache, anorexia, malaise, generalised myalgia and fevers may occur. Tenderness of the parotid glands and otalgia often precede parotitis, which is bilateral in 95% of cases.8 The swelling can be extensive enough to interfere with speech and chewing, and can even cause trismus.13
The intraoral entry point to the duct of the parotid gland (Stensen’s duct) is often swollen and erythematous during parotitis.8 This point is found at the level of the upper second molar. In 10% of cases, other salivary glands may also be involved.14
The parotitis tends to resolve within a week, with children being less sick than adolescents and adults.8 Long-term complications of parotitis are uncommon, but sialectasia with recurrent bouts of inflammation may occur.13
Classical infection can occur with or without extra-parotid complications. Some of the more common or serious extra-parotid complications of mumps are listed in Box 2.
Two-thirds of cases of mumps-related epididymo-orchitis develop during the first week of parotitis. The clinical presentation is typically of acute scrotal pain, fevers and other constitutional symptoms. Defervescence occurs over 5 days, and local symptoms resolve shortly afterwards in most cases. Up to 50% of males with epididymo-orchitis will suffer from testicular atrophy, with oligospermia or asthenospermia in up to 13%. Sterility is a rare complication.13
The neurological manifestations of mumps are diverse. Meningitis, which occurs in up to 10% of cases, appears 3–4 days after the onset of clinical parotitis.24 Both acute encephalitis and post-infectious immune-mediated encephalomyelitis are very uncommon. The former tends to be a mild self-limiting illness, while the latter tends to be more severe, with focal neurological features and case-fatality rates of up to 10%. The overall case-fatality rate for mumps-related central nervous system disease is about 1%.8
Several rare complications of mumps have been recorded, including Guillain-Barré syndrome, thyroiditis, polyarthritis, mastitis, thrombocytopaenia and hepatitis.14
While consideration of mumps is easy in the presence of parotitis, up to 30% of cases are asymptomatic and, of symptomatic cases, 10%–30% will not be associated with parotitis.8,13 This highlights the limitation of the case definition given above, which implies that swelling of the salivary glands is an essential diagnostic feature.
Although mumps is probably the best known cause of bilateral parotitis, a number of differential diagnoses should be considered (Box 3). A suspected mumps infection can be confirmed by detection of antibodies to the virus, detection of viral RNA by reverse transcriptase-polymerase chain reaction (RT-PCR) techniques, or viral cultures of various clinical specimens. In Australia, mumps viral cultures are rarely performed. Serum, saliva and/or urine specimens may be useful in cases of uncomplicated mumps, but if mumps meningitis is suspected, cerebrospinal fluid (CSF) examination may be indicated.
IgM can be detected not only in primary mumps but even in secondary immune responses in cases of mumps due to secondary vaccine failure.12 While IgM may be detectable in serum as early as 11 days after exposure (before symptoms have appeared), the optimal time for detection is probably 7–10 days after the patient develops symptoms.19 However, the sensitivity of IgM testing is variable, being as low as 24%–51% in one study of five ELISA assays.26 Both false negative and false positive IgM results can occur. False negative IgM results may occur in people previously immunised or infected.27 In such settings, a rise in serum IgG titres may be a more useful indicator of current infection.19 False positive IgM results may occur after infection with parainfluenza viruses 1 and 3 or in the context of recent immunisation with vaccines containing a mumps component.27
Both IgM and RT-PCR tests can be used to detect mumps in saliva. The salivary IgM test has high specificity (98%), and its sensitivity increases from 75% in the first week after symptoms appear to 100% thereafter.8 The RT-PCR test on saliva, which has a sensitivity of about 70%,28 is typically positive from 2–3 days before the onset of parotitis to 4–5 days afterwards,14 and thus can often detect mumps virus in saliva when the salivary IgM test is negative.
Mumps virus can be detected in the urine during the first 2 weeks of illness by RT-PCR testing.14 However, for reasons that are unclear, the RT-PCR test has a much lower sensitivity for urine specimens than for viral cultures. One study found the sensitivity of different PCR techniques to be as low as 2% and 29%.26
In mumps meningitis, the CSF characteristically demonstrates normal opening pressure; a normal cell count or lymphocytic pleocytosis (about 250 cells/mm3) (pleocytosis is present in about 50% of cases);24 an elevated protein level in two-thirds of cases; and a reduced CSF : serum glucose ratio (< 50%) in up to a quarter of cases.8 RT-PCR and antibody tests (IgG and IgM) can be used to detect mumps in CSF, with the former being more sensitive than the latter.29,30 At least one nested RT-PCR assay had a sensitivity of 96% in CSF, was highly specific and was positive for up to 2 years after infection.31 One study of mumps meningitis found that IgG and IgM could be detected in CSF at rates of 90% and 50% respectively.29
Currently, treatment of mumps is generally supportive for both parotid and extra-parotid manifestations, including mumps meningitis. The use of local measures, such as heat or cold packs, and a combination of antipyretics and analgesics is generally recommended.14
Treatment with intramuscular mumps immune globulin may be of benefit in the early stages in certain cases, but this product is not available in Australia. Intravenous immunoglobulin therapy appears to have reduced certain complications of mumps, but this has not led to universal recommendations for its use.19
The role of subcutaneous interferon alpha-2b in preventing testicular atrophy in mumps orchitis has been examined, but there are conflicting data on outcome, presumably reflecting the small numbers of both subjects and studies.32-34
There is no effective post-exposure prophylaxis for mumps cases.35
In Australia, the measles–mumps–rubella (MMR) vaccine is currently recommended for children at the ages of 1 and 4 years. For adults who have only ever received a single dose of vaccine containing a mumps component, a second dose of MMR can be given at any age. As it is a live vaccine, its use is contraindicated for immunocompromised hosts.35 Short-term efficacy and seroconversion rates of about 90% are achieved after a single dose.4 The second dose of vaccine results in about 95% seroconversion, with a slower decline in antibody titres over time compared with subjects vaccinated only once.36 Immunogenicity and observational data tend to concur in showing that two doses of vaccine are more efficacious than one.37
In Australia, the Jeryl-Lynn strain of mumps vaccine is used.35 Despite being less efficacious and more expensive than the Urabe strain, its use is still cost-effective and less likely to cause vaccine-related aseptic meningitis.38
Apart from minor local reactions at the injection site, the major systemic reactions that may occur after mumps vaccination are low-grade fever, aseptic meningitis, meningoencephalitis and parotitis. Post-vaccine meningitis occurs 2–3 weeks after vaccination.4 The meningitis is mild to moderate in severity, and all reported cases have resolved completely within a week.39 The Jeryl-Lynn vaccine strain is associated with the lowest rate of vaccine-related aseptic meningitis, ranging from less than 1 case/525 312 doses to 0.1 cases/100 000 doses.3 Sensorineural deafness, orchitis and even post-vaccination pancreatitis have also been reported as extremely rare complications following vaccination.4,40
1 Posters produced for mumps education campaigns in response to large Canadian outbreaks that affected many adolescents and adults
  | |||||||||||||||
|
Courtesy of the Nova Scotia Department of Health Promotion and Protection. | |||||||||||||||
3 Causes of bilateral parotid swelling8,25
Viral infection (caused by influenza A virus, parainfluenza virus, adenovirus, coxsackie virus, Epstein-Barr virus or HIV)
Bacterial sialadenitis (often caused by Staphylococcus aureus)
Salivary calculi
Autoimmune disease (sarcoidosis, Sjögren’s syndrome, Wegener’s granulomatosis)
Neoplasia (Warthin’s tumour, mucosal-associated lymphoid tissue lymphoma)
Iatrogenic/self-induced disease (reaction to iodide contrast media or radioactive iodine; ingestion of starch or thiazide diuretics)
Polycystic parotid disease
Kimura disease*
* A chronic inflammatory disease of lymph nodes and subcutaneous tissue.
- Sanjaya N Senanayake1
- Department of Microbiology, Canberra Hospital, Canberra, ACT.
None identified.
- 1. Mühlemann K. The molecular epidemiology of mumps virus. Infect Genet Evol 2004; 4: 215-219.
- 2. Brotherton J, Wang H, Schaffer A, et al. Vaccine preventable diseases and vaccine coverage in Australia, 2003 to 2005. Commun Dis Intell 2007; 31 Suppl: S1-S152.
- 3. Bonnet MC, Dutta A, Weinberger C, Plotkin SA. Mumps vaccine virus strains and aseptic meningitis. Vaccine 2006; 24: 7037-7045.
- 4. Mumps virus vaccines. Wkly Epidemiol Rec 2007; 82: 51-60.
- 5. Gemmill IM. Mumps vaccine: is it time to re-evaluate our approach? CMAJ 2006; 175: 491-492.
- 6. Centers for Disease Control and Prevention. Update: multistate outbreak of mumps — United States, January 1–May 2, 2006. MMWR Morb Mortal Wkly Rep 2006; 55: 559-563.
- 7. Cohen C, White JM, Savage EJ, et al. Vaccine effectiveness estimates, 2004–2005 mumps outbreak, England. Emerg Infect Dis 2007; 13: 12-17.
- 8. Gupta RK, Best J, MacMahon E. Mumps and the UK epidemic 2005. BMJ 2005; 330: 1132-1135.
- 9. Australian Department of Health and Ageing. National Notifiable Diseases Surveillance System. http://www9.health.gov.au/cda/Source/CDA-index.cfm (accessed Aug 2008).
- 10. Narita M, Matsuzono Y, Takekoshi Y, et al. Analysis of mumps vaccine failure by means of avidity testing for mumps virus-specific immunoglobulin G. Clin Diagn Lab Immunol 1998: 5: 799-803.
- 11. Nöjd J, Tecle T, Samuelsson A, Orvell C. Mumps virus neutralizing antibodies do not protect against reinfection with a heterologous mumps virus genotype. Vaccine 2001; 19: 1727-1731.
- 12. Atrasheuskaya AV, Kulak MV, Rubin S, Ignatyev GM. Mumps vaccine failure investigation in Novosibirsk, Russia, 2002–2004. Clin Microbiol Infect 2007; 13: 670-676.
- 13. Singh R, Mostafid H, Hindley RG. Measles, mumps and rubella — the urologist’s perspective. Int J Clin Pract 2006; 60: 335-339.
- 14. Litman N, Baum SG. Mumps virus. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and practice of infectious diseases. 6th ed. Philadelphia: Churchill Livingstone, 2005: 2003-2008.
- 15. Campos-Outcalt D. Mumps epidemic in 2006: are you prepared to detect and prevent it? J Fam Pract 2006; 55: 500-502.
- 16. Gut JP, Lablache C, Behr S, Kirn A. Symptomatic mumps virus reinfections. J Med Virol 1995; 45: 17-23.
- 17. World Health Organization. WHO-recommended surveillance standard of mumps. http://www.who.int/immunization_monitoring/diseases/mumps_surveillance/en/index.html (accessed Aug 2008).
- 18. Centers for Disease Control and Prevention. Mumps case definition and case classification (CSTE). http://www.cdc.gov/nip/diseases/mumps/case-def.htm (accessed Aug 2008).
- 19. Hviid A, Rubin S, Mühlemann K. Mumps. Lancet 2008; 371: 932-944.
- 20. Kawashima Y, Ihara K, Nakamura M, et al. Epidemiological study of mumps deafness in Japan. Auris Nasus Larynx 2005; 32: 125-128.
- 21. Taparelli F, Squadrini F, De Rienzo B, et al. Isolation of mumps virus from vaginal secretions in association with oophoritis. J Infect 1988; 17: 255-258.
- 22. Caranasos GJ, Felker JR. Mumps arthritis. Arch Intern Med 1967; 119: 394-398.
- 23. Ornoy A, Tenenbaum A. Pregnancy outcome following infections by coxsackie, echo, measles, mumps, hepatitis, polio and encephalitis viruses. Reprod Toxicol 2006; 21: 446-457.
- 24. Bajaj NP, Rose P, Clifford-Jones R, Hughes PJ. Acute transverse myelitis and Guillain-Barré overlap syndrome with serological evidence for mumps viraemia. Acta Neurol Scand 2001; 104: 239-242.
- 25. Mandel L, Surattanont F. Bilateral parotid swelling: a review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93: 221-237.
- 26. Krause CH, Molyneaux PJ, Ho-Yen DO, et al. Comparison of mumps-IgM ELISAs in acute infection. J Clin Virol 2007; 38: 153-156.
- 27. Centers for Disease Control and Prevention. Mumps — laboratory testing for mumps infection Q & A. http://www.cdc.gov/vaccines/vpd-vac/mumps/outbreak/faqs-lab-test-infect.htm (accessed Aug 2008).
- 28. Uchida K, Shinohara M, Shimada S, et al. Rapid and sensitive detection of mumps virus RNA directly from clinical samples by real-time PCR. J Med Virol 2005; 75: 470-474.
- 29. Forsberg P, Frydén A, Link H, Orvell C. Viral IgM and IgG antibody synthesis within the central nervous system in mumps meningitis. Acta Neurol Scand 1986; 73: 372-380.
- 30. Ukkonen P, Granström ML, Räsänen J, et al. Local production of mumps IgG and IgM antibodies in the cerebrospinal fluid of meningitis patients. J Med Virol 1981; 8: 257-265.
- 31. Poggio GP, Rodriguez C, Cisterna D, et al. Nested PCR for rapid detection of mumps virus in cerebrospinal fluid from patients with neurological diseases. J Clin Microbiol 2000; 38: 274-278.
- 32. Yeniyol CO, Sorguc S, Minareci S, Ayder AR. Role of interferon-alpha-2B in prevention of testicular atrophy with unilateral mumps orchitis. Urology 2000; 55: 931-933.
- 33. Erpenbach KH. Systemic treatment with interferon-alpha 2B: an effective method to prevent sterility after bilateral mumps orchitis. J Urol 1991; 146: 54-56.
- 34. Ku JH, Kim YH, Jeon YS, Lee NK. The preventive effect of systemic treatment with interferon-alpha2B for infertility from mumps orchitis. BJU Int 1999; 84: 839-842.
- 35. National Health and Medical Research Council. The Australian immunisation handbook. 8th ed. Canberra: NHMRC, 2003. http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-home (accessed Aug 2008).
- 36. Davidkin I, Valle M, Julkunen I. Persistence of anti-mumps virus antibodies after a two-dose MMR vaccination. A nine-year follow-up. Vaccine 1995; 13: 1617-1622.
- 37. Harling R, White JM, Ramsay ME, et al. The effectiveness of the mumps component of the MMR vaccine: a case control study. Vaccine 2005; 23: 4070-4074.
- 38. Hinman AR, Irons B, Lewis M, Kandola K. Economic analyses of rubella and rubella vaccines: a global review. Bull World Health Organ 2002; 80: 264-270.
- 39. World Health Organization. Global Advisory Committee on Vaccine Safety. Adverse events following mumps vaccination [Internet]. Geneva: WHO, 2003. http://www.who.int/vaccine_safety/topics/mumps/statement/en (accessed Aug 2008).
- 40. Toovey S, Jamieson A. Pancreatitis complicating adult immunisation with a combined mumps measles rubella vaccine. A case report and literature review. Travel Med Infect Dis 2003; 1: 189-192.





Abstract
While mumps is easily suspected if parotitis is present, parotitis is absent in 10%–30% of symptomatic cases.
Mumps is a systemic infection with a variety of extra-parotid complications.
In Australia, mumps diagnosis is confirmed by antibody testing and reverse transcriptase-polymerase chain reaction techniques. Suitable specimens for testing are serum, saliva, urine and cerebrospinal fluid.
Treatment is generally supportive, although intravenous immunoglobulin therapy may have a future role in mumps management. Interferon alpha-2b treatment may be considered specifically for mumps epididymo-orchitis.
Mumps vaccine is included in the measles–mumps–rubella (MMR) vaccine. In Australia, this vaccine is routinely administered at the ages of 1 and 4 years.
Serious reactions to the mumps components of the MMR vaccine are rare.