Imaging should be considered only after a provisional clinical diagnosis is reached, and only if it will influence management
Musculoskeletal imaging in sports medicine is a rapidly developing field, being driven by both continuously advancing technology and improved understanding of the disabilities that may result from sporting injuries, many of which can be minimised or avoided by early diagnosis and appropriate treatment.
Paradoxically, as imaging tests become ever more sophisticated and sensitive, the importance of clinical judgement in determining both when to order tests and the relevance of abnormal findings increases.1 This is because real but incidental anatomical derangements, such as normal developmental variants, and asymptomatic degenerative changes which become more prevalent with age and high-level sporting activity, are frequently detected. Studies have shown that subclinical pathological change is present in a large proportion of asymptomatic or minimally symptomatic athletes.2-7 It has long been recognised that even gross pathological derangements, such as osteoarthritic joints, intervertebral disc protrusions and rotator cuff tears, can sometimes be completely asymptomatic. Thus, physicians must always remember to “treat the patient, not the scan”.
The common-sense rule of only ordering a test if the result is likely to influence management applies. In sports medicine, a specific anatomical diagnosis is not always required and does not necessarily constitute best practice. For example, mild-to-moderate back pain in young adults without neurological signs may be appropriately managed with physiotherapy alone, irrespective of the actual anatomical diagnosis.8 A recent interesting study has found that in back pain, early use of computed tomography (CT) or magnetic resonance imaging (MRI) leads to slightly better patient outcomes without changing management.9 Despite this, the study concluded that whether such imaging was cost effective remained unresolved.
In general, the indications for imaging are as follows:
When the clinical diagnosis is uncertain and management may be affected by one or more of the particular possibilities being considered;
When clinical “red flags” are present and sinister or systemic abnormality must be excluded;
When the clinical diagnosis is obvious, but the extent of injury or presence of complications is unclear and either of these considerations may affect management;
When treatment has failed and the reasons for this are unclear (was the original diagnosis correct?);
When objective evidence is required to document the existence, progression or resolution of disease (eg, medicolegal situations);
When preoperative localisation or planning information is needed.
The selection of the best test or tests will vary, depending on (i) the provisional clinical diagnosis, (ii) the local availability of appropriate radiological equipment and expertise, (iii) patient considerations such as cost, convenience, and compliance, (iv) safety considerations such as patient age, radiation dose and contrast sensitivity, and (v) other costs such as that to the tax payer or insurance company. Radiation safety is an important consideration, as adverse effects are known to occur.10-15 In particular, multislice CT, which can readily generate large exposures, should be used judiciously. The United States Food and Drug Administration estimates that an effective dose of 10 mSv may carry a one in 2000 lifetime risk of inducing fatal cancer.16 A short list of relative radiation doses is given in Box 1.16 The actual dose delivered in any given CT examination can vary greatly, depending on the type of scanner and scan technique used. It has been estimated that over one million CT scans are performed each year in Australia, and that the collective radiation dose arising from these studies could be inducing as many as 280 fatal cancers per year.10 Thus, in sports medicine, where disease is not life-threatening, the question of whether CT scans or isotope bone scans are essential to management is important. For younger patients in particular, safer tests such as ultrasound or MRI should be used wherever they will provide equivalent diagnostic efficacy.
It is always important to provide a request form which offers a guiding differential diagnosis or asks specific questions that the radiologist must attempt to answer. This not only allows appropriate optimisation of imaging protocol, but also increases the likelihood of disease detection (because subtle or equivocal findings are easily overlooked if the clinical notes provided do not adequately direct the radiologist’s search pattern and analysis). It is worth asking your local radiologist for advice if uncertain about such issues of cost, access, accuracy, safety or the significance of the report findings.
This provides a comprehensive anatomical overview at low cost and relatively low radiation dose, and should generally be the first imaging test.17 Combined with the clinical assessment, plain films alone will often allow a reasonable provisional diagnosis and management plan to be formulated without the need for more sophisticated tests. Even when the clinical features suggest that an injury involves soft tissue structures alone, plain films may be required to detect important features that other tests may miss (eg, soft-tissue calcifications, foreign bodies, bone spurs, accessory centres of ossification, periosteal reactions, joint malalignments, old injuries and other predisposing conditions, clinically unsuspected fractures). X-rays that show no abnormalities are not a waste of time, as they help to exclude or reduce the likelihood of many conditions. Failure to obtain plain films can lead to significant errors in the interpretation of more sophisticated tests, such as MRI, bone scans or ultrasound.
MRI provides a comprehensive, panoramic, and multi-planar image of both superficial and deep soft-tissue structures. Although MRI resolves bone mineral poorly, it is the ideal modality whenever a detailed characterisation of bone marrow disorder is sought. This gives MRI a special place in evaluating osteochondral injury, osteonecrosis, bone bruising, bone stress, transient osteoporosis of the hip, and tumours. MRI has equivalent sensitivity to isotope bone scanning for the detection of bone stress, but provides considerably more anatomical information without exposing patients to ionising radiation. MRI also provides excellent delineation of both deep and superficial soft tissues in a more panoramic and less operator-dependent format than ultrasound, and is the best non-invasive imaging test for injuries of articular cartilage and fibrocartilage (eg, meniscal tears). Some types of ligament, muscle and tendon injury are also best seen with MRI, especially when these involve deep or inconveniently positioned structures that do not afford ready ultrasound access. In recent years, MRI has been shown to be very useful in helping to provide a prognosis for muscle strain injuries in professional athletes (Box 2), although the cost makes it inappropriate as a routine test in amateurs (on the basis that management would not be changed). MRI may be contraindicated or complicated by factors such as cardiac pacemakers, cerebral aneurysm clips, claustrophobia, inability to remain still, prostheses and other surgical hardware.
Under the current Australian health system, cost and access are also significant issues because Medicare rebates do not apply to MRI scans ordered by primary care providers (including sports physicians, even if they are consulted on a referral basis). For both CT and MRI examinations of joints where intra-articular abnormality is suspected (particularly for the hip and shoulder), joint surface resolution may be improved by the use of an intra-articular contrast material. The benefits of this must be weighed against the added patient discomfort and risks, such as allergic reaction, chemical synovitis or, rarely, septic arthritis.
New and impressive medical imaging techniques emerging over the last two decades have greatly expanded our ability to non-invasively interrogate complex anatomical structures in fine detail, and to diagnose a variety of conditions in sports medicine. Nevertheless, the complicated array of available imaging technology now makes the choice of exactly which test to order, and when, challenging. In many situations, there are simply no authoritative guidelines available, and the choice of test may also be influenced by individual patient or local community circumstances.
It must never be forgotten that imaging does not replace or reduce the need for a thorough clinical evaluation. Such evaluation, coupled with knowledge of the relevant anatomy and an understanding of likely pathological conditions, remains the cornerstone of accurate diagnosis. Only when a provisional clinical diagnosis has been reached can a rational decision be made about the need for additional diagnostic tests and the significance of any subsequent results.
Evidence-based recommendations
Abnormal findings on scans do not necessarily indicate clinical relevance (Evidence level I [E1]; based on National Health and Medical Research Council levels of evidence24). Many studies of asymptomatic patients have revealed a high incidence of radiological “abnormality”.2-7 While such lesions sometimes increase the risk of clinical syndromes developing, they should serve as a warning against injudicious ordering of imaging tests.
Moderately severe chronic back pain without neurological symptoms and signs is generally treated in the same fashion whether or not three-dimensional imaging techniques are used (E1).8,9,20 However, a recent randomised controlled trial suggested that despite similar treatment, early imaging slightly, but significantly, improves outcome (E2).9
Magnetic resonance imaging (MRI) of the knee is useful when the clinical diagnosis is equivocal,18 but not necessarily when the clinical diagnosis is clear.25 Studies comparing the accuracy of physical examination with that of MRI in diagnosing intra-articular knee disorders have generally found 70%–80% accuracy with both methods (E2).25
Imaging techniques that involve ionising radiation (x-ray, CT scan, bone scan) may have the potential to be carcinogenic (E4).21
1 Comparison of radiation doses from common diagnostic procedures16
Diagnostic procedure |
Typical effective dose (mSv) |
No. of chest x-rays (PA film) for equivalent effective dose* |
Time for equivalent effective dose from background radiation† |
||||||||||||
Chest x-ray (PA film) |
0.02 |
1 |
2.4 days |
||||||||||||
Skull x-ray |
0.07 |
4 |
8.5 days |
||||||||||||
Lumbar spine x-ray series |
1.3 |
65 |
158 days |
||||||||||||
Intravenous urogram |
2.5 |
125 |
304 days |
||||||||||||
Upper gastrointestinal examination |
3.0 |
150 |
1.0 years |
||||||||||||
Barium enema |
7.0 |
350 |
2.3 years |
||||||||||||
Computed tomography; head |
2.0 |
100 |
243 days |
||||||||||||
Computed tomography; abdomen |
10.0 |
500 |
3.3 years |
||||||||||||
* Based on the assumption of an average “effective dose” from chest x-ray (PA film) of 0.02 mSv. † Based on the assumption of an average “effective dose” from natural background radiation of 3 mSV per year in the United States. PA = posteroanterior. |
|||||||||||||||
2 Magnetic resonance image

Fat-suppressed T2-weighted axial magnetic resonance image showing high-signal-intensity strain of hamstring muscle (long head of biceps femoris).
Case study 1 — knee pain
A 50-year-old, mainly sedentary, male ex-footballer with gradual onset knee pain. There are no mechanical symptoms such as locking. He has well-localised tenderness on the medial joint line and a mild effusion. He gets medial knee pain on squatting but can move his knee from full extension to full flexion without any catching (equivocal or negative McMurray’s test). Differential diagnosis: Medial compartment osteoarthritis and/or degenerative posterior horn tear of the medial meniscus. Imaging options: A plain x-ray series (with weightbearing views) is essential to determine the presence and degree of any degenerative change in the medial joint compartment, which dramatically affects management. At his age, severe degenerative changes may indicate definitive surgery, such as total or unicompartmental knee replacement. If the x-ray shows no degenerative changes, the likelihood of a clinically-relevant medial meniscal tear is significantly increased, as is the likelihood of knee arthroscopy giving an excellent result. It is in this scenario (clinical picture compatible with meniscal tear, but diagnosis uncertain) that an additional test such as magnetic resonance imaging (MRI) becomes valuable,18 as a confirmed diagnosis would alter the management (see Figure). If the x-ray shows moderate degeneration of the medial compartment, but not to the degree of needing major surgery (yet), then the recommended management of this patient is generally to persist with conservative treatment (glucosamine, moderate activity, hyaluronic acid injections). In this situation, surgical management is unlikely to be indicated as there is no mechanical restriction of movement,19 which means an MRI is probably an over-investigation. |
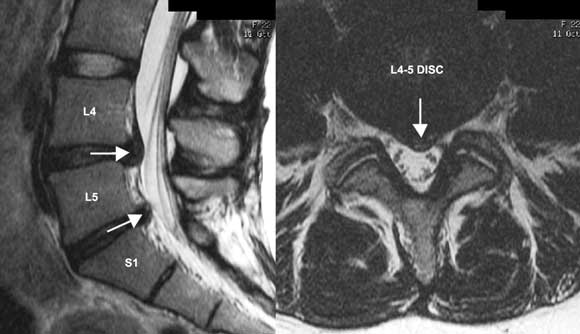
Case study 2 — back injury with neural symptoms
A 25-year-old woman with a 2-week history of gym-related back injury, some “soft” left leg neural symptoms (radicular pain and pins and needles) and signs (positive slump test and straight leg raise but intact reflexes, power and sensation). Clinical examination in this scenario can often confirm a diagnosis of likely lumbar disc prolapse.20 Differential diagnosis: Very likely to be a mild to moderate acute lumbar disc prolapse in this age group. Imaging options: X-ray is probably of minimal use and represents unnecessary radiation in a young woman. Surgery is probably not going to be indicated if neural signs are soft (ie, no reflex or sensory changes or wasting). An initial trial of a few weeks of conservative treatment based on the provisional clinical diagnosis alone (ie, without any immediate imaging) is reasonable if no complicating features are present.9 If this trial of treatment fails, or particularly if complicating features are present, imaging is indicated. Although a computed tomography (CT) scan (available on Medicare) would be sufficient to diagnose a disc protrusion, this carries an undesirable radiation risk in a young woman.21 Thus, despite its expense, an MRI scan (available on Medicare only with specialist referral) is the preferred imaging test (Figure). A positive result will confirm the cause and exact level of radicular irritation. This will assist management if conservative measures are not working and a second line of treatment is needed (eg, guided peri-neural cortisone injection). |
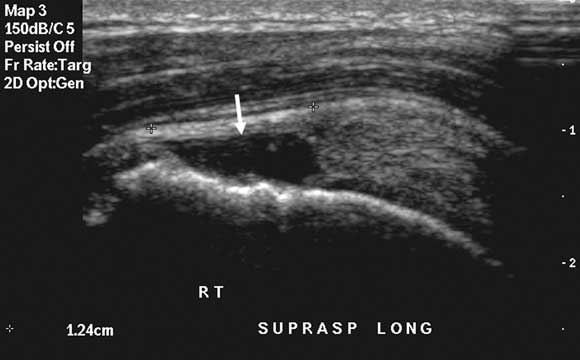
Case study 3 — shoulder impingement pain
A 35-year-old man with sudden worsening of deep shoulder impingement pain from doing upper body weights at the gym. Differential diagnosis: Rotator cuff tendinopathy is the most likely diagnosis. Shoulder instability is very common in younger athletes, but becomes less relevant in older athletes. Therefore, although a glenoid labral tear (associated with shoulder instability) remains possible, the diagnosis not to be missed is a full thickness rotator cuff tear (as surgical repair would probably be indicated at this age). Imaging options: If rotator cuff power remains strong, initial imaging may not be necessary, and a trial of physiotherapy may be justified. A single clinically-guided subacromial cortisone injection22 or topical glyceryl trinitrate therapy23 are also justified. If rotator cuff power is reduced, or first-line management fails, any cuff tear should be accurately characterised to determine the need for surgical intervention. The imaging options are ultrasound (Figure), MRI, or CT-arthrogram, and the choice will vary with local circumstances (eg, the preference of the shoulder surgeon, the skill set of the radiologist, the availability and affordability of MRI). A preliminary x-ray is also of definite value in assessing other factors (eg, acromial bone spurring, acromial morphology, acromioclavicular joint status) that might influence the surgical management. Both ultrasound and MRI would avoid invasive arthrography but may not always be locally available or reliable. Ultrasound is more useful in older patients, in whom glenoid labral tears are not a major concern, whereas MRI is preferred in younger patients, in whom underlying glenohumeral joint instability is an important consideration. A further advantage of ultrasound can be its ability to accurately guide an injection of subacromial cortisone, which may be the best management option if an initial clinically-guided injection has failed and there is no significant rotator cuff tear. |
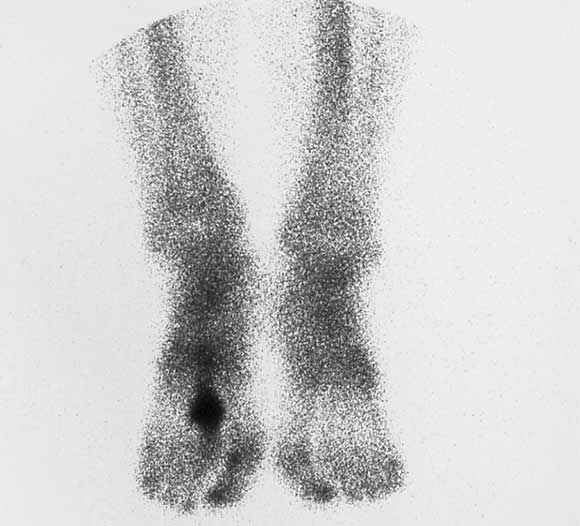
Case study 4 — forefoot pain
An 18-year-old competitive female hurdler with painful forefoot and tenderness over the second metatarsal, and inability to jump off the foot or sprint. She would like to compete in a major event in 8 weeks. Differential diagnosis: Probable second metatarsal stress fracture. Imaging options: The first investigation should be plain x-ray, which would confirm the diagnosis if a corresponding fracture line or periosteal reaction is detected. If the plain x-ray is normal, because of the need to plan the patient’s competitive season, either MRI or bone scan (Figure) would be indicated. MRI has the advantage of avoiding exposure to ionising radiation, whereas bone scan has the advantage of providing a total skeletal survey. |
- John W Orchard1
- John W Read2
- Ian (Jock) F Anderson3
- 1 Sports Medicine at Sydney University, University of Sydney, Sydney, NSW.
- 2 Sports Imaging (Castlereagh Imaging), North Sydney Orthopaedic and Sports Medicine Centre, Sydney, NSW.
- 3 UNSW Sports Medicine Program, University of New South Wales, Sydney, NSW.
None identified.
- 1. Anderson I, Read J, Steinweg J. Atlas of imaging in sports medicine. Sydney: McGraw-Hill, 1998.
- 2. Tempelhof S, Rupp S, Seil R. Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg 1999; 8: 296-299.
- 3. Sher JS, Uribe JW, Posada A, et al. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 1995; 77: 10-15.
- 4. Haims AH, Schweitzer ME, Patel RS, et al. MR imaging of the Achilles tendon: overlap of findings in symptomatic and asymptomatic individuals. Skeletal Radiol 2000; 29: 640-645.
- 5. Cook JL, Khan KM, Kiss ZS, et al. Prospective imaging study of asymptomatic patellar tendinopathy in elite junior basketball players. J Ultrasound Med 2000; 19: 473-479.
- 6. Orchard J, Read J, Neophyton J, Garlick D. Ultrasound findings of inguinal canal posterior wall deficiency associated with groin pain in footballers. Br J Sports Med 1998; 32: 134-139.
- 7. Beattie K, Boulos P, Pui M, et al. Abnormalities identified in the knees of asymptomatic volunteers using peripheral magnetic resonance imaging. Osteoarthritis Cartilage 2005; 13: 181-186.
- 8. Bigos S, Davis G. Scientific application of sports medicine principles for acute low back problems. J Orthopaed Sports Phys Ther 1996; 24: 192-207.
- 9. Gilbert F, Grant A, Gillan M, et al. Low back pain: influence of early MR imaging or CT on treatment and outcome — multicentre randomized trial. Radiology 2004; 231: 343-351.
- 10. Thomson J, Tingey D. Radiation doses from computed tomography in Australia. Canberra: Australian Radiation Laboratory, Department of Health and Family Services, 1997.
- 11. Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci U S A 2003; 100: 13761-13766.
- 12. Brenner D. Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology 2004; 231: 440-445.
- 13. de Gonzalez A, Darby S. Risk of cancer from diagnostic x-rays: estimates for the UK and 14 other countries. Lancet 2004; 363: 345-351.
- 14. Infante-Rivard C, Mathonnet G, Sinnet D. Risk of childhood leukemia associated with diagnostic irradiation and polymorphisms in DNA repair genes. Environ Health Perspect 2000; 108: 495-498.
- 15. Morin Doody M, Lonstein J, Stovall M, et al. Breast cancer mortality after diagnostic radiography: findings from the US Scoliosis Cohort Study. Spine 2000; 25: 2052-2063.
- 16. United States Food and Drug Administration. Center for Devices and Radiological Health. Whole body scanning using computed tomography (CT). What are the radiation risks from CT? Available at: http://www.fda.gov/cdrh/ct/risks.html (accessed Sep 2005).
- 17. Lau L. Imaging guidelines. 4th ed. Melbourne: Royal Australian and New Zealand College of Radiologists, 2001.
- 18. McNally E. Magnetic resonance imaging of the knee: is accurate and helps in making therapeutic decisions [editorial]. BMJ 2002; 325: 115-116.
- 19. Moseley J, O’Malley K, Petersen N, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 2002; 347: 81-88.
- 20. Gonski A. Scanless diagnosis of a lumbar disc protrusion. Med J Aust 1995; 162: 380-381.
- 21. Cross T, Smart R, Thomson J. Exposure to diagnostic ionizing radiation in sports medicine: assessing and monitoring the risk. Clin J Sport Med 2003; 13: 164-170.
- 22. van der Windt D, Koes B. Are corticosteroid injections as effective as physiotherapy for the treatment of a painful shoulder? In: MacAuley D, Best T, editors. Evidence-based sports medicine. London: BMJ Books, 2002: 289-317.
- 23. Paoloni J, Nelson J, Murrell G. Topical glyceryl trinitrate application in the treatment of chronic supraspinatus tendinopathy. A randomized, double-blind, placebo controlled clinical trial. Am J Sports Med 2005; 33: 8-16.
- 24. National Health and Medical Research Council. A guide to the development, implementation and evaluation of clinical practice guidelines. Canberra: NHMRC, 1998.
- 25. Donaldson WR, Diguilio M, Richmond JC. How reliable is the physical examination in the diagnosis of sports related knee injuries? In: MacAuley D, Best T, editors. Evidence-based sports medicine. London: BMJ Books, 2002: 371-388.






Abstract
Imaging should only be undertaken if it is likely to influence patient management.
The dose of ionising radiation to the patient should be considered.
Requesting the appropriate imaging method requires an understanding of the pathological process.
Plain x-ray should still generally be the first imaging technique; exceptions include some forms of superficial tendinopathy, in which ultrasound may be more appropriate, and situations where radiation exposure is contraindicated, such as in a pregnant patient.
The cost of the examination to the patient and the community should also be considered (eg, ultrasound v magnetic resonance imaging).