One of the most consistent findings in health services research is the gap between best practice (as determined by scientific evidence), on the one hand, and actual clinical care, on the other. Studies in countries such as the United States and the Netherlands suggest that at least 30%–40% of patients do not receive care according to current scientific evidence, while 20% or more of the care provided is not needed or potentially harmful to patients.1
Reflecting on this failure of implementation, most experts in healthcare improvement now emphasise the crucial importance of acquiring a good understanding of the problem, the target group, its setting and the obstacles to change in order to develop more effective strategies for change.2 For instance, a researcher may ask why some physicians in outpatient clinics have adopted strict surveillance of patients with diabetes through regular examination of feet and eyes and cardiovascular and renal risk assessments, while others have not. Is it because some physicians have a better understanding of guidelines, more support staff, more active self-care patients and/or greater financial incentives to change their behaviour? Although the answers to such questions could be crucial in developing targeted and effective implementation strategies, there is a dearth of quality overviews of factors relevant to effective implementation of evidence.1 We aim here to briefly provide such an overview, to describe how barriers and incentives to change in practice can be identified, categorised and used to tailor interventions to facilitate desired change.
Most knowledge of barriers to and incentives for change is not derived from well designed prospective studies, but rather from observational studies and theoretical reflections. A summary of some of the theories and models relating to implementing change in diabetes care is given in Box 1. Most of the theories overlap, and most are not supported by scientific research on their ability to facilitate change in clinical practice. Nevertheless, they are useful for identifying potential barriers and promoters for change. For example, a study of the failing implementation of evidence on hand hygiene in the healthcare setting1 identified a variety of barriers to change, including a lack of awareness, knowledge, reinforcement, control, social norms, leadership and facilities. Furthermore, the study showed that different theories can indeed contribute to explaining the failure to adopt best practice. A survey of perceived barriers to implementing guidelines on diabetes care showed similar results (Box 2).
In attempting to categorise the determinants for change, two complementary approaches may be used, the first focusing on characteristics of individual professionals and the second on interpersonal factors and system characteristics.
Individual professionals need to be informed, motivated and perhaps trained to incorporate the latest evidence into their daily work. For instance, Cabana et al4 used a “professional perception model”. Based on a review of 76 studies on barriers to guideline adherence, they identified salient factors as lack of awareness, lack of familiarity, lack of agreement, lack of self-efficacy (ie, the belief in one’s ability to perform a behaviour), low expectancy of favourable outcomes, inertia/lack of motivation, and perceived external barriers beyond the control of individuals. Empirical data showed that lack of awareness and motivation, as well as perceived external factors, were particularly important barriers to adopting guidelines.
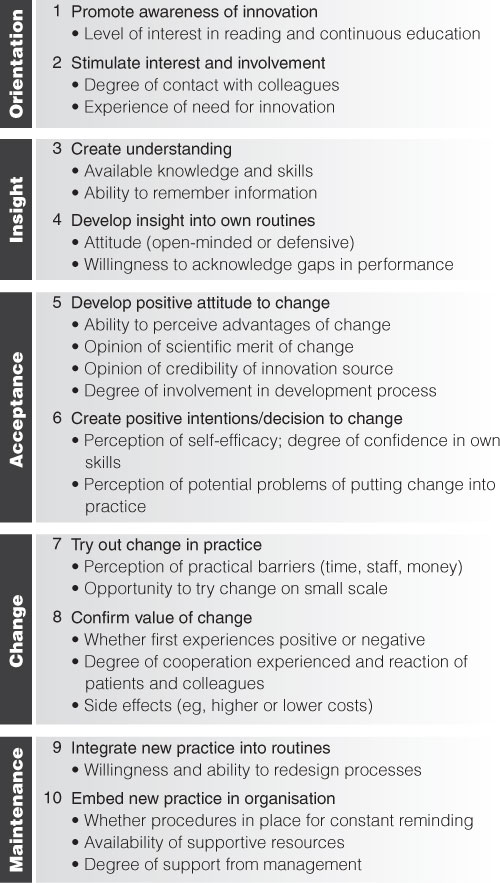
Other models describe the stepwise change process that individuals need to undergo to alter their behaviour. “Stages-of-change” theories5-8 have mostly been used to distinguish between patients with different degrees of motivation to adopt better lifestyles, but are increasingly being used in research of implementation strategies. However, a systematic review of stage-based interventions has found only limited evidence for their effectiveness.9 Integrating various stages-of-change theories, we have compiled a 10-step model for inducing change in professional behaviour (Box 3). Studies are under way to test the validity of these steps.
Healthcare professionals work in specific social, organisational and structural settings involving factors at different levels that may support or impede change. For instance, the “PRECEDE–PROCEED” model7,10,11 makes a distinction between “predisposing factors” (eg, knowledge and attitudes in the target group), “enabling factors” (eg, capacity, resources, availability of services) and “reinforcing factors” (eg, opinions and behaviour of others). Systematic reviews of studies on effective implementation of evidence and guidelines12,13 have shown that strategies that take into account factors at all three levels (predisposing, enabling and reinforcing) are the most successful.
Many quantitative and qualitative studies have shown that failure to implement evidence involves factors at different levels of the healthcare system (including characteristics of professionals and patients; team functioning; influence of colleagues; organisation of care processes; available time, staff and resources; policymaking and leadership).14,15 The example of barriers to implementing guidelines on diabetes care (Box 2) underlines such findings.
Based on analyses of the literature and research conducted at our research centre, we propose that barriers and incentives be examined at six different levels: the innovation itself, the individual professional, the patient, the social context, the organisational context, and the economic and political context (Box 4). Relatively little attention has been given so far to research on characteristics of the innovation itself that affect its likelihood of being implemented.1
Information on potential barriers and incentives for change can be obtained in various ways, including interviews, surveys, focus groups, Delphi methods, observation in the care setting, auditing records of routinely collected data, and analysis of documents. This information can be used to tailor implementation strategies.
There is limited evidence to show whether tailored interventions are more effective. We do know that some efforts at tailored intervention have been unsuccessful. For instance, a UK study of general practitioners used face-to-face interviews, guided by psychological theory, to identify barriers to implementing guidelines on depression.16 However, this tailored intervention did not change professional performance any more than distribution of the guidelines only. Another study, in Norwegian general practice, on guidelines for sore throat and urinary tract infections used multiple methods to identify barriers to change: observations, telephone interviews, a postal survey and data extracted from medical records.17 A multifaceted intervention was developed, tailored to the problems found, including a short summary of the guidelines, patient education materials, computer-based decision support, extra fees for telephone consultations, and interactive courses for professionals. Despite this intensive intervention, no change in the main outcomes was found. Process evaluations after completion of the project suggested that lack of time and resources contributed significantly to this failure.
Thus, we still lack the information on how to effectively tailor interventions to produce change. Some new methods, such as “intervention mapping”, are being devised, but their usefulness is yet to be tested.18
Although we are now aware of the importance of understanding factors that facilitate or hinder change in clinical practice, we still lack in-depth knowledge of which factors are decisive in achieving which changes, in which target groups and which settings. Better use and testing of existing theories in prospective trials may help us, along with studies to test the implementation processes, in-depth analyses of putative success/failure factors, and meta-analyses of research on improvement programs. In the absence of this knowledge, the success or failure of an implementation intervention may well be left to chance.
1: Theories/models relating to implementing change to improve diabetes care
Theories/models |
Important factors |
Lessons for improving diabetes care |
|||||||||
Relating to individual professionals |
|||||||||||
Cognitive |
Mechanisms of thinking and deciding; balancing benefits and risks |
Provide convincing information on diabetes care evidence |
|||||||||
Educational |
Individual learning needs and styles |
Involve professionals in improving diabetes care; define personal improvement plan |
|||||||||
Attitudinal |
Attitudes, perceived behavioural control, self-efficacy, social norms |
Convince professionals of importance; show that they can do it and that others will follow |
|||||||||
Motivational |
Different motivational stages with different factors/barriers |
Tailor interventions to different target groups (doctors, nurses, patients) within diabetes care |
|||||||||
Relating to social context |
|||||||||||
Social learning |
Incentives, feedback, reinforcement, observed behaviour of role models |
Model best practices of diabetes care; give feedback on progress |
|||||||||
Social network and influence |
Existing values and culture of network, opinion of key people |
Use opinion leaders in network to improve routines |
|||||||||
Patient influence |
Perceived patient expectations and behaviour |
Involve patients actively in improving their care; stimulate self-management |
|||||||||
Leadership |
Leadership style, type of power, commitment of leader |
Obtain commitment of management to improving diabetes care |
|||||||||
Relating to organisational and economic context | |||||||||||
Innovativeness of organisation |
Extent of specialisation, decentralisation, professionalisation, functional differentiation |
Take into account type of organisation; encourage teams to develop their own plans for change |
|||||||||
Quality management |
Culture, leadership, organisation of processes, customer focus |
Reorganise processes for diabetes care; develop systems for continuous improvement |
|||||||||
Complexity |
Interactions between parts of a complex system, behavioural patterns |
Focus on system as a whole; find main “attractors” for improving diabetes care |
|||||||||
Organisational learning |
Capacity and arrangements for continuous learning in organisation |
Encourage continuous exchange of expertise on diabetes at all levels of organisation |
|||||||||
Economic |
Reimbursement arrangements, rewards, incentives |
Reward achievement of treatment targets in diabetes care |
|||||||||
2: Perceived barriers to implementing guidelines on diabetes care, from a survey of physicians in general hospitals in the Netherlands3
Cognitive factors |
Proportion of respondents citing reason (n = 96; 91% response rate) |
||||||||||
|
|||||||||||
Guideline will not be read |
44% |
||||||||||
Insufficient evidence base |
35% |
||||||||||
Lack of knowledge of complications |
34% |
||||||||||
Attitude of physicians |
|
||||||||||
Guideline too rigid |
56% |
||||||||||
Use of guideline costs too much time |
54% |
||||||||||
Don’t like imposed activities |
50% |
||||||||||
Social and organisational context |
|
||||||||||
No support by management |
44% |
||||||||||
Disagreement among physicians |
35% |
||||||||||
Heavy workload of physicians |
81% |
||||||||||
Lack of necessary staff |
46% |
||||||||||
Economic context |
|
||||||||||
No financial compensation |
57% |
||||||||||
3: Potential barriers/incentives in relation to a proposed 10-step model for inducing change in professional behaviour6
4: Barriers to and incentives for change at different levels of healthcare
Level |
Barriers/incentives |
||||||||||
Innovation |
Advantages in practice, feasibility, credibility, accessibility, attractiveness |
||||||||||
Individual professional |
Awareness, knowledge, attitude, motivation to change, behavioural routines |
||||||||||
Patient |
Knowledge, skills, attitude, compliance |
||||||||||
Social context |
Opinion of colleagues, culture of the network, collaboration, leadership |
||||||||||
Organisational context |
Organisation of care processes, staff, capacities, resources, structures |
||||||||||
Economic and political context |
Financial arrangements, regulations, policies |
||||||||||
- 1. Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change. Lancet 2003; 362: 1225-1230.
- 2. Grol R. Beliefs and evidence in changing clinical practice. BMJ 1997; 315: 418-421.
- 3. Dijkstra R, Braspenning J, Uiters E, et al. Perceived barriers to the implementation of diabetes guidelines in hospitals in the Netherlands. Neth J Med 2000; 56: 80-85.
- 4. Cabana M, Rand C, Power N, et al. Why don’t physicians follow clinical practice guidelines? JAMA 1999; 282: 1458-1465.
- 5. Rogers E. Diffusion of innovations. New York: Free Press, 1983.
- 6. Grol R. Implementing guidelines in general practice care. Qual Health Care 1992; 1: 184-191.
- 7. Davis D, Evans M, Jadad A, et al. The case of knowledge translation: shortening the journey from evidence to effect. BMJ 2003; 327: 33-35.
- 8. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot 1997; 12: 38-48.
- 9. Riemsma RP, Pattenden J, Bridle C, et al. A systematic review of the effectiveness of interventions based on a stages-of-change approach to promote individual behaviour change. Health Technol Assess 2002; 6(24): 1-231.
- 10. Green LW, Kreuter MW. Health promotion planning: an educational and environmental approach. 2nd ed. Mountain View, Calif: Mayfield, 1991.
- 11. Green LW, Eriksen MP, Schor EL. Preventive practices by physicians: behavioral determinants and potential interventions. Am J Prev Med 1988; 4(4 Suppl): 101-107.
- 12. Davis D, Thomson M, Oxman A, Haynes R. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA 1995; 274: 700-705.
- 13. Solomon DH, Hashimoto D, Daltroy L, Liang M. Techniques to improve physicians’ use of diagnostic tests. JAMA 1998; 280: 2020-2027.
- 14. Oxman A, Flottorp S. An overview of strategies to promote implementation of evidence based health care. In: Silagy C, Haines A, editors. Evidence based practice in primary care. London: BMJ Books, 2001.
- 15. Solberg L. Guideline implementations: what the literature doesn’t tell us. Jt Comm J Qual Improv 2000; 26: 525-537.
- 16. Baker R, Reddish S, Robertson N, Hearnshaw H. Randomised controlled trial of tailored strategies to implement guidelines for the management of patients with depression in general practice. Br J Gen Pract 2001; 51: 737-741.
- 17. Flottorp S, Havelsrud K, Oxman AD. Process evaluation of a cluster randomized trial of tailored interventions to implement guidelines in primary care — why is it so hard to change practice? Fam Pract 2003; 20: 333-339.
- 18. Grol R, Baker R, Moss F, editors. Quality improvement research: understanding the science of change in health care. London: BMJ Books, 2003.





Abstract
To bridge the gap between scientific evidence and patient care we need an in-depth understanding of the barriers and incentives to achieving change in practice.
Various theories and models for change point to a multitude of factors that may affect the successful implementation of evidence. However, the evidence for their value in the field is still limited.
When planning complex changes in practice, potential barriers at various levels need to be addressed. Planning needs to take into account the nature of the innovation; characteristics of the professionals and patients involved; and the social, organisational, economic and political context.