Australians inhabit a continent of extraordinary natural beauty and biodiversity. But in recent years our lives have been defined by unprecedented extreme weather events — catastrophic bushfires blanketing cities in smoke for months, multiple once in a century floods, severe droughts that devastate rural communities, and record‐breaking heatwaves — all of which have impacts on our health system. Climate change is not a future risk with targets for 2050 or 2100: it is a process that is reshaping Australian lives and health and wellbeing today.
The increase in the frequency and severity of extreme weather events poses significant challenges, and climate scientists warn that these events will intensify in coming decades.1,2 Heat, for example, is already a significant contributor to mortality in Australia,3 and will increasingly affect our health and wellbeing as our planet continues to warm. For our health system — federal and state government health departments, hospital networks and individual facilities, primary care and individual doctors — the question is how best to understand and integrate the effects of environmental variables on health and wellbeing into clinical practice to reduce the adverse impact of climate change on our health.
In this issue of the MJA, Stewart and colleagues report the findings of their clinical trial of a program for reducing bio‐behavioural vulnerability to weather events in people with multimorbid heart disease.4 Their conclusion is sobering but informative: the intervention “was ineffective in increasing the proportion of days alive and out of hospital for people … after hospital admissions with multimorbid heart disease.” But they also note “the efficacy of our intervention could be improved by modifying its components and applying it in a more targeted manner to reduce the impact of weather‐triggered events.”4
Despite its negative findings, this trial illustrates a critical inflection point in how we conceptualise health and disease in the context of an increasingly volatile climate, and the investigators are to be commended for explicitly incorporating environmental factors into their intervention. This is a significant shift for clinical work, but also crucial territory for exploration and research as our climate changes.
For decades, medical education, training, and research, and health care more broadly, have been served well by a conceptual model based on a biopsychosocial framework.5 However, environmental changes — increasing temperature, extreme weather events, and the changing climate, as well as water, soil and air contamination — are factors that will increasingly influence health and wellbeing during the 21st century. The biopsychosocial model must evolve to more explicitly acknowledge the foundational relationship between human health and the environment.
Leading health organisations, including the World Health Organization, recognise climate change as a fundamental threat to human health6 and one of the greatest health problems for this century. We must improve our understanding of the importance of the environment for health, but this is difficult because of the complex epidemiological science, definitional debate, and intricate interdependencies among environmental variables. Research and clinical interventions for better reflecting this complexity in practice are crucial.
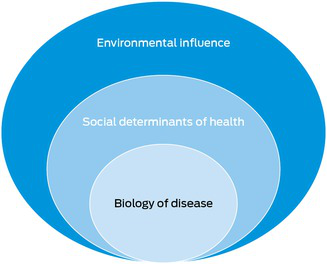
A biology–society–environment model (Box) would be an evolution in our approach and could be applied to any specialty and condition. For example, genetics, hypertension, and smoking are important biological variables in cardiovascular disease; education, geography, and socio‐economic status are also influential. Finally, the environment affects the incidence and natural history of cardiovascular disease. Air pollution, agricultural and nutritional change, soil quality, extreme weather events, including floods, heatwaves, and bushfires, all increase the incidence of cardiovascular disease.7 The environment is the final layer of the milieu that protects or harms us, associated with multiple acute and chronic diseases. As these three layers — biology, society, and environment — are incorporated routinely into medical research and clinical management, the opportunities for reducing the burden of disease are remarkable.
Developing a framework for environmental influence could improve our understanding of human health. Core elements include the air we breathe, the food we eat, and the water we need to survive. Where we live and how we live there can both exacerbate and ameliorate the health impact of changes in climate, biodiversity, and weather events, the key environmental variables. These variables and the core elements provide a framework for the relationship between environment and health. Including the layers of biology, society, and environment in health care research and interventions will position us better to protect and preserve health and wellbeing as climate changes during this century and beyond.
The increase in the frequency and severity of extreme weather events and changes to our natural environment and its biodiversity affect our health and wellbeing in myriad ways across all stages of life and across all medical specialties. Our health care sector should better acknowledge and understand the foundational relationship between people and place. Incorporating a model of biology, society, and environment when collecting health care data and undertaking research and interventions will place us in a better position to protect and preserve health and wellbeing, not just for people with multimorbid heart disease, but for all of us in a challenging century for planetary health.
Provenance: Commissioned; not externally peer reviewed.
- 1. The Intergovernmental Panel of Climate Change. Climate change 2022: impacts, adaptation and vulnerability. 28 Feb 2022. https://www.ipcc.ch/report/ar6/wg2 (viewed May 2025).
- 2. Commonwealth Scientific and Industrial Research Organisation. Climate projections for Australia. Updated 23 Feb 2024. https://www.csiro.au/en/research/environmental‐impacts/climate‐change/Climate‐change‐information (viewed May 2025).
- 3. Longden T, Quilty S, Haywood P, et al. Heat‐related mortality: an urgent need to recognise and record. Lancet Planet Health 2020; 4: e171.
- 4. Stewart S, Patel SK, Lancefield TF, et al. Promoting resilience to weather‐related and seasonal provocations to health in people with multimorbid heart disease: a prospective pragmatic, randomised trial. Med J Aust 2025; 223: 000‐000.
- 5. Engel GL. The need for a new medical model: a challenge for biomedicine. Science 1977; 196: 129‐136.
- 6. World Health Organization. Climate change and health. 12 Oct 2023. https://www.who.int/news‐room/fact‐sheets/detail/climate‐change‐and‐health (viewed May 2025).
- 7. Rajagopalan S, Landrigan PJ. Pollution and the heart. N Engl J Med 2021; 385: 1881‐1892.





No relevant disclosures.