The known: Aboriginal and Torres Strait Islander people who need dialysis have low access to waitlisting for kidney transplantation.
The new: Barriers to waitlisting occur at all steps, from not commencing work‐up assessments to temporary and permanent contraindications. While cardiovascular disease and obesity were contraindications proportionally equal in Aboriginal and Torres Strait Islander and non‐Indigenous patients, delayed work‐up assessments were more frequent in Aboriginal and Torres Strait Islander patients.
The implications: Transplantation equity requires a prioritised investment in system and quality improvements, from enhanced referral and assessment pathways to optimising all elements of care and ongoing accountability measures.
Access to kidney transplantation remains a persistent inequality within Australia's health care systems. Despite a four‐to‐five times higher burden of kidney failure (previously known as “end‐stage kidney disease”),1 Aboriginal and Torres Strait Islander people, compared with other Australians, have lower access to kidney transplantation — the optimal treatment for kidney failure that significantly enhances both quality and length of life.2,3 In 2023, only 16% of Aboriginal and Torres Strait Islander patients with kidney failure were living with a functioning transplant, compared with 48% of non‐Indigenous patients.1
Achieving transplantation is a complex process for both patients and the health care system, as it depends on a series of decisions that confirm the patient–clinician acceptability based on multiple health care assessments (Box 1).4 To receive a deceased donor transplant, patients must undergo a series of work‐up tests and transplant‐specific surgical and medical assessments before they can be placed on the active waitlist. Once on the waitlist, patients are then allocated an organ based on national algorithms provided they remain in good health and on the active waitlist. Evidence from the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA) shows that time from waitlisting to transplantation is similar for all Australians.5 The core issue (and inequity) lies in achieving active waitlisting status.
For Aboriginal and Torres Strait Islander people with kidney failure, the pivotal question is “am I on the list?“6 Given the complexity of the process, achieving active waitlisting is a good litmus test of a patient's health, the strength of patient–clinician partnerships, and the performance of an equitable health care system, particularly in the context of the structural inequities imposed through the ongoing impacts of colonisation, racism and intergenerational trauma. These systemic factors drive disparities across the spectrum of kidney care7 but are particularly highlighted in achieving waitlisting.
Efforts to address these disparities have been ongoing, with research highlighting systemic barriers; these include institutional racism, miscommunication, and a lack of culturally appropriate, safe and reliable resources available to Aboriginal and Torres Strait Islander people seeking kidney care.8,9 The inequity was underscored again in 2019,10 which led the federal government to fund the National Indigenous Kidney Transplantation Taskforce (NIKTT) to improve access to transplantation in collaboration with patients, community leaders, the Transplantation Society of Australia and New Zealand, and jurisdictional clinical advocates.11 A specific activity of the NIKTT was to assess access to waitlisting through enhanced data collection.
In December 2020, just 2% of Aboriginal and/or Torres Strait Islander patients (47 of 2046) were waitlisted, compared with 8% of non‐Indigenous patients (904 of 11 214) (odds ratio, 0.27 [95% confidence interval, 0.19–0.36]; P < 0.001). The numbers waitlisted for the first time in each year are shown Box 2.12 In response to this disparity and strong patient advocacy, the NIKTT prioritised improving equity in access to waitlisting.10 To achieve this, the NIKTT developed a pilot data collection tool within ANZDATA to capture clinician‐reported reasons for non‐waitlisting, aiming to pinpoint barriers and opportunities to enhance patient care and transplantation equity. This was implemented initially for the 2019 data collection and again in 2020. To our knowledge, the clinician‐reported reasons for non‐waitlisting have not been previously examined in Australia.
This article presents the findings from this pilot data collection as a cross‐sectional analysis of the 2020 data collection, examining both individual and systemic barriers to achieving active waitlisting for Aboriginal and Torres Strait Islander patients with kidney failure.
Methods
Research prioritisation
This analysis was prioritised within the NIKTT Data Working Group following patient‐partnered meetings where Aboriginal and Torres Strait Islander people living with kidney failure advocated for transparency and efficiency in attaining kidney transplantation.8
Study design
This was a retrospective cross‐sectional analysis of all patients undergoing kidney replacement therapy in 26 renal units in Australia as of 31 December 2020. We adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines to ensure comprehensive and transparent reporting of our study (Supporting Information, section 1, table 1).13
Data sources
ANZDATA is a clinical quality registry that collates data on all people in Australia and Aotearoa New Zealand who undergo kidney replacement therapy. Data are submitted from all renal units and transplant centres on an annual basis. People seeking kidney transplantation for the first time, including those waitlisted for multiple organ transplantation (eg, pancreas and kidney) as well as kidney‐only transplantation, were included in this analysis. ANZDATA collects data from treating renal units, and receives data about waitlisting for transplantation from OrganMatch.14
Data variables
ANZDATA routinely reports on clinical information provided by renal units, including date of birth, location (state or territory) of treatment at the end of the year, kidney replacement modality (haemodialysis, peritoneal dialysis, transplantation), time on dialysis, primary kidney disease, diabetes as a comorbidity at the end of the year, other comorbidities (such as coronary artery, cerebrovascular and peripheral vascular disease, and chronic lung disease), weight and height, smoking status, and late referral (defined as first encounter with the renal unit fewer than 3 months before dialysis was started). This health equity analysis focuses on two main groups — Aboriginal and Torres Strait Islander people and other Australians (non‐Indigenous) — identified using coded responses to the ANZDATA primary ethnicity field.
Novel data capture
To accompany the routine ANZDATA survey, we designed the Transplant Assessment Stage ancillary form (form TA; Supporting Information, section 1, figure 1),15 which was provided to participating renal units as a voluntary table, added to the existing annual ANZDATA collection. This form prompted respondents to select where in the transplant pathway each patient was at the end of 2020, focusing on seven points on the pathway:
- eligibility assessment not yet conducted;
- eligible — work‐up commenced but not completed;
- eligible — work‐up complete, awaiting assessment by transplanting unit;
- not eligible — temporary contraindications;
- not eligible — permanent contraindications;
- not ready to pursue a transplant — patient preference; and
- already on waitlist.
If a patient was listed as not eligible on the assessment stage, outcome reasons were sought and respondents were provided with several reasons to choose from (Supporting Information, section 1, figure 1). If respondents chose an outcome reason which contained the word “specify,” the respondent was prompted to provide one or more free‐text reasons for non‐waitlisting. In the clinical context of transplantation eligibility, “temporary” contraindications imply reversible (or potentially treatable) factors; this is in contrast to “permanent” contraindications, which (if present) imply that a patient will never be eligible for transplantation.
All adult renal units in Australia were invited to participate in the data collection. However, the NIKTT recognised that the substantial additional data collection effort required was a barrier to implementation; to address this, funding support was offered to the 20 Australian renal units that provided dialysis care for the great majority of Aboriginal and Torres Strait Islander people across Australia in 2020.
Statistical analysis
The analysis was primarily descriptive, and aimed to investigate the characteristics of adults, alive and receiving dialysis in the 2020 ANZDATA annual survey reporting period, and to determine the reasons for non‐waitlisting of those not on the active waitlist. While age itself is not a barrier to transplantation,4 we stratified data by age — and in particular < 65 years versus ≥ 65 years — as younger people were expected to have no contraindications, or only temporary contraindications to waitlisting. Confidence intervals were calculated using a binomial distribution, and simple categorical comparisons were conducted using χ2 analyses. To account for unit‐based practice variation, comparisons of the reasons for non‐waitlisting were also conducted using a hierarchical logistic regression model, with a random effect for treating unit. No adjustments were made for multiple comparisons. All analyses were performed using Stata version 18.0 (StataCorp).
Positionality statement
This study was co‐led by Jaquelyne Hughes, a Torres Strait Islander woman (Wagadagam tribe) and Co‐Chair of the NIKTT, with Stephen McDonald. Kelli Karrikarringka Owen, a Kaurna, Narungga and Ngarrindjeri woman and the NIKTT National Community Engagement Coordinator, and Matilda D’Antoine, a Paakantyi woman from Far West New South Wales, contributed as authors and knowledge holders. Their leadership and lived experience shaped the framing, interpretation and equity‐centred focus of the work. The broader team included non‐Indigenous collaborators: Stephen McDonald (Executive Director of ANZDATA and Co‐Chair of the NIKTT), Katie Cundale (Program Director, NIKTT), Christopher Davies and Feruza Kholmurodova (biostatisticians, ANZDATA), and Kerry Dole (Co‐Lead of the NIKTT Data Working Group), who are of Australian, British and Central Asian backgrounds. Their roles supported the statistical analysis, project delivery, and registry and NIKTT management of this work. The reporting of the study was guided by the Consolidated Criteria for Strengthening the Reporting of Health Research Involving Indigenous Peoples (CONSIDER) statement (Supporting Information, section 2).16
Ethics approval and Indigenous governance
ANZDATA data collection is conducted under the auspices of the Central Adelaide Local Health Network Human Research Ethics Committee (HREC/17/RAH/408). The data extraction and analyses for this NIKTT project were approved by the Aboriginal Health Research Ethics Committee of the Aboriginal Health Council of South Australia (AHREC protocol number 04‐24‐1111). The project was developed to comply with ANZDATA's Indigenous data governance policy17 and was endorsed by the ANZDATA Aboriginal and Torres Strait Islander Health Working Group, which includes Aboriginal and Torres Strait Islander clinicians experienced in kidney health care, scientists, and lived‐experience members.
Results
Overall characteristics
Twenty‐six Australian renal units participated in the additional data collection and provided dialysis care for 7960 adults, including 1832 Aboriginal and Torres Strait Islander people, at the end of 2020 (Box 3). This comprised 90% (1832/2046) of Aboriginal and Torres Strait Islander people receiving dialysis treatment in Australia at the end of 2020 and 55% (6128/11 214) of non‐Indigenous patients receiving dialysis.
The median age of patients receiving dialysis was lower for Aboriginal and Torres Strait Islander people (57 years; interquartile range [IQR], 49–64 years) than for non‐Indigenous people (68 years; IQR, 57–77 years). Larger proportions of Aboriginal and Torres Strait Islander people were female (1073 [59%] v 2214 [36%]) and receiving haemodialysis (1703 [93%] v 4744 [77%]), and the median time on dialysis was longer for Aboriginal and Torres Strait Islander people (3.6 years [IQR, 1.5–6.6 years] v 2.5 years [IQR, 1.1–4.9 years]) (Box 3). Diabetes was reported more commonly, both as the principal cause of kidney failure (1252 [71%] v 2207 [38%]) and as a comorbidity (1479 [82%] v 3088 [53%]) for Aboriginal and Torres Strait Islander people (Box 3). Eighty‐seven per cent of all Aboriginal and Torres Strait Islander patients (1556) in this analysis received care within three jurisdictions: Northern Territory (676 [38%]), Queensland (434 [24%]) and Western Australia (446 [25%]).
Waitlisting status
Waitlisting status was coded as active for only 36 of 1832 (2%) Aboriginal and Torres Strait Islander patients in the 2020 cohort who were receiving dialysis and had not had a kidney transplant registered (Box 3). This proportion was lower than the 8% (512 of 6128) of non‐Indigenous patients in 2020 who were recorded as being on the active waitlist (Box 3).
Waitlist stage
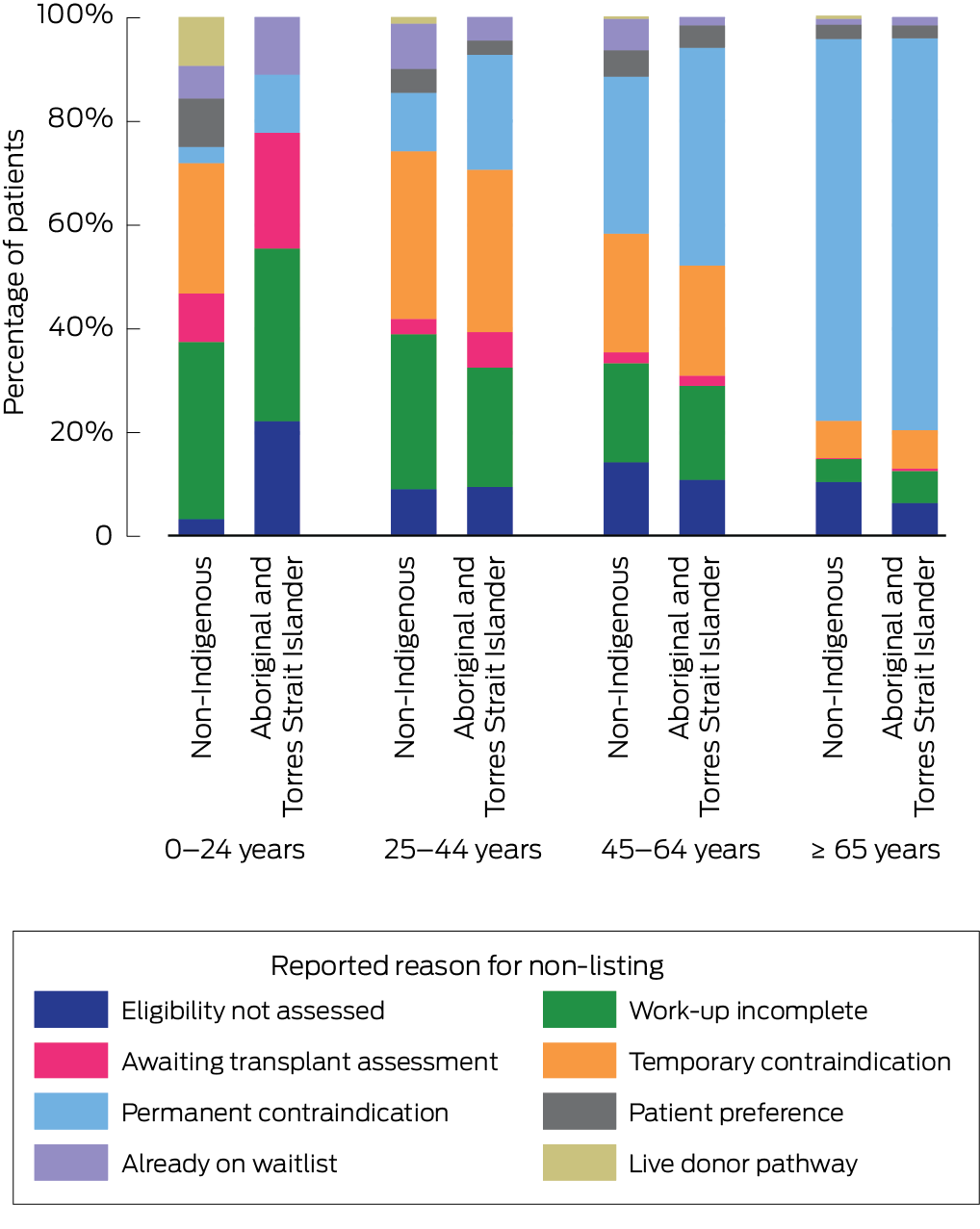
Reported reasons for why patients were not waitlisted are shown in Box 4 (and in more detail in the Supporting Information, section 3, table 1). Work‐up incomplete was a commonly reported reason for patients not being on the active waitlist; 28% (158 of 562) of 0–44‐year‐old patients had an assessment outcome of work‐up commenced but not completed, compared with 11% (535 of 4846) of people aged ≥ 45 years. Among people aged < 25 years, greater proportions of Aboriginal and Torres Strait Islander patients, compared with non‐Indigenous patients, had eligibility not assessed (two of nine [22%] v one of 32 [3%]) and awaiting transplant assessment (two of nine [22%] v three of 32 [9%]) given as reasons for not being waitlisted.
Not eligible for waitlisting
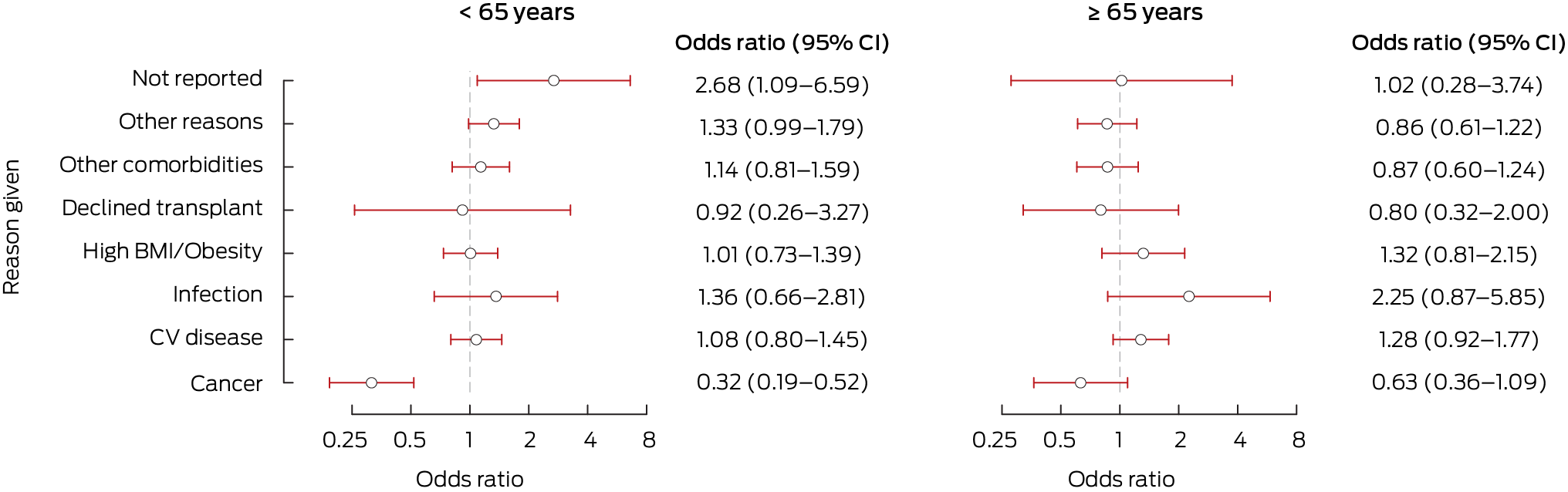
Reasons cited as temporary or permanent contraindications preventing waitlisting are shown in Box 5. Cardiovascular disease was the most common contraindication reason recorded across all people (regardless of age group and ethnicity) (Supporting Information, section 3, table 2). Among those younger than 65 years, non‐eligibility for waitlisting was attributed to:
- cancer in 4% (28 of 733) of Aboriginal and Torres Strait Islander people and 11% (86 of 794) of non‐Indigenous people (P < 0.001);
- obesity (or high body mass index [BMI]) in similar proportions regardless of ethnicity (163 [22%] v 207 [26%]; P = 0.96);
- other comorbidities (with the option to specify) in similar proportions regardless of ethnicity (193 [26%] v 135 [17%]; P = 0.45); and
- other reasons (with the option to specify) in similar proportions regardless of ethnicity (233 [32%] v 192 [24%]; P = 0.06).
Among those aged 65 years or older, obesity was cited as a reason for non‐waitlisting for 30 Aboriginal and Torres Strait Islander patients (10%) and 163 non‐Indigenous patients (9%) (P = 0.6).
Exploring other reasons
Further analysis was performed on the free‐text answers that clinicians were encouraged to provide. Clinicians gave additional reasons for non‐waitlisting for 2002 patients (612 Aboriginal and Torres Strait Islander patients; 1390 non‐Indigenous patients). All free‐text responses were recoded into common categories (Supporting Information, section 3, table 3). Terms such as “compliance,” “adherence” and “attendance” were re‐classified into “patient safety”; as a reason for non‐waitlisting, this did not significantly differ by ethnicity for those aged < 65 years (105 [14%] v 70 [9%] for Aboriginal and Torres Strait Islander patients versus non‐Indigenous patients, respectively) but was significantly higher for Aboriginal and Torres Strait Islander patients among those aged ≥ 65 years (11 [4%] v 13 [1%]; P < 0.001). Substance use was more frequently cited as a reason for non‐waitlisting for Aboriginal and Torres Strait Islander patients younger than 65 years (39 [5%] v 11 [1%]; P = 0.002), and mental health was less frequently cited (10 [1%] v 30 [4%]; P = 0.004).
Discussion
Kidney transplantation is the preferred treatment for kidney failure where medically possible. This article builds on previous evidence showing that a major block in the transplantation pathway for Aboriginal and Torres Strait Islander people is being added to the active transplant waitlist. We asked why patients were not added to the active waitlist, using data from participating renal units that provided care for the majority of Aboriginal and Torres Strait Islander patients receiving dialysis in Australia. The clinician‐reported reasons for non‐waitlisting that we discuss here occur within a broader context shaped by systemic racism and multilayered institutional barriers.18 Addressing such barriers to improve access to transplantation requires not only recognising and dismantling structural contributors to inequity, but also supporting clinicians to critically reflect on their and their colleagues’ own practices. For patients, it is the clinician's responsibility to not accept racist practices on their behalf. For clinicians, it is our responsibility as a health care community with integrity to actively challenge and reform discriminatory systems so that racism in care is identified, addressed and disrupted through action and accountability.
From our analysis, we found that most patients were not waitlisted due to incomplete work‐up, because they were awaiting transplant assessment, or because their eligibility had not yet been assessed. Aboriginal and Torres Strait Islander patients receiving dialysis who were not eligible for the waitlist were younger than their non‐Indigenous counterparts, with a greater proportion of young Aboriginal and Torres Strait Islander patients (aged < 25 years) having incomplete work‐up or awaiting transplant assessment. While we have attempted to define this problem through this analysis, questions remain around why these delays occur, particularly for younger people, and what can be done to accelerate the waitlisting process. We believe that analyses that monitor and report how long patients remain in these stages are crucial for identifying areas for practice change.
Outside of reasons listed as “other,” the most common contraindications to waitlisting (regardless of patient group) related to cardiovascular disease and high BMI or obesity. Interpretation of our results needs to account for both relative and absolute rates. While the proportions of people not waitlisted for these broad categories of cardiovascular disease and obesity appear similar among Aboriginal and Torres Strait Islander and non‐Indigenous people on dialysis — about a quarter of patients for both categories — the impact of these conditions on Aboriginal and Torres Strait Islander people is greater given the overall higher prevalence of non‐waitlisting for Aboriginal and Torres Strait Islander people receiving dialysis. This higher prevalence of antecedent conditions necessitates more intensive and prolonged health optimisation efforts to achieve transplant eligibility for Aboriginal and Torres Strait Islander patients.19,20 While current national transplant guidelines do not specifically refer to obesity in recipient eligibility criteria,4 obesity has been associated with a higher rate of surgical complications during and following transplantation in people with additional comorbidities21 (although recent systematic reviews and meta‐analyses disagree on its impact22,23,24,25). In practice, most Australian transplant units use BMI greater than 35 kg/m2 as a non‐acceptance criterion, with the decision typically based on assessment of major postoperative surgical risk.26,27 Further studies are needed on clinical practice models in Australia that promote safe outcomes with no BMI restriction and/or clinical practice models that reduce the burden of abdominal obesity before waitlisting, and maximise patient and graft survival and wound healing after transplantation. There is a growing number of models of care designed to facilitate weight loss for Aboriginal and Torres Strait Islander people, beyond lifestyle and dietetic advice, including the Too Deadly for Diabetes program. However, these models are not uniformly funded, which is itself another contributor to waitlisting inequity.28 Solutions must consider local context and leadership from Aboriginal and Torres Strait Islander peoples to achieve high value outcomes.29,30
Chaturvedi and colleagues31 challenged the terms “non‐compliance” and “non‐adherence”, as terms such as these assume an individual (patient)‐level problem following medical advice. They instead suggest that the problem lies within broader system‐level factors (such as policies and resourcing), preventing efficient health optimisation.31 In our analysis, we reclassified mentions of adherence to patient safety, indicating that the first level of concern of safely participating in clinical care lies within clinical structures and processes. Furthermore, there is no standardised metric to evaluate non‐adherence, leaving it as a subjective judgement by the clinical team and therefore vulnerable to bias. Substance misuse is similarly evaluated subjectively; we do not know the extent to which differences reported here reflect true differences in rates of substance misuse or bias in evaluation. Regardless, both non‐adherence and substance misuse are manifestly reversible barriers. Addressing these issues around patient safety and ensuring that patients have the support to continue treatment both during work‐up assessment and after transplantation are essential. Such change requires not only funded and human‐resourced patient‐centred models of care, but also deliberate efforts by clinicians to reflect on and transform their own biases and practices as part of meaningful systemic reform.32,33
Historically, the overall waitlisting rates for individual renal units were not publicly reported by ANZDATA. The NIKTT recommended specific reporting of waitlisting rates for Aboriginal and Torres Strait Islander people, for both the renal units where people receive their routine care and the affiliated transplant centres.11 Consultation with consumers engaged across NIKTT activity indicated strong support for this approach34 and, following the initial period of NIKTT work, funding was secured to develop a data dashboard to track equity metrics in transplantation. Understanding the differential access to transplantation between units and transplant centres will be useful to guide future research into regional disparities and support accountability by strengthening transparency and performance across health systems nationally. With national dashboard funding in place — and 2020 marking the first year of coronavirus disease 2019 (COVID‐19) pandemic‐related data — reporting of post‐2020 trends in access and equity will be possible.
Limitations
The Transplant Assessment Stage form was an enhanced data reporting opportunity beyond routine ANZDATA activity. We identified two main challenges: firstly, most renal units did not systematically record the reasons for non‐placement on waiting lists and there are no national standards for categorisation of this; and secondly, systematic reporting of patients not waitlisted required substantial workforce input that was not readily available or sustainable within current resourcing. Related to this is the substantial number of differing responses in the “other medical” category and number of missing responses. If there is to be ongoing reporting in this area, further work is needed to refine these categories to reach a balance between information that is clinically relevant and able to be collected in a sustainable manner. A policy review to identify the staff resources needed to achieve equity in the clinical teams that enable assessment and waitlisting may accelerate equity in transplantation.
The renal units that participated included almost 90% of Aboriginal and Torres Strait Islander people receiving dialysis nationally, which is likely to be highly representative of the overall cohort in 2020, so inferences around barriers to waitlisting for Aboriginal and Torres Strait Islander people are likely appropriate. It is possible that the barriers at participating units differ from those at non‐participating Australian units, but given that the participating units provide care for about 60% of all non‐Indigenous dialysis patients, we believe this effect likely to be modest and that inferences based on the results are relevant to this cohort. The need to remunerate participating units to cover the burden of the extra data collection underscores the challenges of collecting these data.
As in other areas of health care, the waitlisting of Aboriginal and Torres Strait Islander patients by renal units in our analysis may be under‐reported — ANZDATA has no procedures for validating completeness of ethnicity information.35
For our work, the meanings of terms such as age, frailty, weight, BMI, compliance and social issues were taken at face value. Formal and standardised assessments of the subjectivity of such terms should be investigated, alongside practice improvements that adopt the newly created culturally safe kidney clinical care guidelines for First Nations Australians,36 and the Australian Health Practitioner Regulation Agency's legal obligations for delivery of cultural safety.37
Conclusion
Aboriginal and Torres Strait Islander peoples in Australia continue to face considerable disparity in access to kidney transplantation, reflected through reduced access to waitlisting. Our findings highlight low rates of active transplant waitlisting in 2020 for Aboriginal and Torres Strait Islander people receiving dialysis in Australia, with barriers occurring at most stages of the transplantation pathway. Addressing these inequities requires targeted equity‐enabling efforts to streamline and expedite work‐up processes. Implementing practice improvement that supports excellent and culturally safe patient–clinician partnerships requires addressing challenges across multiple sectors, starting with denormalising the disproportionate burden of kidney disease and reframing the internalised racism of health systems. Governments and care providers face a cogent opportunity to prioritise practice change and structural reform that effectively manages and mitigates these barriers, ensuring culturally safe and equitable access to care.
Box 1 – Transplant assessment process: activities and outcomes from kidney failure to achieved transplantation, with waitlisting assessment decisions highlighted
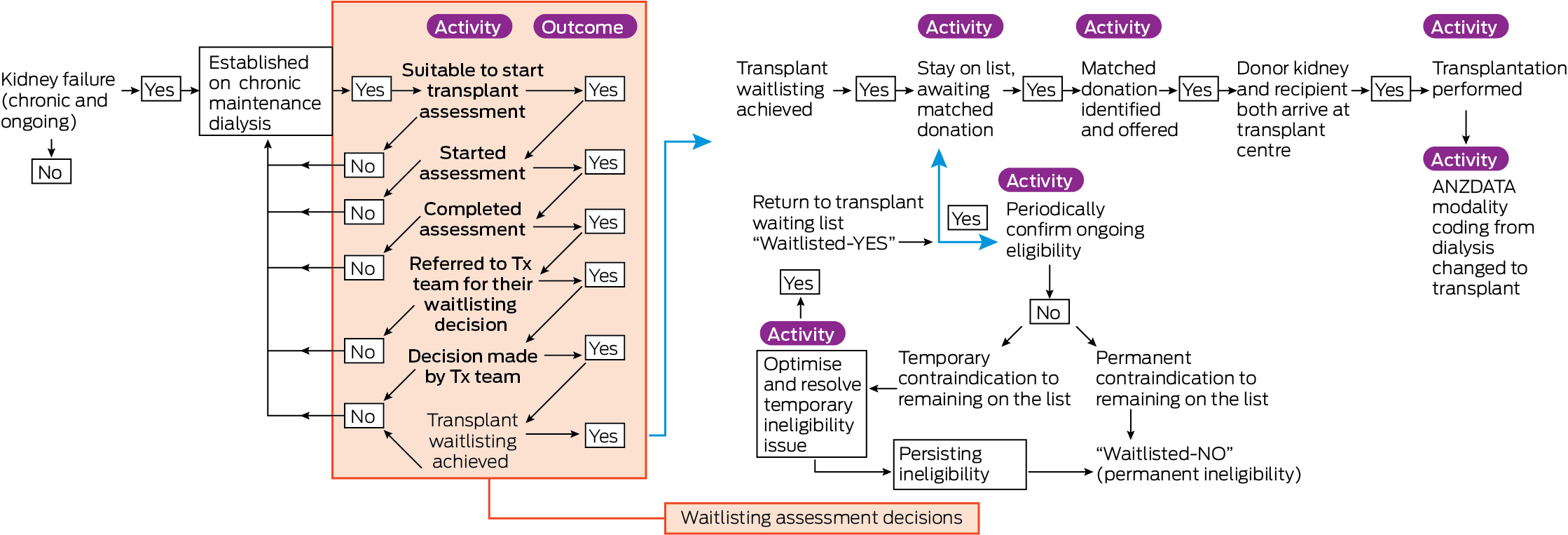
ANZDATA = Australia and New Zealand Dialysis and Transplant Registry; Tx = transplant. Source: Figure reproduced with permission from Professor Jaquelyne Hughes, who is the copyright holder.
Box 2 – Number of patients placed on kidney transplant waiting list for the first time, by ethnicity and year, 2007–2021*
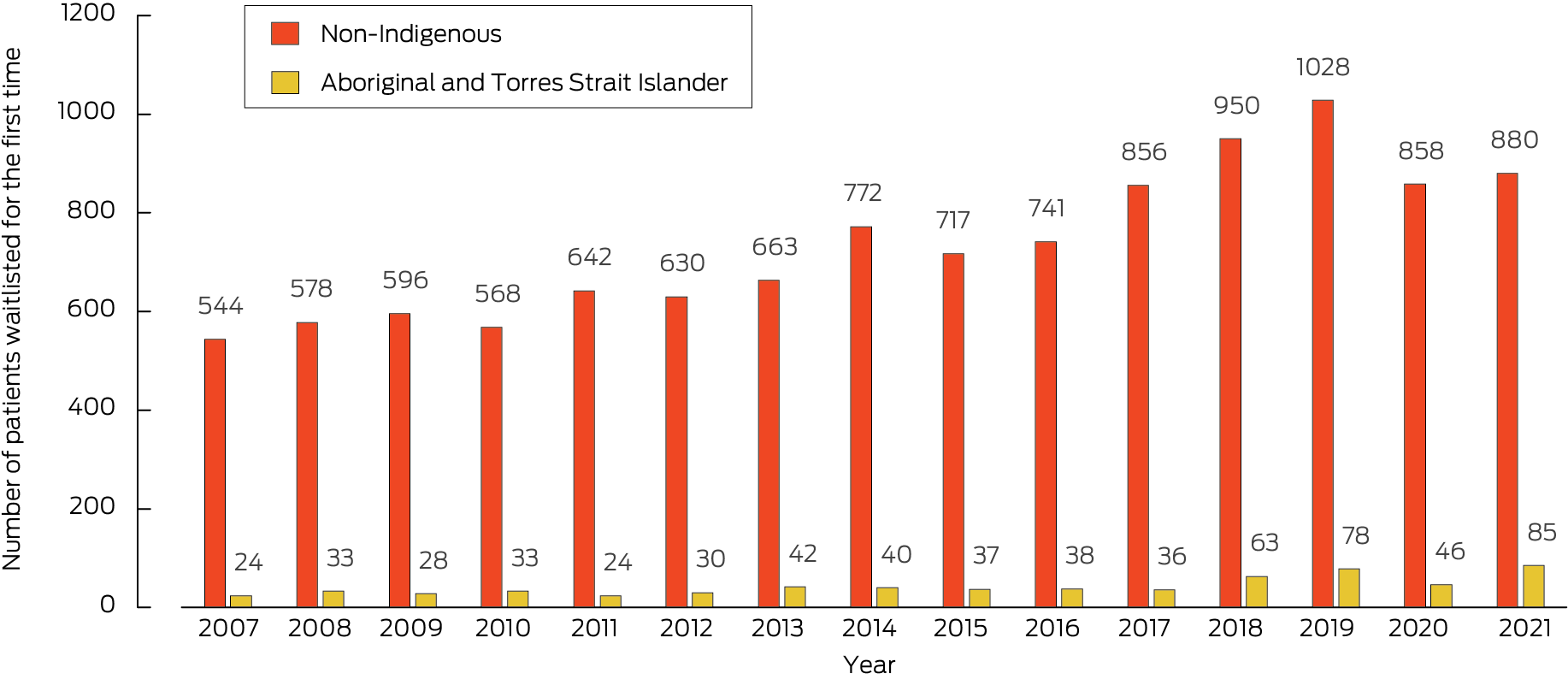
*Analysis based on data supplied by the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA).
Box 3 – Demographic and clinical characteristics of the 2020 cohort of patients receiving dialysis at renal units participating in the National Indigenous Kidney Transplantation Taskforce data collection, who had not previously had a kidney transplant, by ethnicity
|
Factor |
Non‐Indigenous |
Indigenous |
|||||||||||||
|
|
|||||||||||||||
|
Number of people receiving treatment in participating units |
6128 |
1832 |
|||||||||||||
|
Age (years) |
|
|
|||||||||||||
|
0–17 |
10 (< 1%) |
2 (< 1%) |
|||||||||||||
|
18–34 |
259 (4%) |
93 (5%) |
|||||||||||||
|
35–44 |
364 (6%) |
189 (10%) |
|||||||||||||
|
45–54 |
700 (11%) |
515 (28%) |
|||||||||||||
|
55–64 |
1282 (21%) |
611 (33%) |
|||||||||||||
|
65–74 |
1690 (28%) |
353 (19%) |
|||||||||||||
|
75–84 |
1519 (25%) |
64 (3%) |
|||||||||||||
|
≥ 85 |
304 (5%) |
5 (< 1%) |
|||||||||||||
|
Gender |
|
|
|||||||||||||
|
Female |
2214 (36%) |
1073 (59%) |
|||||||||||||
|
Male |
3914 (64%) |
759 (41%) |
|||||||||||||
|
Dialysis modality |
|
|
|||||||||||||
|
Peritoneal dialysis |
1384 (23%) |
129 (7%) |
|||||||||||||
|
Haemodialysis |
4744 (77%) |
1703 (93%) |
|||||||||||||
|
Taskforce targeted status |
|
|
|||||||||||||
|
Targeted unit |
4303 (70%) |
1789 (98%) |
|||||||||||||
|
Non‐targeted unit, participating |
1825 (30%) |
43 (2%) |
|||||||||||||
|
State or territory at end of year |
|
|
|||||||||||||
|
Northern Territory |
70 (1%) |
678 (37%) |
|||||||||||||
|
New South Wales or Australian Capital Territory |
1867 (30%) |
128 (7%) |
|||||||||||||
|
Victoria |
1384 (23%) |
23 (1%) |
|||||||||||||
|
Queensland |
1316 (21%) |
432 (24%) |
|||||||||||||
|
South Australia |
537 (9%) |
106 (6%) |
|||||||||||||
|
Western Australia |
954 (16%) |
465 (25%) |
|||||||||||||
|
Time on dialysis (years) |
|
|
|||||||||||||
|
0 to < 1 |
1457 (24%) |
271 (15%) |
|||||||||||||
|
1 to < 2 |
1119 (18%) |
301 (16%) |
|||||||||||||
|
2 to < 3 |
920 (15%) |
219 (12%) |
|||||||||||||
|
3 to < 4 |
641 (10%) |
209 (11%) |
|||||||||||||
|
4 to < 5 |
480 (8%) |
167 (9%) |
|||||||||||||
|
5 to < 6 |
368 (6%) |
129 (7%) |
|||||||||||||
|
6 to < 7 |
293 (5%) |
119 (6%) |
|||||||||||||
|
≥ 7 |
850 (14%) |
417 (23%) |
|||||||||||||
|
Primary kidney disease category* |
|
|
|||||||||||||
|
Diabetic kidney disease |
2207 (38%) |
1252 (71%) |
|||||||||||||
|
Glomerular disease |
1128 (20%) |
198 (11%) |
|||||||||||||
|
Hypertension |
819 (14%) |
127 (7%) |
|||||||||||||
|
Polycystic disease |
338 (6%) |
7 (< 1%) |
|||||||||||||
|
Other/uncertain |
1273 (22%) |
176 (10%) |
|||||||||||||
|
Diabetes as a comorbidity at end of year* |
|
|
|||||||||||||
|
No |
2749 (47%) |
320 (18%) |
|||||||||||||
|
Yes |
3088 (53%) |
1479 (82%) |
|||||||||||||
|
Waitlisted at end of year |
|
|
|||||||||||||
|
No |
5616 (92%) |
1796 (98%) |
|||||||||||||
|
Yes |
512 (8%) |
36 (2%) |
|||||||||||||
|
|
|||||||||||||||
|
*Data on primary kidney disease category were missing for 87 non‐Indigenous people and 41 Indigenous people, and data for diabetes as a comorbidity were missing for 15 non‐Indigenous people and two Indigenous people. |
|||||||||||||||
Received 3 January 2025, accepted 15 May 2025
- Stephen P McDonald AM1,2
- Katie Cundale3
- Christopher E Davies1,4
- Kelli Karrikarringka Owen (Kaurna, Nharangga, and Ngarrindjeri)3,5
- Kerry Dole6
- Feruza Kholmurodova1
- Matilda D’Antoine (Paakantyi)3
- Jaquelyne T Hughes (Wagadagam)7,8
- 1 Australia and New Zealand Dialysis and Transplant Registry, Adelaide, SA
- 2 Adelaide EpiCentre, Adelaide, SA
- 3 National Indigenous Kidney Transplantation Taskforce, Adelaide, SA
- 4 University of Adelaide, Adelaide, SA
- 5 AKction Reference Group, Adelaide, SA
- 6 Northern Territory Department of Health, Alice Springs, NT
- 7 Flinders University, Darwin, NT
- 8 Royal Darwin Hospital, Darwin, NT
Open access:
Open access publishing facilitated by The University of Adelaide, as part of the Wiley – The University of Adelaide agreement via the Council of Australian University Librarians.
Data Sharing:
ANZDATA has established policies for access to various types of data (including those underlying this manuscript). These policies and associated application procedures are available at https://www.anzdata.org.au/anzdata/data‐requests/request‐procedure.
The National Indigenous Kidney Transplantation Taskforce is funded by a grant from the Australian Government Department of Health and Aged Care (4‐BIA3J8Y) that is held by the Transplantation Society of Australia and New Zealand. The Australia and New Zealand Dialysis and Transplant Registry (ANZDATA) receives funding from the Australian Organ and Tissue Authority to support its core operations. Neither body had a role in study design, data collection, data analysis or interpretation of findings. The authors recognise Indigenous peoples research leadership and their knowledges contained within the following cited references: 1,2,8,11,12,18,19,20,31,32 and 34,35,36.
Jaquelyne Hughes is a Guest Editor for the 2025 NAIDOC Week MJA Special Issue and was not involved in any editorial decision making about this article.
Author contributions:
McDonald SP: Conceptualization; formal analysis; methodology; supervision; writing – original draft; writing – review and editing. Cundale K: Formal analysis; project administration; writing – original draft; writing – review and editing. Davies C: Data curation; formal analysis; visualization; writing – original draft; writing – review and editing. Owen K: Conceptualization; writing – review and editing. Dole K: Conceptualization; supervision; writing – review and editing. Kholmurodova F: Data curation; formal analysis; visualization. D’Antoine M: Project administration; writing – review and editing. Hughes JT: Conceptualization; methodology; supervision; writing – original draft; writing – review and editing. All authors have reviewed and approved the final manuscript and agree to be accountable for their contributions.
- 1. Bateman S, Solomon B, Davies C, et al. Chapter 10: Kidney failure in Aboriginal and Torres Strait Islander Australians. In: Australia and New Zealand Dialysis and Transplant Registry 46th annual report. Adelaide: ANZDATA, 2023. https://www.anzdata.org.au/wp‐content/uploads/2023/09/ANZDATA_AR‐2022‐23_Chapter‐10_F2.pdf (viewed Sept 2024).
- 2. Bateman S, Owen K, Lester R, et al. The survival benefit of deceased donor kidney transplantation for Aboriginal and Torres Strait Islander people, 2006–20: a retrospective national cohort study. Med J Aust 2024; 221: 111‐116. https://www.mja.com.au/journal/2024/221/2/survival‐benefit‐deceased‐donor‐kidney‐transplantation‐aboriginal‐and‐torres
- 3. Wyld ML, Wyburn KR, Chadban SJ. Global perspective on kidney transplantation: Australia. Kidney360 2021; 2: 1641‐1644.
- 4. Transplantation Society of Australia and New Zealand. Clinical guidelines for organ transplantation from deceased donors, version 1.1. Canberra: TSANZ, 2017.
- 5. Khanal N, Lawton PD, Cass A, McDonald SP. Disparity of access to kidney transplantation by Indigenous and non‐Indigenous Australians. Med J Aust 2018; 209: 261‐266. https://www.mja.com.au/journal/2018/209/6/disparity‐access‐kidney‐transplantation‐indigenous‐and‐non‐indigenous
- 6. Goodman D, Atkinson A. Self empowerment of Indigenous Australians with renal failure to ask their doctors “Am I on the kidney transplant waiting list?” [abstract]. Australian and New Zealand Society of Nephrology Annual Scientific Meeting; Sydney (hybrid), 17–19 Oct 2022. https://anzsnevents.com/15664 (viewed Sept 2024).
- 7. Vanholder R, Annemans L, Braks M, et al. Inequities in kidney health and kidney care. Nat Rev Nephrol 2023; 19: 694‐708.
- 8. Hughes JT, Dembski L, Kerrigan V, et al. Gathering perspectives—finding solutions for chronic and end‐stage kidney disease: Indigenous patient voices. Nephrology (Carlton) 2021; 26: 215‐223.
- 9. Tiong MK, Thomas S, Fernandes DK, Cherian S. Examining barriers to timely waitlisting for kidney transplantation for Indigenous Australians in Central Australia. Intern Med J 2022; 52: 288‐294.
- 10. Garrard E, McDonald SP. Improving access to and outcomes of kidney transplantation for Aboriginal and Torres Strait Islander people in Australia: performance report. Sydney: Transplantation Society of Australia and New Zealand, 2019. https://tsanz.com.au/storage/NIKTT/TSANZ‐Performance‐Report‐‐‐Improving‐Indigenous‐Transplant‐Outcomes‐Final‐edited‐1.pdf (viewed Sept 2024).
- 11. Cundale K, Hughes JT, Owen K, McDonald SP. Final report: National Indigenous Kidney Transplantation Taskforce. Adelaide: NIKTT, 2023. https://www.niktt.com.au/finalreport (viewed Sept 2024).
- 12. Lee D, Davies C, Au E, et al. Chapter 6: Australian transplant waiting list. In: Australia and New Zealand Dialysis and Transplant Registry 47th annual report. Adelaide: ANZDATA, 2024. https://www.anzdata.org.au/wp‐content/uploads/2024/12/06_waiting_list_2023_ar_2024_chapter_F_20241224.pdf (viewed Nov 2024).
- 13. Von Elm E Altman D, Egger M, et al. STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453‐1457.
- 14. Australia and New Zealand Dialysis and Transplant Registry. Data collection. Adelaide: ANZDATA, 2023. https://www.anzdata.org.au/anzdata/services/data‐management/data‐collection (viewed Sept 2024).
- 15. Australia and New Zealand Dialysis and Transplant Registry. Transplant Assessment Stage [form TA]. Adelaide: ANZDATA, 2019. https://www.anzdata.org.au/wp‐content/uploads/2020/01/TxAssessmentStage_TA.pdf (viewed Sept 2024).
- 16. Huria T, Palmer SC, Pitama S, et al. Consolidated criteria for strengthening the reporting of health research involving Indigenous peoples: the CONSIDER statement. BMC Med Res Methodol 2019; 19: 173.
- 17. Australia and New Zealand Dialysis and Transplant Registry. Data requests relating to patient ethnicity. Adelaide: ANZDATA, 2021. https://www.anzdata.org.au/wp‐content/uploads/2021/12/ANZDATA_update_on_data_requests_related_to_patient_ethnicity.pdf (viewed Sept 2024).
- 18. Bateman S, Riceman M, Owen K, et al. Models of care to address disparities in kidney health outcomes for First Nations people. Kidney Int 2023; 104: 681‐689.
- 19. Hughes J, Kirkham R, Min OA, et al. Patient‐identified health service transformation: an Aboriginal patient's experience with extensive chronic tinea corporis and delayed kidney transplantation wait‐listing. Ren Soc Australas J 2019; 15: 92‐96.
- 20. Naidu P, Paolucci O, Luta R, Hughes JT. Optimisation during transition to dialysis commencement. Med J Aust 2024; 221: 18‐24. https://www.mja.com.au/journal/2024/221/1/optimisation‐during‐transition‐dialysis‐commencement
- 21. Mehrabi A, Fonouni H, Wente M, et al. Wound complications following kidney and liver transplantation. Clin Transplant 2006; 20: 97‐110.
- 22. Nicoletto BB, Fonseca NKO, Manfro RC, et al. Effects of obesity on kidney transplantation outcomes: a systematic review and meta‐analysis. Transplantation 2014; 98: 167‐176.
- 23. Hill CJ, Courtney AE, Cardwell CR, et al. Recipient obesity and outcomes after kidney transplantation: a systematic review and meta‐analysis. Nephrol Dial Transplant 2015; 30: 1403‐1411.
- 24. Sood A, Hakim DN, Hakim NS. Consequences of recipient obesity on postoperative outcomes in a renal transplant: a systematic review and meta‐analysis. Exp Clin Transplant 2016; 14: 121‐128.
- 25. Lafranca JA, IJzermans JNM, Betjes MG, et al. Body mass index and outcome in renal transplant recipients: a systematic review and meta‐analysis. BMC Med 2015; 13: 111.
- 26. Gioco R, Sanfilippo C, Veroux P, et al. Abdominal wall complications after kidney transplantation: a clinical review. Clin Transplant 2021; 35: e14506.
- 27. Boan P, Swaminathan R, Irish A. Infectious complications in Indigenous renal transplant recipients in Western Australia. Intern Med J 2017; 47: 648‐655.
- 28. Power T, East L, Gao Y, et al. A mixed‐methods evaluation of an urban Aboriginal diabetes lifestyle program. Aust N Z J Public Health 2021; 45: 143‐149.
- 29. Grunseit AC, Bohn‐Goldbaum E, Crane M, et al. Participant profile and impacts of an Aboriginal healthy lifestyle and weight loss challenge over four years 2012–2015. Aust N Z J Public Health 2019; 43: 328‐333.
- 30. Sushames A, Engelberg T, Gebel K. Perceived barriers and enablers to participation in a community‐tailored physical activity program with Indigenous Australians in a regional and rural setting: a qualitative study. Int J Equity Health 2017; 16: 172.
- 31. Chaturvedi S, Ullah S, Hughes JT. Kidney transplantation access and outcomes for Aboriginal and Torres Strait Islander children and young adults, 1963–2020: an ANZDATA registry study. Med J Aust 2024; 221: 47‐54. https://www.mja.com.au/journal/2024/221/1/kidney‐transplantation‐access‐and‐outcomes‐aboriginal‐and‐torres‐strait‐islander
- 32. Saunders P. Fulfilling cultural safety expectations in specialist medical education and training: considerations for colleges to advance recognition and quality. Med J Aust 2024; 221: 8‐12. https://www.mja.com.au/journal/2024/221/1/fulfilling‐cultural‐safety‐expectations‐specialist‐medical‐education‐and
- 33. Medical Board of Australia. Cultural safety education requirements for specialist registration. Melbourne: Australian Health Practitioner Regulation Agency, 2024. https://www.medicalboard.gov.au/Registration/Types/Specialist‐Registration/Cultural‐safety‐education‐requirements.aspx (viewed Apr 2025).
- 34. Hughes JT, Cundale K, Webster A, et al. Towards equity in kidney transplantation: the next steps. Med J Aust 2023; 219(8 Suppl): S19‐S22. https://www.mja.com.au/journal/2023/219/8/towards‐equity‐kidney‐transplantation‐next‐steps
- 35. Ryder C, Hossain S, Howard L, et al. Indigenous governance, ethics, and data collection in Australian clinical registries. Med J Aust 2024; 221: 156‐161. https://www.mja.com.au/journal/2024/221/3/indigenous‐governance‐ethics‐and‐data‐collection‐australian‐clinical‐registries
- 36. Tunnicliffe DJ, Bateman S, Arnold‐Chamney M, et al. Recommendations for culturally safe clinical kidney care for First Nations Australians: a guideline summary. Med J Aust 2023; 219: 374‐385. https://www.mja.com.au/journal/2023/219/8/recommendations‐culturally‐safe‐clinical‐kidney‐care‐first‐nations‐australians
- 37. Australian Health Practitioner Regulation Agency. National Law amendments. Melbourne: AHPRA, 2024. https://www.ahpra.gov.au/About‐Ahpra/Ministerial‐Directives‐and‐Communiques/National‐Law‐amendments (viewed Dec 2024).






Abstract
Objectives: To describe clinician‐reported reasons for non‐waitlisting of patients with kidney failure for deceased donor kidney transplantation, and to examine disparities affecting Aboriginal and Torres Strait Islander people.
Design: Retrospective cross‐sectional analysis of data from a national clinical quality registry.
Participants and setting: Patients receiving dialysis in 26 Australian renal units as of 31 December 2020.
Main outcome measures: Rates of active waitlisting for kidney transplantation and clinician‐reported reasons for non‐waitlisting.
Results: Thirty‐six of 1832 Aboriginal and Torres Strait Islander people (2.0%) were actively waitlisted, compared with 512 of 6128 non‐Indigenous people (8.4%). For Aboriginal and Torres Strait Islander patients aged < 65 years, 457 of 1204 (38%) were not waitlisted due to a permanent contraindication, 276 (23%) due to a temporary contraindication, and 232 (19%) due to incomplete work‐up. Among those with a contraindication, cardiovascular disease was reported as the reason for about a quarter of people in both groups. Obesity was cited for 163 Aboriginal and Torres Strait Islander patients aged < 65 years (22%) and 30 Aboriginal and Torres Strait Islander patients aged ≥ 65 years (10%); in the non‐Indigenous group, obesity was cited for 207 (26%) and 163 (9%) patients aged < 65 years and ≥ 65 years, respectively. Cancer was reported for 28 Aboriginal and Torres Strait Islander patients aged < 65 years (4%) and 86 non‐Indigenous patients aged < 65 years (11%). Other reasons for non‐waitlisting, reported as free text, included patient safety, smoking, age and mental health.
Conclusions: Aboriginal and Torres Strait Islander people experience inequities in waitlisting for kidney transplantation across multiple stages of a complex process. Addressing these barriers requires system‐level reform and accountability to improve equity in transplantation access.