Clinical record
A 53‐year‐old Indigenous male farmer presented with several weeks of fluctuating lumbar back pain while physically supporting an older family member. The pain worsened despite expectant management by his general practitioner, and four months later he had an acute exacerbation after jumping off a utility truck. The pain was intense, constant, kept him awake, and was associated with left thigh paraesthesia. He reported intermittent night sweats but no fever, weight loss or incontinence. His past medical history included human leukocyte antigen B27 (HLA‐B27)‐associated chronic uveitis and hypertension. There was no history of immunocompromising conditions, medications or substance use. Differential diagnoses included fracture or degenerative spondyloarthropathy (given the trauma), malignancy or infection (given the night sweats), or ankylosing spondylitis.
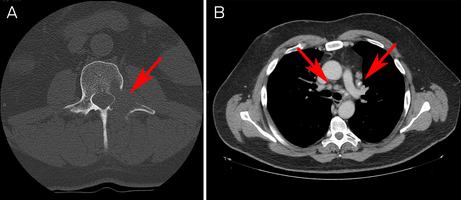
A computed tomography scan revealed a lytic lesion in the left L2 pedicle, mediastinal and hilar lymphadenopathy, and scattered pulmonary nodules concerning for malignancy (Box 1). There were also ground glass and tree‐in‐bud opacities in the right lower lobe suggesting inflammatory change.
A bone biopsy was sent for histopathology only. This unexpectedly revealed no evidence of malignancy, but instead, florid histiocytic and multinucleate giant cell inflammation with numerous round organisms with prominent, thick capsules and narrow‐necked budding (Box 2). They were pale blue on haematoxylin and eosin staining and labelled strongly with periodic acid–Schiff and methenamine silver staining. Thickened capsules were highlighted by mucicarmine staining. The morphology was most consistent with Cryptococcus species. Fungal polymerase chain reaction (PCR) was not performed on formalin‐fixed tissue.
Serum cryptococcal antigen via lateral flow assay was 1:256. Myco/F lytic blood cultures were negative. Magnetic resonance imaging did not demonstrate any evidence of cerebral cryptococcosis. Lumbar puncture had normal opening pressure, biochemistry and cell count with an indeterminate cryptococcal antigen titre (1:2). Human immunodeficiency virus (HIV) and human T‐lymphotropic virus type 1 and type 2 (HTLV‐1/2) serology, interferon‐γ release assay, viral hepatitis screens, and T cell subsets were unremarkable.
Ophthalmological review indicated stable, chronic uveitis unrelated to his presentation. There were no respiratory symptoms, but pulmonary cryptococcosis was unable to be excluded on imaging.
Further history revealed significant exposure to pigeon faeces. The patient's tractor was stored in a shed filled with dried pigeon excrement and the exhaust blew it into the air. He did not wear a mask.
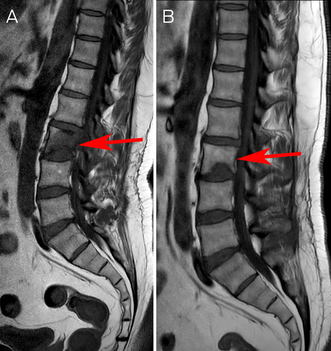
Cryptococcal vertebral osteomyelitis was diagnosed based on characteristic histology and positive serology. Biopsy for culture was not re‐attempted due to patient preference. Liposomal amphotericin B and 5‐fluorocytosine four‐week induction was commenced. His back pain improved, and he was changed to fluconazole consolidation and then maintenance therapy. Currently, he has completed 13 of 18 planned months of therapy with radiological improvement of the osteomyelitis (Box 3). The right lower lobe opacities have resolved; the pulmonary nodules and lymphadenopathy are unchanged.
Discussion
Cryptococcosis is an opportunistic fungal infection, usually affecting immunocompromised hosts. Disease is primarily caused by Cryptococcus neoformans complex or Cryptococcus gattii complex.1 The former is more common and ubiquitous in the environment, particularly in soil and avian excreta; the latter is found in eucalyptus trees.1 Inhalation of avian excreta can be avoided through work safety practices.2 The incidence of cryptococcosis has increased due to the rise in HIV infections, organ transplants, malignancies and their therapies.1 Australian epidemiology is only available from local studies. For example, the incidence of cryptococcosis in Cairns in 2019 was 14.3 cases per 1 million population. The infection was associated with Indigeneity and rural residence.3
The pathogenesis involves inhalation of basidiospores or yeast cells that deposit in alveoli. A type 1 T‐helper cell reaction results in granuloma formation or, if defective, leads to disseminated disease.1
Cryptococcosis most commonly presents with subacute meningitis and raised intracranial pressure, or pulmonary disease ranging from asymptomatic nodules to rapidly progressive pneumonia. It can also affect the skin, eyes, prostate, peritoneum, gastrointestinal tract, and bone.1
Although skeletal disease occurs in less than 10% of patients with disseminated disease,4 it is notable that the first human isolate of Cryptococcus was from a woman with tibial osteomyelitis in 1894.1 Skeletal cryptococcosis usually affects the vertebrae and long bones, but it is uncommon in immunocompetent hosts.4 Since 1979, only five cases of primary vertebral osteomyelitis have been described in immunocompetent hosts.5,6,7
Low back pain is common and Australia's Low Back Pain Clinical Care Standard emphasises management with education and physical activity.8,9 In this case, however, the “red flags” (recalcitrant symptoms, trauma and night sweats) necessitated further investigation.
Cryptococcosis is diagnosed on history, examination, chest imaging and lumbar puncture with cryptococcal antigen testing or culture.1,10 Cryptococcus can be identified using India ink microscopy with high specificity, but sensitivity is user‐dependent.1 Histologically, methenamine silver identifies the spherical shape with narrow‐based budding. Mucicarmine highlights the polysaccharide capsule.1 Cryptococcal antigen can be detected in serum or cerebrospinal fluid via latex agglutination or, more commonly, lateral flow assay.1 Culture is considered the gold standard.1
There is a paucity of treatment data for cryptococcal osteomyelitis. The Infectious Diseases Society of America recommends treating as meningitis with amphotericin B and 5‐fluorocytosine for two to four weeks (induction), followed by high dose fluconazole for up to eight weeks (consolidation), then a maintenance dose for six to 12 months,4 or up to 18 months per the Australian Therapeutic Guidelines.11
In summary, cryptococcosis presents variably. In patients with back pain and lytic lesions, especially if immunocompromised or exposed to avian excreta, cryptococcosis should be considered. In these cases, microbiological assessment may yield a different diagnosis to what was initially expected.
Lessons from practice
- In patients with skeletal lytic lesions of unclear aetiology, biopsies should be taken for culture as well as histopathology to ensure occult infections are not missed.
- It is important to maintain a suspicion for occult infections (such as cryptococcosis) for common clinical presentations such as back pain, especially if recalcitrant in nature.
- Reducing exposure to bird droppings in the workplace includes the use of personal protective equipment, personal hygiene and the regular removal of bird droppings.
- According to the new Australian Low Back Pain Clinical Care Standard, imaging is indicated if there are signs or symptoms suggestive of a serious or specific pathology.
Box 1 – (A) Axial section computed tomography (CT) scan of lytic lesion in left L2 pedicle. (B) Axial section CT chest scan showing mediastinal lymphadenopathy
Box 2 – (A) Mucicarmine stain (to highlight thickened capsules). (B) Periodic acid–Schiff stain*
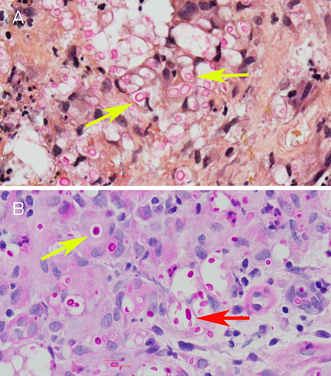
* Yellow arrows: yeast‐like forms. Red arrow: narrow‐necked budding.
Box 3 – (A) Sagittal section T1‐weighted turbo‐spin‐echo (TSE) magnetic resonance imaging (MRI) scan showing L2 osteomyelitis and discitis two months after treatment commencement (June 2022). (B) Sagittal section T1‐weighted TSE MRI scan showing radiological improvement after nine months of treatment (January 2023)
Provenance: Not commissioned; externally peer reviewed.
- 1. Gushiken AC, Saharia KK, Baddley JW. Cryptococcosis. Infect Clin North Am 2021; 35: 493‐514.
- 2. Queensland Government. Work with bird and bat droppings [website]. Brisbane: WorkSafe, Workplace Health and Safety Queensland; 2020. https://www.worksafe.qld.gov.au/safety‐and‐prevention/hazards/hazardous‐exposures/biological‐hazards/diseases‐from‐animals/work‐with‐bird‐and‐bat‐droppings (viewed May 2023).
- 3. Sim BZ, Conway L, Smith LK, et al. The aetiology and clinical characteristics of cryptococcal infections in Far North Queensland, tropical Australia. PLoS One 2022; 17: e0265739.
- 4. Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 2010; 50: 291‐322.
- 5. Al‐Tawfiq JA, Ghandour J. Cryptococcus neoformans abscess and osteomyelitis in an immunocompetent patient with tuberculous lymphadenitis. Infection 2007; 35: 377‐382.
- 6. Li Z, Liang J, Shen J, et al. Thoracolumbar scoliosis due to cryptococcal osteomyelitis: a case report and review of the literature. Medicine (Baltimore) 2016; 95: e2613.
- 7. Zhong Y, Huang Y, Zhang D, et al. Isolated cryptococcal osteomyelitis of the sacrum in an immunocompetent patient: a case report and literature review. BMC Infect Dis 2023; 23: 116.
- 8. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators; Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1545‐1602.
- 9. Maher CG, Archambeau A, Buchbinder R, et al. Introducing Australia's clinical care standard for low back pain. Med J Aust 2023; 218: 354‐356. https://www.mja.com.au/journal/2023/218/8/introducing‐australias‐clinical‐care‐standard‐low‐back‐pain
- 10. Chang CC, Hall V, Cooper C, et al. Consensus guidelines for the diagnosis and management of cryptococcosis and rare yeast infections in the haematology/oncology setting, 2021. Intern Med J 2021; 51: 118‐142.
- 11. Therapeutic Guidelines. Cryptococcal meningitis [website]. Melbourne: Therapeutic Guidelines Limited; 2019. https://www‐tg‐org‐au.salus.idm.oclc.org (viewed May 2023).






Open access:
Open access publishing facilitated by The University of Adelaide, as part of the Wiley ‐ The University of Adelaide agreement via the Council of Australian University Librarians.
Patient consent:
The patient gave written consent for publication.
No relevant disclosures.