The known: The mental health and wellbeing of health and aged care workers in Australia during the second and third years of the COVID‐19 pandemic have not been assessed longitudinally.
The new: Increased burnout and reduced optimism, wellbeing, and resilience were more frequently reported by Victorian health and aged care workers during late 2021 and mid‐2022 than in mid‐2021, and the proportion considering leaving their profession increased from 32% to 54%. In contrast, self‐reported measures of depression, anxiety, and post‐traumatic stress were higher in late 2021 than mid‐2021, but had again declined by mid‐2022.
The implications: Continuing support for health care workers is required to alleviate the ongoing mental health and wellbeing effects of the COVID‐19 pandemic.
The coronavirus disease 2019 (COVID‐19) pandemic has imposed considerable physical and psychological demands on health care workers (including aged care workers) over a long period.1,2 Despite the easing of public health restrictions, facilitated by high vaccination rates, the burden on the health care system and health care workers remains substantial.
Few studies have explored the longitudinal impact of COVID‐19 on the mental health of health care workers.3 Sustained psychological stress affects lifestyle (eg, alcohol consumption),4 workforce retention, and ultimately the quality of patient care.5 A recent survey found that 29% of primary health care nurses planned to leave their positions within two to five years,6 consistent with other reports on the impact of the pandemic on the nursing workforce.7
Analyses of longitudinal data on the mental health and wellbeing of health care workers can help guide workplace risk reduction strategies and policies. In this article, we report findings from the Coronavirus in Victorian Healthcare and Aged Care Workers (COVIC‐HA) Cohort study. We compared quantitative mental health and wellbeing data collected in three surveys over twelve months to examine changes over time, both overall and by occupation group.
Methods
The COVIC‐HA Cohort Study (retrospectively registered with the Australian New Zealand Clinical Trials Registry as an observational study: ACTRN12621000533897; 6 May 2021) employs a mixed methods longitudinal approach to examine the physical and psychosocial wellbeing of Victorian health care workers during the COVID‐19 pandemic and to assess organisational responses to the pandemic. Quantitative data were collected in three REDCap8 surveys — May–July 2021 (survey 1), October–December 2021 (survey 2), and May–June 2022 (survey 3) — with each survey open for six to eight weeks. The participating study sites, recruitment, data collection methods, and eligibility criteria have been described elsewhere, as have the baseline survey data.9 In brief, participating sites were recruited from the Monash Partners and related clinical networks, and were primarily located in southeast Melbourne. Senior personnel from each site sent all employees an email including an explanatory statement and survey link. All adult employees working at a participating study site were considered eligible. Our report conforms with the Strengthening the reporting of observational studies in epidemiology (STROBE) guidelines.10
In the open recruitment study design, survey invitations were circulated (by email) by the participating study sites for each survey, enabling new participants to join over time. After completing each survey, participants were asked to opt in to receiving email invitations to subsequent surveys.
Data collection
The surveys (Supporting Information 1) included questions about primary mental health outcomes during the two weeks preceding completion of the survey: symptoms of depression (Patient Health Questionnaire‐9, PHQ‐9), anxiety (Generalized Anxiety Disorder scale, GAD‐7), post‐traumatic stress (Impact of Event Scale‐6, IES‐6), burnout (abbreviated Maslach Burnout Inventory, aMBI), quality of life (Personal Wellbeing Index–Adult, PWI‐A), resilience (Connor–Davidson Resilience Scale 2, CD‐RISC‐2), and optimism about the future (10‐point visual analogue scale) (Supporting Information 2, table 1). The survey also included questions about COVID‐19 exposure, alcohol consumption, mental health support seeking, COVID‐19‐related effects on work and personal life, and concerns about contracting, transmitting, and serious consequences of COVID‐19, each based on experiences since the beginning of the pandemic (survey 1) or during the preceding six months (surveys 2 and 3). The analysis of responses to two free response survey questions, not discussed in this article, have been reported elsewhere.9,11
Data analysis
Respondent characteristics are summarised as means and standard deviations (SDs) or counts and proportions. Missing data were imputed by multiple imputation using chained equations. Data were deemed missing for a question if the response was “not applicable” or similar, and for all items of a survey not completed by a participant who completed at least one other survey.
We compared primary mental health outcomes across the three surveys and between survey pairs, separately for all respondents and by occupation group, in longitudinal mixed effect models that included fixed effects for time (ie, survey; three‐level categorical variable), occupation group (five categories), and an interaction between time and occupation group. The models included the demographic variables age, gender, and linear and squared terms for residential postcode socio‐economic status decile (Index of Relative Socio‐economic Advantage and Disadvantage, IRSAD12). To account for clustering within worksites and repeated responses by individuals, all models included random effects for respondent and worksite (four hospital clusters and one cluster each for ambulance, general practices, and aged care), and an interaction between time and worksite (cluster‐by‐time random effect); given the small total number of clusters, Kenward–Roger small sample correction of standard errors and degrees of freedom was applied.13
Continuous outcomes were modelled in linear mixed models and results reported as adjusted mean outcomes and adjusted mean differences. Binary outcomes were modelled in generalised linear mixed models with a logit link function and results are reported as adjusted proportions and adjusted odds ratios (for moderate to severe symptoms, except for PHQ‐9 item 9 and GAD‐7 item 6 [“on at least some days” modelled] and optimism [“high optimism” modelled]).
As sensitivity analyses, we also undertook complete case analyses; that is, without imputing missing data.
Summary statistics and plots were prepared in R 4.1.2 (R Foundation for Statistical Computing) using the packages dplyr 1.0.7 (https://cran.r‐project.org/web/packages/dplyr/index.html) and ggplot2 3.3.5 (https://cran.r‐project.org/web/packages/ggplot2/index.html). Longitudinal analyses were conducted in SAS 9.4 using the PROC MIXED and PROC GLIMMIX commands, and the LSMEANS subcommand for adjusted means and proportions. Multiple imputation used the Stata 17 mi impute chained command (further details: Supporting Information 2, statistical analysis).
Ethics approval
The study was approved by the Victorian Streamlined Ethical Review Process (project number 68086).
Results
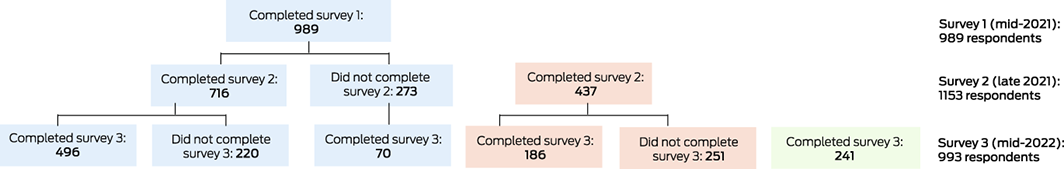
Study invitations were sent to all employees of participating organisations, about 50 000 health care workers according to employee data provided by the organisations at study commencement. We received 989 responses to survey 1, 1153 to survey 2, and 993 to survey 3 (1667 unique respondents; approximate response rate, 3.3%); 496 people completed all three surveys (50.2% of survey 1 respondents) (Box 1). The demographic characteristics of respondents were similar for the three surveys. A total of 1211 of the 1667 participants were women (72.6%), 890 were people under 45 years of age (53.4%); the corresponding reported proportions for the participating organisations were 62% and 63%. In survey 1, 22 respondents reported having had COVID‐19 (2.2%), 19 in survey 2 (1.6%), and 369 in survey 3 (37.2%) (Box 2). By setting, 1289 participants worked in hospitals (77.3%), 315 were ambulance staff (18.9%), 16 were aged care workers (1.0%), and 47 were primary care workers (2.8%).
Mental health and wellbeing
The adjusted proportions of participants who reported moderate to severe symptoms of depression (survey 1, 16.4%; survey 2, 22.6%; survey 3, 19.2%), anxiety (survey 1, 8.8%; survey 2, 16.0%; survey 3, 11.0%), or post‐traumatic stress (survey 1, 14.6%; survey 2, 35.1%; survey 3, 14.9%) were each larger in survey 2 than in survey 1, and smaller in survey 3 than survey 2 (decline for depression not statistically significant). The adjusted proportions of respondents who reported being irritable on at least some days (GAD‐7 item 6) was higher in survey 2 than in survey 1, and the proportion who reported thoughts of being better off dead or of hurting themselves on at least some days (PHQ‐9 item 9) was higher in surveys 2 and 3 than in survey 1 (Box 3).
The adjusted proportions of participants who reported moderate to severe symptoms in all three burnout domains (emotional exhaustion, depersonalisation, personal accomplishment) were higher in surveys 2 and 3 than in survey 1 (emotional exhaustion: survey 3 v survey 1 not statistically significant). Correspondingly, the adjusted proportion who reported high optimism was smaller in surveys 2 and 3 than in survey 1 (Box 4).
Adjusted mean scores for resilience, wellbeing, and life satisfaction (PWI‐A item 1) were similar in surveys 2 and 3 and lower than in survey 1 (resilience: survey 2 v survey 1 not statistically significant) (Box 5).
The patterns by survey for each psychological measure were similar but differed in magnitude by occupation group. Adjusted mean scores for wellbeing and life satisfaction were generally higher for doctors than other respondent occupation groups, and a smaller proportion of doctors reported moderate to severe depression than respondents from other occupation groups (Supporting Information 2, figures 1–5).
Psychosocial impact, workplace support, and personal COVID‐19 risk
The unadjusted proportion of respondents who reported considering leaving their profession at any stage of the pandemic was 32.2% in survey 1, 42.5% in survey 2, and 54.0% in survey 3 (Box 6). The proportion who reported having sought mental health support was similar in all three surveys (about 36%). The proportions of respondents concerned about contracting or transmitting COVID‐19, serious symptoms, increased social isolation, or the impact of COVID‐19‐related restrictions, or who reported increased alcohol consumption were larger in survey 2 than in surveys 1 and 3. About 90% of respondents in each survey reported feeling informed by their organisation about workplace changes. However, the proportions who felt their organisation cared about staff welfare, were comfortable with raising concerns within their organisation, or were satisfied with their organisations’ responses to concerns were smaller in survey 3 than surveys 1 or 2 (Box 6).
Complete case analyses
Complete case analyses yielded results similar to those of the major analyses (Supporting Information 2, tables 8–11).
Discussion
In three surveys of Victorian health care workers during the COVID‐19 pandemic, the prevalence of burnout was higher during late 2021 and mid‐2022 than in mid‐2021; in the third survey, 54% of survey respondents reported considering leaving their profession. Similarly, reported measures of wellbeing, optimism, and resilience were lower in late 2021 and mid‐2022 than in mid‐2021. In contrast, the proportions of respondents with moderate to severe symptoms of depression, anxiety, or post‐traumatic stress were highest, both overall and by occupation group, in late 2021, just before major increases in the numbers of COVID‐19 infections and hospitalisations (Supporting Information 2, figure 6), but by mid‐2022 the proportions were similar to those of mid‐2021.
Most overseas longitudinal studies of the mental health of health care workers during the COVID‐19 pandemic have focused on the period from 2020 to early 2021.1,14,15 Our findings suggest an ongoing impact on health care workers in Victoria during the second and third years of the pandemic.
Several aggressive interventions were imposed during 2020 and 2021 to suppress community transmission of COVID‐19 in Australia, including curfews and prolonged lockdowns. As the national strategy shifted in late 2021 and 2022 to promoting economic recovery and limiting the number of people with severe disease and the burden on health care services, restrictions were not reinstated, despite subsequent surges in infection numbers.16 The differences between changes in measures of burnout, wellbeing, resilience, and optimism and those of depression, anxiety, and post‐traumatic stress suggest that they were differently affected by the pandemic, community restrictions, and work‐related stressors, and should consequently be assessed separately when attempting to understand changes to mental health and wellbeing.
The negative changes in all psychological measures during mid‐ and late 2021 are consistent with local and overseas reports of relationships between mental health effects and periods of peak hospital and intensive care unit admissions.17,18 The decline between late 2021 and mid‐2022 in the proportions of respondents with moderate to severe symptoms of depression, anxiety, and post‐traumatic stress, despite high numbers of COVID‐19 cases, hospitalisations, and deaths, may reflect responses to the easing of public health measures; stringent restrictions have been linked with poorer mental health in the general community in Australia.19,20 In contrast, some health care‐specific policies, such as the coordinated Pandemic Code Brown in Victorian hospitals (an emergency management structure including the possibility of cancelled leave)21 and visitor face‐to‐face restriction orders may have exacerbated wellbeing problems and burnout in health care workers. However, the overall mental health and wellbeing of health care workers is influenced by many factors, including pandemic persistence, declining levels of concern about COVID‐19, the effects of recurrent lockdowns and restrictions, and work‐related stress. The psychological changes we report probably reflect these and other factors, but defining their separate effects was beyond the scope of our study.
The patterns of rise and fall in mental health and wellbeing measures were similar for respondents from each occupation group (Supporting Information 2, figures 1–5), despite initial differences in the prevalence of psychological symptoms9 and in the magnitude of the changes. Including data on pre‐pandemic mental health factors, to establish a pre‐pandemic baseline, would have been ideal and would have helped us assess the contribution of healthy worker biases.22 Further, assessing the same psychological characteristics in people working outside health care would have facilitated more secure assessment of the contribution of health care‐related work to the changes. Overseas studies have reported that psychological distress increased to a greater degree among health care workers than other people during the pandemic.14,15As local comparative data are limited, we could not determine whether similar changes in psychological status affected other workers in Victoria. However, the proportion of respondents reporting thoughts of being better off dead or harming themselves (9.1% in mid‐2022) was smaller than estimated for the general Victorian population in 2020 (9.3% in April–May and 14.7% in July–August),19 suggesting that the psychological impact of the pandemic may not be restricted to health care workers.
Our findings are consistent with previous reports that health care workers experience significant psychological distress during and immediately after outbreaks of new infectious diseases.23,24,25 Together with our qualitative investigation of organisational responses to COVID‐19,11 they indicate that health and aged care organisations should maintain strong leadership and communication systems in the workplace, provide mental health and wellbeing support for staff, and respond efficiently to evolving pandemic challenges. This may require specific funding and policies that facilitate systemic changes for supporting health care worker wellbeing.
Limitations
First, we did not have pre‐pandemic (baseline) data on the mental health of health care workers in Australia. Second, only 50% of people who completed the first survey completed all three surveys.
Third, as survey invitations were emailed, participants who provided work‐affiliated addresses (55% of survey 1 respondents) may have been lost to follow‐up if they left health care during the course of the study. Fourth, we could recruit only small numbers of participants from primary and aged care, precluding meaningful cross‐setting analyses. Fifth, psychological health assessment was self‐reported; no diagnostic or clinical interviews were performed. Finally, our study was subject to convenience sampling, voluntary participation, and low response rates. It cannot be assumed that respondents were representative of all health care workers or their occupation groups; it is probable that people particularly affected by the pandemic were more likely to complete our survey. Only 3.3% of eligible health care workers responded to at least one survey; further, the proportions of women and people over 45 years of age were larger than those among the wider group of all employees in their source organisations. Although our statistical models were adjusted for age, gender, and socio‐economic status, the effects of residual selection and response biases are unknown. As most respondents worked in the south‐eastern suburbs of Melbourne, the generalisability of our findings to all health care workers in Australia is uncertain. We attempted to adjust for missing responses for the psychological measures at each survey (proportion, 30–50%) by using an extensive multiple imputation modelling procedure that assumed we included all factors predictive of responses being missing.
Conclusion
Our longitudinal, 12‐month survey study assessed changes in the mental health of Victorian health care workers during a period of the COVID‐19 pandemic characterised by fluctuations in social restrictions, attitudes to COVID‐19, and disease incidence. We found that measures of burnout, optimism, wellbeing, and resilience were poorer in late 2021 and mid‐2022 than in mid‐2021, but that measures of depression, anxiety, and post‐traumatic stress had improved between late 2021 and mid‐2022. Our findings suggest that ongoing monitoring of the mental health and wellbeing of Australian health care workers is warranted, as they continue to be affected by COVID‐19, particularly in terms of burnout. Our findings also indicate that greater support for sector‐wide mental health and wellbeing support programs for health care workers is required.
Box 2 – Characteristics of the respondents to the three Coronavirus in Victorian Healthcare and Aged Care Workers (COVIC‐HA) Cohort study surveys, by survey*
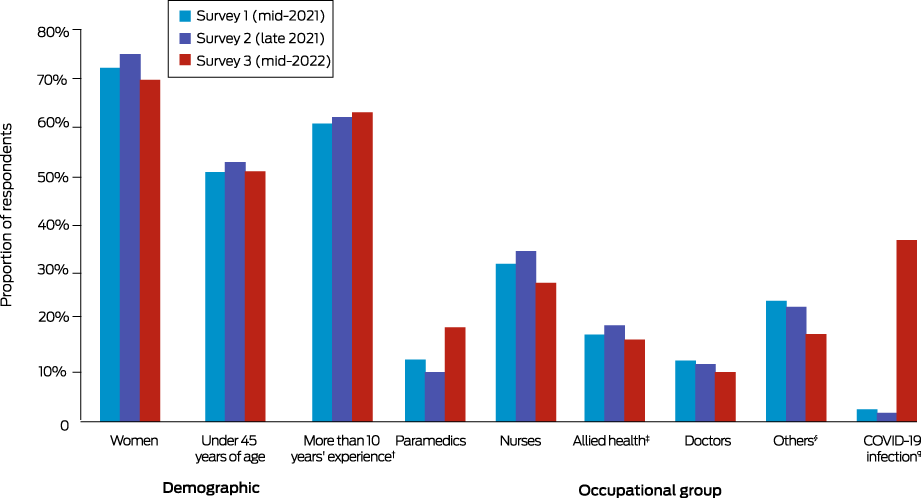
* The data for this graph, and also the characteristics of respondents by occupation group, are reported in the Supporting Information 2, table 2. † Work experience information was not available for new respondents recruited for survey 2. ‡ People working in audiology, chiropractic, dietetics, exercise physiology, medical radiation, occupational therapy, optometry, orthotics or prosthetics, pharmacy, physiotherapy, psychology, social work, speech pathology. § Administrative and clerical staff, orderlies, food service staff, information technology staff, engineering staff. ¶ Positive test result at any point since the beginning of the pandemic.
Box 3 – Adjusted proportions of respondents (all occupation groups) who reported moderate to severe symptoms of depression, anxiety, or post‐traumatic stress, or being irritable on at least some days (GAD‐7 item 6) or thoughts of being better off dead on at least some days (PHQ‐9 item 9), with 95% confidence intervals, by survey*
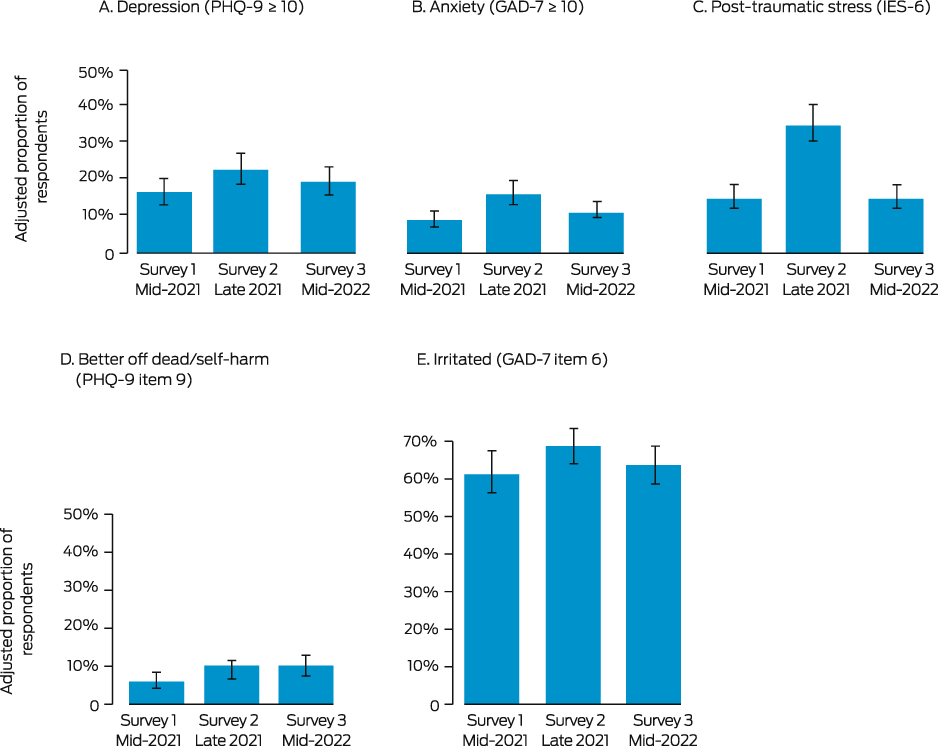
GAD‐7 = Generalised Anxiety Disorder 7‐item scale; IES‐6 = Impact of Event Scale – 6 items; PHQ‐9 = Patient Health Questionnaire – 9 items. * Multiple imputation of missing data, adjusted for age, gender, and socio‐economic status. The data for this graph are reported in the Supporting Information 2, table 3. The corresponding data by occupation group are depicted in the Supporting Information 2, figures 1 and 2.
Box 4 – Adjusted proportions of respondents (all occupation groups) who reported moderate to severe burnout or high optimism, with 95% confidence intervals, by survey*
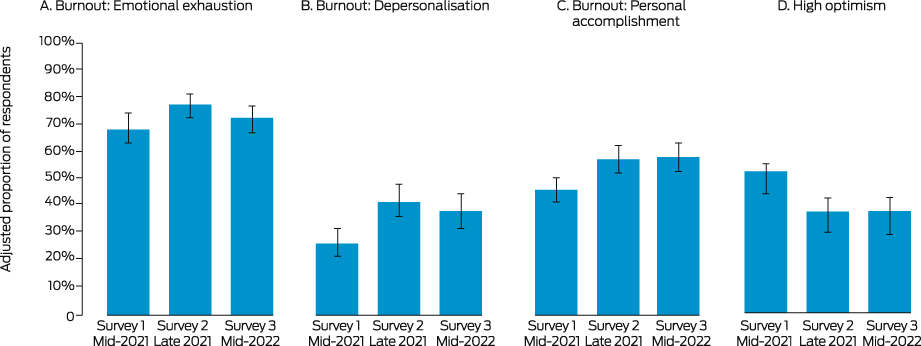
* Multiple imputation of missing data, adjusted for age, gender, and socio‐economic status. The data for this graph are reported in the Supporting Information 2, table 3. The corresponding data by occupation group are depicted in the Supporting Information 2, figures 3 and 4.
Box 5 – Adjusted mean scores for resilience, wellbeing, and life satisfaction (all occupation groups), with 95% confidence intervals, by survey*
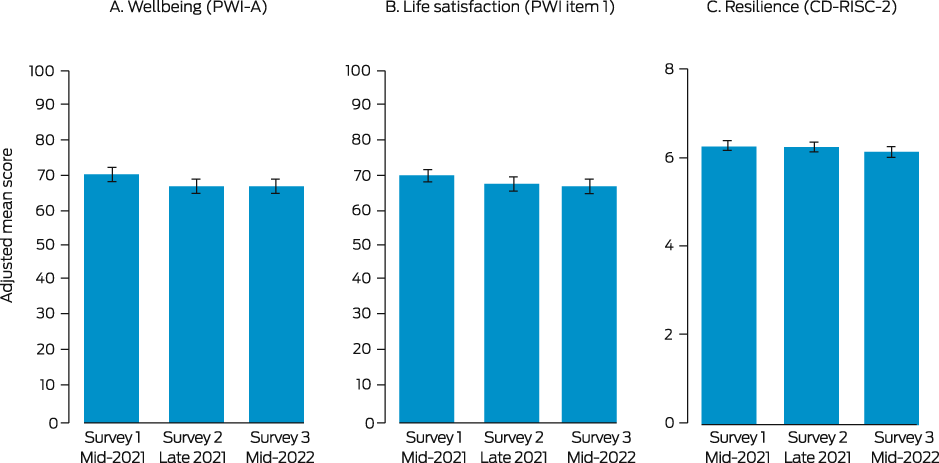
CD‐RISC‐2 = Connor‐Davidson Resilience Scale – 2 items; PWI‐A = Personal Wellbeing Index – Adult. * Multiple imputation of missing data, adjusted for age, gender, and socio‐economic status. The data for this graph are reported in the Supporting Information 2, table 4. The corresponding data by occupation group are depicted in the Supporting Information 2, figure 5.
Box 6 – Perceptions of psychosocial impact, workplace support, and personal COVID‐19 risk*
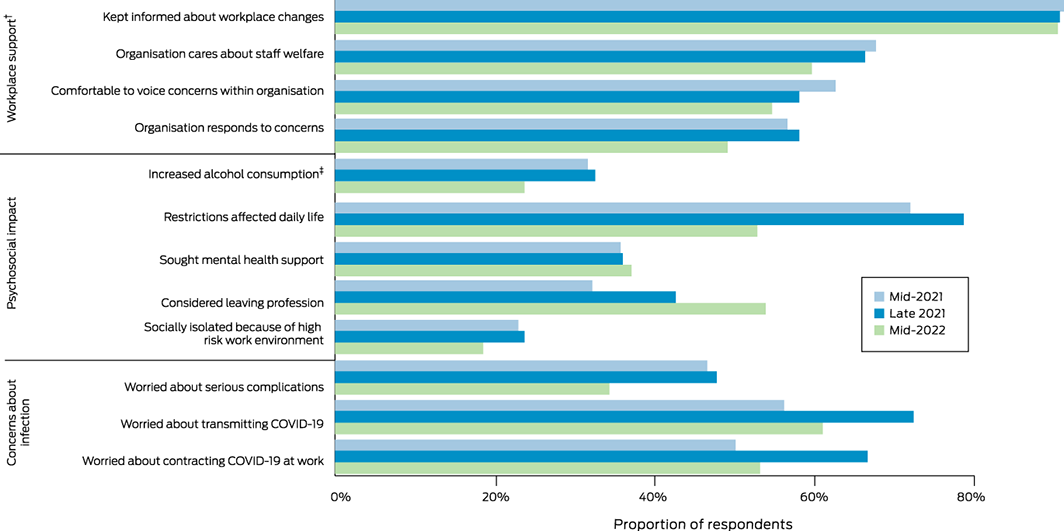
COVID‐19 = coronavirus disease 2019. * The data for this graph are reported in the Supporting Information 2, table 5. † Optional questions. ‡ Since the beginning of the pandemic in surveys 1 and 2, in the past six months in survey 3.
Received 15 December 2021, accepted 19 December 2022
- Sarah L McGuinness1,2
- Owen Eades1,2
- Kelsey L Grantham2
- Shannon Zhong1,2
- Josphin Johnson1,2
- Peter A Cameron2,3
- Andrew B Forbes2
- Jane RW Fisher2
- Carol L Hodgson1,2
- Jessica Kasza2
- Helen Kelsall2
- Maggie Kirkman2
- Grant M Russell2
- Philip L Russo2,4
- Malcolm R Sim2
- Kasha Singh5,6
- Helen Skouteris7
- Karen Smith2,8
- Rhonda L Stuart2,9
- James M Trauer2
- Andrew Udy1,10
- Sophia Zoungas2
- Karin Leder2,11
- 1 Alfred Health, Melbourne, VIC
- 2 Monash University, Melbourne, VIC
- 3 The Alfred Emergency and Trauma Centre, Alfred Health, Melbourne, VIC
- 4 Cabrini Health, Melbourne, VIC
- 5 The Peter Doherty Institute for Infection and Immunity, Melbourne, VIC
- 6 Peninsula Health, Melbourne, VIC
- 7 Monash Centre for Health Research and Implementation, Monash University, Melbourne, VIC
- 8 Ambulance Service of Victoria, Melbourne, VIC
- 9 Monash Health, Melbourne, VIC
- 10 Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne, VIC
- 11 Royal Melbourne Hospital, Melbourne, VIC
Open access
Open access publishing facilitated by Monash University, as part of the Wiley ‐ Monash University agreement via the Council of Australian University Librarians.
This investigation was supported by the Victorian Government COVID‐19 research fund (Department of Jobs, Precincts and Regions, HHSF/20/12957) and WorkSafe Victoria. The COVIC‐HA investigator team acknowledges the contributions of Allen Cheng, Danny Liew, and Helena Teede (Monash University) to the conceptualisation and delivery of the COVIC‐HA project. The COVIC‐HA investigator team also acknowledges all participating institutions and health care workers for their time and contribution to the COVIC‐HA project and their efforts to keep all Victorians safe throughout the COVID‐19 pandemic. Karin Leder (APP115500), Carol Hodgson (APP1173271), and Philip Russo (APP1156312) are supported by National Health and Medical Research Fellowships. James M Trauer is supported by a Monash Senior Postdoctoral Fellowship.
No relevant disclosures.
If you or anyone you know is experiencing distress, please call Lifeline on 13 11 14 (www.lifeline.org.au) or beyondblue (www.beyondblue.org.au) on 1300 22 46 36.
- 1. Marvaldi M, Mallet J, Dubertret C, et al. Anxiety, depression, trauma‐related, and sleep disorders among healthcare workers during the COVID‐19 pandemic: a systematic review and meta‐analysis. Neurosci Biobehav Rev 2021; 126: 252‐264.
- 2. Saragih ID, Tonapa SI, Saragih IS, et al. Global prevalence of mental health problems among healthcare workers during the Covid‐19 pandemic: a systematic review and meta‐analysis. Int J Nurs Stud 2021; 121: 104002.
- 3. Chutiyami M, Cheong AMY, Salihu D, et al. COVID‐19 pandemic and overall mental health of healthcare professionals globally: a meta‐review of systematic reviews. Front Psychiatry 2022; 12: 804525.
- 4. Searby A, Burr D, Redley B. The impact of COVID‐19 on nurse alcohol consumption: a qualitative exploration. J Clin Nurs 2022: https://doi.org/10.1111/jocn.16467 [online ahead of print].
- 5. Willis K, Maple JL, Bismark M, et al. A burnt‐out health workforce impacts patient care. The Conversation (Australia), 5 May 2022. https://theconversation.com/a‐burnt‐out‐health‐workforce‐impacts‐patient‐care‐180021 (viewed June 2022).
- 6. Australian Primary Health Care Nurses Association. One in four primary health care nurses plans to quit [media release]. 17 Feb 2022. https://www.apna.asn.au/about/media/one‐in‐four‐primary‐health‐care‐nurses‐plans‐to‐quit (viewed June 2022).
- 7. Buchan J, Catton H, Shaffer F; International Centre on Nurse Migration. Sustain and retain in 2022 and beyond: the global nursing workforce and the COVID‐19 pandemic. Jan 2022. https://www.intlnursemigration.org/wp‐content/uploads/2022/01/Sustain‐and‐Retain‐in‐2022‐and‐Beyond‐The‐global‐nursing‐workforce‐and‐the‐COVID‐19‐pandemic.pdf (viewed June 2022).
- 8. Harris PA, Taylor R, Minor BL, at al; REDCap Consortium. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019; 95: 103208.
- 9. McGuinness SL, Johnson J, Eades O, et al. Mental health outcomes in Australian healthcare and aged‐care workers during the second year of the COVID‐19 pandemic. Int J Environ Res Public Health 2022; 19: 4951.
- 10. von Elm E, Altman DG, Egger M, et al; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007; 335: 806‐808.
- 11. McGuinness SL, Josphin J, Eades O, et al. Organizational responses to the COVID‐19 pandemic in Victoria, Australia: a qualitative study across four healthcare settings. Front Public Health 2022; 10: 965664.
- 12. Australian Bureau of Statistics. 2033.0.55.001. Census of population and housing: Socio‐economic Indexes for Areas (SEIFA), Australia, 2016. IRSAD. 27 Mar 2018. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2033.0.55.001~2016~Main%20Features~IRSAD~20 (viewed June 2022).
- 13. Kenward MG, Roger JH. An improved approximation to the precision of fixed effects from restricted maximum likelihood. Computational Statistics and Data Analysis 2009; 53: 2583‐2595.
- 14. Sasaki N, Asaoka H, Kuroda R, et al. Sustained poor mental health among healthcare workers in COVID‐19 pandemic: a longitudinal analysis of the four‐wave panel survey over 8 months in Japan. J Occup Health 2021; 63: e12227.
- 15. Schmid B, Schulz SM, Schuler M, et al. Impaired psychological well‐being of healthcare workers in a German department of anesthesiology is independent of immediate SARS‐CoV‐2 exposure: a longitudinal observational study. Ger Med Sci 2021; 19: Doc11.
- 16. Porter AF, Sherry N, Andersson P, et al. New rules for genomics‐informed COVID‐19 responses: lessons learned from the first waves of the Omicron variant in Australia. PLoS Genet 2022; 18: e1010415.
- 17. Lamb D, Gafoor R, Scott H, et al. Mental health of healthcare workers in England during the COVID‐19 pandemic: a longitudinal cohort study [preprint]. medRxiv 2022.06.16.22276479; 16 June 2022. https://www.medrxiv.org/content/10.1101/2022.06.16.22276479v1 (viewed Aug 2022).
- 18. Wynter K, Holton S, Trueman M, et al. Hospital clinicians’ psychosocial well‐being during the COVID‐19 pandemic: longitudinal study. Occup Med (Lond) 2022; 72: 215‐224.
- 19. Fisher J, Tran T, Hammarberg K, et al. Quantifying the mental health burden of the most severe COVID‐19 restrictions: a natural experiment. J Affect Disord 2021; 293: 406‐414.
- 20. Butterworth P, Schurer S, Trinh TA, et al. Effect of lockdown on mental health in Australia: evidence from a natural experiment analysing a longitudinal probability sample survey. Lancet Public Health 2022; 7: e427‐e436.
- 21. Victorian Health Association. Pandemic Code Brown in place to support Victorian hospitals. 19 Jan 2022. Archived: https://web.archive.org/web/20230311025816/https://vha.org.au/news/pandemic‐code‐brown‐in‐place‐to‐support‐victorian‐hospitals (viewed Aug 2022).
- 22. Chowdhury R, Shah D, Payal AR. Healthy worker effect phenomenon: revisited with emphasis on statistical methods: a review. Indian J Occup Environ Med 2017; 21: 2‐8.
- 23. Lee SM, Kang WS, Cho AR, et al. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry 2018; 87: 123‐127.
- 24. Nickell LA, Crighton EJ, Tracy CS, et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ 2004; 170: 793‐798.
- 25. Marsden KM, Robertson IK, Porter J. Stressors, manifestations and course of COVID‐19 related distress among public sector nurses and midwives during the COVID‐19 pandemic first year in Tasmania, Australia. PLoS One 2022; 17: e0271824.






Abstract
Objectives: To assess the mental health and wellbeing of health and aged care workers in Australia during the second and third years of the coronavirus disease 2019 (COVID‐19) pandemic, overall and by occupation group.
Design, setting, participants: Longitudinal cohort study of health and aged care workers (ambulance, hospitals, primary care, residential aged care) in Victoria: May–July 2021 (survey 1), October–December 2021 (survey 2), and May–June 2022 (survey 3).
Main outcome measures: Proportions of respondents (adjusted for age, gender, socio‐economic status) reporting moderate to severe symptoms of depression (Patient Health Questionnaire‐9, PHQ‐9), anxiety (Generalized Anxiety Disorder scale, GAD‐7), or post‐traumatic stress (Impact of Event Scale‐6, IES‐6), burnout (abbreviated Maslach Burnout Inventory, aMBI), or high optimism (10‐point visual analogue scale); mean scores (adjusted for age, gender, socio‐economic status) for wellbeing (Personal Wellbeing Index–Adult, PWI‐A) and resilience (Connor Davidson Resilience Scale 2, CD‐RISC‐2).
Results: A total of 1667 people responded to at least one survey (survey 1, 989; survey 2, 1153; survey 3, 993; response rate, 3.3%). Overall, 1211 survey responses were from women (72.6%); most respondents were hospital workers (1289, 77.3%) or ambulance staff (315, 18.9%). The adjusted proportions of respondents who reported moderate to severe symptoms of depression (survey 1, 16.4%; survey 2, 22.6%; survey 3, 19.2%), anxiety (survey 1, 8.8%; survey 2, 16.0%; survey 3, 11.0%), or post‐traumatic stress (survey 1, 14.6%; survey 2, 35.1%; survey 3, 14.9%) were each largest for survey 2. The adjusted proportions of participants who reported moderate to severe symptoms of burnout were higher in surveys 2 and 3 than in survey 1, and the proportions who reported high optimism were smaller in surveys 2 and 3 than in survey 1. Adjusted mean scores for wellbeing and resilience were similar at surveys 2 and 3 and lower than at survey 1. The magnitude but not the patterns of change differed by occupation group.
Conclusion: Burnout was more frequently reported and mean wellbeing and resilience scores were lower in mid‐2022 than in mid‐2021 for Victorian health and aged care workers who participated in our study. Evidence‐based mental health and wellbeing programs for workers in health care organisations are needed.
Trial registration: Australian New Zealand Clinical Trials Registry: ACTRN12621000533897 (observational study; retrospective).